Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 16
Needs Assessment and Identification of the Multifaceted COPD Care Bundle in the Emergency Department of a Tertiary Hospital in Nepal
Authors Shrestha R , Shrestha AP , Sonnenberg T , Mistry J, Shrestha R, MacKinney T
Received 8 October 2020
Accepted for publication 30 December 2020
Published 22 January 2021 Volume 2021:16 Pages 125—136
DOI https://doi.org/10.2147/COPD.S285744
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Roshana Shrestha,1 Anmol Purna Shrestha,1 Taylor Sonnenberg,2 Janki Mistry,3 Rajeev Shrestha,4,5 Theodore MacKinney3
1Department of General Practice and Emergency Medicine, Kathmandu University School of Medical Sciences, Dhulikhel, Kavrepalanchok, Nepal; 2Department of Emergency Medicine, Medical College of Wisconsin, Milwaukee, WI, USA; 3Department of Medicine, Medical College of Wisconsin, Milwaukee, WI, USA; 4Department of Pharmacology, Kathmandu University School of Medical Sciences, Dhulikhel, Kavrepalanchok, Nepal; 5Nepal Pharmacovigilance Unit/Research & Development Division, Dhulikhel Hospital, Kathmandu University Hospital, Dhulikhel, Kavrepalanchok, Nepal
Correspondence: Roshana Shrestha
Department of General Practice and Emergency Medicine, Kathmandu University School of Medical Sciences, Dhulikhel, Nepal
Tel + 977 9841558332
Email [email protected]
Purpose: Acute care of patients with exacerbation of chronic obstructive pulmonary disease (AECOPD) in the emergency department (ED) is crucial, however not studied extensively in Nepal. The purpose of this study is to identify the opportunities for succinct measures to optimize the AECOPD care in ED with a multifaceted bundle care approach in a resource-limited setting.
Methods: We conducted a prospective cross-sectional observational study as an initial baseline stage of the quality improvement project. Demographic data, clinical characteristics, the current diagnosis and treatment performances of AECOPD were recorded. The primary outcome measures were 30-day ED revisit and near-fatal events which were compared with other variables and performances with binary and logistic regression. The multidisciplinary team performed the root cause and Pareto analysis to identify the potential gaps in the AECOPD care.
Results: The AECOPD performance measures were suboptimal. Written AECOPD emergency management clinical guidelines and advice regarding pulmonary rehabilitation were absent. Among the 249 AECOPD encounters, bilevel positive-airway pressure ventilation was started in 6.4%. At discharge, 11.8% and 39.7% were given oral steroids and antibiotics respectively; 2.2% were advised vaccination. Near-fatal events and 30-day revisit occurred in 19% and 38.2% of the encounters respectively. Those who required domiciliary oxygen had significantly higher 30-day revisits (OR=2.5; 95% CI=1.43– 4.4; P value =0.001) as did those who were previously admitted (OR=1.98; 95% CI 1.11– 3.59; P value =0.022). Those who had a 30-day revisit had increased near-fatal events (OR=2.86; 95% CI=1.362– 6.18; P value =0.006). The opportunities for improving the ED care were identified and feasible interventions and their indicators are summarized for future implementation.
Conclusion: The current COPD performance measures were suboptimal with high 30-day revisit and near-fatal outcomes. We suggest the urgent implementation of the enlisted feasible bundles-care involving multifaceted team and protocol-based management plans for AECOPD in a busy resource-limited ED.
Keywords: clinical practice guideline, near-fatal outcome, performance measure, quality improvement, resource-limited setting, root cause analysis
Introduction
Chronic obstructive pulmonary disease (COPD) is a common non-communicable disease (NCD) and the second leading cause of death worldwide.1 A prevalence of 251 million cases of COPD was reported in 2016 with 3.17 million deaths estimated globally by the disease, more than 90% of which occur in low and middle income countries (LMIC).2 The worldwide prevalence is about 10% as reported in a recent systematic review.3 In Nepal, the prevalence of COPD is 23–43%.4–6 COPD is the third leading cause of years lived with disability (YLD) in Nepal, the second most common cause of death after ischemic heart disease (IHD), and the fourth most common cause of premature death.7
Acute exacerbation of COPD (AECOPD) is defined as an acute worsening of respiratory symptoms precipitated by several factors that results in need of emergency treatment and additional therapy.8,9 AECOPD is a leading cause of morbidity and mortality in the South Asian context.10 A study done in India found dyspnea as the third most common Emergency Department (ED) presentation.11 Patients frequently visit the ED to receive urgent care for acute onset dyspnea, and the major cause of which was COPD in two tertiary level EDs in Nepal.12,13 There is little to no data about the prevalence of COPD in the ED, the care of patients including the best way to manage them in the ED in a Nepali context, or the outcomes of COPD care. Therefore, there is a great opportunity to understand the baseline ED service provision, and to identify opportunities to improve the care of this very common condition.
Frequent AECOPD is associated with higher mortality, poor quality of life, accelerated decline in lung function and future adverse events.14–17 Frequent exacerbations have a devastating effect on a patient’s quality of life, rapid disease progression and increased healthcare cost.18 Patient readmissions are associated with a greater risk of mortality.19 Therefore, the goal for treatment of AECOPD is to minimize the negative impact of the current exacerbation and to reduce COPD readmissions with effective interventions. A number of individual interventions or bundles of interventions have been shown to reduce the readmission rate and mortality.20–22 Interventions to prevent ED revisits after AECOPD are urgently needed to improve outcomes and reduce costs. A small number of quality improvement (QI) studies have been done in Nepal23,24 in other domains, including primary care and community settings,25,26 but there have been virtually no studies based in EDs.
The goal of this project is to evaluate the gaps in care of AECOPD patients in the ED of Dhulikhel Hospital-Kathmandu University Hospital (DH-KUH) in order to perform root cause analysis of the pertinent problem areas and plan a multifaceted, contextualized, feasible and evidence-based COPD care bundle. Following a better understanding of the baseline characteristics and current management of COPD patients in the ED, we intend to gain insight on how to improve the ED care and management of patients with COPD and implement the identified management strategies in a resource-limited setting.
Methods
Study Design
This is a prospective cross-sectional observational study as an initial baseline stage for a QI project to explore the current problems in ED care of patients with AECOPD.
Study Setting
Emergency Medicine is in its primitive stage in Nepal.27 DH-KUH is a not for profit, community hospital located in the Kavrepalanchok district. DH-KUH is a 350-bedded tertiary care teaching hospital with a 30-bedded ED. The clinical providers include 5 consultant physicians, 12 house officers, 3 resident doctors, 18 nurse practitioners including health assistants and paramedics. The ED is equipped with central oxygen supply, 2 bedside nebulizers, and 2 bilevel positive-airway pressure (BiPAP) machines. The ED has approximately 20,000 visits annually and has a high acuity level as per internal audits. It serves the community from various neighboring districts, namely, Kavrepalanchok, Sindhupalchok, Ramechaap, Bhaktapur and Kathmandu. The population from these districts are significantly exposed to tobacco smoke and indoor air pollution due to traditional cooking with biomass fuel and COPD is the leading cause of death in Nepal.4,7 The previous study showed that the prevalence of dyspnea among patients attending the ED at our hospital was 8.9% (95% CI = 4.6%, 13.2%) in 2019.12 Patients presenting to the ED are immediately triaged and directed towards different designated areas according to the severity of their disease. Respiratory therapy, pulmonary rehabilitation and structured drug counseling services are currently unavailable in our ED.
Patient Population
Consecutive patients presenting to DH-KUH ED with a primary diagnosis of AECOPD were included during two representative time periods of the year: one month (July 2019) during summer and three months (November 2019-January 2020) during winter. Patients were triaged and a diagnosis of AECOPD was made by attending physicians based on clinical history and examination. Both AECOPD encounters with the first and repeated presentation for subsequent exacerbation were included. Patients who were not admitted through the ED (6 patients), who did not consent to answer the survey questions (2 patients), and those with primary disease other than COPD (2 lung cancer, 1 active tuberculosis, 4 left heart failure, 1 pulmonary embolism) were excluded from the study. Revisit was considered as any unplanned visit to ED within one year following discharge from any center with a primary complaint related to AECOPD. The revisit duration was further categorized into within 3 days, 3–7 days, 30 days, and 1–12 months.
Sample Size
The recent study done in our ED12 showed the prevalence of COPD in our ED of 5.6%. By using the formula of z2pq/d2, based on the prevalence (p) 5.6%, a precision (d) of 3.0% with 95% confidence interval (CI), we calculated the sample size for this study to be a minimum of 225 patients.
Study Protocols/Variables
As the standard regular ED practice at our hospital, AECOPD patient management disposition decision and strategy were based on individual treating physicians. A trained research assistant and interns posted in the ED collected the data from electronic medical records (EMR) and recorded the demographic characteristics, clinical characteristics, past medical history, details of current ED care delivery, and disposition (supplementary file 1). As one of the objectives of this study was to describe current treatment practices in the ED, the drugs administered and its route, the use of BiPAP and assisted ventilation were noted. They administered the questionnaire (items 50–55 supplementary file 1) to the patients before disposition after a verbal consent and recorded the details in a predesigned form. The identity of the patient was kept confidential.
Variables studied included patient demographics (age, gender, address, education), mode of transportation, smoking status at the time of interview, lifetime exposure to woodfire smoke, use of domiciliary oxygen, self-reported drug compliance, hospitalization in the last year for AECOPD, comorbidities {hypertension (HTN), diabetes mellitus (DM), and IHD} triage details {triage category: red -highest acuity (level 1), orange (level 2), yellow (level 3), green (lowest acuity level 4) and triage vitals: oxygen saturation, pulse rate, respiratory rate, systolic and diastolic BP}, and presenting complaints. ED care variables or the quality improvement variables were previous presentations to the ED (within the last 1 year, 1 month, 7 days and 3 days); vaccination status and counseling during discharge, use of spirometry for diagnosis (self-reported), compliance to treatment (self-reported), investigations performed in the ED, treatment details offered in the ED (use of steroids, antibiotics, BiPAP), duration of stay in the ED, disposition of the patients, COPD medication prescribed at discharge, follow-up advice, inhaler technique explained and reaffirmed by staff in the ED, and written action plan.
The primary outcome measures were 30-day ED revisit and near-fatal events. The 30-day ED revisit was defined as an ED visit for AECOPD within 30 days of discharge from any center. Near-fatal events encompassed the severe triage category (red- level 1), need of intensive care unit (ICU) admission, mortality cases, referral (as a referral from our hospital would mostly be for ICU due to unavailability of ICU beds) and those who were intubated and in whom BiPAP was initiated during their ED stay. The authors or a trained research assistant and interns entered data into the predesigned proforma from the EMR system and asked the five survey questions before disposition from the ED after verbal consent. (items 50–55, Supplementary file 1)
Data Analysis
Data were collected and entered in Excel and analyzed with the statistical package for social sciences (SPSS) version 21. The categorical variables are expressed as frequency/proportion and continuous ones with mean with standard deviation (SD) or median with interquartile range (IQR) as appropriate. Categorical variables were compared with the chi-square test. The Independent-samples t-test or Mann–Whitney U-test was used to compare the continuous variables with the categorical variables. P values of less than 0.05 were considered significant. Variables significant at P value ≦ 0.2 were further combined and analyzed with binary logistic regression.
The problems and system failures were identified and categorized. The multidisciplinary team (emergency physician, internal medicine specialist and pharmacologist) worked together to perform the root cause analysis to identify the potential problems based on evidence-based guidelines on best practices and current ED practice in our setting. The root cause analysis is illustrated in the cause-effect diagram. The Pareto analysis was performed for the identified list of problems in the ED care delivery to help prioritize the ones with the biggest impact which would guide decisions to make action plans in the next phase of our study.
Results
A total of 249 COPD patient encounters were studied. One-third of the patients were aged 60–80 years, and the majority of patients (67.9%) were female. The literacy rate was 15.7%. The 30-day ED revisit rate was 38.2% (95/249) and 28.4% of them (27/95) had visited the ED within the last 7 days. Mean oxygen saturation on presentation was 75% (SD ±16%) and 84% (209/249) patients had SPO2 < 90%. In contrast, 39% (97/249) had home oxygen. Further characteristics of patients presenting to ED with AECOPD during the sampling period are presented in Table 1.
 |
Table 1 Characteristics of Patients Presenting to ED with AECOPD (n=249) |
Dyspnea was the most common presenting complaint (93.6%). There was 1.2% ED mortality and another 19% near-fatal outcome. The detailed clinical characteristics of the patients is shown in Table 2. BiPAP was started in 6.4% of the patients. Arterial blood gas (ABG) analysis was performed in 87 patients (35%), out of which 54 (62%) had PaCO2 >45 mm Hg. Three (5.6%) out of these 54 patients with hypercarbia required intubation and eight (14.8%) received BiPAP. Rest (79.6%) did not receive BiPAP though it was indicated according to the ABG finding. One hundred and thirty-six patients (54.6%) were discharged home, 73 (29.3%) were admitted to the ward, and 10 (4%) to an ICU, with 18 (7.2%) leaving against medical advice (LAMA). Written COPD emergency management clinical practice guidelines and discharge action plans were absent. The smoking cessation was discussed among 24 out of 32 (75%) current smokers. The details of investigations sent from ED, current treatment pattern and disposition are shown in Table 3.
 |
Table 2 Clinical Characteristics of the Patients on Presentation to ED with AECOPD (n=249) |
 |
Table 3 Current ED Treatment Pattern, Disposition and Discharge Details of AECOPD Patients |
The relation of near-fatal outcome and 30-day ED revisit to other variables is depicted in Tables 4 and 5. Patients with near-fatal outcomes during presentation were significantly less compliant to medication (P value <0.001) and had visited the ED within 30 days of prior ED visit (P value= 0.007). Patients who required domiciliary oxygen had more 30-day revisits to the ED (54.7% vs 29.2%; P value < 0.001). Similarly, 30-day revisits were significantly higher for those who had a previous inpatient admission (P value = 0.001), Those who had 30-day revisit had significantly worse PaCO2 in the ABG (P value =0.0310) and had more near-fatal outcomes (P value =0.007). Those independent variables which showed P value of <0.2 in the bivariate analysis of 30-day revisits (age, previous admission, domiciliary oxygen, duration of ED stay) and near-fatal outcome (mode of transportation, compliance to treatment, present smoker, domiciliary oxygen, visit to ED within 30 days, duration of ED stay and triage saturation) were chosen for binary logistic regression. For 30-day revisits, the Hosmer-Lemeshow goodness-of-fit test indicated that the model described the data well (P value = 0.796). The model explained 14.9% (Nagelkerke R2) of the variance in 30-day revisit and correctly classified 67.1% of cases. The 30-day revisit was twice more likely among those who were previously admitted (OR=1.98; 95% CI 1.11–3.59; P value =0.022) and 2.5 times more among those who were in domiciliary oxygen (OR=2.5; 95% CI=1.43–4.4; P value =0.001). For near-fatal outcome, the Hosmer-Lemeshow goodness-of-fit test indicated that the model described the data well (P value = 0.770). The model explained 19.1% (Nagelkerke R2) of the variance in near-fatal outcome and correctly classified 81.8% of cases. The near-fatal outcome was 3.5 times likely among those who were non-compliant to treatment (OR=3.55; 95% CI=1.64–7.67; P value =0.001) and 2.9 times more among those who had visited within 30 days (OR=2.86; 95% CI=1.362–6.18; P value =0.006). Other variables failed to show the significant relation with the regression test. ABG was not included in the regression analysis as it was performed only in 35% of the cases.
 |
Table 4 Near-Fatal Outcome in Relation to Variables Among the AECOPD Patients (n=231) |
 |
Table 5 30-Day ED Revisit in Relation to Other Variables Among the AECOPD Patients (n=249) |
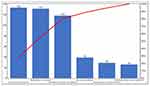
Based on the categories and themes (patients factor, ED providers, ED policies, equipment failure, discharge process and follow ups including spirometry to confirm those cases who were diagnosed to have COPD on clinical grounds only), the fishbone cause effect diagram was created (Figure 1). A Pareto analysis was performed for key identifiable errors during the discharge process from the ED. They were ranked according to the frequency, cumulative percentage was calculated and expressed in the Pareto chart in Figure 2. The team discussed the errors, recent evidence-based guidelines8,28 and feasibility to identify various potential interventions with their indicators (input measures and/or process measures) (Table 6).
 |
Table 6 Interventions and Quality Indicators Planned for Phase 2 of ED AECOPD QI Project |
 |
Figure 1 Fishbone cause and effect diagram in reference to the baseline findings. |
Discussion
In this study, we studied detailed data on characteristics, current treatment practices and outcomes of AECOPD patients presenting to the ED of a major teaching hospital in Nepal. Various performances of COPD care were measured and the lacunes were identified which are illustrated in the cause-effect diagram and Pareto chart (Figures 1 and 2). Potential interventions were listed with their indicators for future implementation (Table 6). Our study showed that 38.2% of the COPD patients presented to ED within 30 days of discharge from the ED and 19% experienced a near-fatal outcome. Moreover, those who visited the ED within 30 days had significantly higher near-fatal outcomes. Therefore, these two variables were identified as the primary outcome targets for future interventions.
General Characteristics of the Study Population
This study in the population presenting to DH-KUH ED affirms and extends results from a previous study. The highest prevalence of AECOPD was seen in women and adults between the age of 60–69 years.22 This high prevalence may stem from a combination of indoor air pollution from unvented fires, cigarette smoking, recurrent chest infections, treated tuberculosis with post-tuberculosis bronchiectasis, as well as ambient outdoor air pollution found in larger cities like Kathmandu and Bhaktapur.23 AECOPD in Southeast Asia has been shown to be associated with greatly increased morbidity and mortality and this study supports this research.21 Our study showed a high near-fatal outcome in the study population (19%). A previous survey done in our ED found that AECOPD is a major presentation and the highest 90-day mortality was in individuals with known COPD.29 Comorbidities like HTN, DM and IHD were present in 18.9%, 7.2% and 2.4% of cases in this study.
COPD Performance Measures
30-Day Revisit to the ED
Revisits to the ED among patients with AECOPD are common, with poorer outcomes and added cost.18 The 30-day revisit rate is a widely used metric indicating the need for improvement in the healthcare system. Identifying and mitigating the risk factors for readmission in patients with COPD has been done earlier in other countries. Rates in the US are documented at 18–20%.30 In this study population, 38% of patients were known to revisit the ED within a month from their initial visit among which 6% visited within 3 days and 22% within 3–7 days. They had significantly higher near-fatal outcomes. Those who were previously admitted in the hospital and on domiciliary oxygen had significantly higher 30-day revisit rates. This may reflect the severity of the disease, as those who require oxygen at home may have a severe form of the disease.
A study evaluating readmission rates for AECOPD in a North American context showed that there were higher readmission rates in an ED setting compared to patients admitted for in-hospital management.31 The authors postulated that a lack of standardized management, as well as counseling and follow-up services, likely contributed to the higher readmission rates. Unlike other studies,32,33 our study did not identify age and gender as significant predictors for revisits to the ED. As fewer patients underwent spirometry (2%) to confirm the diagnosis of COPD, we suspect that a proportion of those patients receiving treatment for COPD may have alternative diagnoses. Recent guidelines suggest that the spirometry is essential for the diagnosis of COPD.8 It is crucial that COPD is diagnosed correctly, as an inappropriate diagnosis (false-positive or false-negative) and over or under treatment may lead to harmful consequences.34 Various pulmonary and cardiac diseases share common symptoms which may create diagnostic error and harmful treatments. Vaccination rates are lower than in western countries (10.8%), in part due to the significant cost to the individual patient. Standardized ED treatment protocols, targeted therapy based on spirometry, action plans for patients during discharge, and improved access to home oxygen services are likely to be important and are listed in the bundle-care.
Near-Fatal Outcomes
Near-fatal outcome was experienced by 19% of the sample population. The patients who left against medical advice (n=18) were excluded from this data analysis as the outcomes of those patients were unknown. Among all the patients, 10.8% were triaged as level 1(red category), 6.4% were on BiPAP, 2.8% required intubation, 1.2% died in the ED, 4% were admitted in the ICU and 3.6% were referred due to unavailability of ICU beds. Almost half of the patients who were transferred to the hospital via ambulance had near-fatal outcomes. A previous study showed that the patients with frequent ED visits accounted for 64.4% of all near-fatal events.33 In our study, those who visited the ED within 30 days of discharge had significantly higher near-fatal events. Non-compliance to treatment was also one of the significant variables related to the near-fatal outcome. This finding may also suggest inadequate or untimely follow up of these patients on an outpatient basis. Compliance with medical treatment was identified as an important outcome, increasing the risk for near-fatal outcomes and 30-day readmissions. There are likely complex reasons for this, including ongoing smoke exposure, affordability of medication, availability of home oxygen, decreased health literacy, and limited routine outpatient care.35 The binary analysis showed that those who stayed in the ED for a longer duration had significantly higher near-fatal events. However, the regression failed to prove the association. Moreover, longer stays may have been needed due to severity of illness and not necessarily long waiting times. Further in-depth study needs to be done in regards to the true association between the waiting time for COPD patients in the ED.
Potential Quality Improvement Interventions
The availability of diagnostic and treatment options for COPD differs across varying resource settings. A number of studies exploring the bundles of interventions have been shown to reduce the readmission rate and mortality.20–22 There is a lack of data on economic evaluation of COPD from resource limited settings. The priorities and feasibility of the bundles in the COPD care vary according to the gap in care and the resources available and cannot be generalized.35 These data evaluated in this study are helpful in determining potential interventions for next phase of the study to ultimately improve the quality of AECOPD treatment in the Nepali ED setting. The first intervention proposed is aimed to improve and standardize the diagnosis of COPD (Table 6). As spirometry was rarely used or recorded in the diagnosis of COPD, the diagnosis was mainly made by clinical presentation. Thus, implementation of a symptom and history checklist in all ED patients who present with chronic respiratory symptoms, as well as increasing the percentage of spirometry and echocardiography done on patients can help standardize the diagnosis. This would allow for a more accurate diagnosis of COPD and standardization of care.
The second intervention proposed is to initiate a COPD emergency care bundle. This entails increasing the use of BiPAP, and generating clinical practice guidelines within the ED team (Table 6). Training ED care providers on LUS in patients presenting with dyspnea can improve point of care diagnosis with less exposure to x-rays.36 Training ED providers to follow and adhere to standard guideline-based treatment may also aid in decreasing the number of revisits to the ED.
The third intervention proposed is to initiate a COPD discharge care bundle (Figure 2, Table 6). Patient education on symptom management can be very beneficial in their care, but because of lower literacy rates, written instructions may be less useful. For example, providing a discharge checklist, written action plan, as well as reinforcing inhaler techniques and providing counseling on smoking cessation and woodfire exposure may improve understanding and compliance if presented in a way that the patient or associated patient family can understand. The data in this study also show very low rates of vaccinations, therefore providing education and increasing vaccination rates can also aid these patients greatly. With more patients being educated on how to manage their chronic condition, this goal can aim to decrease revisits to the ED. Improving follow-up care outpatient clinic visits, and improved rates of pneumococcal and influenza vaccinations may help reduce ED excess utilization. Pulmonary rehabilitation services are available in our hospital and should be utilized with generous referrals of the patients and consultations in the ED. Attendance in pulmonary rehabilitation would be useful, as it has been demonstrated to improve outcomes in other settings.26
This study has certain limitations as it was conducted in one institution only. Though the findings of the current study are likely to be similar to other institutions, the findings cannot be generalized. The findings of the ‘current system’ and identified opportunities are only specific to this single-center as each context varies in its resources. The diagnosis was based on the judgement of the physician and 98% of patients labeled with AECOPD did not have objective confirmation with spirometry hence there is a possibility that the included patients were mislabeled as COPD and had another diagnosis than COPD. A portion of patients were not included due to missing data or transfer to another facility. The compliance mentioned was self-reported, and would benefit from external validation as recall bias from the patient interviews is likely. The details about the patient’s medication history could not be traced and explored in relation to the primary outcome (ED revisits and near-fatal outcome). The detailed interview with the patients revisiting the ED would be helpful to explore their perspective and also find out other diagnoses.
Conclusion
The measures of COPD performance were overall inadequate. More than one-third of the ED patients with the diagnosis of AECOPD had 30-day revisits and near-fatal outcomes were statistically associated with the revisit rate. Special focus needs to be targeted to this group of patients. The opportunities to improve the diagnosis of COPD, ED care and discharge bundles were identified and the feasible interventions involving multifaceted teams were recommended to better manage COPD patients presenting to the ED. The present study recommends the urgent implementation of these bundles care and protocol-based management plan for AECOPD in a busy resource-limited ED which could decrease the ED revisits and the deleterious outcomes.
Abbreviation
AECOPD, acute exacerbation of chronic obstructive pulmonary disease; ABG, arterial blood gas; BiPAP, bilevel positive airway pressure ventilation; BP, blood pressure; COPD, chronic obstructive pulmonary disease; CI, confidence interval; DH-KUH, Dhulikhel Hospital-Kathmandu University Hospital; DM, diabetes mellitus; ED; emergency department; EP; emergency physician; EMR, electronic medical records; HTN, hypertension; ICU, intensive care unit; IQR, interquartile range; IHD, ischemic heart disease; KUSMS, Kathmandu University School of Medical Sciences; LAMA, leave against medical advice; LMIC, low and middle income countries; LUS, lung ultrasound; MCW, Medical College of Wisconsin; NCD, non-communicable disease; OPD, outpatient department; OR, Odds ratio; PDSA, Plan Do Study Act; QI:quality improvement; SD, standard deviation; SPSS, statistical package for social sciences; YLD, years lived with disability.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval
Ethical approval was provided by the institutional review committee of Kathmandu University School of Medical Sciences/Dhulikhel Hospital (KUSMS-DH, number: 166/19). The written consent was waived as this is a part of the quality improvement project. Verbal consent was taken from the participants prior to administration of the 5-item survey questionnaire before discharge.
Acknowledgments
The authors thank DH-KUH ED staff for support during the study period, Ms. Soniya Makaju for help in data collection. We highly appreciate the generosity of Dr Kristopher Brickman, University of Toledo, USA for making the BiPAP machines available in our ED.
Author Contributions
RS, AP and TM conceptualized the study. RS, APS, TM and RaS obtained ethical approval. APS, RS and JM performed data collection and analysis. RS, APS, TM and JM wrote the draft manuscript. All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. López-Campos JL, Tan W, Soriano JB. Global burden of COPD. Respirology. 2016;21:14–23. doi:10.1111/resp.12660
2. Chronic obstructive pulmonary disease (COPD). Available from: https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd).
3. Adeloye D, Chua S, Lee C, et al. Global and regional estimates of COPD prevalence: systematic review and meta-analysis. J Glob Health. 2015;5:020415. doi:10.7189/jogh.05.020415
4. Bhandari GP, Angdembe MR, Dhimal M, et al. State of non-communicable diseases in Nepal. BMC Public Health. 2014;14:23. doi:10.1186/1471-2458-14-23
5. Pokharel BR, Humagain S, Pant P, et al. Spectrum of diseases in a medical ward of a teaching hospital in a developing country. J College Med Sci. 2012;8:7–11. doi:10.3126/jcmsn.v8i2.6831
6. Bhandari R, Sharma R. Epidemiology of chronic obstructive pulmonary disease: a descriptive study in the mid-western region of Nepal. Int J Chron Obstruct Pulmon Dis. 2012;7:253–257. doi:10.2147/COPD.S28602
7. Nepal; 2015. Available from: http://www.healthdata.org/nepal.
8. Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease, 2020 report; 2020. Available from: https://goldcopd.org/wp-content/uploads/2019/11/GOLD-2020-REPORT-ver1.0wms.pdf.,
9. World Health Organization. Country Office for Nepal. [Package of essential non communicable disease (PEN) intervention at primary health service setting: PEN training trainee’s manual]; 2019. Available from: https://apps.who.int/iris/handle/10665/310930.
10. Bishwajit G, Tang S, Yaya S, et al. Burden of asthma, dyspnea, and chronic cough in South Asia. Int J Chron Obstruct Pulmon Dis. 2017;12:1093–1099. doi:10.2147/COPD.S133148
11. Clark EG, Watson J, Leemann A, et al. Acute care needs in an Indian emergency department: A retrospective analysis. World J Emerg Med. 2016;7:191–195. doi:10.5847/wjem.j.1920-8642.2016.03.005
12. Shrestha AP, Shrestha R, Shrestha SK, et al. Prevalence of dyspnea among patients attending the emergency department of a tertiary care hospital: a descriptive cross-sectional study. J Nepal Med Assoc. 2019. doi:10.31729/jnma.4582.
13. Shrestha A, Bajracharya S, Acharya S, et al. Clinical profile of patient presenting with shortness of breath at patan hospital emergency. Heart Fail. 2017;6:33–41.
14. Soler-Cataluna JJ. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax. 2005;60:925–931. doi:10.1136/thx.2005.040527
15. Seemungal TA, Donaldson GC, Paul EA, et al. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;157:1418–1422. doi:10.1164/ajrccm.157.5.9709032
16. Makris D, Moschandreas J, Damianaki A, et al. Exacerbations and lung function decline in COPD: new insights in current and ex-smokers. Respir Med. 2007;101:1305–1312. doi:10.1016/j.rmed.2006.10.012
17. Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363:1128–1138. doi:10.1056/NEJMoa0909883
18. Guerrero M, Crisafulli E, Liapikou A, et al. Readmission for acute exacerbation within 30 days of discharge is associated with a subsequent progressive increase in mortality risk in COPD patients: a long-term observational study. PLoS One. 2016;11:e0150737. doi:10.1371/journal.pone.0150737
19. Almagro P, Calbo E, Ochoa de Echagüen A, et al. Mortality after hospitalization for COPD. Chest. 2002;121:1441–1448. doi:10.1378/chest.121.5.1441
20. Zafar MA, Loftus TM, Palmer JP, et al. COPD care bundle in emergency department observation unit reduces emergency department revisits. Respir Care. 2020;65:1–10. doi:10.4187/respcare.07088
21. McCarthy C, Brennan JR, Brown L, et al. Use of a care bundle in the emergency department for acute exacerbations of chronic obstructive pulmonary disease: a feasibility study. Int J Chron Obstruct Pulmon Dis. 2013;8:605–611. doi:10.2147/COPD.S52883
22. Ospina MB, Mrklas K, Deuchar L, et al. A systematic review of the effectiveness of discharge care bundles for patients with COPD. Thorax. 2017;72:31–39. doi:10.1136/thoraxjnl-2016-208820
23. Bock A, Chintamaneni K, Rein L, et al. Improving pneumococcal vaccination rates of medical inpatients in urban Nepal using quality improvement measures. BMJ Qual Improv Rep. 2016;10. doi:10.1136/bmjquality.u212047.w4835.
24. Kc A, Wrammert J, Clark RB, et al. Reducing perinatal mortality in nepal using helping babies breathe. Pediatrics. 2016;137:e20150117–e20150117. doi:10.1542/peds.2015-0117.;.
25. Schwarz D, Schwarz R, Gauchan B, et al. Implementing a systems-oriented morbidity and mortality conference in remote rural Nepal for quality improvement. BMJ Qual Saf. 2011;20:1082–1088. doi:10.1136/bmjqs-2011-000273
26. Siddharthan T, Pollard SL, Quaderi SA, et al. Effectiveness-implementation of COPD case finding and self-management action plans in low- and middle-income countries: global excellence in COPD outcomes (GECo) study protocol. Trials. 2018;19:571. doi:10.1186/s13063-018-2909-8
27. Shrestha AP, Shrestha R, Shrestha SK, et al. Emergency medicine education and research in nepal: challenges and opportunities. JNMA J Nepal Med Assoc. 2018;56:716–718. doi:10.31729/jnma.3573
28. World Health Organization. Chronic respiratory diseases management of Asthma, management of chronic obstructive pulmonary disease. Available from: https://www.who.int/ncds/management/2.3_Chronic_respiratory_diseases-WHOPEN.pdf.
29. Giri S, Rogne T, Uleberg O, et al. Presenting complaints and mortality in a cohort of 22 000 adult emergency patients at a local hospital in Nepal. J Glob Health. 2019;9. doi:10.7189/jogh.09.020403.
30. Goto T, Faridi MK, Gibo K, et al. Trends in 30-day readmission rates after COPD hospitalization, 2006–2012. Respir Med. 2017;130:92–97. doi:10.1016/j.rmed.2017.07.058
31. Bartels W, Adamson S, Leung L, et al. Emergency department management of acute exacerbations of chronic obstructive pulmonary disease: factors predicting readmission. Int J Chron Obstruct Pulmon Dis. 2018;13:1647–1654. doi:10.2147/COPD.S163250
32. Simmering JE, Polgreen LA, Comellas AP, et al. Identifying patients with COPD at high risk of readmission. Int J Chron Obstruct Pulmon Dis. 2016;3:729–738.
33. Hasegawa K, Tsugawa Y, Tsai C-L, et al. Frequent utilization of the emergency department for acute exacerbation of chronic obstructive pulmonary disease. Respir Res. 2014;15:40. doi:10.1186/1465-9921-15-40
34. Hangaard S, Helle T, Nielsen C, et al. Causes of misdiagnosis of chronic obstructive pulmonary disease: A systematic scoping review. Respir Med. 2017;129:63–84. doi:10.1016/j.rmed.2017.05.015
35. Aït-Khaled N, Enarson D, Bousquet J. Chronic respiratory diseases in developing countries: the burden and strategies for prevention and management. Bull World Health Organ. 2001;79:971–979.
36. Shrestha R, Blank W, Shrestha AP, et al. Evaluation of interdisciplinary emergency ultrasound workshop for primary care physicians in Nepal. Open Access Emerg Med. 2020;12:99–109. doi:10.2147/OAEM.S246656
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.