Back to Journals » Patient Preference and Adherence » Volume 9
Needs of family caregivers of stroke patients: a longitudinal study of caregivers’ perspectives
Authors Tsai P, Yip P, Tai JJ, Lou M
Received 18 November 2014
Accepted for publication 17 January 2015
Published 18 March 2015 Volume 2015:9 Pages 449—457
DOI https://doi.org/10.2147/PPA.S77713
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Pei-Chun Tsai,1 Ping-Keung Yip,2 John Jen Tai,3 Meei-Fang Lou1
1School of Nursing, College of Medicine, National Taiwan University, Taipei, 2School of Medicine, 3Department of Statistics and Information Science, College of Management, Fu-Jen Catholic University, New Taipei City, Taiwan
Background: After a stroke, patients often suffer from varying degrees of disability that require acute inpatient treatment and extended care at home. Therefore, the caregivers assume multiple responsibilities that can result in stress, particularly when their own needs are inadequately addressed during the patient’s recovery.
Objectives: This study aimed to explore the changing needs of family caregivers of stroke patients and factors related to the needs in four stages, before the transfer from intensive care unit to neurological unit, before discharge, 2 weeks post-hospitalization, and 3 months post-hospitalization.
Methods: The design of this study was based on longitudinal research, and the participants were family caregivers of stroke patients. Sixty family caregivers were recruited in this study. Data were collected at four time points by questionnaire.
Results: We found that the total number of needs of family caregivers decreased as the illness duration increased and that needs differed significantly between the four time points (P<0.01). Although the needs were different in each stage, health information, professional support, and community networks were the leading need domains in all four stages. The major factors affecting the care needs of family caregivers were the National Institutes of Health Stroke Scale scores of patients on admission, length of hospital stay, and physical dependence of patients.
Conclusion: Family caregivers expected to obtain assistance and related care information from professionals during the course of the disease. Assessing the needs of family caregivers is important for health care workers in understanding problems from the caregivers’ perspectives. Relevant information and counseling should be provided to family caregivers to help them access support when needed.
Keywords: chronic illness, family needs, transitional care
Background
Stroke is the third leading cause of death due to cerebrovascular diseases in Taiwan1 and is one of the main causes of chronic disability. Strokes tend to present abruptly and can critically affect individuals and their caregivers. After a stroke, patients often suffer from varying degrees of disability that require acute inpatient treatment and extended care at home. Therefore, the caregivers assume multiple responsibilities that can result in stress, particularly when their own needs are inadequately addressed during the patient’s recovery.2,3
Family caregivers have different needs at different stages of the patient’s illness. Cameron and Gignac summarized five different stages of caregiver support needs across the care continuum as follows: event/diagnosis, stabilization, preparation, implementation, and adaptation.4 Of these five stages, the first two occur during acute care, the third occurs during acute care or inpatient rehabilitation, and the final two stages occur in the community. In the acute stage, the caregivers require information about disease progression and treatment. They must obtain prompt information regarding changes in the patient’s condition. The caregivers expect health care workers to honestly answer questions about the patient’s condition and potential changes.5–7 If such information is not provided to family caregivers in the acute stage, it can result in uncertainty and anxiety.4
During the transition stage at discharge, family caregivers must face new problems related to the disease and its symptoms. These include the safety and the emotional response of the patients, the equipment required in their homes, the level of care needed, medication management, the prevention of stroke recurrence, and the availability of community resources.8–12 To independently care for the patients at home, the caregivers require appropriate knowledge, skills, social resources, and emotional support. Anxiety and worry may begin to increase if information on the impact of the stroke is not provided.4
Providing care during the first few months after a stroke is stressful, and it is important to provide appropriate information and support.13 Smith et al explored the care experience of primary caregivers 1 year after a stroke and found that the caregivers frequently lacked the knowledge and the skills required to provide home care after the patients were discharged; in addition, they had to obtain the information and the assistance on their own.14 The caregivers must adapt to the changes caused by the patient’s illness. The studies of the home care needs of stroke patients and family caregivers have uncovered unmet needs. For example, Zwygart-Stauffacher et al found that primary caregivers paid more attention to information about the disease and its progression,15 while Chiou et al ranked the needs of the caregivers by care needs for the patient and personal needs for themselves.16 When caring for the patients, the caregivers required financial assistance, instrumental services, information to provide skilled care, and help applying for social welfare services; however, they also had personal needs, including social, health promotion, maintenance, and emotional needs, related to the caring process.16 Professional care during this stage can vary among patients.4
Although the literature suggests that family caregivers have different needs at different stages of the patient’s illness,4–16 to date, most studies have only focused on the needs of family caregivers during specific periods. They have not explored the changing needs of family caregivers from admission to discharge. Therefore, this study aimed to explore the changing needs of family caregivers of stroke patients from admission to the intensive care unit (ICU) to 3 months post-hospitalization. Specifically, we expected these results to provide the health care workers with an understanding of the needs of family caregivers at the different stages of care. This should help to improve the quality of care provided to the patients and their families by ensuring the provision of health education and information to family caregivers at the appropriate stages.
Methods
Participants and setting
We recruited consecutive family caregivers of the patients admitted to a stroke ICU in Northern Taiwan during 2009–2010. The participants were required to be the primary caregiver. The inclusion criteria were: 1) family caregivers of patients with stroke diagnosed by a physician; 2) family caregivers who were over 18 years old and able to communicate in Mandarin and Taiwanese; and 3) family caregivers who spent most of the time in caring for the patient. If family members take turns in caring for patients, then the family decision maker was the one to provide information. In Taiwan, stroke patients were admitted to the stroke ICU for acute care. Then, patients were transferred to the neurological unit for further management of medical conditions and rehabilitation. After discharged from hospital, most patients had to follow-up at the outpatient clinics of the study hospital. Some patients chose to follow-up at other clinics because of location or being self-referred.
Design
This was a longitudinal study. Data were collected at four time points, which were before transferring out of the ICU, before discharge, 2 weeks post-hospitalization, and 3 months post-hospitalization.
Questionnaire design
Our questionnaire consisted of the following two parts:
Patient and family caregiver characteristics: Patient information included sociodemographic characteristics, such as age, sex, and disease-related information, such as length of hospital stay, number of diagnosed chronic diseases, severity of stroke at admission (National Institutes of Health Stroke Scale; NIHSS), and physical dependence (Barthel Index). NIHSS was assessed by a physician at admission. The higher the NIHSS score, the more the severity of stroke.17 Barthel Index was assessed by the researcher at discharge, 2 weeks post-hospitalization, and 3 months post-hospitalization. The higher the score, the more the physical independence of the patient. Family caregivers’ demographic information included age, sex, education, occupation, and religion.
Family needs of stroke patient questionnaire: This questionnaire was based on the needs questionnaire for family caregivers by Kreutzer and Marwitz and translated by Chung.18 Items were added based on the previous research findings and researcher’s clinical experience.19,20 A total of 43 items of needs were listed as the instrument in this study.
The importance, relevance, and semantic clarity of the content of each item were evaluated by nine experts in this field using a four-point Likert scale. The content validity indexes were 0.99, 0.98 and 0.93, respectively. Factor analysis showed that there were six domains in the scale, which were needs of health information (13 items), needs of instrumental support (nine items), needs of emotional support (eight items), needs of involvement with patient care (five items), needs of professional support (four items), and needs of community networks (four items). For each question, family caregivers checked the needed item. The total number of needs ranged from 0 to 43. A higher number indicated more needs. The overall questionnaire internal consistency reliability (KR-20) is 0.89–0.93 for the four stages.
Data collection
The aims, methods, and time commitment required at four time points were explained to the potential participants who met the inclusion criteria to obtain informed consent. Signed informed consent was provided before starting the questionnaire data collection. The patients received a brief explanation of the study from the investigator once their primary caregiver had consented to participate and we obtained their consent to use their medical data. If the patient had language/cognitive impairments, the caregiver provided consent on their behalf.
At the first and second time points, the location of data collection was in the hospital. At the third and fourth time points, timing could include during patient’s return visits to the outpatient clinic or during home visits. The questionnaire was self-administered by caregivers. For the one caregiver who was illiterate, each question was asked by the researcher and the answers of the participant were transcribed to the questionnaire by the researcher. Patient characteristics and disease-related information were obtained from medical records.
Statistical analysis
This study used statistical software package SPSS for Windows 16.0 (Chicago, IL, USA) to conduct statistical analysis. Descriptive statistics and inferential statistics such as repeated measures analysis of variance and Pearson product–moment correlation were used to explore the changes and related factors of the care needs of family caregivers in the four stages.
Ethical considerations
This study was reviewed and approved by the Research Ethics Committee of National Taiwan University Hospital where the study took place. Written consent was obtained from the participants. Participants were explicitly informed that the data found in this study would be confidential, would not affect patient’s treatment, and would be used only for academic research and no other purpose. During the course of the study, the questionnaire could be stopped at any time if the participants were uncomfortable or unwilling.
Results
Patient and family caregiver characteristics
Sixty-three stroke patients and their primary caregivers met the inclusion criteria during the study period. Three caregivers refused to participate because patients were readmitted to ICU and died due to complicated physical conditions. Sixty stroke patients and their primary caregivers completed the four assessments for analysis in this study. There were 39 male patients and 21 female patients with a mean age of 64 years (SD=15.58). The average years of education was 9 years (SD=6.0). There were 41 (68.3%) ischemic stroke patients. A total of 44 (73.3%) patients had first-time stroke and the remaining 16 had a second stroke or more. On average, patients had two chronic diseases besides stroke. The NIHSS score when admitted ranged from 3 to 26 with a mean of 14.5 (SD=5.86). For physical dependence, the mean scores of the Barthel Index for the three stages of before discharge, 2 weeks post-hospitalization, and 3 months post-hospitalization were 52.00 (SD=30.23), 53.42 (SD=30.71), and 54.92 (SD=31.12), respectively.
There were 60 family caregivers of the stroke patients, with 25 males and 35 females. The mean age was 44 years (SD=13.08). The mean years of education was 13.7 years (SD=4.25). There were 48 (80%) caregivers who lived with the patients before hospitalization. Most of the caregivers were sons (n=19), followed by daughters or spouses, with 16 in each group (Table 1).
  | Table 1 Caregivers’ demographic information (n=60) |
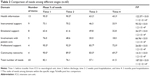
Number of family caregiver needs in the four stages after stroke
The means of overall needs were 35.30 (SD=5.64), 32.72 (SD=6.88), 24.55 (SD=9.04), and 17.85 (SD=9.40) for time points 1, 2, 3, and 4, respectively. The total numbers of needs of family caregivers in the four stages were analyzed by repeated measures analysis of variance. There were significant differences in the total number (F=187.03, P<0.01) of needs and in each subdomain in the various stages. The results showed that the total number of needs of family caregivers decreased as the illness duration increased. We used the total number of needs divided by the number of domain items to represent the mean percentage of needs for each domain. In the four stages, the items most frequently needed were in the health information and professional support domains at times 1 and 2, and in the community networks and professional support domains at times 3 and 4 (Table 2).
The greatest needs (Table 3) identified before transfer from the ICU to the neurological unit (time 1) were for the following items: respect the patient when performing education, treatment or rehabilitation; providing information on disease progress; to have my question answered honestly; information on medication and treatment; information on the patient’s physical problems; and rehabilitation progress. All family caregivers had those needs in the health information domain.
The greatest needs before discharge (time 2) were for the following items: respect the patient when performing education, treatment or rehabilitation; information on medication and treatment; information on the patient’s physical problems in the health information domain; and being informed of how to handle the medical emergencies of the patients in the professional support domain. Most (98%) family caregivers had those needs.
At 2 weeks post-hospitalization (time 3), the greatest needs were for information on how to handle the medical emergencies and what to do when the patient became upset or acted strange in the professional support domain; information about physical problems and medication and treatment in the health information domain; and conveying advice with the help of professionals in the community networks domain. Around 88%–95% of family caregivers had those needs.
At 3 months post-hospitalization (time 4), the greatest needs were for information on how to handle the medical emergencies and what to do when the patient became upset or acted strange in the professional support domain; information about physical problems and medication and treatment in the health information domain; and conveying advice with the help of professionals and support from family and friends in the community networks domain. About 75%–93% of family caregivers had those needs (Table 3).
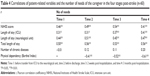
Related factors of care needs of family caregivers
The patient’s sex, religion, number of stroke episodes, number of diagnosed chronic diseases, and care needs of family caregivers in the four stages showed no significant correlations. The NIHSS score at admission and length of stay had significant positive correlations with caregiver needs in the four stages. It indicated that in patients with a higher NIHSS score at admission and longer length of stay, the family caregivers had more care needs. Physical dependence (Barthel Index) had significant negative correlations with caregivers’ needs. It indicated that the higher the physical dependence of patients, the more the care needs of family caregivers (Table 4). The caregiver’s sex, living status, occupation, education level, and relationship with patients had no significant correlations with the care needs of the four stages.
Discussions
We found that the total number of needs of family caregivers decreased as the illness duration increased and that the individual needs differed between the four time points. Although the needs were different at each assessment point, the greatest needs were at times in the domains of health information, professional support, and community networks. The major factors affecting the care needs of family caregivers were the NIHSS scores of the patients on admission, the length of hospital stay, and the physical dependence of the patients.
Changes in the overall care needs of family caregivers
We found that family caregivers had the greatest care needs during the ICU stage. The mean percentage of needs by the total need items were 82.1%, 76.1%, 57.1%, and 41.5% for times 1, 2, 3, and 4, respectively. The needs of family caregivers were significantly lower before discharge than before transferring out of the ICU and were lower after discharge than before discharge (ie, at times 3 and 4 versus 1 and 2). These findings might have occurred because the health care workers in the study hospital were able to provide health education, stroke-related medical information, and prognostic details to the family during hospitalization. Additionally, the longer the family caregivers took care of a patient, the more familiar they may have become with the care needs. Regular return visits and rehabilitation may also have provided the caregivers with greater insight into the progression of the disease and the patient’s rehabilitation, which may have resulted in a gradual decrease in their needs.
Consistent with previous reports,5,9–11,16 we found that health information, professional support, and community networks were the leading need domains of the caregivers regardless of the time of assessment. However, the caregivers did require different information and support at the different stages. For example, the items most needed by family caregivers before transfer out of the ICU were in the health information domain. This result was similar to that reported by Chen et al on the needs of family caregivers of the patients admitted to the ICU over 24 hours when the patients were clinically unstable.5 In the pre-discharge stage, the caregivers needed health-related information about the patient’s condition, treatment, and rehabilitation, which is consistent with the previous reports.9–12,21 Communication between the health care workers and the caregivers during hospitalization, specifically when discussing the needs of the caregivers and providing information, was essential before discharge.10 Indeed, the provision of information during the first two stages might be a critical time for health care workers to provide information to the caregivers. Thus, as the cost of health care increases and hospital stays become shorter, the health care workers must perform adequate need assessments of family caregivers for effective discharge transition. If nurses could anticipate the care problems encountered by family caregivers after discharge, those needs could be addressed during hospitalization, leading to an improved quality of care at home.11,22,23
Changes in the specific care needs of family caregivers
Consistent with the previous reports,5–7 family caregivers expected to obtain assistance and care-related information from the professionals. However, this information changed with time. For example, in the acute stage, the caregivers required information and communication about disease progression and treatment requiring prompt information about changes in the patient’s condition. The caregivers expect the health care workers to answer questions about the patient’s condition and the potential changes honestly. Nurses took full responsibility for the patient’s care in the ICU during their stay, and by providing information about the disease soon after admission, they facilitated better understanding of the medical treatment and care received by the patients, which may have relieved anxiety and uncertainty among family caregivers. Providing home care for a stroke patient is a stressful experience, and family caregivers will face new problems related to the disease and its symptoms after discharge.7,9–12 In order to care for the patients, independently at home, the caregivers require specific knowledge, skills, social resources, and emotional support.13 If related care information and emotional support are provided in a timely manner, the well-being of family caregivers during discharge transition could be significantly improved.
Even though the needs reduced over time, the number at 3 months post-stroke remained high. The handling of cognitive, behavioral, and emotional changes has been reported as needs of the caregivers of stroke patients after the hospitalization.8,11 We also found that family caregivers needed information about what to do when the patient became upset or started to act strange. These needs are different from those of family caregivers in conditions other than stroke or brain injury.24 Indeed, stroke patients can exhibit emotional or behavioral problems after discharge that require long-term care and could lead to dramatic life changes and stress for the caregiver. If information related to behavioral or emotional management is provided early, it could improve the quality of home care and reduce family caregiver stress. It is important in this stage to be providing strategies to help the caregivers manage their competing roles and health needs, including information about respite care, future care options, community activities, and support groups.4
In the current study, professional support and community networks were the most needed domains during the post-hospitalization stage. Given that stroke is a chronic disease with long-term care needs and with lengthy rehabilitation and disease control, it is unsurprising that the needs in these domains were the greatest. During admission, the health care workers could routinely provide information about social welfare and financial assistance and resolve many problems of the post-hospitalization stage before discharge.25,26
Factors related to the care needs of family caregivers
This study found that the NIHSS scores on admission and the needs of family caregivers correlated significantly with the family caregivers of patients with more severe strokes having greater care needs. Studies on the prognosis of stroke patients have found that the NIHSS score at admission was an indicator of disease progression and prognosis.27,28 In these studies, higher scores indicated poorer prognoses, and the researchers considered that a patient’s NIHSS score was a very good predictor of physical function in stroke patients. Furthermore, the NIHSS is widely used for determining prognosis.29 This study demonstrated that the NIHSS score and needs of family caregivers correlated significantly, indicating that the NIHSS could be of help in the nursing care of stroke patients and caregivers. The study suggests that nurses should understand the NIHSS and apply it during clinical assessments. Our study showed that the length of stay, physical dependence, and the care need scores of family caregivers had moderately positive correlations, which suggested greater needs in these domains. The difference may be that the severity of stroke is associated with longer stays in hospital and family caregivers having more care needs due to the more complicated conditions.
Limitations
This study has several limitations. First, we used a structured questionnaire for data collection, so we could not explore the care needs of family caregivers in depth. Second, the scale for family caregiver needs was developed specifically for this study. The reduction in reported needs might be due to bias in the questionnaire, favoring assessment of hospital care needs, and failing to identify later care needs. Although its content validity was tested, further validation of the instrument is required to clarify the most appropriate care need items. Third, we recruited a consecutive sample of family caregivers who cared for stroke patients from admission to home. It is possible that the patients with severe stroke were not represented because family members might have decided to discharge the patient to an institution or the patient might have died during hospitalization. Thus, the care needs of family caregivers in these circumstances might be underestimated. Fourth, the number of participants was limited, which means that we may lack the power to assess the caregiver needs. Finally, we only collected data at one site, which may limit the generalizability of our results.
Conclusion
We found that the total number of needs of family caregivers decreased as the illness duration increased. Health information, professional support, and community networks were the leading need domains at all four transition time points. Furthermore, family caregivers expected to obtain continued assistance and related care information from professionals during the course of the disease. The first two stages during hospitalization might be a critical time for the health care workers to perform need assessments and provide appropriate information to the caregivers. Need assessments are important to enable the health care workers to understand the problems from the caregivers’ perspectives. Relevant information and counseling should be provided to family caregivers to help them access support as needed.
Acknowledgments
The authors are grateful to the 60 family caregivers and patients in the neurological units of National Taiwan University Hospital.
Authors’ contributions
PCT conceived the study, performed data collection and statistical analysis, and helped to draft the manuscript. PKY participated in the design of the study and helped to draft the manuscript. JJT participated in statistical analysis and helped to draft the manuscript. MFL conceived and participated in the design of the study, participated in statistical analysis, and drafted the manuscript. All authors approved the final manuscript.
Disclosure
No conflicts of interest have been declared by the authors. This research received no specific grant from any funding agency in the public, commercial, or non-for-profit sectors.
References
Ministry of Health and Welfare, Executive Yuan, Taiwan, 2013. 2012 Statistics of Causes of Death; 2013. Available from: http://www.mohw.gov.tw/cht/DOS/Statistic.aspx?f_list_no=312&fod_list_no=2747. Accessed July 8, 2013. | ||
Brandon IL. Easing the burden on family caregivers. Nursing. 2013;43(8):36–42. | ||
King RB, Ainsworth CR, Ronen M, Hartke RJ. Stroke caregivers: pressing problems reported during the first months of caregiving. J Neurosci Nurs. 2010;42(6):302–311. | ||
Cameron JI, Gignac MA. “Timing it right”: a conceptual framework for addressing the support needs of family caregivers to stroke survivors from the hospital to the home. Patient Educ Couns. 2008;70(3):305–314. | ||
Chen SM, Du YH, Wu JC. A study of psychological needs and its influential factors among families in intensive care unit. Kaohsiung J Nurs. 2004;21(1):1–16. [Chinese]. | ||
Cullinane JP, Plowright CI. Patients’ and relatives’ experiences of transfer from intensive care unit to wards. Nurs Crit Care. 2013;18(6):289–296. | ||
Maclsaac L, Harrison MB, Buchanan D, Hopman WM. Supportive care needs after an acute stroke: a descriptive enquiry of caregivers’ perspective. J Neurosci Nurs. 2011;43(3):132–140. | ||
Grant JS, Glandon GL, Elliott TR, Giger JN, Weaver M. Caregiving problems and feelings experienced by family caregivers of stroke survivors the first month after discharge. Int J Rehabil Res. 2004;27(2):105–111. | ||
Hayashi Y, Hai HH, Tai NA. Assessment of the needs of caregivers of stroke patients at state-owned acute-care hospitals in Southern Vietnam, 2011. Prev Chronic Dis. 2013;10:130023. | ||
Mackenizie A, Perry L, Lockhart E, Cottee M, Cloud G, Mann H. Family carers of stroke survivors: needs, knowledge, satisfaction and competence in caring. Disabil Rehabil. 2007;29(2):111–121. | ||
Mak AK, Mackenizie A, Lui MH. Changing needs of Chinese family caregivers of survivors. J Clin Nurs. 2007;16(5):971–979. | ||
Plank A, Mazzoni V, Cavada L. Becoming a caregiver: new family carers’ experience during the transition from hospital to home. J Clin Nurs. 2012;21:2072–2082. | ||
Cecil R, Thompson K, Parahoo K, McCaughan E. Towards an understanding of the lives of families affected by stroke: a qualitative study of home carers. J Adv Nurs. 2013;69(8):1761–1770. | ||
Smith ML, Lawrence M, Kerr SM, Langhorne P, Lees KR. Informal carer’s experience of caring for stroke survivors. J Adv Nurs. 2004;46(3):235–244. | ||
Zwygart-Stauffacher M, Lindquist R, Savik K. Development of health care delivery systems that are sensitive to the needs of stroke survivors and their caregivers. Nurs Adm Q. 2000;24(3):33–42. | ||
Chiou CJ, Hsu SM, Wu SZ. Needs of home-care primary caregivers. J Health Sci. 2003;5(1):12–25. | ||
Jeng GY, Chiu SC, Sun TK, et al. Clinical application of the national institute of health stroke scale by neurological care professionals in Taiwan. J Evid-Based Nurs. 2006;2(3):189–200. [Chinese]. | ||
Chung KC. Perceptions of needs of home health care by family caregivers of patients with traumatic brain injury and nurses, Thesis, Taipei, Taiwan: National Defense University, 2005. [Chinese]. | ||
Chiou CJ, Chen WT, Chen IP. The support system for family caregivers of chronically ill patients. J Long Term Care. 2005;9(3):245–262. [Chinese]. | ||
Liou CA, Su WL. A study on the needs and satisfaction of the in-patients’ families at a medical center. J Nurs. 1998;45(2):47–59. [Chinese]. | ||
Yonaty SA, Kitchie S. The educational needs of newly diagnosed stoke patients. J Neurosci Nurs. 2012;44(5):E1–E9. | ||
Kalra L, Evans A, Perez I, et al. Training carers of stroke patients: randomized controlled trial. British Med J. 2004;328(7448):1099. | ||
Shyu YI, Chen MC, Chen ST, Wang HP, Shao JH. A family caregiver-oriented discharge planning program for older stroke patients and their family caregivers. J Clin Nurs. 2008;17:2497–2508. | ||
Lefebvre H, Lvert MJ. The needs experienced by individuals and their loved ones following a traumatic brain injury. J Trauma Nurs. 2012;19(4):197–207. | ||
Mant J, Winner S, Roche J, Wade DT. Family support for stroke: one year follow up of a randomized controlled trial. J Neurol Neurosurg Psychiatry. 2005;76:1006–1008. | ||
Pierce L, Steiner V. Usage and design evaluation by family caregivers of a stroke intervention web site. J Neurosci Nurs. 2013;45(5):254–261. | ||
Liu X, Lu Y, Wang B, Zhao G, Yan Y, Xu D. Prediction of functional outcome of ischemic stroke patients in northwest China. Clin Neurol Neurosurg. 2007;109(7):571–577. | ||
Ahmed R, Zuben BF, Afsar S. Stroke scale score and early prediction of outcome after stroke. J Coll Physicians Surg Pak. 2004;14(5):267–269. | ||
Nedeltchev K, Renz N, Karamesbev A, Haefeli T, Brekenfeld C, Meier N. Predictors of early mortality after acute ischaemic stroke. Swiss Med Wkly. 2010;140(17):254–259. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.