Back to Journals » Clinical Epidemiology » Volume 15
Neonatal Phototherapy and Clinical Characteristics: The Danish National Patient Registry 2000–2016
Authors Sun Y , Petersen JP, Wu C, Dreier JW, Maimburg RD, Henriksen TB , Christensen J
Received 23 June 2022
Accepted for publication 23 December 2022
Published 25 January 2023 Volume 2023:15 Pages 123—136
DOI https://doi.org/10.2147/CLEP.S373289
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Eyal Cohen
Yuelian Sun,1– 4 Jesper Padkær Petersen,5 Chunsen Wu,6,7 Julie Werenberg Dreier,3,8 Rikke Damkjær Maimburg,9– 11 Tine Brink Henriksen,5 Jakob Christensen1,2
1Department of Neurology, Aarhus University Hospital, Aarhus, Denmark; 2Department of Clinical Medicine, Aarhus University, Aarhus, Denmark; 3National Centre for Register-Based Research, Aarhus University, Aarhus, Denmark; 4Department of Clinical Epidemiology, Aarhus University Hospital, Aarhus University, Aarhus, Denmark; 5Department of Paediatrics, Clinical Institute, Aarhus University, Aarhus University Hospital, Aarhus, Denmark; 6Department of Clinical Research, University of Southern Denmark, Odense, Denmark; 7Department of Gynaecology and Obstetrics, Odense University Hospital, Odense, Denmark; 8Centre for Integrated Register-Based Research (CIRRAU), Aarhus University, Aarhus, Denmark; 9Department of Clinical Medicine, Aarhus University, Denmark; Department of Occupational Health, Aarhus University Hospital, Aarhus, Denmark; 10Department of Midwifery, University College of Northern Denmark, Hjørring, Denmark; 11School of Nursing and Midwifery, Western Sydney University, Blacktown, NSW, Australia
Correspondence: Yuelian Sun, Department of Neurology, Department of Clinical Epidemiology, Aarhus University Hospital, Aarhus, Denmark, Email [email protected]
Purpose: Phototherapy is the standard treatment for neonatal hyperbilirubinemia. It is important to collect data on phototherapy to support research related to the efficacy and safety of phototherapy. We explored the registration of phototherapy in the Danish National Patient Registry (DNPR) and the clinical characteristics of neonates treated with phototherapy.
Methods: We identified children born alive in Denmark from 1 January 2000 through 30 November 2016 from the DNPR (N=1,044,502). We calculated the proportion of children registered that received phototherapy during the neonatal period and examined temporal trends, both nationwide and at the level of individual hospitals. In a sub-cohort of children born at Aarhus University Hospital (AUH) in 2002– 2016 (N=71,781), we analyzed the proportions of children registered that received phototherapy, according to sex, gestational age, birth weight, and neonatal characteristics, like Apgar score, birth asphyxia, and infections.
Results: We identified 11,295 (1.1%) registered that received phototherapy. The proportions of children registered that received phototherapy differed among hospitals (range: 0 to 4.1%). Nationwide registration was low during the study period, but it increased to 1.8% in 2016. For the AUH sub-cohort the proportion of children registered with phototherapy averaged 4.4% (N=3182, range:3.9– 5.1%). The proportion of children registered with phototherapy was inversely correlated with gestational age and birth weight, and positively correlated with neonatal characteristics, including low Apgar score, birth asphyxia, and infections.
Conclusion: Phototherapy was under-reported in the DNPR and the proportions of children registered that received phototherapy differed among hospitals. The non-compulsory policy for reporting treatment and care in hospitals to the DNPR might explain the variation. The most consistent reporting was observed among children born in an university hospital, where 4.4% of children registered that received phototherapy, and phototherapy was inversely associated with gestational age, birth weight, and positively associated with clinical characteristics like birth asphyxia, and infections.
Keywords: Danish National Patient Registry, health administrative data, neonates, hyperbilirubinemia, neonatal jaundice, phototherapy
Introduction
Phototherapy is the standard treatment for hyperbilirubinemia in neonates. In severe cases, phototherapy is combined with immunoglobulin treatment and exchange transfusion.1 Phototherapy has saved the lives of millions from death and disability, since 1957, when it was introduced as a treatment for hyperbilirubinemia.2 Although phototherapy is known to reduce serum bilirubin levels effectively, some unresolved questions remain, related to the effectiveness and safety of phototherapy.3 For example, the efficacy of phototherapy in reducing mortality and morbidity remains unquantified, and it remains unclear whether phototherapy increases the short-term risk of asthma or the long-term risk of cancer.3 Access to valid information on phototherapy is important for research on its effectiveness and safety. The Danish National Patient Registry (DNPR) contains information on disease diagnoses, surgical procedures, in-hospital treatments, and care, including phototherapy.4,5 The Danish Health and Medicines Authority guidelines for registering treatments in the DNPR state that “It is not compulsory to register all treatment and care, but the individual department has the opportunity to register the treatment and care of interest at a clinically meaningful level.”6 Thus, for some treatments and care (including phototherapy), there is little incentive to reporting, which often results in incomplete registration. Here, we explored the nationwide registration of phototherapy in the DNPR. Preliminary analyses showed that phototherapy was evidently under-reported in the DNPR across the nation, except at the Aarhus University Hospital (AUH). Therefore, we analyzed an AUH sub-cohort to explore in detail the proportions of phototherapy registered annually and the clinical characteristics of children registered with phototherapy.
Methods
Study Population
We examined the Danish Medical Birth Registry7,8 to identify all children born alive in Denmark from 1 January 1997 through 30 November 2016 (N=1,063,119). Children were excluded when they could not be linked to the Danish Civil Registration System (N=576) or had a missing value for gestational age (N=18,041). Thus, 1,044,502 children were included in the analyses.
In Denmark, all residents are assigned a unique identification number in the Danish Civil Registration System,9 which enables linkage between nationwide registries. All data were analyzed at Statistics Denmark with encrypted identification numbers. According to Danish law, analyses of anonymous data do not require approval from an ethical review board. The study was approved by the Danish Data Protection Agency.
Information on the Registration of Phototherapy
The DNPR, established in 1976, is a national registry of data on the activities performed at Danish hospitals. The DNPR contains information on the diagnosis, surgery, treatment, and care related to each hospital contact.4 Phototherapy is registered in the DNPR with the procedure code BNGC for phototherapy in general population and the procedure code BNGC0 for phototherapy to neonates. We included children registered that received phototherapy within 28 days after the birth.
In Denmark, the Danish Pediatric Society developed guidelines for treating neonatal hyperbilirubinemia with phototherapy, and two major versions were issued (in 1992 and 2012).10,11 In the 1992 version, phototherapy was indicated for bilirubin levels above the criteria that corresponded to 10% of the birth weight, in grams, and 300 µmol/L was set as the criteria if the amount of 10% of the birth weight was larger than 300.11 The latest guidelines (the 2012 version) defined the criteria for phototherapy based on the age of the child when bilirubin was measured and the birth weight. When the bilirubin measurement is taken at 72 h or later after birth, phototherapy is indicated for bilirubin levels above 350, 250, 200, and 100 µmol/L, for children with birth weights >2500, 1500–2499, 1000–1499, or <1000 g, respectively. For children born at gestational ages 34–36 weeks with a birth weight >2500 g, phototherapy is indicated when the bilirubin level is above 300 µmol/L.10
Information on Bilirubin Testing
For children born at AUH, information on bilirubin measurements was obtained from the clinical laboratory information system (LABKA).12 The LABKA system contains test results from samples taken in a public or private hospital, or by a general practitioner, that were sent to a clinical chemistry department. The database was considered to include full geographical coverage for the Central Denmark region, where Aarhus University Hospital is located, since the year 2000.12 The main bilirubin measurements examined in this study were: the total serum bilirubin concentration and the unconjugated bilirubin concentration. The total serum bilirubin was coded with NPU04145 and NPU01370 in the LABKA where the code NPU04145 was specifically used for the measurement in neonates. The unconjugated bilirubin was coded with NPU01366. These data also contained information on the sampling date, sampling time, results, and test units. We included all the measurements measured within 28 days after the birth.
Information on Birth and Neonate Characteristics
We accessed the Danish Medical Birth Registry to obtain information on the sex, singleton or multiple births (twins+), gestational age, birth weight, parity, Apgar score at five minutes, and the hospital of birth (see Supplementary Table 1 for a list of hospitals). Based on gestational ages and birth weights, we identified children born small for gestational age (SGA), appropriate size for gestational age (AGA), and large for gestational age (LGA). SGA was defined as a birth weight below the 10th percentile for the corresponding gestational age. LGA was defined as a birth weight above the 90th percentile for the corresponding gestational age. AGA was defined as a birth weight between the 10th and 90th percentiles for the corresponding gestational age. We obtained information on neonate characteristics from the DNPR. Those data included birth asphyxia, acidosis, infection (including sepsis), newborn brain disturbances, birth injury, infant of mother with diabetes syndrome, hypoglycemia, underfeeding, neonatal convulsions, respiratory disorders, cardiovascular disorders, intracranial hemorrhage, hemolytic disease (including the type of disease), and neonatal jaundice diagnosis (see Supplementary Table 2 for the ICD-10 codes). Some of these factors were shown to be related to decisions of giving phototherapy treatment to neonates.13 We assigned children a given characteristic, when the DNPR indicated that they had a primary or secondary diagnosis of the disease or condition during the neonatal period. We also obtained information from the DNPR on the birth delivery method and any diagnoses of major congenital malformations in the first year of life (see Supplementary Tables 2 and 3 for the ICD-10 codes).
Analyses
Children were followed from birth to age 28 days, death, or emigration, whichever came first. All of children were followed up for 28 days if they did not die or emigrated in the neonatal period. We calculated the proportion of children registered with phototherapy in the entire country and the proportions registered in the individual hospitals. We also investigated the temporal trends in registering phototherapy in the DNPR.
We conducted a detailed analysis of phototherapy registrations in the neonatal period among children born at AUH from 1 January 2002 through 30 November 2016 (N=71,781). First, we estimated the proportions of children registered with phototherapy, according to sex (girls/boys), number of births in a pregnancy (ie, singleton, twins or more), gestational age (20–27, 28–31, 32–34, 35, 36, 37, 38, or 39–45 weeks), birth weight (<1000, 1000–1499, 1500–1999, 2000–2499, 2500–2999, 3000–3499, 3500–3999, or ≥4000 g), neonate size (SGA, AGA, LGA), maternal parity (1, 2+), Apgar score at 5 minutes, major congenital malformation in the first year of life, delivery method, and other characteristics observed in the neonatal period (see Supplementary Table 2). To estimate the proportion of children that were registered with phototherapy among children born at gestational ages 20–27 weeks and among children with birth weights <1000 g, we excluded children that died within the first two days after birth. Children born in a multiple birth are more likely to be born at a shorter gestational age. Therefore, we estimated the proportions of children that were registered with phototherapy, grouped according to gestational age, separately for singletons and children of a multiple birth. We also estimated the proportions of children that were registered with phototherapy, grouped according to neonate size, separately for children born preterm and children born at term. Second, we estimated the temporal trends of phototherapy registration among children, according to sex, the number of births in a pregnancy, gestational age, birth weight, neonate size, and parity. Third, we estimated the proportions of children with and without phototherapy that underwent a bilirubin measurement, including total serum bilirubin and/or unconjugated bilirubin, during the neonatal period.
All analyses were performed with STATA, version 16 (StataCorp LLC, College Station, TX, USA).
Results
Among children born from 1 January 2000 to 30 November 2016 (N=1,044,502), we identified 11,295 (1.1%) children registered with phototherapy in the DNPR. Phototherapy registration varied among the hospitals studied; the proportion of children registered with phototherapy ranged from 0 to 4.1% (Supplementary Table 1). In five hospitals, more than 2.0% of children were registered with phototherapy in the DNPR. AUH had reported the highest proportion of children (4.1%) treated with phototherapy between 2000 and 2016, followed by Regional Hospital West Jutland (3.5%), Odense University Hospital (2.6%), Roskilde Hospital (2.4%), and Regional Hospital Central Jutland (2.3%) (Supplementary Table 1).
Nationwide registration of phototherapy in the DNPR was low in 2000 (0.3%) and increased by the end of the study period in 2016 (1.8%; Figure 1). Phototherapy registration at the AUH was low in 2000 (0.5%) and 2001 (0.5%), but it increased to a high level in 2002 (4.5%), and maintained this level to 2016. We found that, at AUH, 3.9–5.1% of all newborns were registered with phototherapy annually between 2002 and 2016 (Figure 1). Temporal trends in neonatal phototherapy registrations at other selected hospitals varied much (Figure 1).
 |
Figure 1 Trends in the registration of neonatal phototherapy in the Danish National Patient Registry, nationwide and at selected Hospitals, during 2000–2016. |
In the sub-cohort of children born at AUH from 2002 through 2016 (N=71,781), we identified 3182 (4.4%) children registered with phototherapy in the DNPR (Table 1). More boys than girls were registered with phototherapy (4.7% vs 4.1%); however, the proportions observed during the individual calendar years showed that the rate was not consistently higher in boys than in girls (Figure 2). The gestational age at birth was inversely correlated with phototherapy registration (Table 1, Figure 3). For example, 86.1% of children born at gestational age 20–27 weeks were registered with phototherapy, compared to 0.5% of those born at gestational age 39–45 weeks (Table 1). The trends in phototherapy registration for children at different gestational ages were stable during 2002–2016 (Figure 3). Similarly, birth weight was inversely correlated with phototherapy (Table 1, Figure 4). Neonatal size (SGA, AGA, LGA) was associated with phototherapy indicating children born SGA were more likely to be registered with phototherapy than children born AGA (Tables 1 and 2). The patterns of children registered with phototherapy for children born LGA compared with children born AGA, however, were different between children born preterm and children born at term (Table 2). Among children born preterm, children born LGA were less likely to be registered with phototherapy than children born AGA (27.7% vs 41.6%, Table 2). Conversely, among children born at term, children born LGA were more likely to be registered with phototherapy than children born AGA (1.4% vs 0.7%, Table 2). The trend of proportion of children registered with phototherapy according to neonatal size is presented in Figure 5.
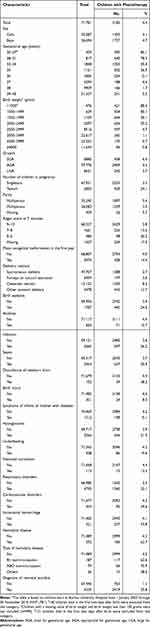 |
Table 1 Registration of Phototherapy According to Newborn Characteristicsa |
 |
Table 2 Proportion of Children Registered with Phototherapy According to Growth and Gestational Age (Preterm and Term)a |
Only 3.3% of singletons were registered with phototherapy in the DNPR; however, 24.1% of children born in multiple births (twins+) were registered with phototherapy (Table 1). The trend of registering singletons treated with phototherapy was stable throughout the study period. However, the trend of registering twins treated with phototherapy was lower in 2016 than in previous years (Figure 6). When children were grouped by gestational age, we found that, at gestational ages 28–37 weeks, the proportion of children registered with phototherapy was lower among children of multiple births than among singletons of the same category of gestational age (Table 3).
 |
Table 3 Proportion of Children Registered with Phototherapy According to Gestational Age Among Singletons and Twinsa |
Children born to nulliparous mothers were more likely to have phototherapy than children born to multiparous mothers (5.4% vs 3.5%; Table 1), and this difference was stable throughout the study period (Figure 7). Children with a low Apgar score at 5 minutes, birth asphyxia, acidosis, sepsis, newborn brain disturbances, hemolytic diseases, etc, were more likely to be registered with phototherapy than children without the corresponding disorder (Table 1). For example, 62.7% of children diagnosed with a hemolytic disease were registered with phototherapy; this proportion included 62.6% of children with hemolytic disease due to Rhesus isoimmunization and 70.9% with hemolytic disease due to ABO isoimmunization. A high proportion of children with intracranial hemorrhage (73.8%) were also registered with phototherapy (Table 1). Among children with a diagnosis of neonatal jaundice in the DNPR, 55.8% were registered with phototherapy (Table 1). Among children 3182 children registered with phototherapy, 763 (24.0%) children, however, did not have a diagnosis of neonatal jaundice.
Among all the children that received phototherapy, 97.4% had a bilirubin measurement, irrespective of gestational age. In contrast, among children that did not receive phototherapy, only 15.1% had a bilirubin measurement, and the percentage varied substantially according to gestational age (Table 4). The mean maximum bilirubin measured in the neonatal period was lower among children without phototherapy than among children with phototherapy (Table 4). The difference between these two groups was only 10.9 µmol/l for children born at gestational ages <32 weeks, but the difference was 124.8 µmol/l for children born at gestational ages >38 weeks.
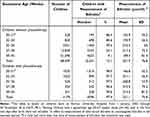 |
Table 4 Clinical Measurement of Bilirubin in the Neonatal Period According to Phototherapy and Gestational Agea |
Discussion
This study showed that only 1.1% of neonatal children were registered with phototherapy between 2000 and 2016 in Denmark. However, the proportion varied from 0 to 4.1% among hospitals. The nationwide registration of phototherapy in the DNPR was, on average, low over the study period, but it increased to 1.8% by the end of the study period in 2016. In the sub-cohort of children born at AUH, the registration was reasonably stable between 2002 and 2016, and an average of 4.4% of children were registered with phototherapy in the DNPR. A comparison of the nationwide registration to the registration in the sub-cohort from AUH suggested that neonatal phototherapy was under-reported nationwide in the DNPR. When we assumed that the actual nationwide phototherapy rate was the same as the rate observed at AUH, then we estimated that 75% of children treated with phototherapy nationwide were not reported to the DNPR. The non-compulsory policy of the Danish Health and Medicines Authority for reporting to the DNPR on treatment and care (like phototherapy)6 might explain the variation in the phototherapy registration rates among the different hospitals. People might argue that the AUH possesses one of three highly specialized units in Denmark (Neonatal Intensive Care Unit, level III); thus, a large proportion of very sick neonates are treated at AUH. However, the present analyses did not include children that were born to mothers registered in other municipalities that were treated at the AUH due to severe conditions. It remains possible that geographic variations may exist in the use of phototherapy, and it may not be reasonable to extrapolate AUH treatment rates to other hospitals.
Although phototherapy registration at AUH has not been validated, data from the AUH sub-cohort might be valuable. Among children registered with phototherapy at AUH, 97.4% had at least one bilirubin measurement in the neonatal period; in contrast, only 15.1% of children without phototherapy had bilirubin measurements. That finding suggested that the phototherapy registration from AUH in the DNPR could be highly valid. The proportion of singletons registered with phototherapy in the AUH sub-cohort was 3.3%, which was lower than the estimate (4.5%) reported from mothers in the Danish National Birth Cohort (DNBC).14 The DNBC is a cohort of 100,000 women, which provided information collected during pregnancy (at 12 and 30 weeks of gestation) and shortly after birth (at 6 and 18 months) through telephone-assisted interviews. Information on phototherapy was collected during the 6-month interview, with the following question to mothers “Has your child had phototherapy treatment for neonatal jaundice?”. Among singletons born in the cohort, 4.5% mothers reported their child had phototherapy for neonatal jaundice as shown in our previous study.14 However, phototherapy in that study included phototherapy after the neonatal period. We found that phototherapy data from the DNBC was slightly overestimated, because we confirmed that only 96% of children had actually received phototherapy after we validated the mothers’ reports by comparing them with the medical records in a pilot validation study including 100 children whose mothers reported phototherapy.14 Another study estimated that 1–2% of children born late preterm or at term were treated with phototherapy in Denmark.15 Similarly, our data from AUH showed that 1.6% children born at 35 gestational weeks and later were registered with phototherapy. In future, it would be useful to validate the phototherapy data registered in the DNPR from AUH, by comparing them to the hospital’s electronic medical records. In the US, a study showed 2.3% of children born at term received phototherapy.16
Our study showed that gestational age and birth weight were inversely associated with phototherapy registration. For example, the proportions of children registered with phototherapy from AUH were 86.1%, 78.3%, and 55.4% for children born at gestational ages <28 weeks, 28–31 weeks, and 32–34 weeks, respectively. Similar findings were reported in a study from the US; they showed that 94.3%, 92.6%, and 75.4% were treated with phototherapy among children born at gestational ages <28 weeks, 28–31 weeks, and 32–34 weeks, respectively.17 The inverse relationships between phototherapy and gestational age and birth weight were also reported in a study based on data from neonatal intensive care units (NICUs).18
Our overall estimates showed that boys were more likely to be registered with phototherapy than girls. However, the pattern was not consistent each year in this study. Data from the Danish Medical Birth Registry, including gestational age, birth weight, Apgar score, sex, and parity, were shown to be virtually complete and of very high validity.8
Our data from AUH showed that the proportion of children registered with phototherapy was correlated with many other characteristics (eg, hemolytic disease, birth asphyxia, infection, intracranial hemorrhage, etc). To some extent, the findings were consistent with findings from previous studies.13,18 For example, 62.7% of neonates diagnosed with hemolytic diseases in the neonatal period were registered with phototherapy. This was consistent with data from NICUs, which estimated that up to 85.3% of neonates with hemolytic diseases received phototherapy.18 We showed that children with infections in the neonatal period were more likely to receive phototherapy than children without infections (26.2% vs 3.6%). However, a previous study showed that fewer infants with infections needed phototherapy, compared to the proportion that needed phototherapy in the overall NICU population.18 Those authors argued that their findings might have been due to special characteristics of the NICU population.18
Our study showed that not all children with phototherapy had a diagnosis of neonatal jaundice. In our study, the neonatal jaundice diagnoses included both primary and secondary diagnoses. However, the number of children diagnosed with neonatal jaundice could be higher, if a different diagnostic approach were used.19 It is also possible that less critical diagnoses, like neonatal jaundice, could be skipped in the diagnoses for a child with other severe disorders. The study based on data from NICUs showed that only 20% of children that received phototherapy in NICUs had a jaundice-related diagnosis as the principal reason for admission.18 However, neonatal jaundice is the only indication for phototherapy in the neonatal period; therefore, it is likely that all children that received phototherapy in the neonatal period would have had neonatal jaundice. These findings indicated that, when researchers use only the diagnosis of neonatal jaundice to identify children with hyperbilirubinemia, they should be cautious about whether the records on neonatal jaundice diagnoses are enough for hyperbilirubinemia. We used the same criteria (including both the primary and secondary diagnoses) to identify neonates with other disorders. Researchers should consider differences in methods of case identification, when comparing estimates across different studies. A previous study from Norway presented neonatal characteristics associated with the use of phototherapy in all infants hospitalized in Norwegian NICUs over a year.18 However, the present study appeared to be the first to have a comprehensive scope with a population-based perspective. Nevertheless, the data on phototherapy in the DNPR did not have information on the phototherapy duration or the age at phototherapy initiation.
The use of phototherapy depends on several factors, including the use of predischarge bilirubin screening, the risk profile of the birth population, and the guidelines used for phototherapy.2 Data from Norway showed that 3.1% of neonates required predischarge phototherapy, but that study was restricted to healthy neonates born at >36 weeks gestation.20 Data from the US showed that 7.6% of neonates received phototherapy during 1995–2011.21 Predischarge bilirubin screening was introduced in the US in 2005;22 thus, when we consider only the data before the predischarge bilirubin screening program was introduced in the US, only around 3% of children received phototherapy.22 A study from Nigeria estimated the proportion of neonates born at term that met the criteria for phototherapy, according to different guidelines that were based on total serum bilirubin measured between 24 and 120 h after birth.23 Those findings showed that 2.7%, 1.1%, 0.4%, and 5.4% of neonates, respectively, required phototherapy based on the criteria from the American Academy of Pediatrics (AAP), the National Institute for Health and Clinical Excellence, UK, the World Health Organization, or an absolute threshold of ≥12 mg/dl (205 µmol/l).23 Another study showed that “clinicians provided phototherapy to only 54% of term infants with hyperbilirubinemia for whom it was recommended by the AAP”.16
Although the guidelines for phototherapy for neonatal hyperbilirubinemia in Denmark changed from the 1992 version to the 2012 version during the study period, we observed no changes in the proportion of children registered with phototherapy from AUH around 2012, when the new guidelines were applied.
The year 2018 marked the 60th year since the discovery of phototherapy for treating neonates with hyperbilirubinemia.2 In Denmark, phototherapy was applied for treating neonatal hyperbilirubinemia since the early 1970s.24 Despite a 60-year history of phototherapy use and research, important questions regarding the basic science, the practical application, and the long-term consequences of phototherapy remain to be addressed, particularly with regard to small, immature, and sick premature neonates.2 High quality data will play an important role, particularly for clinical assessments and research into the long-term consequences of phototherapy. To improve the registration of treatments and care (like phototherapy) in the DNPR, the Danish Health Authority might consider revising its policy of optional reporting to compulsory reporting on specific conditions that are associated with significant short and long-term health issues. New technologies might facilitate the automatic collection of phototherapy use. Moreover, more information could be reported, including, eg, the light source, timing, duration, number of sessions, etc.
Conclusion
Our findings suggested that phototherapy has been under-reported in the DNPR. The non-compulsory policy for reporting treatment and care in hospitals to the DNPR might explain the nationwide incomplete registration of phototherapy. A university hospital (AUH) was found to have more consistent reporting, where 4.4% of children were registered with phototherapy. We found that the registration of phototherapy was inversely associated with gestational age, birth weight, and positively associated with clinical characteristics like the low Apgar score, congenital malformations, birth asphyxia, and infections. Based on these findings, we advocate a nation-wide improvement in registering phototherapy in the DNPR to improve the quality and usefulness of the registry data. The Danish Health Authority might consider changing its policy from optional to compulsory reporting for treatments and care that might be associated with significant short and long-term health issues, like phototherapy.
Acknowledgments
This study was supported by the Independent Research Fund Denmark – project number 9039-00296B. Dr Jakob Christensen was supported by the Novo Nordisk Foundation (NNF16OC0019126 and NNF22OC0075033).
Disclosure
Dr Jakob Christensen reports grants from the Novo Nordisk Foundation, Central Denmark Region, and the Danish Epilepsy Association; personal fees from UCB and Eisai, during the conduct of the study. The authors report no other conflicts of interest related to this work.
References
1. Shapiro SM, Riordan SM. Review of bilirubin neurotoxicity II: preventing and treating acute bilirubin encephalopathy and kernicterus spectrum disorders. Pediatr Res. 2020;87(2):332–337. doi:10.1038/s41390-019-0603-5
2. Hansen TWR, Maisels MJ, Ebbesen F, et al. Sixty years of phototherapy for neonatal jaundice - from serendipitous observation to standardized treatment and rescue for millions. J Perinatol. 2020;40(2):180–193. doi:10.1038/s41372-019-0439-1
3. Grosse SD, Prosser LA, Botkin JR. Screening for neonatal hyperbilirubinemia-first do no harm? JAMA Pediatr. 2019;173(7):617–618. doi:10.1001/jamapediatrics.2019.1194
4. Schmidt M, Schmidt SA, Sandegaard JL, et al. The Danish national patient registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–490. doi:10.2147/clep.s91125
5. Schmidt M, Schmidt SAJ, Adelborg K, et al. The Danish health care system and epidemiological research: from health care contacts to database records. Clin Epidemiol. 2019;11:563–591. doi:10.2147/clep.S179083
6. Sundhedsdatastyrelsen (The Danish Health Data Authority). Fællesindhold for basisregistrering af sygehuspatienter 2019, Vejledningsdel (Common content for basic registration of hospital patients 2019, Guidance section); 2019.
7. Knudsen LB, Olsen J. The Danish medical birth registry. Dan Med Bull. 1998;45(3):320–323.
8. Bliddal M, Broe A, Pottegard A, et al. The Danish medical birth register. Eur J Epidemiol. 2018;33(1):27–36. doi:10.1007/s10654-018-0356-1
9. Schmidt M, Pedersen L, Sorensen HT. The Danish civil registration system as a tool in epidemiology. Eur J Epidemiol. 2014;29(8):541–549. doi:10.1007/s10654-014-9930-3
10. Behandlingsstandard for neonatal hyperbilirubinemia; 2012. Available from: https://paediatri.dk/images/pdf_filer/dps_vejl/neo/008neo.pdf.
11. Ebbesen F, Andersson C, Verder H, et al. Extreme hyperbilirubinemia in term and near-term infants in Denmark. Acta paediatrica. 2005;94(1):59–64. doi:10.1080/08035250410022170
12. Grann AF, Erichsen R, Nielsen AG, et al. Existing data sources for clinical epidemiology: the clinical laboratory information system (LABKA) research database at Aarhus University, Denmark. Clin Epidemiol. 2011;3(133–8). doi:10.2147/clep.s17901
13. Hansen TW. Therapeutic approaches to neonatal jaundice: an international survey. Clin Pediatr. 1996;35(6):309–316. doi:10.1177/000992289603500604
14. Maimburg RD, Olsen J, Sun Y. Neonatal hyperbilirubinemia and the risk of febrile seizures and childhood epilepsy. Epilepsy Res. 2016;124:67–72. doi:10.1016/j.eplepsyres.2016.05.004
15. Donneborg ML, Hansen BM, Petersen JP, et al. Opdatering af neonatal ukonjugeret hyperbilirubinæmi i Danmark [An update on unconjugated neonatal hyperbilirubinemia in Denmark]. Ugeskr Laeger. 2020;182(14a):V11190671. Danish.
16. Atkinson LR, Escobar GJ, Takayama JI, et al. Phototherapy use in jaundiced newborns in a large managed care organization: do clinicians adhere to the guideline? Pediatrics. 2003;111(5):e555–e561. doi:10.1542/peds.111.5.e555
17. Mukherjee D, Coffey M, Maisels MJ. Frequency and duration of phototherapy in preterm infants <35 weeks gestation. J Perinatol. 2018;38(9):1246–1251. doi:10.1038/s41372-018-0153-4
18. Mreihil K, Benth J, Stensvold HJ, et al. Phototherapy is commonly used for neonatal jaundice but greater control is needed to avoid toxicity in the most vulnerable infants. Acta paediatrica. 2018;107(4):611–619. doi:10.1111/apa.14141
19. Sun Y, Dreier JW, Wu C, et al. Importance of reporting complete procedures of identifying patients from the Danish national patient registry: the case of neonatal jaundice and epilepsy. Clin Epidemiol. 2022;14:445–452. doi:10.2147/clep.S353215
20. Tølløfsrud PA, Bjørhus E, Vårdal MH, et al. Bilirubin Levels and Need for Phototherapy During the First 4 Postnatal Days in Healthy Norwegian Neonates >36 Weeks of Gestation. Boston, MA: Pediatric Academic Societies; 2012.
21. Newman TB, Wu YW, Kuzniewicz MW, et al. Childhood seizures after phototherapy. Pediatrics. 2018;142(4). doi:10.1542/peds.2018-0648
22. Kuzniewicz MW, Escobar GJ, Newman TB. Impact of universal bilirubin screening on severe hyperbilirubinemia and phototherapy use. Pediatrics. 2009;124(4):1031–1039. doi:10.1542/peds.2008-2980
23. Olusanya BO, Emokpae AA. Use of transcutaneous bilirubin to determine the need for phototherapy in resource-limited settings. Neonatology. 2017;111(4):324–330. doi:10.1159/000452788
24. Ebbesen F. Fototerapi hos nyfødte [Phototherapy in newborn infants]. Ugeskr Laeger. 1971;133(47):2326–2331. Danish.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.