Back to Journals » International Medical Case Reports Journal » Volume 16
Neonatal COVID-19 with Atypical Lung Cystic Lesions Mimicking Congenital Pulmonary Airway Malformation – A Diagnostic Dilemma
Authors Ghazwani S
Received 22 January 2023
Accepted for publication 24 March 2023
Published 27 March 2023 Volume 2023:16 Pages 209—213
DOI https://doi.org/10.2147/IMCRJ.S405684
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas
Salman Ghazwani
Department of Surgery, Faculty of Medicine, Jazan University, Jazan, Saudi Arabia
Correspondence: Salman Ghazwani, Department of Surgery, Faculty of Medicine, Jazan University, Jazan, 45041, Saudi Arabia, Tel +96655355016, Fax +966073141288, Email [email protected]
Abstract: The COVID-19 epidemic is a major public health emergency that has affected every part of society worldwide, including neonates with different clinical presentations. It is essential to differentiate between increased incidence of complications related to this infection rather than an underlying congenital etiology. We report a rare case with atypical lung cystic lesions, diagnosed initially as congenital pulmonary airway malformation (CPAM) with management controversy but which turned out to be a COVID-19 viral pneumonia complication. Clinical tolerance and proper uses of radiological modalities are crucial to achieving better outcomes for patients. The literature is still missing reports on this topic and needs more studies to provide conclusive, evidence-based practice of this emerging neonatal viral infection. Vigilance in neonates with COVID-19 infection is highly recommended.
Keywords: SARS‐CoV‐2, pneumonia, congenital pulmonary airway malformations
Introduction
The COVID-19 epidemic is a severe public health emergency that has affected every part of society worldwide, including neonates. The virus has a significant influence on all age groups, but little is known about its clinical presentation in the neonatal population.1 Lack of knowledge on the clinical impact of COVID-19 infection in neonates is due to the recent outbreak of this emerging viral infection and few published studies to date. The literature needs more reports on this topic to provide clinicians with a better understanding of this viral tendency in neonates. We report a rare case of neonatal COVID-19 viral infection with atypical lung cystic lesions, diagnosed initially as congenital pulmonary airway malformation (CPAM) but which turned out to be a viral pneumonia complication. Congenital cystic lung lesions include a heterogeneous group of embryologically related lung malformations comprising congenital pulmonary airway malformation, pulmonary sequestrations, bronchial atresia, lobar agenesis, bronchogenic cyst and congenital lobar emphysema. The most common of these are congenital pulmonary airway malformation (CPAM) which usually diagnosed with persisting neonatal respiratory distress with significant radiological changes.2 This study aims to contribute toward a better understanding of neonatal COVID-19 presentation to achieve better outcomes for these patients and to avoid diagnosis pitfalls with congenital persisting lung lesions. Clinicians must recognize early typical and atypical presentations and complications in order to establish their associated factors, appropriate management strategies, prognoses, and the probability of long-term recovery.3
Case Presentation
This paper presents the case of a 38-week gestational age female with birth weight of 3.2 kg born to a 26-year-old primigravida mother via cesarean section for breech presentation. The baby was fine until the age of 15 days, when she developed signs of respiratory distress (tachypnea and fever and feeding refusal). She was initially admitted to the neonatal intensive care unit at a peripheral hospital at the age of 16 days for fever and respiratory distress. The provisional diagnosis was pneumonia and septicemia with left lung consolidation and right lung cysts, and it was treated with oxygen therapy and intra-venous antibiotics. On day 7 of admission, chest X-ray was performed and showed aggravating cystic lesions in the right lung, which was the reason why she was referred to our hospital at the age of 24 days and admitted to our neonatal intensive care unit for further management, with mild respiratory distress. Upon arrival, a detailed history was obtained, which revealed that some of her family members were COVID-19-positive in the previous month. A nasopharyngeal swab for SARS‐CoV‐2 RNA by polymerase-chain reaction (PCR) testing was performed, which came back positive after 24 h. On admission, the baby had tachypnea with a respiratory rate of 72 breaths/min with subcostal/intercostal retractions. On auscultation, there were absent breath sounds on the right side of the chest. On cardiovascular examination, the heart sounds were better audible on the right side. Blood investigation showed normal white blood cells count with Hb level at 13 gm/dL; Blood gas analysis revealed pH of 7.25, pO2 55, bicarbonate of 18, a base deficit of 4 and pCo2 of 55. O2 Saturation was maintained between 90% and 95% with nasal flow cannula. Chest X-ray (Figure 1) and chest tomography (Figure 2A–C) revealed left lung opacities and consolidation, as well as right cystic lesions. A chest-CT scan suggested the diagnosis of congenital pulmonary airway malformation CPAM. An echocardiogram was performed, which revealed normal findings. Blood culture was sterile. Multidisciplinary team discussion was held with the pediatric radiology, pediatric pulmonology, and neonatal intensive care teams, and the decision was made to monitor this baby closely with the indication of surgical resection if there was no improvement or clinical deterioration occurred within the same admission. The respiratory distress was treated with low-flow nasal oxygen with a 50% fraction of inspired oxygen (FiO2), along with intravenous antibiotics. After 7 days of close monitoring, clinical improvement in the neonate’s status was observed. She was taken off oxygen, signs respiratory distress disappeared, and normal feeding resumed with effortless discharge. Out-patient follow-up and reassessment was held after 8 weeks (to help lungs to recover from pneumonia and for better radiological assessment away from the inflammatory process). A control chest-CT was performed after 8 weeks and showed complete resolution of these cystic lesions, with only a picture of post-pneumonia healing changes (Figure 3A and B).
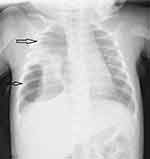 |
Figure 1 (Chest X-Ray) White arrows in right lung shows cystic lesions. |
Discussion
Our study showed that conservative management and clinical tolerance was successful in this case. Close follow up helped us to avoid aggressive and unnecessary surgical resection of lung lobes. Multidisciplinary decision was helpful in the management. Chest CT-Scan was modality of choice upon aggravation of the cystic lesions on serial chest X-Ray and persisting respiratory distress for better anatomical description of this lesion and its extension as well as to detect any systemic blood supply in case of pulmonary sequestration. There was limited data in literature about severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in neonate as it’s an emerging pathogen initially identified in December 2019.4 The epidemiology, clinical presentation, and prognosis of SARS‐CoV‐2 in neonates is still under-reported. A recent study in literature described the vertical transmission of COVID-19 from mother to newborn as a congenital viral infection which reported by Pandit et al.5 Relation between cystic lung disease in neonates and Covid-19 viral infection complications still not understood. Cystic lung disease of lung is divided into congenital and acquired lesions. Congenital form includes several malformations with distinct anatomical and histological features with significant overlapping suggesting a common pathologic mechanism for their occurrence. The disease includes (congenital pulmonary adenomatoid malformations CPAM, pulmonary sequestrations PS, congenital lobar emphysema CLE, and peripheral bronchogenic cysts BC as described by Shanti et al6 we reported our results of managing a rare case of a neonate with COVID-19 viral pneumonia and respiratory distress confirmed by reverse transcription polymerase chain reaction (RT-PCR). As diverse clinical presentations in various age groups are being described, it thus becomes difficult to differentiate between the increased incidence of complications related to underlying cause or COVID-19-related illnesses.7 The diagnostic dilemma in this case was to differentiate the cause for these multiple right lung cystic lesions between congenital lung malformations as an underlying cause of or as a complication of COVID-19 viral pneumonia. Making a management decision was controversial: emergency surgery via (thoracotomy or thoracoscopy) if there was no improvement versus conservative surgery if conditions improved, weighing the benefits and the risk of surgical complications in this acute stage.8 Observation and close follow-up and tolerance was a key stone in the management of this case. Upon clinical improvement of the patient’s status, the decision was made to discharge her with a close follow-up and to repeat chest CT after 8 weeks (for follow-up and as pre-operative assessment if surgery will be indicated for any form of congenital cystic disease of the lung). Out-patient follow-up showed dramatic clinical and radiological improvement, with complete resolution of these lesions. Close monitoring and clinical tolerance for this patient avoided unnecessary lung lobe resection. Chest-CT has the upper hand on chest X-ray to diagnose and follow-up our case. Furthermore, management should be focused on the clinical status rather than radiological findings. Proper timing of clinical and radiological evaluation was crucial. COVID-19 infection in neonates still under-reported but seems to have a benign course. As diverse clinical presentations in various age groups are being described, it becomes difficult to differentiate the increased incidence of complications related to an underlying pathology from COVID-19-related illness. A multidisciplinary team approach is helpful in the management of neonatal COVID-19 viral pneumonia for better decision making and outcomes and to avoid unnecessary, high-risk surgery without a clear strategy. Obstetricians should be aware of prenatal follow-up of infected pregnant and possible associated perinatal complications for better planning with neonatologist for save delivery.9 This report might help neonatologists, pediatric surgeons, and pediatric pulmonologists to understand the clinical presentation of neonatal COVID-19 and best practices for better management. Limitation of this report was lack of similar cases in literature to be reviewed. The literature still needs more complementary reports to achieve protocoled management lines to address this emerging viral infection in neonates.
Conclusion
In conclusion, the management of neonatal COVID-19 is still challenging, with many unanswered questions. A high index of suspicion for atypical neonatal lung lesions is crucial. Clinical tol-erance is recommended if the patient’s clinical status allows it. The literature needs more reports focusing on neonatal COVID-19 infection to provide clinicians with better understanding and protocolling management lines to address these ongoing concerns in the neonatal population.
Data Sharing Statement
The data presented in this study are available on request from the corresponding author.
Informed Consent Statement
Written informed consent has been obtained from the patient’s parents to publish this paper.
Institutional Review Board Statement
The study was approved by the Jazan Health Ethics Committee (approval number 22115 dated 6 November 2022).
Funding
This research received no external funding.
Disclosure
The author declares no conflicts of interest in this work.
References
1. Dumpa V, Kamity R, Vinci AN, Noyola E, Noor A. Neonatal Coronavirus 2019 (COVID-19) infection: a case report and review of literature. Cureus. 2020;12:e8165. doi:10.7759/cureus.8165
2. Disu EA, Kehinde OA, Anga AL, et al. Congenital pulmonary airway malformation: a case report of a rare cause of neonatal respiratory distress and review of the literature. Niger J Clin Pract. 2019;22(11):1621–1625. doi:10.4103/njcp.njcp_20_19
3. Muñoz-Palacio BJ, Syro D, Pinzón MA, Ramirez B, Betancur JF. Pulmonary cystic disease associated with cOVID 19 pneumonia: an emerging atypical manifestation. Cureus. 2021;13(11):e19352. doi:10.7759/cureus.19352
4. Pinzón MA, Ortiz S, Holguín H, et al. Dexamethasone vs methylprednisolone high dose for COVID-19 pneumonia. PLoS One. 2021;16:e0252057. doi:10.1371/journal.pone.0252057
5. Pandit T, Pandit R, Bhattar K. Possible COVID-19 maternal-to-neonate vertical transmission in a case of early neonatal infection. Cureus. 2022;14(7):e27141. PMID: 36017288; PMCID: PMC9392985. doi:10.7759/cureus.27141
6. Shanti C, Klein M. Cystic lung disease. In:
7. Kamity R, Nayak A, Dumpa V. Pneumothorax in neonates born to COVID-19-positive mothers: fact or fortuity? Am J Perinatol Rep. 2021;11:e49–e53. doi:10.1055/s-0041-1726020
8. She WH, Chung HY, Lan LCL, Wong KK, Saing H, Tam PKH. Management of choledochal cyst: 30 years of experience and results in a single center. J Pediatr Surg. 2009;44:2307–2311. doi:10.1016/j.jpedsurg.2009.07.071
9. Getahun D, Peltier MR, Lurvey LD, et al. Association between SARS-CoV-2 infection and adverse perinatal outcomes in a large health maintenance organization. Am J Perinatol. 2022. PMID: 35738286. doi:10.1055/s-0042-1749666
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


