Back to Journals » The Application of Clinical Genetics » Volume 14
NAT2 Gene rs1041983 is Associated with Anti-Tuberculosis Drug Induced Hepatotoxicity Among Pediatric Tuberculosis in Bandung, Indonesia
Authors Headriawan A, Pramono AA , Sukadi A, Chairulfatah A, Maskoen AM, Nataprawira HM
Received 11 February 2021
Accepted for publication 23 April 2021
Published 3 June 2021 Volume 2021:14 Pages 297—303
DOI https://doi.org/10.2147/TACG.S303668
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Martin Maurer
Achmad Headriawan,1 Alvinsyah Adhityo Pramono,2 Abdurachman Sukadi,1 Alex Chairulfatah,1 Ani Melani Maskoen,2,3 Heda Melinda Nataprawira1
1Department of Child Health; 2Research Center of Medical Genetics; 3Department of Biomedical Sciences, Faculty of Medicine, Universitas Padjadjaran/Dr. Hasan Sadikin General Hospital, Bandung, Indonesia
Correspondence: Heda Melinda Nataprawira
Department of Child Health, Faculty of Medicine, Universitas Padjadjaran/Dr. Hasan Sadikin General Hospital, Jl. Pasteur No. 38, Bandung, 40161, Indonesia
Tel +62811229294
Email [email protected]
Background: As pediatric tuberculosis (TB) globally is still reported challenging in diagnosis, to date, a lot of efforts have been established to eliminate the disease including proper treatment regimen using anti-TB drugs. However, antituberculosis drug-induced hepatotoxicity (ADIH) is known to interfere the success of the prescribed therapy. ADIH was found to be correlated with polymorphisms of NAT2 gene, that is responsible to transcript the NAT2 enzyme, a metabolizer of isoniazid (INH). The most common NAT2 gene polymorphisms in Asian population associated with ADIH are rs1041983, rs1799929, rs1799930 and rs1799931. The study aimed to investigate the 4 single nucleotide polymorphisms (SNPs) in pediatric TB that experienced ADIH.
Methods: We conducted a case–control study comparing 31 each of pediatric TB experience with and without ADIH. All pediatric TB was selected from 451 pediatric TB Registry of Respirology Division, Department of Child Health Faculty of Medicine Universitas Padjadjaran/Dr Hasan Sadikin Hospital during January 2016 to July 2018. Genomic DNA PCR and sequencing to identify polymorphisms of rs1041983, rs1799929, rs1799930 and rs1799931 were performed in both groups. Data analysis was performed using the Epi info Ver. 7 software.
Results: Thirty-one pediatric TB experiences with and without ADIH were enrolled in this study. SNP rs1041983 significantly affected the occurrence of ADIH (OR 2.39, CI 95% (1.15– 4.96), p=0.019). The rs1799929, rs1799930 and rs1799931 did not significantly affect the occurrence of ADIH (p=0.133, p=0.150 and p=0.659, respectively).
Conclusion: Polymorphism SNP rs1041983 had association with the occurrence of ADIH.
Keywords: NAT2 polymorphism, ADIH, children
Introduction
Tuberculosis (TB) remains a major public health problem in the world.1–3 There are approximately 10 million cases of TB every year, of which pediatric TB accounted for 7.1% of the global cases.3 Administration of anti-TB treatment may cause antituberculosis drug-induced hepatitis (ADIH) that is known as the most common adverse event.4–6 ADIH is caused by INH metabolism impairment as a consequence of NAT2 gene polymorphisms. NAT2 gene encodes arylamine N-acetyltransferase enzyme that consists of 254 to 332 amino acid variation that creates different phenotypes of isoniazid metabolizing capacity.7,8 Rapid NAT2 acetylators will be at risk of treatment failure due to rapid metabolism of INH, however slow NAT2 acetylators may develop ADIH as a result of highly circulated INH.(Figure 1)8
 |
Figure 1 Pediatric TB inclusion process. |
Several countries have conducted studies regarding NAT2 enzyme activities; however, these studies were limited to adult TB patients.1,9–13 A study in Thailand reported alterations in rs1041983, rs1799929, rs1799930 and rs1799931 in TB patients with ADIH.1 Other study discovered polymorphisms in rs1041983, rs1208, rs1801280 in 1–15 year old TB patients with ADIH.8 Some studies found that rs1041983, rs1799929, rs1799930, rs1799931 were the most common single nucleotide polymorphisms (SNPs) among Asian population.1,11,12,14 A study in Indonesia reported that 22.9% and 77.1% of adult TB patients were found to be rapid and slow acetylators of NAT2 gene, respectively.9 Previous retrospective study in pediatric TB patients in Hasan Sadikin Hospital, Indonesia found that 3.5% of pediatric TB developed ADIH.15 The study aimed to investigate the 4 single nucleotide polymorphisms (SNPs) in pediatric TB that experienced ADIH in Bandung, Indonesia.
Methods
Study Design
This is an observational case control study exploring the case of ADIH in pediatric TB patients documented in the TB Registry of Respirology Division, Department of Child Health, Universitas Padjadjaran/Hasan Sadikin Hospital, Bandung from January 2016 to July 2018.
Study Subjects
Pediatric pulmonary or extrapulmonary TB confirmed by clinical, laboratory, microbiology and molecular rapid test, and treated using pediatric anti-TB regiment between 2016 to 2018 were included in the study. Pediatric pulmonary TB is TB infection location in the lung. Extrapulmonary TB is TB within a location in the body other than lungs. Pediatric TB developing ADIH during treatment period were grouped into the case group, while non-ADIH pediatric TB were classified as the control group. However, Pediatric TB who showed evidence of acute viral hepatitis and its carriers, hepatic cirrhosis, drug induced hepatitis caused by other drugs, sepsis, elevated liver enzyme or total bilirubin serum level prior to anti-TB administration were excluded from the study.
Confirmed cases of pediatric pulmonary and extrapulmonary TB were treated according to the International Standards for Tuberculosis Care, Edition 3.2 Treatment of pediatric pulmonary TB were divided into two consecutive phases, namely initial and continuation phases. The initial phase lasted for two months, consisted of isoniazid 10 (7–15) mg/kgBW; rifampicin 15 (10–20) mg/kgBW; and pyrazinamide 35 (30–40) mg/kgBW given on a daily basis. Pediatric TB with positive evidence of Mycobacterium tuberculosis, destroyed lung TB, extrapulmonary TB, miliary TB, and meningitis TB received an additional drug regimen of ethambutol 20 (15–25) mg/kgBW for the initial phase. The continuation phase consisted of isoniazid 10 (7–15) mg/kgBW and rifampicin 15 (10–20) mg/kgBW for 4 months. The continuation phase for tuberculous osteomyelitis, miliary TB, and meningitis TB lasted for 10 months.2
Diagnosis of ADIH was established based on clinical and laboratory presentations, including the presence of jaundice and/or raised serum total bilirubin level (> 1.5 mg/dL) and/or 3-5-fold rise of serum alanine aminotransferase (ALT) above normal levels in patients receiving anti-TB treatment. In order to achieve the minimum clinically significant result, at least 31 subjects must be enrolled in both ADIH and non-ADIH groups.
All subjects underwent blood collection for DNA extraction and genotyping test. The study protocol was approved by the Medical Ethics Committee of Hasan Sadikin Hospital number LB.04.01/A05/EC/158/V/2018. Prior to the study, all parents of the study subjects were given adequate information about the study and asked for the consent to participate in the study.
DNA Extraction and Genotyping
Five mL of venous blood was extracted in EDTA tube and stored in 4°C refrigerator for 4 days. Extracted DNA was analyzed and quantitatively determined according to the manufacturer’s protocol (Davis RW, 1980; Buffone GS, 1985. Pharmacia DNA genomic kit). Isolated DNA was amplified using the forward primer 5ʹ – GGG ATC ATG GAC ATT GAA GC – 3ʹ and reverse primer 5ʹ – GGG TGA TAC ATA CAC AAG GGT TTA – 3ʹ.16 One sample of polymerase chain reaction (PCR) consists of premixed solution containing 21 µL master mix solution (produsen, cat no.8), 19 µL deiodination water, 1 µL forward primer, 1 µL reverse primer and 2 µL DNA from the patients. PCR process was done in the following sequence: denaturation (94°C, 3 minutes), denaturation (94°C, 3 minutes per cycle), annealing (58°C, 30 seconds per cycle), extension (72°C 30 seconds per cycle) and final extension (72°C, 7 minutes). Denaturation, annealing and extension phase were repeated for 35 cycles. PCR products were then embedded in 1% agarose 1% gel with 90V power for 30 minutes for electrophoresis reaction. Amplified NAT2 gene samples were further sequenced (First Base, Singapore).
Identification of 4 SNPs of NAT2 namely rs1041983, rs1799929, rs1799930 and rs1799931 was based on the Arylamine-acetyltransferase Gene Nomenclature Committee (http/asia.ensembl.org/Homo_sapiens/Gene/Sequence?db=core;g=ENSG00000156006;r=8:18391245–18401218) accessed in August 2018. NAT2 gene sequence was analyzed using BioEdit sequence alignment editor.
Data Analysis
Data analysis was performed using Epi Info™ 7 (Epi Info™, Division of Health Informatics & Surveillance (DHIS), Center for Surveillance, Epidemiology & Laboratory Services (CSELS)). Aspartate aminotransferase (AST), ALT, bilirubin total and direct were calculated as median (range). Characteristics of data was presented as percentage ± standard deviation. Each of the SNPs allele and genotype in both groups were analyzed for Hardy-Weinberg equilibrium (HWE) using chi-square test.
Results
Study Population Characteristics
There were 451 pediatric TB registered in the Respiratory Division, Department of Child Health, Universitas Padjadjaran/Hasan Sadikin Hospital during January 2016 to July 2018. There were 384 cases of pulmonary TB and 67 cases of extrapulmonary TB cases. Diagnosis was established on the basis of clinical presentations and at least one of the supporting diagnostics tools, including radiology/imaging test (419 cases), gastric lavage culture (22 cases), and molecular diagnostics test (10 cases).
Among all registered pediatric TB, there were 100 subjects developing ADIH during the treatment period. However, 69 pediatric TB ADIH were excluded due to incomplete data, death, and refusal to participate in the study (Figure 1). Pediatric TB without ADIH were randomly selected from the same registry and categorized as the control group. Demographic presentations of all subjects are shown in Table 1. All pediatric TB with or without ADIH were of Sundanese population.
 |
Table 1 Characteristic of ADIH and without ADIH Pediatrics TB |
Most cases of ADIH and non-ADIH were found to be extrapulmonary TB which accounted of 58% and 68% of pediatric TB in Hasan Sadikin Hospital, respectively. Liver enzymes increased as high as 50-fold in some ADIH pediatric TB with respect to the non-ADIH group.
Association Analysis of Each Allele and Genotype
Allele distribution of the SNPs studied and their association on the NAT2 gene are shown in Table 2. SNP rs1799929 C>T was not significantly associated with the occurrence of ADIH (OR 2.24 95% CI (0.78–6.41), p=0.133). Both SNPs rs1799930 and rs1799931 have risk allele A, however they were not significantly associated with ADIH (OR 1.69 95% CI (0.83–3.45), p=0.150; and OR 1.22 95% CI (0.51–2.89), p=0.659, respectively). The SNP rs1041983 C>T was significantly associated with ADIH (OR 2.39 95% CI (1.15–4.96), p=0.019).
 |
Table 2 Allelic Frequency Allele of ADIH and without ADIH |
Table 3 shows that the genotype C/T and T/T on rs1041983 were significantly associated with ADIH, p= 0.093. SNPs rs1799929, rs1799930 and rs1799931 were not associated with ADIH in both groups (p=0.203, p=0.311, p=0.866, respectively).
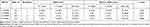 |
Table 3 SNPs-Based Genotype Association Tests in ADIH and without ADIH |
Discussions
This study linked the genetic polymorphisms of NAT2 gene to the occurrence of ADIH in pediatric TB patients in Bandung, West Java, Indonesia. We conducted a case–control study involving 31 ADIH and 31 non-ADIH Sundanese pediatric TB.
Our study is in line with a study in Argentina which reported that 40% of adult female TB patients developed anti-tuberculosis drug hepatotoxicity (ATDH).17 54.5% of adult Brazilian TB patients developing ADIH were found to have comorbid factors such as tobacco smoking, alcohol abuse, HIV and other medication that impairs liver functions.18 Both studies marked the limitation of our study did not register comorbid factors of ADIH.
Unfortunately, the occurrence of ADIH in hospitalized TB pediatric patients in tertiary care hospital did not show significant different among genders.1,12,15,19 Our study showed that 65% subjects in ADIH group were female. Several studies revealed that ADIH occurred in adult pulmonary TB patient in Argentina and Singapore which were accounted for 70% and 70.8%, respectively.11,17 Our study showed that ADIH mostly occurred in pediatric extrapulmonary TB.
NAT2 gene is responsible for INH metabolism. The impairment of NAT2 enzyme activity affects the detoxification process of INH.20 Alterations of NAT2 enzyme activity exhibited polymorphism.4 The most common SNPs associated with ADIH in Asian population were rs1041983, rs1799929, rs1799930 and rs1799931.1,11,13,14 Our study found that SNP rs1041983 C>T was strongly associated with ADIH (OR 2.39, 95% CI (1.15–4.96), p=0.019, as shown in Table 2). This is in line with Gupta et al who found that rs1041983 of NAT2 gene had a higher risk in developing ATDH.19 In Caucasian population, rs1041983 significantly increased risk of ADIH.13
Our study mentioned that the other SNPs rs1799929, rs1799930 and rs1799931 were not significantly associated with ADIH. We successfully confirmed the NAT2 polymorphisms study in Chinese population reporting that rs1799929, rs1799930 and rs1799931 were not significantly associated to ADIH.12 Taiwanese genotyping for NAT2 showed that rs1495741 was the most numerous heterozygote mutation among the 8 SNPs examined.21
Analysis of SNP based genotype association in both groups revealed that the genotype TT in rs1041983 was significantly associated with ADIH (p=0.093, as shown in Table 3). Our result is consistently similar with previous studies in Singapore, Vietnam, Thailand and Japan in adult TB population.1,11,13,22,23 It was known that rs1041983 was associated with increased risk of hepatotoxicity.24
Limitation of Study
Our study did not stratify risks other than NAT2 gene polymorphisms, such as smoking, alcohol abuse, etc. into the analysis. Liver function tests were limited for ALT, AST, and bilirubin as the regular protocol for hepatotoxicity in our hospital. Alkaline phosphatase was not examined due to limited funds. We strongly recommend to continue this study by conducting genetic function study to reveal the exact mechanism and interaction between NAT2 gene, its polymorphisms, and ADIH in TB patients.
Conclusion
Rs1041983 was associated with ADIH in pediatric TB treated with anti-TB drug regimen.
Data Sharing Statement
The software of Bioedit analyzed during the current study is available at https://bioedit.software.informer.com/7.2/ The datasets analyzed during the current study is available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The study was approved in accordance to the requirement of the Ethics Committee Hasan Sadikin Hospital. Written informed consent was obtained from parents of participants in compliance with the Declaration of Helsinki.
Acknowledgment
The authors appreciate the assistance of Fensi Amalina and Erlina Widiarsih from Molecular and Genetic Laboratory Faculty of Medicine Universitas Padjadjaran. We are grateful to participants who participated to this study.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
Funding was provided by Academic Leaderships Grant Program of Universitas Padjadjaran. The funders were not involved in the data analysis or manuscript preparation.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Wattanapokayakit S, Mushiroda T, Yanai H, et al. NAT2 slow acetylator associated with anti-tuberculosis drug-induced liver injury in Thai patients. Int J Tuberc Lung Dis. 2016;20(10):1364–1369. doi:10.5588/ijtld.15.0310
2. TB CARE I. International Standards for Tuberculosis Care.
3. World Health Organization. Global tuberculosis report 2018. Geneva: World Health Organization; 2018.
4. Donald PR. Antituberculosis drug-induced hepatotoxicity in children. Pediatr Rep. 2011;3(2):e16. doi:10.4081/pr.2011.e16
5. Saukkonen JJ, Cohn DL, Jasmer RM, et al. An official ATS statement: hepatotoxicity of antituberculosis therapy. Am J Respir Crit Care Med. 2006;174(8):935–952. doi:10.1164/rccm.200510-1666ST
6. Tostmann A, Boeree MJ, Aarnoutse RE, de Lange WC, van der Ven AJ, Dekhuijzen R. Antituberculosis drug-induced hepatotoxicity: concise up-to-date review. J Gastroenterol Hepatol. 2008;23(2):192–202. doi:10.1111/j.1440-1746.2007.05207.x
7. Butcher NJ, Boukouvala S, Sim E, Minchin RF. Pharmacogenetics of the arylamine N-acetyltransferases. Pharmacogenomics J. 2002;2(1):30–42. doi:10.1038/sj.tpj.6500053
8. Verhagen LM, Coenen MJ, López D, et al. Full-gene sequencing analysis of NAT2 and its relationship with isoniazid pharmacokinetics in Venezuelan children with tuberculosis. Pharmacogenomics. 2014;15(3):285–296. doi:10.2217/pgs.13.230
9. Artini IGA, Artana IGNB. Acetylator status on tuberculosis patients receiving isoniazid-contained antituberculosis regiment. Int J Sci Res. 2017;6(7):586–588.
10. Azuma J, Ohno M, Kubota R, et al. NAT2 genotype guided regimen reduces isoniazid-induced liver injury and early treatment failure in the 6-month four-drug standard treatment of tuberculosis: a randomized controlled trial for pharmacogenetics-based therapy. Eur J Clin Pharmacol. 2013;69(5):1091–1101. doi:10.1007/s00228-012-1429-9
11. Chan SL, Chua APG, Aminkeng F, et al. Association and clinical utility of NAT2 in the prediction of isoniazid-induced liver injury in Singaporean patients. PLoS One. 2017;12(10):e0186200. doi:10.1371/journal.pone.0186200
12. Lv X, Tang S, Xia Y, et al. NAT2 genetic polymorphisms and anti-tuberculosis drug-induced hepatotoxicity in Chinese community population. Ann Hepatol. 2012;11(5):700–707. doi:10.1016/S1665-2681(19)31446-2
13. Leiro-Fernandez V, Valverde D, Vázquez-Gallardo R, et al. N-acetyltransferase 2 polymorphisms and risk of anti-tuberculosis drug-induced hepatotoxicity in Caucasians. Int J Tuberc Lung Dis. 2011;15(10):1403–1408. doi:10.5588/ijtld.10.0648
14. Soejima M, Sugiura T, Kawaguchi Y, et al. Association of the diplotype configuration at the N-acetyltransferase 2 gene with adverse events with co-trimoxazole in Japanese patients with systemic lupus erythematosus. Arthritis Res Ther. 2007;9(2):R23. doi:10.1186/ar2134
15. Nataprawira HM, Hannah RA, Kartika HH. Hospitalized pediatric antituberculosis drug induced hepatotoxicity: experience of an Indonesian referral hospital. Asian Pac J Trop Dis. 2017;7(5):276–279. doi:10.12980/apjtd.7.2017D6-402
16. Pramono AA, Penggoam S, Sahiratmadja E, Utami NV, Achmad TH, Panigoro R. Status Asetilator Gen NAT2 pada Pasien Tuberkulosis dan Tuberkulosis dengan Diabetes Melitus di Kupang, Nusa Tenggara Timur [NAT2 Gene Acetylator Status of Tuberculosis and Tuberculosis with Diabetes Mellitus Patients in Kupang, Nusa Tenggara Timur]. Majalah Kedokteran Bandung. 2017;49(1):61–66. Indonesian. doi:10.15395/mkb.v49n1.989
17. Chamorro JG, Castagnino JP, Musella RM, et al. Sex, ethnicity, and slow acetylator profile are the major causes of hepatotoxicity induced by antituberculosis drugs. J Gastroenterol Hepatol. 2013;28(2):323–328. doi:10.1111/jgh.12069
18. Santos NP, Callegari-Jacques SM, Ribeiro dos santos AK, et al. N-acetyl transferase 2 and cytochrome P450 2E1 genes and isoniazid-induced hepatotoxicity in Brazilian patients. Int J Tuberc Lung Dis. 2013;17(4):499–504. doi:10.5588/ijtld.12.0645
19. Gupta VH, Amarapurkar DN, Singh M, et al. Association of N-acetyltransferase 2 and cytochrome P450 2E1 gene polymorphisms with antituberculosis drug-induced hepatotoxicity in Western India. J Gastroenterol Hepatol. 2013;28(8):1368–1374. doi:10.1111/jgh.12194
20. Huang YS. Recent progress in genetic variation and risk of antituberculosis drug-induced liver injury. J Chin Med Assoc. 2014;77(4):169–173. doi:10.1016/j.jcma.2014.01.010
21. Ho HT, Wang TH, Hsiong CH, et al. The NAT2 tag SNP rs1495741 correlates with the susceptibility of antituberculosis drug-induced hepatotoxicity. Pharmacogenet Genomics. 2013;23(4):200–207. doi:10.1097/FPC.0b013e32835e95e1
22. Cavaco I, Asimus S, Peyrard-Janvid M, et al. The Vietnamese Khin population harbors particular N-acetyltransferase 2 allele frequencies. Clin Chem. 2007;53(11):1977–1979. doi:10.1373/clinchem.2007.092684
23. Higuchi N, Tahara N, Yanagihara K, et al. NAT2 6A, a haplotype of the N-acetyltransferase 2 gene, is an important biomarker for risk of anti-tuberculosis drug-induced hepatotoxicity in Japanese patients with tuberculosis. World J Gastroenterol. 2007;13(45):6003–6008. doi:10.3748/wjg.v13.45.6003
24. Ben Mahmoud L, Ghozzi H, Kamoun A, et al. Polymorphism of the N-acetyltransferase 2 gene as a susceptibility risk factor for antituberculosis drug-induced hepatotoxicity in Tunisian patients with tuberculosis. Pathol Biol. 2012;60(5):324–330. doi:10.1016/j.patbio.2011.07.001
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
