Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 14
NDSP 09: Risk Assessment of Pakistani Individual for Diabetes (RAPID) – Findings from Second National Diabetes Survey of Pakistan (NDSP) 2016–2017
Authors Abdul Basit K, Fawwad A, Riaz M, Tahir B, Khalid M, Basit A
Received 20 August 2020
Accepted for publication 25 November 2020
Published 19 January 2021 Volume 2021:14 Pages 257—263
DOI https://doi.org/10.2147/DMSO.S277998
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Antonio Brunetti
Khalid Abdul Basit,1,2 Asher Fawwad,3,4 Musarrat Riaz,5 Bilal Tahir,4 Maria Khalid,4 Abdul Basit5
1Department of Acute Medicine, Whipps Cross University Hospital, Barts Health NHS Trust, London, England; 2Department of Population Health, University College London, London, England; 3Department of Biochemistry, Baqai Medical University, Karachi, Pakistan; 4Department of Research, Baqai Institute of Diabetology and Endocrinology, Baqai Medical University, Karachi, Pakistan; 5Department of Medicine, Baqai Institute of Diabetology and Endocrinology, Baqai Medical University, Karachi, Pakistan
Correspondence: Abdul Basit
Department of Medicine, Baqai Institute of Diabetology and Endocrinology, Baqai Medical University, Plot No.: 1-2, II-B, Nazimabad No 2, Karachi, Pakistan
Tel +92 21 36707179
Email [email protected]
Objective: To elucidate the effectiveness of Risk Assessment of Pakistani individuals with diabetes (RAPID) tool in epidemiological and population-based second National Diabetes Survey of Pakistan (NDSP) 2016– 2017 for identifying risk of developing type 2 diabetes.
Methodology: This observational study was a sub-analysis of the second National Diabetes Survey of Pakistan (NDSP) 2016– 2017 conducted from February 2016 to August 2017 in all four provinces of Pakistan. Ethical approval was obtained from National Bioethics Committee Pakistan. RAPID score, a validated and published scoring scale to assess risk of diabetes, originally developed from community-based surveys was used. The risk score is assessed by parameters namely: age, waist circumference, and positive family history of diabetes. Subjects with score greater ≥ 4 were considered at risk of diabetes.
Results: A total of 4904 individuals were assessed (2205 males and 2699 females). Mean age of participants was 41.8± 14.2 years. Positive family history of diabetes was seen in 1379 (28.1%) people. According to RAPID score 1268 (25.9%) individuals scored ≥ 4 and were at risk of diabetes. OGTT status of people at risk of diabetes according to RAPID score showed that 18.1% people with diabetes and 29.2% were prediabetic. Whereas, OGTT status of people not at risk of diabetes showed that only 7.6% people with diabetes, 20% were prediabetic.
Conclusion: A simple diabetes risk score can be used for identification of high-risk individuals for diabetes so that timely intervention can be implemented. Community-based awareness programs are needed to educate people regarding healthy lifestyle in order to reduce risk of diabetes.
Keywords: risk score, diabetes, NDSP, RAPID, Pakistan
Introduction
Type 2 diabetes is amongst the most common chronic disease and a serious public health challenge of 21st century for both the developed and developing world.1,2 The increasing prevalence is not only contributing to the health burden, a significant economic impact is also noted.3 According to the International Diabetes Federation (IDF), it is anticipated that the number of people with diabetes in 2019 will rise approximately by two-fold in 2045 from 463 to 700 million.4
The second National Diabetes Survey of Pakistan (NDSP) 2016–2017 showed that 26.3% of the population is suffering from diabetes.5 This high prevalence is fueled by aging, physical inactivity, unhealthy food choices and stress of diverse origins.6 However, the effect of these environmental factors changes with variance in the genome.7 With maternal gene predominance, the lifetime risk of developing diabetes escalates to about 40% with single parental disease and to around 70%, if both parents are affected.8
Recent statistics have revealed that more than a quarter of the total diabetic population are unaware of their disease.9 Laboratory screening modalities including fasting blood glucose, HbA1c, OGTT are all reliable in detecting diabetes.10 However, mass screening is essential for early detection and appropriate intervention as the disease is usually asymptomatic in the early stages., a cost-effective measure for resource-limited health care systems.11 For this reason, The American Diabetes Association (ADA) recommends regular screening for type 2 diabetes and repeating subsequently every three years.12
Various models have been proposed for risk assessment of diabetes, but results are almost always heterogeneous. This includes Finnish, British, Canadian, Australian, German, Chinese and Indian risk assessment models comprising of designed questionnaires, anthropometric, demographic, family history and elementary lifestyle information.13–17
A similar algorithm was designed named, RAPID (risk assessment of Pakistani individuals for diabetes) for identification of high-risk individuals through readily available variables without laboratory intervention or physician interpretation.18 In the present study we aim to access effectiveness of Risk Assessment of Pakistani individual with diabetes (RAPID) tool in the epidemiological and population-based second National Diabetes Survey of Pakistan (NDSP) 2016–2017 for identifying the risk of developing type 2 diabetes.
Methodology
This community-based observational study was a sub-analysis of second National Diabetes Survey of Pakistan (NDSP) 2016–2017 conducted from February 2016 to August 2017 in all four provinces of Pakistan. Ethical approval was obtained from National Bioethics Committee (NBC) of Pakistan. All Pakistani individuals aged 20 years or more, were eligible to participate after obtaining informed consent and this study was performed in accordance with the Declaration of Helsinki.
Detailed information regarding demographics, anthropometric and medical examinations was obtained with the help of the predesigned questionnaire.5 All information was gathered in one-to-one-based interviews by a trained survey officer. Detailed methodology has been published earlier.5 Stratification of the population was done based on urban and rural areas of all four provinces of Pakistan (Punjab, Sindh, Khyber, Pakhtunkhwa (KPK), and Baluchistan) as defined in the latest census. Each province was taken as a stratum and the districts a subdivision of provinces taken as clusters were identified from each stratum. Tehsils or towns are further bifurcation of districts considered as sub-clusters were taken from each identified cluster. Clusters and sub-clusters were selected randomly using probability proportional to size technique, and the number of clusters was taken from each province using the “rule of thumb”. Twenty-seven clusters were taken out of a total of 213 clusters throughout Pakistan. A total of 46 sub-clusters 21 from urban and 25 from rural were identified respectively.5
Out of 10,834 participants only 4904 fulfil the inclusion criteria for this study as shown in flow diagram of Figure 1.
 |
Figure 1 Flow diagram of the study. |
RAPID score was used in the study to estimate the risk of diabetes. RAPID score, a validated and published scoring scale to assess risk of diabetes in Pakistani individuals originally developed from community-based surveys was used.18 The risk score is assessed by parameters namely; age, waist circumference, and positive family history of the diabetes. Age in between 40–50 years was marked 1 whereas, age greater than 50 years was marked 3 points. Waist circumference greater than, or equal to cutoff point (80 cm for females and 90 cm for males) was marked 2 points and positive family history of diabetes was marked 1 point. Subjects with score greater or equal to 4 are considered at risk of diabetes.18
Oral glucose tolerance test (OGTT) was used for diagnosis of newly diabetes, prediabetes and normal individuals according to WHO criteria.5 Newly diagnosed diabetes was defined as fasting plasma glucose (FPG) level 126 mg/dL or greater or two-hour post/glucose load 200 mg/dL or greater or both. Known diabetes was considered if the participant had been already diagnosed or taking anti-diabetic medication. Subjects without diabetes were considered if FPG below 100 mg/dL and two-hour post/glucose load below 140 mg/dL.
Samples of intravenous blood was collected in vials containing EDTA-anticoagulant agent from all participants as per the standard producers.5 Sodium fluoride tube (for glucose), gel (for lipids) and EDTA K2 (for HbA1c). CHOD-PAP method for total cholesterol (TC), GPO-PAP method for triglycerides, homogeneous enzymatic calorimetric method for high density lipoprotein cholesterol (HDL-C) and CHOD-PAP method (Selectra Pro S instrument) for low-density lipoprotein cholesterol (LDL-C). HbA1c were performed by high-performance liquid chromatography (HPLC) method by D10. Detailed biochemical information has been published earlier.5
Statistical Analysis
Descriptive statistics were performed by using SPSS v. 20. Continuous variables were presented as mean ±standard deviation while categorical variables were presented as frequency (percentage).
Results
Demographic and biochemical characteristics of study population was shown in Table 1. Out of 4904 subjects, 44.9% were males and 55.1% were females. Mean age of the subjects was 41.8±14.2 years. Majority of the subjects were married (84.1%), and nontobacco users (84.4%). Positive family history of diabetes was present in 28.1% subjects. Mean body mass index and waist to hip ratiowere 26.84±5.83 kg/m2 and 0.94±0.2 cm respectively. Mean systolic and diastolic blood pressure was 124.69±18.22 and 83.2±13.01 mmHg respectively. Whereas, mean HbA1c was 5.53±1.35%.
 |
Table 1 Demographic and Biochemical Characteristics of Study Population |
Out of 4904 subjects, 25.9% people screened positive for risk of developing diabetes by RAPID score as shown in Figure 2. When these subjects undergo OGTT which is considered a gold standard for the diagnosis of diabetes, 18.1% turned out to be people with diabetes.
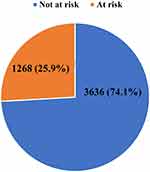 |
Figure 2 Risk status of diabetes by RAPID score. |
OGTT status of people at risk of diabetes (as per RAPID score) was shown in Table 2. According to OGTT criteria, 18.1% people at risk were diagnosed as diabetic, 29.2% were diagnosed as prediabetic while 52.7% were found to be nondiabetic. Similarly, OGTT status of people who were not at risk of diabetes was shown 7.6% people were diagnosed as diabetics, 20% were diagnosed as prediabetic while 72.4% were found to be nondiabetic.
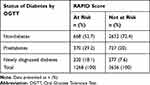 |
Table 2 OGTT Status Study Participants |
Discussion
In this sub-analysis of nationwide survey, a modest non-blood-based risk score based on age, family history of diabetes and waist circumference was built. This study found 25.9% people screened positive for risk of developing diabetes by RAPID score, of whom 18.1% turned out to be diabetic by OGTT. While, 74.1% people who were not at risk of diabetes by RAPID score, only 7.6% had developed diabetes by OGTT. We observed that the diabetes risk score performed approximately equally well and this second nationwide National Diabetes Survey of Pakistan (NDSP) 2016–2017 survey is comparable to studies from other parts of the world.19,20
Many studies have focused on the fact that type 2 diabetes can be prevented in high-risk subjects by lifestyle intervention.21 In prior studies, obesity measured by body mass index or waist circumference played a considerable role as modifiable risk factor in preventing early diabetes.22 In this sub-analysis, waist circumference instead of body mass index as other risk scores was used to provide a better indicator of accumulation of visceral fat and metabolic dysfunction. Our main aim was to provide a simple diabetes risk assessment tool, therefore, several other variables such as occupation, education, ethnicity, and lipid lowering therapy were excluded.18 In our study, waist circumference was used as a modifiable risk factor and was given a high-risk score of 2, in contrast, age and family history of diabetes are non-modifiable risk factors and were given a low risk score parallel to Indian Diabetes Risk Score (IDRS).23
Robust impact of BMI and family history leading to increased risk of diabetes was observed in Western European studies.24,25 Family history of diabetes is known to be an important marker for increased risk of diabetes. It reflects the genetic predisposition which may be necessary but not sufficient for development of type 2 diabetes.26 So, individuals with genetic susceptibility to diabetes, but with a healthy lifestyle can avoid the symptomatic phase of the disease.27 Physical activity, quality, and quantity of dietary fat and fiber intake have been demonstrated to modify the risk of diabetes.28
Existing recommendations that rely on blood testing for diabetes screening are not widely followed, resulting in the majority of subjects being left undiagnosed.29 The self-assessment method helps people to decide that they should seek medical care for testing diabetes.30 It gives a way to address the lack of interaction with health-care facilities/providers, alternatively reduce the percentage of undiagnosed diabetes, particularly in underserved people. However, RAPID score in our study was designed as a screening tool based on only three variables ensuring its simplicity for use and implementation. To our knowledge, this study is unique in demonstrating the simplified and convenient diabetes risk score (RAPID-score), an efficient screening tool used for estimating the risk of developing type 2 diabetes with several factors that are easy to measure with noninvasive methods, easily comprehensible, and direct attention to modifiable risk factors of diabetes among the Pakistani population. Moreover, RAPID score is safe and inexpensive screening test in a practical way to identify individuals at high risk of diabetes in general population, seems to demonstrate improvements upon the existing methods comparable to other studies, the model warrants further scrutiny before it can be used in other populations.31
Conclusion
A simple diabetes risk score can be used for the identification of individuals at high-risk for diabetes so that timely intervention can be implemented. Community-based awareness programs are needed to educate people regarding healthy lifestyle in order to reduce the risk of diabetes.
Highlights
- Risk assessment score used for exploring people who are at risk of developing diabetes
- Assessing parameters were age, waist circumference, and family history of diabetes
- Participant with score ≥4 was considered at risk of developing diabetes
- It is noninvasive, cost efficient and easily available score for predicting diabetes
Acknowledgments
We are very grateful to our NDSP members (with surnames in alphabetical order); Dr Mujeeb Ur Rehman Abro, Assistant Professor of Medicine, Chandka Medical College, Shaheed Mohtarma Benazir Bhutto Medical University, Larkana; Sindh, Dr Khawaja Ishfaq Ahmed, Ex-PGR, Pakistan Institute of Medical Sciences, Islamabad; Punjab, Dr Khurshid Ahmed, Consultant Physician, Zahid Medical Centre, Hub, Baluchistan; Dr Sobia Sabir Ali, Assistant Professor, Department of Diabetes and Endocrinology, Lady Reading Hospital, Peshawar, Khyber Pakhtunkhwa; Prof. Ahmed Bilal, Professor and Head of Medical Department Faisalabad Medical College, Faisalabad, Punjab; Dr Anam Butt, Research Officer, Baqai Institute of Diabetology and Endocrinology, Baqai Medical University, Karachi, Sindh; Prof. Bikha Ram Devrajani, Chairman, Department of Medicine and Director Sindh Institute of Endocrinology and Diabetes, Liaquat University of Medical and Health Sciences, Jamshoro, Sindh; Mr Ijaz Hayder, Research Officer, Pakistan Health Research Council, Karachi, Sindh; Dr Yasir Humayun, EPI coordinator, DHO Office, Mansehra, Khyber Pakhtunkhwa; Mrs Rabia Irshad, Research Officer, Pakistan Health Research Council, Karachi, Sindh; Dr Riasat Ali Khan, Diabetologist, Canada Medical Group Hospital, Defence, Karachi, Sindh; Dr Asima Khan, Head of Diabetes Department, Sindh Government Hospital, New Karachi, Karachi, Sindh; Dr Aamir Akram Khowaja, Postgraduate Resident, Sindh Government Qatar Hospital, Karachi, Sindh; Dr Raheela Khowaja, Postgraduate Resident, Baqai Institute of Diabetology and Endocrinology, Baqai Medical University, Karachi, Sindh; Prof. Qazi Masroor, Professor of Medicine and Head of Department, Quaid-e-Azam Medical College, Bahawalpur, Punjab; Dr Maqsood Mehmood, Head of Department, Fatma tu Zahra Hospital, Gujranwala, Punjab; Mr Hassan Moin, Statistician, Baqai Institute of Diabetology and Endocrinology, Baqai Medical University, Karachi, Sindh; Ms Nida Mustafa, Statistician, Baqai Institute of Diabetology and Endocrinology, Baqai Medical University, Karachi, Sindh, Pakistan; Dr Wasif Noor, Diabetologist, Akhuwat Health Services Diabetes Centre, Lahore, Punjab; Dr Huma Qureshi, Ex-Director, Pakistan Health Research Council, Islamabad, Punjab; Mr Ibrar Rafique, Research Officer, Pakistan Health Research Council, Islamabad, Punjab; Dr Tahir Rasool, Diabetologist, Akhuwat Health Services Diabetes Centre, Lahore, Punjab; Mrs Rubina Sabir, Laboratory Manager, Baqai Institute of Diabetology and Endocrinology, Baqai Medical University, Karachi, Sindh; Dr M. Arif N. Saqib, Senior Research Officer, Pakistan Health Research Council, Islamabad, Punjab; Dr Pir Alam Said, Medical Specialist DHQ, Sawabi, Khyber Pakhtunkhwa; Prof. Abrar Shaikh, Head Department of Medicine, Ghulam Muhammad Mahar Medical College, Sukkur, Sindh; Prof. AS Shera, Secretary General, Diabetic Association of Pakistan and WHO Collaborating Centre, Karachi, Sindh; Prof. Bilal Bin Younus, Head of Sakeena Institute of Diabetes & Endocrine Research, Lahore, Punjab; Prof. Salma Tanveer, Professor of Medicine, In-charge Diabetes and Endocrinology, Nishter Medical University, Multan, Punjab; Prof. Jamal Zafar, Professor of Medicine, Pakistan Institute of Medical Sciences, Islamabad, Punjab; for the supervision of the survey, concept, design, involved in the quality control and data management in their respective areas. We also acknowledge the support of the Clinical Laboratory and Research Department of BIDE, Karachi for data management and we would also like to thank Mr Muhammad Sohail and Mr Abdul Rashid from PHRC, Karachi. We are thankful to all study subjects for their participation and collaborating partner of this community-based second National Diabetes Survey of Pakistan (NDSP) 2016–2017. The abstract of this paper was presented at the International Diabetes Federation Conference (December 2–7, 2019) as an abstract presentation with interim findings.
Authors’ Authorship Statement
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The funding source for the study remained the same as in the second NDSP (2016–2017).3 Hemoglobin A1c evaluation and lipid profiles were performed by Pakistan Health Research Council (PHRC). Field visits and data collection including clinical and anthropometric measurements, fasting plasma glucose and two2-hour post/glucose load samples were run by the respective teams through their own funds. The whole survey was coordinated and supported by the Baqai Institute of Diabetology & Endocrinology (BIDE) on their own resources.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Gujral UP, Pradeepa R, Weber MB, et al. Type 2 diabetes in South Asians: similarities and differences with white Caucasian and other populations. Ann N Y Acad Sci. 2013;1281(1):51–63. doi:10.1111/j.1749-6632.2012.06838.x
2. Narayan KV. Type 2 diabetes: why we are winning the battle but losing the war? 2015 Kelly West award lecture. Diabetes Care. 2016;39(5):653–663. doi:10.2337/dc16-0205
3. Hex N, Bartlett C, Wright D, et al. Estimating the current and future costs of Type 1 and Type 2 diabetes in the UK, including direct health costs and indirect societal and productivity costs. Diabet Med. 2012;29(7):855–862. doi:10.1111/j.1464-5491.2012.03698.x
4. IDF diabetes atlas 9th edition; 2019. Available from: https://www.diabetesatlas.org.
5. Basit A, Fawwad A, Qureshi H, Shera AS. Prevalence of diabetes, pre-diabetes and associated risk factors: second national diabetes survey of Pakistan (NDSP), 2016–2017. BMJ Open. 2018;8(8):e020961. doi:10.1136/bmjopen-2017-020961
6. Mytton OT, Clarke D, Rayner M. Taking unhealthy food and drinks to improve health. BMJ. 2012;344(may15 2):2931. doi:10.1136/bmj.e2931
7. Sim X, Ong RT, Suo C, et al. Transferability of type 2 diabetes implicated loci in multi-ethnic cohorts from Southeast Asia. PLoS Genet. 2011;7(4):1001363. doi:10.1371/journal.pgen.1001363
8. Ahlqvist E, Ahluwalia TS, Groop L. Genetics of type 2 diabetes. Clin Chem. 2011;57(2):241–254. doi:10.1373/clinchem.2010.157016
9. Al Dawish MA, Robert AA, Braham R, et al. Diabetes mellitus in Saudi Arabia: a review of the recent literature. Curr Diabetes Rev. 2016;12(4):359–368. doi:10.2174/1573399811666150724095130
10. Nolan CJ, Damm P, Prentki M. Type 2 diabetes across generations: from pathophysiology to prevention and management. Lancet. 2011;378(9786):169–181. doi:10.1016/S0140-6736(11)60614-4
11. Zhou X, Pang Z, Gao W, et al. Performance of an A1C and fasting capillary blood glucose test for screening newly diagnosed diabetes and pre-diabetes defined by an oral glucose tolerance test in Qingdao, China. Diabetes Care. 2010;33(3):545–550. doi:10.2337/dc09-1410
12. American Diabetes Association. Screening for type 2 diabetes. Diabetes Care. 2004;27(11–4).
13. Rowan CP, Miadovnik LA, Riddell MC, Rotondi MA, Gledhill N, Jamnik VK. Identifying persons at risk for developing type 2 diabetes in a concentrated population of high-risk ethnicities in Canada using a risk assessment questionnaire and point-of-care capillary blood HbA1c measurement. BMC Public Health. 2014;14(1):929. doi:10.1186/1471-2458-14-929
14. Chen L, Magliano DJ, Balkau B, et al. AUSDRISK: an Australian Type 2 diabetes risk assessment tool based on demographic, lifestyle and simple anthropometric measures. Med J Aust. 2010;192(4):197. doi:10.5694/j.1326-5377.2010.tb03478.x
15. Gao WG, Dong YH, Pang ZC, et al. A simple Chinese risk score for undiagnosed diabetes. Diabet Med. 2010;27(3):274–281. doi:10.1111/j.1464-5491.2010.02943.x
16. Joshi SR. Indian diabetes risk score. J Assoc Physicians India. 2005;53:755–757.
17. Lee YH, Bang H, Park YM, et al. Non-laboratory-based self-assessment screening score for non-alcoholic fatty liver disease: development, validation and comparison with other scores. PLoS One. 2014;9(9):e107584. doi:10.1371/journal.pone.0107584
18. Riaz M, Basit A, Hydrie MZ, et al. Risk assessment of Pakistani individuals for diabetes (RAPID). Prim Care Diabetes. 2012;6(4):297–302. doi:10.1016/j.pcd.2012.04.002
19. Štiglic G, Fijačko N, Stožer A, Sheikh A, Pajnkihar M. Validation of the Finnish Diabetes Risk Score (FINDRISC) questionnaire for undiagnosed type 2 diabetes screening in the Slovenian working population. Diabetes Res Clin Pract. 2016;120:194–197. doi:10.1016/j.diabres.2016.08.010
20. Abbasi A, Peelen LM, Corpeleijn E, et al. Prediction models for risk of developing type 2 diabetes: systematic literature search and independent external validation study. BMJ. 2012;345(sep18 2):e5900. doi:10.1136/bmj.e5900
21. Lindström J, Tuomilehto J. The diabetes risk score: a practical tool to predict type 2 diabetes risk. Diabetes Care. 2003;26(3):725–731. doi:10.2337/diacare.26.3.725
22. Aekplakorn W, Bunnag P, Woodward M, et al. A risk score for predicting incident diabetes in the Thai population. Diabetes Care. 2006;29(8):1872–1877. doi:10.2337/dc05-2141
23. Kaushal K, Mahajan A, Parashar A, et al. Validity of madras diabetes research foundation: Indian diabetes risk score for screening of diabetes mellitus among adult population of urban field practice area, Indira Gandhi Medical College, Shimla, Himachal Pradesh, India. Indian J Endocrinol Metab. 2017;21(6):876. doi:10.4103/ijem.IJEM_361_16
24. Isomaa B, Forsén B, Lahti K, et al. A family history of diabetes is associated with reduced physical fitness in the Prevalence, Prediction and Prevention of diabetes (PPP)–Botnia study. Diabetologia. 2010;53(8):1709–1713. doi:10.1007/s00125-010-1776-y
25. Hippisley-Cox J, Coupland C, Robson J, et al. Predicting risk of type 2 diabetes in England and Wales: prospective derivation and validation of QDScore. BMJ. 2009;338(mar17 2):880. doi:10.1136/bmj.b880
26. Heianza Y, Qi L. Gene-diet interaction and precision nutrition in obesity. International Journal of Molecular Sciences. 2017;18(4):787.
27. Rosen ED, Kaestner KH, Natarajan R, et al. Epigenetics and epigenomics: implications for diabetes and obesity. Diabetes. 2018;67(10):1923–1931. doi:10.2337/db18-0537
28. Colberg SR, Sigal RJ, Yardley JE, et al. Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2016;39(11):2065–2079. doi:10.2337/dc16-1728
29. Cho N, Shaw JE, Karuranga S, et al. IDF diabetes atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–281. doi:10.1016/j.diabres.2018.02.023
30. Bang H, Edwards AM, Bomback AS, et al. A patient self-assessment diabetes screening score: development, validation, and comparison to other diabetes risk assessment scores. Ann Intern Med. 2009;151(11):775. doi:10.7326/0003-4819-151-11-200912010-00005
31. Bernabe-Ortiz A, Smeeth L, Gilman RH, et al. Development and validation of a simple risk score for undiagnosed type 2 diabetes in a resource-constrained setting. J Diabetes Res. 2016;2016:1–9. doi:10.1155/2016/8790235
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
