Back to Journals » Infection and Drug Resistance » Volume 13
Neonatal Sepsis and Its Associated Factors Among Neonates Admitted to Neonatal Intensive Care Units in Primary Hospitals in Central Gondar Zone, Northwest Ethiopia, 2019
Authors Agnche Z, Yenus Yeshita H, Abdela Gonete K
Received 12 August 2020
Accepted for publication 26 October 2020
Published 3 November 2020 Volume 2020:13 Pages 3957—3967
DOI https://doi.org/10.2147/IDR.S276678
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Suresh Antony
Zelalem Agnche,1 Hedja Yenus Yeshita,2 Kedir Abdela Gonete3
1Amhara Regional State, Central Gondar Zone, West Dembia District, Kolladba Primary Hospital, Kolladba, Ethiopia; 2Department of Reproductive Health, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia; 3Department of Human Nutrition, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Correspondence: Kedir Abdela Gonete
University of Gondar, P.O. BOX: 196, Gondar, Ethiopia
Email [email protected]
Background: Neonatal sepsis contributes substantially to neonatal morbidity and mortality and is an ongoing major global public health challenge particularly in developing countries. Studies conducted on the proportion and risk factors of neonatal sepsis in Ethiopia are from referral hospitals, which may not be generalized to primary health care units where a significant proportion of mothers give birth in these health facilities. This study sought to determine the proportion of clinical neonatal sepsis and associated factors in the study areas.
Methods: Institutional-based cross-sectional study was conducted from March to April 2019, in Amhara regional state, central Gondar zone public primary hospitals in Ethiopia. A total of 352 subjects (mother-neonate pairs) were selected using a systematic random sampling technique and pre-tested and structured questionnaires were used to collect data. Multivariable logistic regression analysis was fitted to identify factors associated with neonatal sepsis. Adjusted odds ratio (AOR) with the corresponding 95% confidence interval (CI) was used to show the strength of associations and variables with p-values of < 0.05 were considered as statistically significant.
Results: The overall proportion of neonatal sepsis was 64.8% (95% CI (59.2, 69.2)). Being male neonate (AOR=3.7; 95% CI (1.76, 7.89)), history of urinary tract infections during the index pregnancy (AOR =6, 26; 95% CI (1.16, 33.62)), frequency of per-vaginal examination greater than three during labor and delivery (AOR=6.06; 95% CI (2.45, 14.99)), neonatal resuscitation at birth (AOR=6.1; 95% CI (1.71, 21.84)), place of delivery at the health center (AOR=3.05; 95% CI (1.19, 7.79)), lack of training of health workers on neonatal resuscitation and infection prevention practices (AOR=2.14; 95% CI (1.04, 4.44)), late age of neonate at onset of illness (AOR=0.05; 95% CI (0.01, 0.21)) and maternal age of 30– 34 years (AOR=0.19; 95% CI (0.047, 0.81)) were significantly associated with neonatal sepsis.
Conclusion: The proportion of neonatal sepsis is high. Maternal, neonatal, and health service related factors were identified for neonatal sepsis. Therefore, training of health workers, provision of health care services as per standards, and monitoring and evaluation of obstetrical/neonatal care during labor and delivery are mandatory.
Keywords: neonatal sepsis, risk factors, neonatal intensive care units
Background
Neonatal sepsis (NS) is defined as systemic inflammatory response syndrome in the presence of or as a result of suspected or proven infection in a neonate.1 Neonatal sepsis contributes substantially to neonatal morbidity and mortality and is an ongoing major global public health challenge.2 According to the World Health Organization (WHO), globally each year over 4 million neonates died within 28 days of birth.3 Infections are considered to be the leading cause of neonatal deaths (35%) followed by deaths resulted from preterm births (28%), intrapartum related complications (24%), and asphyxia (23%).4
Globally 7% of mortality in children under 5 years and 15% in neonates were related to sepsis and meningitis in 2016.4 Sepsis is the commonest cause of neonatal mortality and is probably responsible for 30–50% of the total neonatal deaths each year in developing countries.4 It is estimated that in 2012 about 6.9 million neonates were diagnosed with a possible serious bacterial infection needing treatment and 2.6 million of these occurred in Sub-Saharan Africa.5,6
In Ethiopia; prematurity (37%), infection (28%), and asphyxia (24%) are the most common causes of death in neonates. Neonatal conditions which used to account for a quarter of under-five deaths in 2004 have recently increased to 43%. According to the current united nation estimate in Ethiopia, the neonatal deaths were reduced slowly by 48% in 2013 from 1990 as compared to a significant reduction rate of under-five mortality by 67%.7
Ethiopia demographic and health survey (EDHS, 2016) reported that the neonatal mortality rate was 29/1000 live birth, which was reduced slowly from 39/1000 in 2005 and 37/1000 live births in 2011. Particularly Amhara region of the country was at the top in infant and neonatal mortality rates (NMRs). It was 67 and 47 per 1000 live births, respectively.8
Neonatal sepsis also has an economic impact that resulted from increased medical costs, prolonged hospital stay, and potentially poor long-term neurodevelopmental outcomes. Despite this fact, the world is witnessing a steady decline in the number of neonatal deaths due to sepsis.9,10
Multiple factors including maternal, fetal, and environmental factors have been associated with increased risk of infections in neonatal life.11
Early identification of the risk factors for neonatal sepsis would enable clinical diagnosis and treatment aiming to reduce neonatal morbidity and mortality.5 The implementation of certain clinical strategies is also effective in reducing the incidence of neonatal sepsis.12
The burden of neonatal sepsis and its complications can be averted and the target of Sustainable Development Goals for child survival can be achieved through the expansion of clinical care for babies and mothers.13 Hence, there have been many advances in the prevention, assessment, and treatment of neonatal sepsis in the past few decades. However, the morbidity and mortality associated with sepsis remain high for susceptible neonates.13
World Health Assembly resolution (WHA) makes several recommendations including prevention, diagnosis, and treatment of sepsis in national health systems, training all health professionals on infection prevention and patient safety, promoting research, and others. Therefore, sepsis is considered as a good example of a crosscutting approach for measurable reductions in neonatal mortality.14
In Ethiopia, various efforts have been made to reduce neonatal morbidity and mortality. However, some studies conducted in referral hospitals of the country showed that neonatal morbidity and mortality related to neonatal sepsis are still high.15
Despite a considerable burden of neonatal sepsis in our setting, there were no studies conducted to assess the proportion and associated factors of neonatal sepsis among neonates admitted in NICUs to recently established primary hospitals in Ethiopia. Therefore, this study was carried out to determine the proportion of neonatal sepsis and factors contributing to it among neonates in central Gondar Zone public primary hospitals of the Amhara region in Ethiopia.
Methods
Study Design, Setting, and Period
An Institutional-based cross-sectional study was conducted in the Amhara region at central Gondar zone public primary hospitals in Ethiopia from March to April 2019. These hospitals were established recently in the last few years. They are providing preventive, promotive, and curative health care services to the population in the central Gondar zone of the region and serve as a referral center for the local health centers in the area. These primary hospitals are found in five districts (Dembiya, Chilga, Wogera, Delgi, and East Belesa) in the central Gondar zone of the region. They are 781, 780, 787, 832, and 867 km away from Addis Ababa, the capital city of Ethiopia towards the Northwest, respectively. All hospitals have a total number of 341 health workers. The neonatal intensive care units of each hospital have five neonatal beds for neonatal admission and have three clinical staff (one physician and two clinical nurses) and one cleaner. More than three thousand neonates were admitted to these hospitals annually to get medical services.
Study Population and Sampling Procedure
All neonates admitted to neonatal intensive care units in central Gondar Zone primary hospitals were included in the study. The sample size was determined by using a single population proportion formula and the proportion was taken from the previous literature in Ethiopia. According to a study conducted at Gondar University teaching hospital, the prevalence of neonatal sepsis was 69.7%.23 By considering 95% confidence interval (CI), 5% marginal error, and 5% non-response rate. Therefore the final minimum adequate sample size was 352.
The study participants included 352 mother-neonate pairs who were admitted to NICUs during the study period and consented to participate in the study. The study enrolled neonates from birth to 28 days of age. Neonates with sepsis admitted for two or more times during the study period were considered to be excluded to avoid double counting. However, there were no such cases in this study. The study populations were neonates admitted and treated in NICUs in central Gondar zone public primary hospitals in Ethiopia. According to the data obtained from these hospitals in 2018, the annual number of neonates admitted in neonatal intensive care units (NICUs) of these hospitals was estimated to be 3000 ie on average 375 neonates were estimated to be admitted during the study period. A systematic random sampling technique was used to select study subjects during the study period. In this study neonatal sepsis is asserted when a medical diagnose of the neonate is stated as “neonatal sepsis” by the physician in the neonate’s medical record chart.
Data Collection Tool, Measurements, and Quality Management
The tool was developed from different kinds of literature to gather the desired information from the sample population. The questionnaire was initially prepared in the English language and translated into Amharic (local language) and again it was retranslated back to the English language to check for any inconsistencies or distortions in the meaning of words and concepts. Two days of training were given to five data collectors (clinical nurses, diploma) and two supervisors (BSc nurses) before the beginning of data collection. Data collectors collected the data from the mother or caregiver of the neonates by using the interviewer-administered structured Amharic version questioner that contains detailed questions comprising all the variables of the study. The admission diagnosis of neonates was taken from the diagnosis of the physician in the unit. The data collectors cross verify the diagnosis of neonatal sepsis with reviewed neonate’s medical record to ascertain the final clinical diagnosis of neonatal sepsis before they collect the data.
The WHO IMNCI criteria were applied to assess babies for clinical sepsis. The IMNCI criteria use the following clinical features to make a diagnosis of clinical neonatal sepsis: not feeding well, convulsions, drowsy or unconscious, the movement only when stimulated or movement at all, fast breathing (60 breaths per min), grunting severe chest in-drawing, raised temperature > 38 °C, hypothermia < 35.5 °C, central cyanosis or could be severe jaundice, severe abdominal distension or localizing signs of infection were diagnosed as having neonatal sepsis.6,17
A retrospective review of the history was taken to find out if the neonate had the symptoms suggestive of neonatal sepsis since birth. A conclusion of clinical neonatal sepsis was ascertained if the baby had any one of the symptoms of sepsis listed in the IMNCI criteria and admitted in NICUs. Medical documents from the health units attended were also used to get information on the presentation of the patient to the health units and the treatment received.
Data were checked for its completeness and accuracy during data collection. Close supervision of trained data collectors (five diploma nurses) was undertaken by the trained supervisors (two BSc nurses). The supervisor strictly supervised the data collection process and provided on-site advice and feedback to the data collectors on daily basis. The daily exchange of information between the principal investigator and supervisors was undertaken by telephone. The principal investigator had had regular onsite supervision of supervisors and data collectors on weekly basis.
Operational Definitions
Neonatal sepsis: Neonates presented with any one of the systemic manifestations of danger signs:- not feeding well, convulsions, drowsy or unconscious, the movement only when stimulated or no movement at all, fast breathing (60 breaths per min), grunting severe chest in-drawing, raised temperature > 38 °C, hypothermia < 35.5 °C, central cyanosis or could be severe jaundice, severe abdominal distension or localizing signs of infection were diagnosed as having neonatal sepsis.6,17
Early onset of sepsis: If sepsis is occurring from birth to 7 days of age.
Late onset of sepsis: If sepsis is occurring between 8 and 28 days of age.18
Data Management and Analysis
Questionnaires were checked daily for completeness and accuracy. All data were double entered, cleaned, edited, coded, and entered into EPI INFO version 7.0 and exported to SPSS version 20.0 for analysis by the binary logistic regression model. Both bivariate and multivariable analyses were used to see the association of different variables. Categorical variables were summarized into percentages and proportions. The continuous variables were summarized into means, medians, standard deviation, and ranges, and the results were presented with tables and figures. The proportion of clinical neonatal sepsis was obtained by calculating the proportion of neonates with symptoms and signs of clinical neonatal sepsis out of the total number of neonates who were admitted to NICUs during the study period. Bivariate analysis was used to determine the association between neonatal sepsis and various independent variables including maternal factors, neonatal factors, and service related factors. Continuous independent variables were categorized and associations established using Chi-squared tests. This was similarly done for categorical variables. An adjusted odds ratio with 95% confidence interval was used to measure the degree of association between variables. P-value of < 0.05 was considered as statistically significant during multivariable logistic regression.
Results
Neonatal Characteristics
A total of 338 mother-neonates pairs were included in five primary hospitals in the central Gondar Zone making the response rate of 96%. The median age of neonates was 2 days with an interquartile range of 4 days. Among all participants, more than half of 200 (59.2%) were male neonates with male to female ratio 1.4:1. Nearly two-thirds of neonates were born at hospitals 212 (62.7%). Similarly, nearly two-thirds of 218 (64.5%) neonates were term and the remaining one-third 120 (35.5%) were preterm. Low birth weight was illustrated among 53.5% of neonates (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Neonates Admitted to Neonatal Intensive Care Units (NICUs) of Central Gondar Zone Primary Hospitals, Northwest Ethiopia, 2019 |
Mothers Socio-Demographic and Economic Characteristics
The median age of mothers of the neonate was 26 years with an interquartile range of 8 years and 4 months. Among the participants, one-third of neonate’s mother 114 (33.7%) were in the age range of 25 to 29 years. More than half of 195 (57.7%) them were from rural areas (Table 2).
 |
Table 2 Socio-Demographic and Economic Characteristics of Mothers of Neonates Admitted to NICU in Central Gondar Zone Primary Hospitals, Northwest Ethiopia, 2019 |
Mothers Medical and Obstetric Conditions
In this study, more than half of the mothers 202 (59.8%) were multiparous women. The majority of the mothers 314 (92.9%) had at least one ANC follow-up at the time of pregnancy and 10 (3%) of them were positive with HIV AIDS. Among the positive mothers, the majority 7 (70%) were from urban areas. About one-third101 (29.9%) of them had a history of PROM during the index pregnancy and nearly three-fourths of 247 (73.1%) neonates were delivered by spontaneous vaginal delivery (Table 3).
 |
Table 3 Medical and Obstetrical Characteristics of Mothers of Neonates Admitted to NICU in Central Gondar Zone Primary Hospitals, Northwest, Ethiopia, 2019 |
Medical Procedures Related to Neonatal Health Care Services
None of the neonates were on mechanical ventilation. About 2.7% of neonates had a history of end tracheal intubation for resuscitation and 61 (18%) were on oxygen therapy through an intranasal oxygen catheter or face mask (Table 4).
 |
Table 4 Medical Procedures are Done for Neonates Who Were Admitted to NICU in Central Gondar Zone Primary Hospitals, Northwest Ethiopia, 2019 |
The Proportion of Neonatal Sepsis and Clinical Characteristics of Neonates
Two-thirds of the neonates158 (72.1%) were admitted within one week of age and the overall proportion of Neonatal sepsis was 64.8% (95% CI (59.2, 69.2)). Of these, 158 (72.1%) were early onset neonatal sepsis. Gross congenital malformation like neural tube defect, cleft palate, and hydrocephalus was also found in 7 (2.1%) of neonates (Table 5 and Figure 1).
 |
Table 5 Clinical Characteristics of Neonates Who Were Admitted to Central Gondar Zone Primary Hospitals, Northwest Ethiopia, 2019 |
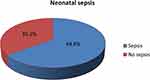 |
Figure 1 The proportion of neonatal sepsis among neonates admitted in central Gondar zone primary hospitals, Northwest Ethiopia, 2019. |
Factors Associated with Neonatal Sepsis
All the variables which fulfilled the chi-square assumption were fitted into bivariable and multivariable logistic regression. Residency, age of the neonate, sex of neonate, place of birth, gestational age, birth weight, maternal age, maternal marital status, parity, ANC follow-up, duration of labor, history of UTI/STIs, history of PROM, history of foul smelling liquor, birth asphyxia, place of delivery and training of health works at NICUs fulfilled the variable screening criteria (p-value < 0.2) and entered into multivariable logistic regression analysis. Consequently, the age of the neonate, sex of neonates, maternal age, history of UTIs, frequency of PV examination, resuscitation at birth, and getting care from trained health workers were significantly associated with neonatal sepsis at multivariable with less than 0.05 p values.
Accordingly, the sex of neonates showed a significant association with the risk of the onset of neonatal sepsis. The odds of having neonatal sepsis among male neonates were 3.7 times higher as compared to female neonates [AOR = 3.73; 95% CI (1.76, 7.89)]
This study showed that neonates born to mothers who had UTIs during the index pregnancy had 6 times higher odds of developing sepsis as compared to those neonates born from mothers who did not have a UTIs during the index pregnancy [AOR =6.26; 95% CI[(1.16, 33.62)]]. Likewise, increased odds of neonatal sepsis was noted among mothers who have a history of more than three PV examination during labor compared to mothers who had PV examination less than or equal to three [AOR = 6.06; 95% CI [(2.45, 14.99)]].
Similarly, those neonates who were resuscitated at birth had 6 times higher odds of developing sepsis compared to those neonates who were not resuscitated [AOR = 6.110; 95% CI[(1.71, 21.84)]]. Nevertheless, the odds of neonatal sepsis decreased by 95% among neonates whose age is less than one week compared to those aged greater than a week [AOR = 0.05; 95% CI[(0.01, 0.21)]].
Maternal age was significantly associated with neonatal sepsis. Neonates from older mother whose age is 30–34 years were 81% less likely to develop neonatal sepsis when compared to neonates from mothers whose age is 35 years and older [AOR=0.19; 95% CI (0.05, 0.81)].
Place of delivery also has a significant effect on neonatal sepsis. Neonates delivered in the health center were three times more likely to develop sepsis compared to those delivered at the hospital [AOR=3.05; 95% CI (1.19, 7.79)].
Finally, neonates who get care by health workers who had no training on NICU/IPPs were 2 times more likely to develop sepsis as compared to neonates who get care by trained health professionals. [AOR = 2.14; 95% CI [(1.04, 4.44)]] (Table 6).
 |
Table 6 Bivariable and Multivariable Analysis of Factors Associated with Neonatal Sepsis Among Neonates Admitted at Central Gonad Zone Primary Hospitals, Northwest Ethiopia, 2019 |
Discussion
Neonatal sepsis contributes substantially to neonatal morbidity and mortality and is a major global public health challenge.10 In this study, the overall proportion of neonatal sepsis was 64.8% (95% CI (59.2, 69.2)).
This finding is in line with a study conducted in Gondar (67.9%).16 The possible reason for having similar results might be due to similarities of study population studied in the same area and the period in which the studies were conducted. This finding is, however, much higher than the findings of studies from Uganda (11%),6 India (32%),11 Tanzania (31.4%),5 and Nigeria (34%).19 This difference might have been contributed by methodological differences and the difference in diagnostic modality to confirm neonatal sepsis. In contrast to the finding of these studies the prevalence of neonatal sepsis in Bishoftu (72.2%)20 and Shashemene (77.9%)15 were much higher than the current finding. This higher prevalence is likely since these study sites are referral hospitals, most frequently receiving neonates with complications as well as complicated pregnancies. Furthermore, these differences could be due to the difference in sample size, socio-demographic, and economic status of the study population and access to health facilities.15
In this study, neonates born from mothers who had a history of urinary tract infections (UTIs) during the index pregnancy were six times more likely to develop neonatal sepsis. This finding is in agreement with the findings of studies conducted previously in Mekelle21 and Bishoftu20 which revealed that maternal urinary tract and sexual infections were a significant factor for the development of neonatal sepsis. This finding may support the reason that maternal health problem is often associated with neonatal sepsis, especially if untreated during the third trimester pregnancy or labor. Hence, neonatal sepsis may result from the colonization of the birth canal by the infectious agent.20,22
This study also identified significant associations between neonatal resuscitation and neonatal sepsis. The odds of developing neonatal sepsis among neonates who have a history of neonatal resuscitation at birth were six times higher as compared to neonates who were not resuscitated. This finding was in agreement with studies from Bangladesh,22 Tanzania5 and Ghana23 which identified neonatal resuscitation at birth was a significant risk factor for neonatal sepsis. Resuscitation procedures at birth pose a greater risk of neonatal sepsis. Many life-supporting procedures such as suctioning and endotracheal intubations can lead to transient and persistent bacteremia.22 Newborn infants are especially vulnerable to nosocomial infections because of their intrinsic susceptibility to infection as well as the performance of invasive procedures for neonatal resuscitation to which they are subjected.23 Studies from China, Korea, and Ethiopia revealed that different medical procedures which are undertaken below the optimal level of asepsis (sterility or disinfection) for the management of neonatal health problems predispose the neonate to a great risk of neonatal sepsis15,24,25 This might result from poor practices and non-adherence to guideline by health professionals during resuscitation that may predispose the neonate with a greater risk of developing sepsis.23
Furthermore, in this study neonatal age was found to be a significant factor for neonatal sepsis. Neonates whose ages were less than or equal seven days were 95% less likely to develop neonatal sepsis compared with the age of neonates greater than seven days of age. This finding is in line with finding from a study in Ghana23 and Shashemene (Ethiopia)15 which revealed that the probability to develop sepsis increased with increasing neonatal age. Nosocomial and community acquired neonatal infections occur after 3 days of life. Consequently, this will affect the prevalence of late onset neonatal sepsis.26 This is also supported by the finding from this study which revealed that the majority of neonates were delivered in the health institutions. This may in turn increase the possibility to develop neonatal sepsis after discharged from these institutions at a late age.
Per-vaginal examination (PV) during labour and delivery was found to be a significant factor for neonatal sepsis. Neonates from mothers who had a history of PV examination greater than three were six times more likely to develop neonatal sepsis. This finding was in line with finding from a study in Bangladesh in which neonates of mothers who have a history of vaginal examination greater than three was found to be 2.5 times more likely to develop neonatal sepsis.22 Vaginal organisms can be introduced into the cervical canal even during sterile conditions. Hence, babies are at risk from ascending infection thought to be caused by vertical transmission from an infected mother. Therefore, the vaginal examination can increase the risk of harm for women and their babies.27 However, a study in Mekelle, Ethiopia reported that there was no significant association between PV examination and neonatal sepsis21 This may also result from differing in study settings where the quality of obstetrical and neonatal health care services provided to mothers and neonates in primary hospitals differs to that of referral hospitals.
The sex of neonates was significantly associated with neonatal sepsis. This study found that being male was 3.7 times more likely to develop neonatal sepsis as compared to their counterparts. This finding is in agreement with the finding of a study in Australia. It reported that the risk of neonatal sepsis was found to increase three times more in male neonates as compared to female neonates.28 Male sex is associated with a higher risk of neurological, pulmonary, cardiovascular, and infectious morbidities as well as overall mortality when compared to female infants of similar preterm gestation.29 Important differences in the immune response between male and female preterm neonates have also been noted.30 However, the etiology of sex-specific differences in disease remains relatively undetermined and is likely multifactorial, with genetic, immunological, and hormonal influences playing key roles.28
The place of birth was found to be statistically significant with neonatal sepsis. Neonates delivered at the health center were three times more likely to develop sepsis as compared to neonates delivered at hospitals. This finding is in agreement with findings from studies in Nigeria19 and Ethiopia.3,19 This might be due to the reason that neonates who were delivered at the health center may be less likely to be screened based on a risk approach and treated with intrapartum antibiotic prophylaxis.31 Furthermore, the difference in the level of knowledge about maternal and neonatal health among health workers in hospitals and health centers and the level of adherence of health workers to guidelines and protocols on IPPs to prevent infections in newborns might be the possible reason for this finding.
Maternal age was also significantly associated with neonatal sepsis. Neonates from mothers whose age was from 30–34 years were 81% less likely to develop neonatal sepsis as compared to those neonates from mothers older than 35 years. However, studies from Bangladesh22 and Tanzania5 showed that the attack rates of sepsis increased significantly among neonates born from mothers less than 20yrs of age. This difference may result from the high number of mothers less than 20 years of age in Bangladesh (67%), and Tanzania (17.7%) as compared to the current finding (13.6%) in Ethiopia. The sample size and methodological difference may also have an impact on this difference.
Training of health workers in NICUs in all matters related to neonatal health and infection prevention, in particular, was significantly associated with neonatal sepsis. Pathogenic agents can be transmitted by direct contact or indirectly via contaminated equipment, intravenous fluids, medications, blood products, or enteral feedings.26 Poor practices and non-adherence to guidelines by health professionals during resuscitation and other medical procedures may predispose the neonate with a greater risk of developing sepsis.23 This might not be different from the finding of the current study.
Residence, ANC, parity, duration of labor, mode of delivery, foul smelling liquor, birth asphyxia, PROM, gestational age, and birth weight were not found to be predictors of neonatal sepsis in this study. This is against the findings of studies on risk factors of neonatal sepsis in different parts of the world.15,19–23
Conclusion
The proportion of neonatal sepsis is high. Late neonatal age at onset of sepsis, being male sex, 30 −34 years of age of the mother, neonatal resuscitation at birth, history of urinary tract infections during pregnancy, frequency of per-vaginal examinations greater than three times during labor and delivery, and place o delivery (health center) were identified risk factors for neonatal sepsis. Therefore, training of health workers, provision of health care services as per standards, and monitoring and evaluation of obstetrical/neonatal care during labor and delivery are mandatory.
Limitations of the Study
Since the study was done on admitted neonates, these findings may lack generalizability to the entire population in the catchment area. Additionally, Clinical diagnosis of neonatal sepsis may overestimate the proportion of neonatal sepsis.
Abbreviations
ANC, Antenatal Care; APGAR, Appearance; Pulse; Grimace; Activity and respiration; CNS, Central Nervous System; EDHS, Ethiopia Demographic and Health Service Survey; EONS, Early Onset Neonatal Sepsis; HEW,Health Extension Workers; HIV, Human Immune Deficiency Virus; LMICs, Low and Middle Income Countries; LONS, Late Onset Neonatal Sepsis; NICU, Neonatal Intensive Care Unit; NMR, Neonatal Mortality Rate; NS, Neonatal Sepsis; PMTCT, Prevention of Mother to Child Transmission; PROM, Premature Rupture of Membrane; PV, Per-vaginal Examination; STIs, Sexually Transmitted Infections; SVD, Spontaneous Vaginal Delivery; UTIs, Urinary Tract Infections; VDRL, Venereal Disease Research Laboratory; VLBW, Very Low Birth Weight; WHO, World Health Organization.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Consideration
The proposal was reviewed and approved by the institutional review board (IRB) of the University of Gondar, Institute of Public Health College of Medicine and Health Science before the start of the study. The study was conducted in accordance with the ethical principles of the Declaration of Helsinki. The Mothers were delivered written informed consent to participate. A neonate aged 0 to 28 days of age who met the selection criteria was enrolled in the study. A pre-tested interviewer administered questionnaire was used to obtain history, physical examination, and evaluate factors associated with neonatal sepsis. These included maternal factors, neonatal factors and neonatal health care practices, and service related factors.
Acknowledgments
The authors would like to thank the study participants, data collectors, and the supervisor.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article was submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
The authors have declared that there was no funding.
Disclosure
We, the authors, declare that there is no competing interest.
References
1. Goldstein B, Giroir B, Randolph A. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics*. Pediatr Crit Care Med. 2005;6(1):2–8. doi:10.1097/01.PCC.0000149131.72248.E6
2. UNICEF. Committing to Child Survival: A Promise Renewed Progress Report. New York; 2014.
3. Yamey G, Horváth H, Schmidt L, Myers J, Brindis CD. Reducing the global burden of Preterm Birth through knowledge transfer and exchange: a research agenda for engaging effectively with policymakers. Reprod Health. 2016;13(26):1–9. doi:10.1186/s12978-016-0146-8
4. Nighat A, Nasrul H. Disease Burden of NICU at a Tertiary Care Hospital, Karachi, Pakistan. J DOW Univ Health Sci. 2012;6(1):32–35.
5. Jabiri A, Wella HL, Semiono A, Sariah A, Protas J. Prevalence and factors associated with neonatal sepsis among neonates in Temeke and Mwananyamala Hospitals in Dar es Salaam, Tanzania. Tanzan J Health Res. 2016;18(4):1–7.
6. Kayom VO, Mugalu J, Kakuru A, Kiguli S, Karamagi C. Burden, and factors associated with clinical neonatal sepsis in urban Uganda: a community cohort study. BMC Pediatr. 2018;18(1):355. doi:10.1186/s12887-018-1323-4
7. FMOH (Ethiopia). Health sector transformation plan (2015/16-2019/20); 2015.
8. CSA. Federal Democratic Republic of Ethiopia Demographic and Health Survey. Addis Ababa, Ethiopia; 2016.
9. Liang L, Kotadia N, English L, et al. Predictors of mortality in neonates and infants hospitalized with sepsis or serious infections in developing countries: a systematic review. Front Pediatr. 2018;6(October):1–12.
10. WHO and UNICEF. Every Newborn: An Action Plan to End Preventable Deaths: Executive Summary. Geneva; 2014.
11. Gandhi S, Ranjan K, Neelima R, Neha S. Incidence of neonatal sepsis in a tertiary hospital: an overview. Int J Med Sci Public Health. 2013;2(3):548–552. doi:10.5455/ijmsph.2013.090320131
12. Kim JK, Chang YS, Sung S, Ahn SY, Park WS. Trends in the incidence and associated factors of late-onset sepsis associated with improved survival in extremely preterm infants born at 23 – 26 weeks ’ gestation: a retrospective study. BMC Pediatr. 2018;18(172):1–9. doi:10.1186/s12887-018-1130-y
13. Maryniak K. Neonatal Sepsis: Assessment and Care. RN.com; 2015:1–51.
14. WHO. WHO sepsis technical expert meeting; 2018:1–36. Available from: http://www.who.int/sepsis/en/.
15. Getabelew A, Aman M, Fantaye E, Yeheyis T. Prevalence of neonatal sepsis and associated factors among neonates in neonatal intensive care unit at selected Governmental Hospitals in Shashemene Town, Oromia Regional State, Ethiopia, 2017. Int J Pediatr. 2018;2018:1–7. doi:10.1155/2018/7801272
16. Demisse AG, Alemu F, Gizaw MA, Tigabu Z. Patterns of admission and factors associated with neonatal mortality among neonates admitted to the neonatal intensive care unit of University of Gondar Hospital, Northwest Ethiopia. Pediatr Health Med Ther. 2017;8:57–64.
17. FMOH (Ethiopia). Neonatal Intensive Care Unit Management Protocol. Addis Abeba, Ethiopia; 2014.
18. Tewabe T, Mohammed S, Tilahun Y, et al. Clinical outcome and risk factors of neonatal sepsis among neonates in Felege Hiwot referral hospital, Bahir Dar, Amhara Regional State, North West Ethiopia 2016: a retrospective chart review. BMC Res Notes. 2017;10(1):1–7. doi:10.1186/s13104-017-2573-1
19. Shobowale E, Ogunsola FT, Oduyebo OO, et al. Aetiology and risk factors for neonatal sepsis at the Lagos University Teaching Hospital Idi-Araba, Lagos, Nigeria. South Africa J Child Health. 2016;10(3):4–7.
20. Woldu M, Lenjisa J, Tegegne G, Tesfaye G, Dinsa H, Guta M. Assessment of the incidence of neonatal sepsis, its risk factors, antimicrobials use and clinical outcomes in Bishoftu general hospital, neonatal intensive care unit, Debrezeit-Ethiopia. Int J Contemp Pediatr. 2014;4(4):1. doi:10.5455/2349-3291.ijcp20141102
21. Gebremedhin D, Berhe H, Gebrekirstos K. Risk factors for neonatal sepsis in public hospitals of Mekelle City, North Ethiopia, 2015: unmatched case control study. PLoS One. 2016;11(5):1–10. doi:10.1371/journal.pone.0154798
22. Hasan S. Predictive values of risk factors in neonatal sepsis. J Bangladesh Coll Physicians Surg. 2011;29(4):187–195. doi:10.3329/jbcps.v29i4.11324
23. Adatara P, Afaya A, Salia SM, et al. Risk factors associated with neonatal sepsis: a case study at a Specialist Hospital in Ghana. Sci World J. 2019;2019:0–2.
24. Hwang J, Choi C, Chang Y, et al. The efficacy of clinical strategies to reduce nosocomial sepsis in extremely low birth weight infants. J Korean Med Sci. 2005;20:177–181. doi:10.1016/j.drudis.2016.09.013
25. Wu IH, Tsai MH, Lai MY, et al. Incidence, clinical features, and implications on outcomes of neonatal late-onset sepsis with concurrent infectious focus. BMC Infect Dis. 2017;17(1):1–10. doi:10.1186/s12879-017-2574-7
26. Md. Behrman RE, Md. Kliegman RM, Md. Jenson HB, Editors. Nelson Textbook of Pediatrics 17th Edition (May 2003). WB Saunders, OkDoKeY; 2003:629–630.
27. Lesley D. The vaginal examination during labour: is it of benefit or harm ? New Zeal Coll Midwives J. 2010;42:21–26.
28. Driscoll DNO, Mcgovern M, Greene CM, Molloy EJ. Gender disparities in preterm neonatal outcomes. Found Acta Pædiatrica. 2018;107(Acta Pædiatrica ISSN 0803–5253):1494–1499. doi:10.1111/apa.14390
29. Kent AL, Wright IM, Abdel-Latif ME. Mortality and adverse neurologic outcomes are greater in preterm male infants. Australian neonatal, territory care, intensive audit, units. Am Acad Pediatr. 2012;129(1):124–131.
30. O’Driscoll DN, Greene CM, Molloy EJ. Immune function ? A missing link in the gender disparity in preterm neonatal outcomes. Expert Rev Clin Immunol. 2017;13:1061–1071. doi:10.1080/1744666X.2017.1386555
31. Edmond K. New approaches to preventing, diagnosing, and treating neonatal sepsis. PLoS Med. 2010;7(3):1–8.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
