Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 16
Native American Patients with Chronic Obstructive Pulmonary Disease Exacerbations in a Tertiary Academic Medical Center – A Pilot Study
Authors Wu H , Rhoades DA, Chen S, Brown B
Received 26 December 2020
Accepted for publication 11 March 2021
Published 28 April 2021 Volume 2021:16 Pages 1163—1170
DOI https://doi.org/10.2147/COPD.S299178
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Huimin Wu,1 Dorothy A Rhoades,2 Sixia Chen,3 Brent Brown1
1Pulmonary, Critical Care and Sleep Medicine, College of Medicine, University of Oklahoma Health Sciences Center, Oklahoma City, OK, USA; 2General Internal Medicine, College of Medicine, and Stephenson Cancer Center, University of Oklahoma Health Sciences Center, OK, Oklahoma, USA; 3Biostatistics and Epidemiology, College of Public Health, University of Oklahoma Health Sciences Center, Oklahoma City, OK, USA
Correspondence: Huimin Wu
Pulmonary, Critical Care and Sleep Medicine, College of Medicine, University of Oklahoma Health Sciences Center, 800 Stanton L Young Blvd, Suite 8400, Oklahoma City, OK, 73104, USA
Tel +1 405-271-6173
Fax +1 405-271-5892
Email [email protected]
Purpose: The prevalence of chronic obstructive pulmonary disease (COPD) and comorbidities (eg diabetes and obesity) among Native American (NA) population are higher than among the general US population. However, studies of COPD in NAs are scarce. Oklahoma has the largest NA population affiliated with federally recognized tribes in the country and is an ideal location for such research. A pilot study was designed to investigate the characteristics of NA patients with COPD exacerbations in a tertiary academic medical center.
Patients and Methods: We conducted a retrospective exploratory study of NA adults with COPD exacerbation hospitalizations and/or emergency department visits at the University of Oklahoma Medical Center between July 2001 and June 2020. Medical records were reviewed to confirm COPD exacerbation and outcomes, including death, mechanical ventilation, intensive care unit (ICU) stay, home oxygen, and 30-day readmission. Additional collected data included socio-demographics, body mass index, diabetes, other COPD comorbidities and clinical variables.
Results: Of 630 encounters reviewed, 159 met the inclusion criteria, representing 91 patients. Most patients were female (64%), obese or overweight (68%), and had diabetes (42%) or hypertension (71%). Mean age was 60 years old, but women were 5 years younger than men. Among the 76 patients with COPD hospitalizations, 31 patients (41%) had an intensive care unit (ICU) stay and 19 (25%) were intubated in their last hospitalization. Among 9 patients (10%) with 30-day readmissions, 8 were female. Medicare, Indian Health Service, Tribal health service, or Medicaid were the most frequently used payment sources. Sex, diabetes, and obesity were not associated with hospital length of stay, 30-day readmission or supplemental O2 use.
Conclusion: Hospitalized NA COPD patients at this tertiary care center had multiple comorbidities. Many required ICU care and intubation. Larger studies of the risk and mitigating factors for COPD health outcomes in NA patients are needed.
Keywords: COPD, Native American, comorbidities, hospitalization
Introduction
Chronic obstructive pulmonary disease (COPD) is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities.1 COPD is a leading cause of death in the U.S.2 with smoking being by far the greatest risk factor for the disease. However, COPD patients often differ by comorbidity profiles, such as type 2 diabetes mellitus (DM) and obesity, and treatment specific to each comorbidity profile can alter the clinical course.3
Nationwide, the US Native American (NA) population has among the highest prevalence proportions of smoking,4 DM, and obesity,5,6 placing the population at high risk of poor outcomes for COPD. COPD prevalence among NAs, including American Indians and Alaska Natives, was 11% in 2011.2 This rate was higher than that among Non-Hispanic Whites (NHWs), non-Hispanic Blacks, Hispanics, or Asian/Pacific Islanders.2 Hospitalization rates for COPD among Medicare beneficiaries were highest among NAs compared with other racial or ethnic groups.2 Between 1999 and 2010, while COPD mortality was highest among NHWs, it significantly increased among NAs, while decreasing or remaining stable in other race/ethnic groups.2
However, description of the characteristics and outcomes of NA patients with COPD remains elusive in the literature. Oklahoma has a very high COPD prevalence (6th in the nation) and mortality (2nd in the nation).7 Oklahoma also has the largest population and highest percentage of American Indians and Alaska Natives affiliated with federally recognized tribes in the country.8 We provide a descriptive analysis of the characteristics of NA patients treated for COPD exacerbation at the University of Oklahoma Medical Center (OUMC) and explore potential risk factors associated with their health outcomes.
Patients and Methods
Study Population and Setting
The University of Oklahoma Health Sciences Center Institutional Review Board (IRB) approved this study (IRB number: 10716). Waiver of informed consent was granted due to the retrospective chart review nature of the study. We declare that all the data which can identify the personal information were encrypted and only de-identified data were included in the data analysis process. The research followed the precepts established by the Declaration of Helsinki.
The study population included NA men and women who had visited the OUMC for COPD exacerbations. Persons were included if they self-identified as NA during the hospital intake process as noted in the medical records. OUMC is the largest academic medical center and major transfer center in Oklahoma. It has the state’s largest intensive care unit (ICU). Approximately 25,000 COPD-related hospitalizations took place in OUMC in the past decade, and the pulmonary function test database has more than 10,000 spirometry reports.
We included both hospitalizations and emergency department (ED) encounters between July 2001 and June 2020. Some participants have only one hospitalization or ED encounter in the time frame, others have multiple hospitalizations or ED encounters. Most analyses presented herein represent characteristics at the last visit unless otherwise specified. Persons discharged from the ED or hospital with any diagnosis of COPD defined by International Classification of Diseases (ICD) codes (ICD-9: 490, 491, 494, 496, ICD-10: J41-44) and treated for COPD-related acute events, such as worsening shortness of breath and acute respiratory failure, were included. Encounters for patients who had stable COPD but were admitted for management of another condition or for other chronic respiratory diseases management, such as interstitial lung disease, bronchiectasis, and lung transplantation, were excluded.
Data Collection
Both primary (chart review) and secondary (administrative) data were obtained from the electronic health records (EHR). Trained research staff reviewed every chart to confirm participants’ treatment for COPD exacerbation and to audit the administrative data. If the primary data did not match the administrative data, the primary data was included for final data analysis. The project principal investigator reviewed more than 20% of the charts abstracted by research staff for quality control purpose.
The data collected from the medical record included age at last encounter, sex, smoking history, encounter type (ED-only vs hospitalization), insurance information, date of visit, height, weight, comorbidities (described below), use of home oxygen, history of prior OUMC visit for COPD exacerbation and pulmonary function test results. The COPD health outcome variables include hospital length of stay, ICU stay, mechanical ventilator use, supplemental O2 use on discharge, discharge disposition (home with self-care, home with home health, rehab facility, long-term acute care, skilled nursing, and others), 30-day readmission and death.
Comorbidities included cardiovascular diseases (coronary artery disease, heart failure, hypertension, peripheral vascular disease, arrhythmias, and stroke), metabolic diseases (DM and dyslipidemia), pulmonary and sleep disorders (asthma, lung cancer, and obstructive sleep apnea), and others (obesity, osteoporosis, anxiety/depression, gastroesophageal reflux, chronic kidney disease and anemia). Obesity was defined by standard categories of the body mass index (BMI; weight in kilograms divided by the square of the height in meters). BMI was classified into six categories: underweight (BMI <18.5), normal (BMI 18.5–24.99), overweight (BMI 25.0–29.99), obesity class I (BMI 30.0–34.99), class II (BMI 35.0–39.99), and class III (BMI of 40.0 or higher).
The payment sources were classified as Indian health (including Indian Health Service, Tribal health program, or Urban Indian health program), Medicare, Medicaid, commercial insurance, self-pay, charity and others. One patient may have more than one payment source.
Data Analysis
Data analysis was performed using STATA 16 software (StataCorp LLC, College Station, Texas).
Continuous variables are expressed as mean ± SD, or median, while discrete variables are shown as percentages. Between group comparisons are made using independent t-test (for 2 groups) or ANOVA (for >2 groups). Chi-squared tests are used to evaluate the relationship of two categorical variables. A two-tailed p value <0.05 is considered statistically significant. Linear regression and logistic regression analyses are performed to determine the association between COPD health outcomes (hospital length of stay, readmission, and home oxygen use) and age, sex, DM, obesity, and other variables.
Results
A total of 630 encounters were identified by ICD codes. After reviewing the EHR by research staff, 91 patients (159 encounters) met the inclusion criteria and were included for data analysis (Figure 1). Only 5 encounters occurred before 2010. A marked increase in the number of encounters was observed in last 10 years with an upward trend.
 |
Figure 1 Selection of patients. |
Table 1 shows characteristics of the 91 patients at the time of their most recent ED or hospital visit. There were more females (64%) than males (36%). Female patients were 5 years younger than male patients (58.7 ± 10.4, 63.5 ± 10.7, p = 0.04). The majority (68%) of patients were overweight or obese. Nearly half of patients had the diagnosis of DM. Most patients had ever smoked. Most patients (96%) had medical comorbidities, with hypertension, obesity, and DM being the most common (Figure 2). Sixty-four patients (70%) had three or more COPD comorbidities. There was no difference in the number of comorbidities by sex (male 3.5 ± 1.9, female 4.1 ± 2.3, p = 0.28).
 |
Table 1 Baseline Characteristics of Patients with COPD Exacerbation (91 Patients) |
 |
Figure 2 COPD comorbidities distribution (91 patients). |
Seventy-six patients had at least one COPD hospitalization; 15 had COPD ED visits only. In univariate analyses, the hospitalized patients were 12 years older than patients with ED-only visit (62.0 ± 9.7, 49.6 ± 9.2 p <0.0001). Neither DM nor obesity was associated with ED-only compared to hospitalized encounters. However, hospitalized patients had more comorbidities than patients who had only ED visits (4.3 ± 2.1, 1.7 ± 0.9, p<0.001).
Among the 76 patients with hospitalization encounters, median length of stay for the more recent encounter was 5 days; 53% of the lengths of stay were between 3 and 9 days. There was no difference in length of stay by sex. Thirty-one (41%) had an ICU stay (age 62 ± 9 years), 19 (25%) were intubated and 27 (36%) required supplemental oxygen use on discharge. Twenty-seven (36%) patients had more than one COPD hospitalization, including 25 patients with COPD rehospitalizations within the previous 2 years. Of these, 9 patients were re-hospitalized for COPD within 30 days. Among these 9 patients, 8 (89%) patients were female, and all 9 had at least 3 comorbidities. Neither DM nor obesity was associated with one versus multiple COPD hospitalizations, or for 30-day readmission. The majority (63%) of hospitalized patients were discharged to home with self-care. Others included long-term acute care, skilled nursing facility, rehabilitation facility or death. A total of 5 patients (4 females, 1 male) died during the hospital stay. All 5 patients presented with first COPD hospitalization at OUMC. Some had other hospitalizations, but those hospitalizations were not related to COPD exacerbations.
Among 76 hospitalized patients, 45 (59%) had Medicare, 21 (28%) had Indian health, and 21 (28%) had Medicaid. Nine patients used Indian health as the single payment source for their hospitalizations. All these 9 patients had only one COPD hospitalization at OUMC, including 6 who received ICU care. Of these, 3 patients required intubation and invasive mechanical ventilatory support.
Linear and Logistic regression were conducted to look for potential association between risk factors and COPD health outcomes (hospital length of stay, 30-day readmission and discharge with supplemental O2) (Tables 2 and Table 3). Only age was associated with oxygen use on discharge. Sex, diabetes, obesity or other comorbidities, history of multiple readmissions, ICU care and invasive mechanical ventilator use were not associated with health outcomes.
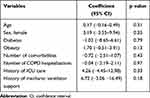 |
Table 2 Linear Regression Analysis for COPD Length of Stay and Clinical Variables |
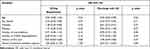 |
Table 3 Logistic Regression Analyses for COPD Health Outcome Variables |
Only 19 of the 91 (21%) individual patients had spirometry reports in our health system. This sample is too small for meaningful analyses.
Discussion
COPD is a common chronic respiratory disease in many NA communities. However, COPD studies among NAs are scarce, and may be hampered by inaccurate data on race.9 Despite efforts to increase the availability and quality of health disparities data collection,10–12 many studies have insufficient sample sizes to describe racial disparities in administrative and EHR data, particularly for NAs.13 Although it is very rare for non-NA patients to be identified as NA, NAs are often reported as other races,14 often leading to undercounts of major diseases.15–17 Indeed, only a few encounters before 2010 were collected in our study. The hospital implemented strategies to help identify NA patients in last 10 years, likely leading to the large increase in numbers of NA COPD patients reported in this study, rather than a marked increase in COPD itself.
In this pilot study, the mean age of 60 years is much younger than the ages reported in prior large COPD studies of hospitalized patients of other races.18,19 There were more female than male patients in the present study. The differences in COPD between women and men are controversial. COPD has been considered to affect mostly older men with a history of smoking. However, a large cohort study showed the risk and annual rate of moderate or severe exacerbations were greater in women than in men.19 Although no association between sex and health outcomes was identified in this small sample size study, notably, female patients were younger than male patients, yet the majority (89%) of patients with 30-day readmissions were women. Although 4 out of 5 deaths were females, the number of deaths is too small for meaningful analysis. These results highlight the unmet need for larger studies to identify the unique risk factors and barriers and develop appropriate intervention programs for younger NA women with COPD.
The prevalence of comorbidities is higher in COPD patients than in the general population.20 In our pilot study, the number of comorbidities in hospitalized patients was higher than in patients who had only an ED visit (4.3 vs 1.7 conditions). Hypertension, obesity, and diabetes were the three most common comorbidities. The larger number of comorbid conditions in hospitalized patients could reflect in part the higher age of the hospitalized patients, as well as the additive risk for COPD exacerbations and worse health outcomes compared to the patients who had an ED visit alone. The sample of patients with ED-only visit was too small for further analyses by age or sex.
Forty-three percent of our patients were obese, which is higher than reported for other races in a COPD epidemiology study.21 Thirty-eight percent of the patients had DM, a much higher proportion than reported for non-Hispanic White and African American COPD patients in a prior study.22 However, given our small NA sample size, we could not further explore the association between obesity, DM, and COPD outcomes. Large studies are needed to further elucidate the relationship in NA population.
Needing ICU care and intubation are serious events for COPD patients. Our pilot study showed 41% of the hospitalized patients had ICU care, and 25% were intubated in last hospitalization. These are much higher than reported in other studies.23,24 One study that enrolled 354 hospitalized COPD patients reported 23 (6.5%) of patients required critical care and 6 (1.7%) patients were intubated after admission.23 A study that enrolled 305 ICU patients with COPD exacerbations revealed the patient mean age was 67.4 years.25 Our patients who had ICU care were much younger.
While further research is needed to look for the risk factors of the poor health outcomes in NA populations, some patients in our study may have been referred from Indian health care facilities for a higher level of care due to the severity of their illness. The Indian Health Service (IHS) is funded by the federal government to deliver health care to NAs and also provides funds for tribal and urban Indian health programs to administer their own healthcare facilities.26 When the health services cannot be provided in its own facilities, IHS as well as tribal and urban programs must refer patients to outside health facilities such as the OUMC. In our study, 21% of the patients used IHS to cover the healthcare cost. Nine patients had IHS as the only payment source. All of these patients had only one COPD hospitalization in our institution, and 6 had a poor health outcome (ICU care, intubation, or death). The availability of specialty pulmonary care and services such as spirometry and pulmonary rehabilitation is beyond the means of many, if not most, Indian health care programs. While details regarding outpatient management and control of COPD are beyond the scope of this study, the poor outcomes raise the concern of financial and health access issues. Additional federal assistance may be needed to improve NA community respiratory healthcare to prevent severe COPD exacerbations and death.
Spirometry is an important tool for COPD diagnosis and severity evaluation. Our study revealed that few of the NA COPD patients had spirometry data available in our system. While most patients were discharged home with self-care, sicker patients who needed supplemental oxygen or were discharged to other health facilities did not have spirometry data available. Such data would be of use for outpatient management of COPD, but formal spirometry is often unattainable in the hospital setting. Further, the proportion of NA respiratory patients who have ever had spirometric testing is unknown in general.
This study has some limitations. It is an exploratory study with small sample size, and is subject to the known limitations of chart review, including incomplete case ascertainment and lack of systematically applied definitions of disease and comorbidities. OUMC is a tertiary transfer center. Less sick patients may be treated in community hospitals in rural areas. Findings cannot be generalized to the population of NA adults in the state or US. However, very few studies of COPD among NA populations exist, and this study provides preliminary data as the basis for future larger research. Race was determined by EHR demographic documentation. Racial misclassification is a particular problem for many NA studies that rely on administrative data,27–29 and our data may not have identified all NA COPD patients. The diagnosis of COPD exacerbation in this study was based on physician documentation and coding. Only a small portion of the participants had available spirometry data, which are required for accurate diagnosis of COPD.1 Indeed, misdiagnosis is common in clinic-based studies of COPD.30 OUMC serves as a tertiary care facility for much of the state, including for patients too ill to be cared for at community hospitals, or Indian Health Service and Tribal health facilities. This likely skewed the NA COPD patient population toward more severe disease. Some outcomes, such as death and 30-day readmission, occurred too infrequently for meaningful analysis. The usage of COPD medications at home was not available in EHR for older encounters. Again, larger studies are needed to clarify the risk factors and barriers of poor COPD health outcomes.
Conclusions
COPD is a common chronic respiratory disease among NAs. Hospitalized NA COPD patients had multiple comorbidities, especially hypertension, diabetes, and obesity. Many required ICU care and intubation. More younger women were affected with severe outcomes, which was unexpected. Along with strategies to improve health disparities data collection, clinical research using large samples of NA COPD patients is needed to better understand the risk factors for poor COPD health outcomes. Such information would be useful for NA health systems to develop implementation plan to mitigate poor COPD outcomes for NA communities.
Acknowledgments
The authors thank Carla Guy, Jarrod Harper, Kelsi Williams and James Webb for medical record review and data audit. The abstract of this paper was presented at the American Thoracic Society International Conference as a poster presentation with interim findings. The poster’s abstract was published in American Journal of Respiratory and Critical Care Medicine: https://www.atsjournals.org/doi/abs/10.1164/ajrccm-conference.2020.201.1_MeetingAbstracts.A5051.
Funding
Research reported in this publication was supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number U54GM104938. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Global Intiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease report; 2020. Available from: https://goldcopd.org/wp-content/uploads/2019/12/GOLD-2020-FINAL-ver1.2-03Dec19_WMV.pdf.
2. Ford ES, Croft JB, Mannino DM, Wheaton AG, Zhang X, Giles WH. COPD surveillance–United States, 1999–2011. Chest. 2013;144(1):284–305. doi:10.1378/chest.13-0809
3. Vanfleteren L, Spruit MA, Wouters EFM, Franssen FME. Management of chronic obstructive pulmonary disease beyond the lungs. Lancet Respir Med. 2016;4(11):911–924. doi:10.1016/S2213-2600(16)00097-7
4. Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: summary of national findings. Available from: https://www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013.pdf.
5. Jernigan VB, Duran B, Ahn D, Winkleby M. Changing patterns in health behaviors and risk factors related to cardiovascular disease among American Indians and Alaska Natives. Am J Public Health. 2010;100(4):677–683. doi:10.2105/AJPH.2009.164285
6. Subica AM, Agarwal N, Sullivan JG, Link BG. Obesity and associated health disparities among understudied multiracial, pacific islander, and American Indian adults. Obesity (Silver Spring). 2017;25(12):2128–2136. doi:10.1002/oby.21954
7. Centers for Disease Control and Prevention. Chronic disease indicators (COPD). Available from: https://www.cdc.gov/cdi/.
8. Centers for Disease Control and Prevention. Tribal population. Available from: https://www.cdc.gov/tribal/tribes-organizations-health/tribes/state-population.html.
9. Bierman AS, Lurie N, Collins KS, Eisenberg JM. Addressing racial and ethnic barriers to effective health care: the need for better data. Health Aff (Millwood). 2002;21(3):91–102. doi:10.1377/hlthaff.21.3.91
10. Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press; 2003.
11. ACT, Affordable Care, and US House of Representatives. Patient Protection and Affordable Care Act, 42 U.S.C. § 18001; 2010. Available from: https://www.hhs.gov/sites/default/files/ppacacon.pdf.
12. Department of Health and Human Services. HHS action plan to reduce racial and ethnic health disparities: a nation free of disparities in health and health care. Available from: https://www.minorityhealth.hhs.gov/npa/files/Plans/HHS/HHS_Plan_complete.pdf.
13. Liebler CA. Counting America’s First Peoples. Ann Am Acad Pol Soc Sci. 2018;677(1):180–190. doi:10.1177/0002716218766276
14. Dougherty TM, Janitz AE, Williams MB, et al. Racial misclassification in mortality records among American Indians/Alaska natives in Oklahoma from 1991 to 2015. J Public Health Manag Pract. 2019;25(Suppl 5):S36–S43. doi:10.1097/PHH.0000000000001019
15. Espey DK, Jim MA, Richards TB, Begay C, Haverkamp D, Roberts D. Methods for improving the quality and completeness of mortality data for American Indians and Alaska Natives. Am J Public Health. 2014;104(Suppl S3):S286–S294. doi:10.2105/AJPH.2013.301716
16. Creswell PD, Strickland R, Stephenson L, et al. Look local: the value of cancer surveillance and reporting by American Indian clinics. Prev Chronic Dis. 2013;10:E197. doi:10.5888/pcd10.130153
17. Rhoades DA. Racial misclassification and disparities in cardiovascular disease among American Indians and Alaska Natives. Circulation. 2005;111(10):1250–1256. doi:10.1161/01.CIR.0000157735.25005.3F
18. Gonzalez AV, Suissa S, Ernst P. Gender differences in survival following hospitalisation for COPD. Thorax. 2011;66(1):38–42. doi:10.1136/thx.2010.141978
19. Stolz D, Kostikas K, Loefroth E, et al. Differences in COPD exacerbation risk between women and men: analysis from the UK clinical practice research datalink data. Chest. 2019;156(4):674–684. doi:10.1016/j.chest.2019.04.107
20. Holguin F, Folch E, Redd SC, Mannino DM. Comorbidity and mortality in COPD-related hospitalizations in the United States, 1979 to 2001. Chest. 2005;128(4):2005–2011. doi:10.1378/chest.128.4.2005
21. Lambert AA, Putcha N, Drummond MB, et al. Obesity is associated with increased morbidity in moderate to severe COPD. Chest. 2017;151(1):68–77.
22. Kinney GL, Black-Shinn JL, Wan ES, et al. Pulmonary function reduction in diabetes with and without chronic obstructive pulmonary disease. Diabetes Care. 2014;37(2):389–395. doi:10.2337/dc13-1435
23. Stiell IG, Clement CM, Aaron SD, et al. Clinical characteristics associated with adverse events in patients with exacerbation of chronic obstructive pulmonary disease: a prospective cohort study. CMAJ. 2014;186(6):E193–E204. doi:10.1503/cmaj.130968
24. Matkovic Z, Huerta A, Soler N, et al. Predictors of adverse outcome in patients hospitalised for exacerbation of chronic obstructive pulmonary disease. Respiration. 2012;84(1):17–26. doi:10.1159/000335467
25. Brown H, Dodic S, Goh SS, et al. Factors associated with hospital mortality in critically ill patients with exacerbation of COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:2361–2366. doi:10.2147/COPD.S168983
26. Health coverage for American Indians & Alaska Natives. Available from: https://www.healthcare.gov/american-indians-alaska-natives/.
27. Joshi S, Warren-Mears V. Identification of American Indians and Alaska Natives in public health data sets: a comparison using linkage-corrected Washington State death certificates. J Public Health Manag Pract. 2019;25(Suppl 5):S48–S53. doi:10.1097/PHH.0000000000000998
28. Grafova IB, Jarrín OF. Beyond black and white: mapping misclassification of medicare beneficiaries race and ethnicity. Med Care Res Rev. 2020;107755872093573. doi:10.1177/1077558720935733
29. Jarrín OF, Nyandege AN, Grafova IB, Dong X, Lin H. Validity of race and ethnicity codes in medicare administrative data compared with gold-standard self-reported race collected during routine home health care visits. Med Care. 2020;58(1):e1–e8. doi:10.1097/MLR.0000000000001216
30. Wu H, Wise RA, Medinger AE. Do patients hospitalized with COPD have airflow obstruction? Chest. 2017;151(6):1263–1271. doi:10.1016/j.chest.2017.01.003
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
