Back to Journals » OncoTargets and Therapy » Volume 11
Neuroendocrine tumor of the common bile duct: a case report and review of the literature
Authors Liu Z, Zhang DY, Lu Z, Zhang P, Sun WL, Ma X, Wu H, Wu BQ, Zhou S
Received 18 January 2018
Accepted for publication 12 March 2018
Published 23 April 2018 Volume 2018:11 Pages 2295—2301
DOI https://doi.org/10.2147/OTT.S162934
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Ingrid Espinoza
Zhong Liu,1 Deng-Yong Zhang,1 Zheng Lu,1 Pei Zhang,2 Wan-Liang Sun,1 Xiang Ma,1 Hua Wu,1 Bin-Quan Wu,1 Shuo Zhou1
1Department of General Surgery, The First Affiliated Hospital of Bengbu Medical College, Bengbu, People’s Republic of China; 2Department of Pharmacy, Bengbu Medical College, Bengbu, People’s Republic of China
Abstract: We report a rare case of neuroendocrine tumor (NET) in the common bile duct (CBD). The patient is a 56-year-old female who presented to our department with symptoms of fever but without jaundice. A preoperative examination showed a tumor in the CBD. The tumor volume was almost 5.5 × 4.5 × 4 cm3, which is the biggest NET in the CBD reported on PubMed. The imaging results (computed tomography [CT] and magnetic resonance imaging [MRI]) were not consistent with CBD adenocarcinoma. The tumor appeared to oppress the growth of the CBD rather than originate in the bile duct wall; combined with the low blood bilirubin index and lack of jaundice symptoms, the preoperative diagnosis was not clear. We performed a radical resection of the cholangiocarcinoma. The patient recovered well before going home. The pathology was NET (Grade 2). The patient showed no recurrence to date, without intravenous chemotherapy (8 months).
Keywords: bile duct adenocarcinoma, neuroendocrine tumors, bile duct
Introduction
Neuroendocrine tumors (NETs) are rare tumors that are derived from peptidergic neurons and neuroendocrine cells. NETs can be seen in multiple organ tissues throughout the body, including the digestive tract, lung, thymus, and uterus.1 NETs most often occur in the gastrointestinal tract and pancreatic tissue and are rare in the common bile duct (CBD). We report a NET that occurred in the middle of the CBD, with a volume of 5.5 × 4.5 × 4 cm3. This is the biggest NET in the CBD (except for other pathologic types, such as neuroendocrine carcinoma [NEC] and mixed adenoneuroendocrine carcinoma) reported on PubMed.
Case presentation
A 56-year-old woman was referred to our department for intermittent fever over the past 4 months. An ultrasonic inspection indicated a solid hypoechoic mass located in the hepatic hilar area close to the right side of the CBD; the intrahepatic bile duct and main pancreatic duct were expansive. Magnetic resonance imaging (MRI) indicated expanded intrahepatic and extrahepatic bile ducts, enlargement of the gallbladder, and a tumor located on the CBD with an iso-signal intensity on a T2-weighted image (Figure 1A). The computed tomography (CT) analysis indicated dilatation of the intrahepatic bile duct, the soft-tissue density in the first hilar, and that it was indistinct from the pancreas. The tumor had an inhomogeneous enhancement after enhancement during the CT detection (Figure 1B). The blood biochemical tests showed the following: alanine aminotransferase 113 U/L, aspartate transaminase 77 U/L, carbohydrate antigen 19-9 (CA19-9) 64.61 IU/mL, without any other abnormalities.
Treatment
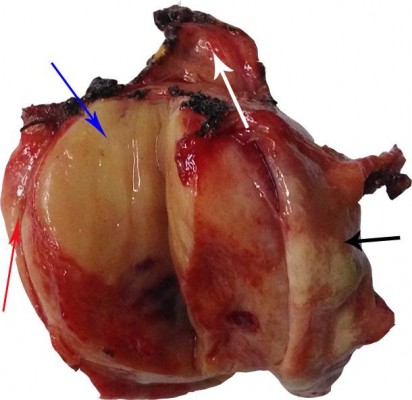
The preoperative diagnosis was that of cholangiocarcinoma or other intraperitoneal tumor compression of the bile duct. We conducted an exploratory laparotomy and found a tough tumor located in the CBD, protruding from the wall of the bile duct to the right abdominal. The tumor was not completely blocking the bile duct lumen and there were no other tissues encroaching on the surrounding tissues, including the portal vein, hepatic artery, inferior vena cava, and pancreas. We excised the CBD 2 cm above and below the tumor with a hepatoduodenal ligament lymph node dissection. The Roux-en-Y anastomosis was conducted for the proximal bile duct and jejunum. The intraoperative pathology of the bile duct showed no tumor cells. The surgical resection specimen is shown in Figure 2.
The pathology is shown in Figure 3: NET of the bile duct (Grade [G] 2) of size 6 × 4.5 × 4 cm3. Histological sections were prepared from the excised bile duct (−), and immunohistochemical staining was performed for cytokeratin ++, C7−/+, cluster of differentiation 56 +, synaptophysin (Syn) ++, α 1 anti-chymotrypsin −/+, chromogranin A (CgA) −, antigen Ki-67 (Ki-67) + (12%). The patient has demonstrated tumor-free survival for 8 months after the operation (to date) without chemotherapy.
Patient consent
This study was approved by the Institutional Review Board of Bengbu Medical College. The patient provided written informed consent and gave permission for the use of biopsies and publication of case details, including publication of the images.
Discussion
The gastrointestinal tissues are the most common site for NETs. The incidence of NET is approximately 75% of digestive tract tumors, and NEC just accounts for approximately 0.1%–0.2% of digestive tract tumors.1,2 In the biliary system, the incidence of NET accounts for just 0.2%–2.0% of tumors,3 and NEC accounts for 0.19% of bile duct tumors,4 because there are no neuroendocrine cells in the extrahepatic bile duct mucosa. For extrahepatic bile duct NET, the common hepatic duct and distal CBD are sites of predilection (accounting for 19.2% of bile duct tumors); the middle of the CBD accounts for 17.9% of tumors, the cystic gall duct accounts for 16.7%, and the proximal CBD accounts for 11.5%.5,6 Many researchers believe that NETs are often derived from chromaffin cells and Kulchitsky cells, both of which originate from the endoderm.7 The bile duct tissues rarely contain these cells, which is why bile duct NET is rare. At present, the etiology of bile duct NETs is unclear. Some studies indicate that NETs are linked with cholelithiasis and congenital malformation of the biliary tract, both of which lead to chronic inflammation.8 Chronic inflammation leads to metaplasia of bile duct epithelial cells, and then metaplasia into NET.
According to previous literature,9,10 cholangiocarcinoma is often located in the upper third of the bile duct and demonstrates invasive growth behavior. The pathology of most cholangiocarcinomas is that of adenocarcinoma, and CBD NETs are rare. The degree of differentiation of NETs is usually determined through immunohistochemistry. NET can be divided into three grades (G1–G3, Table 1), according to the number of mitotic images and the Ki-67 index.11 Poorly differentiated NETs (also known as NECs, which are classed as G3) can be divided into three types according to the tumor cell type: large cell NEC, small cell NEC, and adenocarcinoma-NEC, which are combined with adenocarcinoma and NET cells.12,13 Other rare types of NETs also exist, such as goblet cell carcinoid and tubular carcinoid.12,13 Many biomarkers are used for diagnosis, such as Syn and CgA. In our case, the immunohistochemical staining results were Syn++ and CgA−, the Ki-67 was 12%, and the mitotic index was approximately 2%, indicating NET G2.
  | Table 1 The common bile duct NETs previously published in PubMed |
Surgical radical resection is the main treatment for choledochus NETs. The operation is classified into three types according to the position of the mass: pancreaticoduodenectomy (tumor located in the distal CBD), bile duct resection, and cholangiojejunostomy (tumor located in the middle CBD), combined with partial hepatectomy for patients who have liver metastases. The National Comprehensive Cancer Network guidelines for gastrointestinal and pancreatic NETs indicate that lymph node dissection is advocated, but there is no uniform standard for the extent of specific dissection. Furthermore, there was no uniform standard before the operation in the current study, and chemotherapy could not be performed because of the difficulty in diagnosis before the operation. Currently, cisplatin and etoposide are often used for chemotherapy after surgery. In a study consisting of 21 patients with biliary duct and pancreatic NEC, who were treated with platinum-based chemotherapy after surgery, three were sensitive to the chemotherapy; the median progression-free survival was 1.8 months, and median overall survival was 5.8 months.21 For low-grade NETs, most patients demonstrated good survival after radical surgery, and the 10-year survival rate was approximately 80%. The survival time for patients with poorly differentiated NEC is short; the majority of NEC patients, especially small-cell NEC patients, died within 1 year.4 According to the 2010 WHO classification guidelines for digestive system tumors, extrahepatic bile duct NETs had metastasized in nearly 1/3 of patients at the time of diagnosis, and the 5-year survival rate was 60%–100%. The prognosis of NEC patients was very poor, with 40%–50% of patients with tumor metastasis at the time of diagnosis, and the 5-year survival rate was low.12 Combined with the data reported by Michalopoulos et al, we can see that patients without lymph node dissection develop intraperitoneal organ metastasis soon after surgery; otherwise, the probability of metastasis is lower. The bile duct NET (G3) patients without postoperative chemotherapy died sooner, whereas patients who underwent postoperative chemotherapy and those who did not undergo chemotherapy had all survived at the reported follow-up time.6 In our case, the patient (NET G2) has survived until now without any chemotherapy. Therefore, we believe that postoperative prophylactic intravenous chemotherapy is beneficial for NETs, especially for patients in G3. Many more clinical trials are ongoing, and these results will clarify this point.
In this case, the patient presented to our ward with fever. The ultrasound analysis found a tumor in the extrahepatic bile duct without the symptom of jaundice (we speculate that the bile duct was not blocked completely by the exophytic tumor). CT and MRI indicated a bile duct tumor; the levels of CA19-9 in the blood were high. We first considered the possibility of cholangiocarcinoma. However, when we considered the uncommon symptoms and CT results the enhancement degree of CT in the arterial phase for cholangiocarcinoma is lower than for the liver, and it is often a delayed enhancement. In this case, the enhancement was early. In addition, the tumor demonstrated exophytic growth, which is unusual in bile duct cholangiocarcinoma. We had doubts about the diagnosis of bile duct cancer before surgery. Some clinicians consider that a biopsy of an endoscopic retrograde cholangiopancreatography (ERCP) for a bile duct mass is a reasonable diagnostic method, which helps to characterize a tumor and guide subsequent surgery. However, we did not consider ERCP, as the bile duct biopsy may cause complications such as bile leakage. Such patients must undergo surgery to remove the tumor and so we conducted an exploratory laparotomy (preparing for radical resection of bile duct cancer). The postoperative pathologic diagnosis was NET (G2).
NETs (G1–G3, except for any other pathologic types) in extrahepatic bile ducts are rare. We found no more than 100 cases on PubMed. PubMed contains just 45 cases of NETs in the CBD (except for NETs in the gallbladder and cystic duct, ampulla, hail bile duct, and left or right hepatic ducts in the liver and also except for any other pathology, such as adenocarcinoma-NET). Michalopoulos et al reported approximately 38 cases from 1961 to 2013.6 Combining the cases from Michalopoulos et al and the other 8 cases of NET of the CBD, 48 cases are included in Table 1. We found that bile duct NETs do not have an endocrine function. Patients with non-functional NETs in the CBD often have the symptom of jaundice first, with or without the symptom of fever and abdominal discomfort. Because of the absence of a specific symptom, NETs in the CBD are often considered to be cholangiocarcinoma, leading to a misdiagnosis.
The WHO has made a classification for extrahepatic and gallbladder tumors, including the bile duct and gallbladder NETs. However, there are no uniform guidelines for NET treatment, especially for radiotherapy and chemoradiotherapy postoperatively. It is useful to report this uncommon tumor. If more cases were reported, uniform guidelines for the treatment of NET of the CBD could be established. In conclusion, patients with CBD NETs of G1–2 demonstrate good survival after resection without chemotherapy. We recommend lymph node dissection for NET of the CBD.
Acknowledgment
This study was supported by the Key Research and Development Plan of Anhui Province, People’s Republic of China (1604a0802088).
Disclosure
The authors report no conflicts of interest in this work.
References
Liang HJ. Diagnosis and treatment of gastroenteropancreatic neuro-endocrine neoplasms. Chin J Digest Surg. 2014;13:756–759. Chinese. | ||
Albores-Saavedra J, Murakata L, Krueger JE, Henson DE. Noninvasive and minimally invasive papillary carcinomas of the extrahepatic bile ducts. Cancer. 2000;89(3):508–515. | ||
Bosman FT, Carneiro F, Hruban RH, Theise ND. W H O Classification of Tumours of the Digestive System. Lyon: IARC Press. 2010;195–334. | ||
Albores-Saavedra J, Batich K, Hossain S, Henson DE, Schwartz AM. Carcinoid tumors and small-cell carcinomas of the gallbladder and extrahepatic bile ducts: a comparative study based on 221 cases from the Surveillance, Epidemiology and End Results Program. Ann Diagn Pathol. 2009;13(6):378–383. | ||
Hosoda K, Kobayashi A, Shimizu A, et al. Neuroendocrine tumor of the common bile duct. Surgery. 2016;160:525–526. | ||
Michalopoulos N, Papavramidis TS, Karayannopoulou G, Pliakos I, Papavramidis ST, Kanellos I. Neuroendocrine tumors of the extrahepatic biliary tract. Pathol Oncol Res. 2014;20(4):765–775. | ||
Takahashi K, Sasaki R, Oshiro Y, Fukunaga K, Oda T, Ohkohchi N. Well-differentiated endocrine carcinoma originating from the bile duct in association with a congenital choledochal cyst. Int Surg. 2012;97(4):315–320. | ||
Park SB, Moon SB, Ryu YJ, et al. Primary large cell neuroendocrine carcinoma in the common bile duct: first Asian case report. World J Gastroenterol. 2014;20(47):18048–18052. | ||
Hong N, Kim HJ, Byun JH, et al. Neuroendocrine neoplasms of the extrahepatic bile duct: radiologic and clinical characteristics. Abdom Imaging. 2015;40(1):181–191. | ||
Sasatomi E, Nalesnik MA, Marsh JW. Neuroendocrine carcinoma of the extrahepatic bile duct: case report and literature review. World J Gastroenterol. 2013;19(28):4616–4623. | ||
Kulke MH, Shah MH, Benson AB, et al. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®: Neuroendocrine Tumors). Version 2. http://guide.medlive.cn/guideline/13095. Accessed March 29, 2017. | ||
Rindi G, Petrone G, Inzani F. The 2010 WHO classification of digestive neuroendocrine neoplasms: a critical appraisal four years after its introduction. Endocr Pathol. 2014;25:186–192. | ||
Kihara Y, Yokomizo H, Urata T, et al. A case report of primary neuroendocrine carcinoma of the perihilar bile duct. BMC Surg. 2015;15:125. | ||
Aigner B, Kornprat P, Schöllnast H, et al. A case of focal small-cell neuroendocrine carcinoma in the vicinity of the extrahepatic bile duct, adjacent to an extensive biliary intraepithelial neoplasm: a diagnostic challenge with major clinical implications. Anticancer Res. 2015;35:4821–4828. | ||
Oshiro Y, Gen R, Hashimoto S, et al. Neuroendocrine carcinoma of the extrahepatic bile duct: a case report. World J Gastroenterol. 2016;22:6960–6964. | ||
Murakami M, Katayama K, Kato S, et al. Large-cell neuroendocrine carcinoma of the common bile duct: a case report and a review of literature. Surg Case Rep. 2016;2:141. | ||
Sánchez Cabús S, Pittau G, Sebagh M. Primary non-functioning neuroendocrine tumor of the extrahepatic bile duct. Rev Esp Enferm Dig. 2016;109:228–229. | ||
Raspanti C, Falco N, Silvestri V, et al. Neuroendocrine tumor of the common bile duct: case report. G Chir. 2016;37:275–280. | ||
Khan FA, Stevens-Chase A, Chaudhry R, et al. Extrahepatic biliary obstruction secondary to neuroendocrine tumor of the common hepatic duct. Int J Surg Case Rep. 2017;30:46–49. | ||
Hoepfner L, White JA. Primary extrahepatic bile duct neuroendocrine tumor with obstructive jaundice masquerading as a Klatskin tumor. J Surg Case Rep. 2017;6:1–3. | ||
Iwasa S, Morizane C, Okusaka T, et al. Cisplatin and etoposide as first-line chemotherapy for poorly differentiated neuroendocrine carcinoma of the hepatobiliary tract and pancreas. Jpn J Clin Oncol. 2010;40:313–318. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



