Back to Journals » Medical Devices: Evidence and Research » Volume 12
NASHA hyaluronic acid for the treatment of shoulder osteoarthritis: a prospective, single-arm clinical trial
Authors McKee MD, Litchfield R, Hall JA, Wester T, Jones J, Harrison AJ
Received 2 October 2018
Accepted for publication 14 March 2019
Published 12 June 2019 Volume 2019:12 Pages 227—234
DOI https://doi.org/10.2147/MDER.S189522
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Michael D McKee,1 Robert Litchfield,2 Jeremy A Hall,3 Tawana Wester,4 John Jones,4 Andrew J Harrison5
1Department of Orthopaedic Surgery, University of Arizona College of Medicine, Phoenix, AZ, USA; 2Department of Surgery, Fowler Kennedy Sport Medicine Clinical, London, ON, Canada; 3Department of Surgery, St Michael’s Hospital, Toronto, ON, Canada; 4Research and Development, Bioventus LLC, Durham, NC 27703, USA; 5Research and Development, Bioventus Cooperatief UA, Hoofddorp, Netherlands
Background: Osteoarthritis of the shoulder or glenohumeral joint is a painful condition that can be debilitating. Intra-articular injection with hyaluronic acid should be considered for patients not responding adequately to physical therapy or anti-inflammatory medication.
Methods: This was a single-arm, open-label, prospective study of a single intra-articular injection of NASHA (non-animal hyaluronic acid) in patients with symptomatic glenohumeral osteoarthritis. Patients were followed up for 26 weeks post-treatment, during which time rescue medication with acetaminophen was permissible. The study objective was to demonstrate that a single injection of NASHA is well tolerated with an over-6-month 25% reduction in shoulder pain on movement, assessed using a 100-mm visual analog scale.
Results: Forty-one patients were enrolled, all of whom received study treatment. The mean decrease in shoulder pain on movement score over the 6-month study period was −20.1 mm (95% CI: −25.2, −15.0 mm), corresponding to a mean reduction of 29.5% (22.0, 37.0%). Statistically significant improvements were also observed in shoulder pain at night and patient global assessment. There was no clear change over time in the percentage of patients using rescue medication and mean weekly doses were below 3500 mg. Seventeen patients (41.5%) experienced adverse events, all of which were mild or moderate. Two adverse events (both shoulder pain) were deemed related to study treatment.
Conclusion: This study provides preliminary evidence that a single injection of NASHA may be efficacious over 6 months and well tolerated in patients with symptomatic glenohumeral osteoarthritis. Larger studies are needed for confirmation.
Keywords: Durolane®, glenohumeral joint, non-animal hyaluronic acid, osteoarthritis, shoulder, viscosupplementation
Background
In the normal shoulder or glenohumeral (GH) joint, smooth motion is facilitated by cartilage, which surrounds the articular portion of the bones, and hyaluronic acid within the synovial fluid. With age and normal wear and tear, cartilage degenerates and osteoarthritis (OA) can develop. The prevalence of GH-OA has not been studied extensively, but it is known to increase with age and has been estimated broadly as 4–26%.1 The features of GH-OA may include joint effusion, stiffness that improves with re st, crepitus, decreased range of motion, joint space narrowing, subchondral sclerosis and osteophyte formation.2
Some GH-OA patients not responding adequately to physical therapy or anti-inflammatory medication may not wish to progress directly to surgery or there may be clinical reasons for avoiding surgery. Under such circumstances, the patient has the option of intra-articular injection with either a corticosteroid or hyaluronic acid (HA). Numerous studies have reported that intra-articular HA injection is well tolerated and can provide statistically significant reductions in pain.3–10 NASHA (non-animal hyaluronic acid) is a biocompatible HA with a prolonged intra-articular residence time that been used as a treatment for knee and hip OA since 2001.11–16 In 2010, the approved indications for NASHA in the EU were expanded to include pain relief associated with OA in joints of all sizes except for the temporomandibular and facet joints.17
This study was performed to evaluate the efficacy, safety and tolerability of a single intra-articular injection of NASHA for the relief of pain over 26 weeks in patients with symptomatic GH-OA.
Methods
This single-arm, open-label study (Clinicaltrials.gov identifier NCT02610504) was performed prospectively at two outpatient clinics in Canada. Approval was obtained from St Michael’s Hospital Research Ethics Board (reference number 14–325) before the study commenced and, because GH-OA was not an approved indication for NASHA in Canada at the time of the study, authorization from Health Canada was required. All patients provided signed informed consent before undergoing study procedures. The principles of Good Clinical Practice and the Declaration of Helsinki were adhered to throughout. As far as possible, this study was conducted in accordance with the Consolidated Standards of Reporting Trials (CONSORT) guidelines.18
Adults aged 19–85 years with a body mass index ≤35 kg/m2, and symptomatic GH-OA and radiographic evidence of disease were eligible for inclusion in the study. Radiographic examinations were performed by a radiologist and reviewed by the relevant surgeon. The Kellgren–Lawrence grading system was applied, and individuals with mild to moderate disease (Kellgren–Lawrence grade 2–3) were selected for inclusion. At screening, pain was assessed using the “shoulder pain on movement” (SPOM) visual analog scale (VAS), with a range from zero (no pain) to 100 mm (severe pain), and a score ≥50 mm was required for study participation. In addition, patients had to have experienced pain on at least 50% of the days during the previous month. All study participants had failed conventional therapy (non-steroidal anti-inflammatory drugs; one or more intra-articular or peri-articular steroid injection; and ≥1 month of physiotherapy) and, for the duration of the study (including the week before administration of study treatment), had to agree to cessation of analgesic treatment apart from acetaminophen which was permitted as rescue medication (except during the 24 hrs preceding each study visit). Intra-articular or peri-articular injections apart from the study intervention were also not permitted during the study period. OA in the contralateral shoulder was permissible provided that OA symptoms were greater in the study shoulder. Exclusion criteria included significant pain from other joints or low back pain requiring chronic analgesic therapy, the presence of any condition that could have confounded the assessment of pain/disability in the study shoulder, and pathologies other than OA in the study shoulder (range of motion <30% in any direction; clinically apparent tense effusion, gross misalignment or instability, acute fracture, severe loss of bone density, avascular necrosis or severe deformity). Individuals who had undergone surgery in the study shoulder within the previous 12 months received an intra-articular or peri-articular steroid injection into the study shoulder within the previous 3 months or received an intra-articular HA injection into the study joint within the previous 9 months were also excluded.
Durolane® (NASHA non-animal hyaluronic acid; Bioventus LLC, Durham, NC, USA; prefilled 3 mL syringe; 20 mg/mL) was injected into the GH joint at the baseline clinic visit. Each patient received a single injection into one shoulder (the “study joint”). 21/23 G needles of length 3.8–5.1 cm were used (needles not provided in the product package). Application of a topical anesthetic (eg, ethyl chloride or lidocaine spray) or subcutaneous lidocaine and the use of image guidance were permissible but not mandatory. All injections were performed by a shoulder surgeon experienced in delivering intra-articular injections into the GH joint. After the injection procedure, patients were asked to remain at the study site for 30 mins to monitor for adverse events (AEs) and advised to rest the study joint for at least 24 hrs.
Follow-up visits were scheduled at 6, 12 and 26 weeks post-treatment, and a phone call was undertaken at 18 weeks. Thus, with the exception of the 18-week timepoint, all data were collected at the outpatient clinics serving as the study centers. The primary efficacy variable was the SPOM VAS score. The secondary efficacy variables shoulder pain at night (SPAN) and patient global assessment were measured using a 0–100 mm VAS. In addition, the American shoulder and elbow surgeons (ASES) patient self-evaluation Shoulder Score Index (SSI; score range 0–100) and rescue medication consumption (mg/week) were assessed. Safety was monitored by recording AEs (classified according to the medical dictionary for regulatory activities [MedDRA]), vital signs and physical examination results. Local symptoms following intra-articular injection were anticipated and recognized as AEs only if they were worse than symptoms occurring before the procedure or were worse than typically expected for this type of treatment. Signs and symptoms of GH-OA occurring after study treatment were not considered as AEs if they were also present before treatment, unless representing a clinically significant exacerbation of the disease or a recurrence following initial recovery.
Statistical methods
Safety data were analyzed based on the safety set, defined as all patients who were exposed to the study treatment. Efficacy data were summarized using descriptive statistics for the full analysis set, defined as all patients in the safety set who had at least one post-treatment efficacy assessment. For missing values, no imputation was performed. A mixed effects repeated measures (MERM) regression analysis was used for all inferential statistics; enrolment site and visit week were fixed-effect covariates and patients were random effects. Least square mean (LSMean) values were calculated for specific time points and for estimates over the 26-week study period; the latter were based on all post-treatment assessments (ie, weeks 6, 12, 18 and 26). All MERM LSMean estimates include and are adjusted for the assessments of patients who withdrew from the study early. SAS version 9.4 or higher was used for all statistical analyses.
The success criterion for the study (the primary outcome) was a 25% reduction from baseline in the SPOM VAS score over the 26-week study period, with the F-statistic for change from baseline achieving the 0.05 type I error level. A minimum sample size of 29 was determined for detecting a reduction in mean SPOM VAS score of 15 mm (25% reduction from a baseline mean of 60 mm) with 80% power. This was based on a standard deviation (SD) within each timepoint of 25 mm and correlation between visits of 0.5. A minimum enrolment of 36 patients was planned to allow the power of the study to be maintained in case of a drop-out rate up to 20%.
Data tables and listings related to the efficacy and safety results of this study are available upon request from the study sponsor.
Results
Study participants
A total of 41 patients were enrolled into the study, all of whom received study treatment. The date of first enrollment was 8th April 2015, and the last patient’s final follow-up visit was on 23rd May 2017. One patient received a subcutaneous injection of celestone for OA of the thumb at the screening visit and was discontinued from the study on Day 1, before any post-baseline efficacy assessments had been made. Consequently, there were 41 patients in the safety set, of whom 40 were included in the full analysis set. Sixteen full analysis set patients discontinued from the study before Week 26: five underwent shoulder replacement surgery, four withdrew consent, three were lost to follow-up, two had protocol violations and two discontinued according to physician decision. Therefore, 24 patients were followed to the end of the study.
The mean age at enrolment was 65.4 years, and the majority of the population (70.7%) were male (Table 1). Twenty-five patients (61.0%) had a body mass index of 25.0–29.9 kg/m2 and were classified as overweight, while nine (22.0%) had a body mass index ≥30.0 kg/m2 and were classified as obese. The study joint was the left shoulder in 20 patients (48.8%) and the right shoulder in the remaining 21 (51.2%). Shoulder OA was diagnosed during the previous 6 months in 26 patients (63.4%). The injection procedure was performed without anesthetic in 29 patients (70.7%), and all treatments were administered without image guidance. No aspirations were performed, and the entire volume (3 mL) was given for all injections. An 18-22G needle was used for 28 of the 41 injections (68.3%) and a 22-25G needle was used for the other 13 (31.7%).
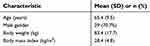 | Table 1 Patient demographics and baseline characteristics (safety set, N=41) |
Primary efficacy analysis
The mean SPOM VAS score at each study timepoint is shown in Figure 1. The decrease versus baseline in SPOM VAS score was greatest at Week 12 and exceeded 25% at every timepoint. A similar pattern was observed with LSMean values, although these data suggest slightly smaller improvements versus baseline compared with the unadjusted means (Table 2). The LSMean change from baseline in SPOM VAS score over the whole 26-week study period was −20.1 mm (95% CI: −25.2, −15.0 mm), corresponding to an LSMean percentage reduction of 29.5% (22.0, 37.0%). The change from baseline F-statistic was 8.97 (p<0.0001) and the t-statistic was −7.92 (p<0.0001), demonstrating that the treatment benefit over the study period was statistically significant. Thus, the study success criterion (SPOM VAS score ≥25% reduction from baseline with F-statistic p≤0.05) was met.
 | Table 2 Primary and secondary efficacy results in the full analysis set (N=40) |
 | Figure 1 Shoulder pain on movement (SPOM) visual analog scale (VAS) results: mean score and mean percentage change from baseline. Error bars represent standard deviation (SD). |
Secondary efficacy analyses
At all post-treatment timepoints, treatment with NASHA produced improvements versus baseline in the SPAN VAS score (Table 2). The LSMean change from baseline over the 26-week study period was −16.7 mm (−23.7, −9.7 mm), corresponding to an LSMean percentage decrease of 16.6%. The change from baseline F-statistic (7.66; p<0.0001) and the t-statistic (−4.78; p<0.0001) confirmed that the improvement in SPAN VAS score over the whole study period was statistically significant. The greatest improvement in SPAN VAS unadjusted mean score was observed at 18 weeks, while the SPAN adjusted LSMean scores were stable at about 50 mm across all visits post-baseline (ranging between 49.3 mm at Week 6 and 51.1 mm at Week 26).
Patient global assessment scores also improved after study treatment, with scores higher than baseline at every timepoint post-treatment (Table 2). For the whole period of the study, the LSMean change from baseline over was +9.80 mm (2.92, 16.68 mm), which corresponded to an LSMean percentage change of +69.08%. The improvement was statistically significant, as shown by the F-statistic (5.79; p=0.0006) and the t-statistic (2.85; p=0.0061). The greatest improvement in patient global assessment was evident at 18 weeks.
Patient numbers were reduced for analysis of ASES SSI scores because if a patient failed to answer any one of the 11 questions the score could not be calculated. Despite this, a statistically significant improvement was evident over the 26-week study period, with an LSMean change from baseline of 6.06 (1.51, 10.61), representing a 5.72% increase. Statistical significance was shown by the F-statistic and the t-statistic (4.29, p=0.0084; 2.71, p=0.0104, respectively). The ASES SSI score peaked at 12 weeks and an improvement versus baseline was apparent at every timepoint, according to both LSMean and unadjusted mean values.
There was no clear change over time in the percentage of patients using rescue medication (ie, acetaminophen) since the previous visit. The highest percentages were at 6 weeks (48.7%) and 18 weeks (48.0%). The mean weekly doses post-treatment were all below 3500 mg, corresponding to mean daily doses less than 500 mg. Dose information was derived from relatively reduced numbers of patients (one patient at baseline, 7–10 patients at the post-treatment timepoints).
Safety
Seventeen out of 41 patients (41.5%) experienced AEs during the study (Table 3). No AEs occurred during the injection procedures. All AEs were mild or moderate in intensity, and the most commonly reported ones were headache, musculoskeletal pain and arthralgia. Two AEs were adjudged to be related to the study treatment, both of which were musculoskeletal pain (shoulder pain). There were no serious adverse events or deaths during the study, and no patients withdrew from the study due to an AE. There were no cases of study joint inflammation and no infections of the skin covering the study joint. Changes from baseline in vital sign measurements were minimal, and only one abnormality was found upon physical examination (sore feet, which was reported as an AE).
 | Table 3 Adverse events occurring in more than one patient (safety set, N=41) |
Discussion
This study represents the first prospective assessment of intra-articular NASHA for shoulder OA. The treatment was well tolerated, and the primary efficacy criterion (SPOM VAS score ≥25% reduction from baseline) was met. Clinically and statistically significant improvements in shoulder pain, both upon movement and at night, were evident throughout the 6-month study period and these were accompanied by improved patient global assessment scores. The percentage of patients taking rescue acetaminophen did not show a tendency to change over time, and the mean dose per day (<500 mg) was well below the maximum allowed (4,000 mg).
The percentage decrease from baseline in the SPOM VAS score of 29.5% (over the whole study period) is very close to the decrease in pain defined in the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) recommendations as “moderately important” (30–49% decrease).19 Previous studies in knee and hip OA have suggested how to interpret changes from baseline in the Western Ontario & McMaster Universities Osteoarthritis Index (WOMAC) pain VAS score. The absolute change from baseline in our study (20.1 mm) was similar to or above the minimum clinically important improvement, and approximately double the minimum clinically perceptible improvement.20,21 The assessment method in our study (SPOM VAS score) was different from the WOMAC method, but the comparisons suggest that the improvement seen in our study was clinically relevant.
Treatment-emergent AEs occurred in less than half of patients and were mild or moderate in intensity. No serious adverse events occurred during the study, there were only two treatment-related adverse events, and no patients withdrew from the study because of AEs. Therefore, there is no suggestion of any safety concerns associated with NASHA as a treatment for GH-OA.
The discontinuation rate in this study was higher than anticipated, with 17/41 patients (41.5%) withdrawing before 26 weeks. Despite the number of patients completing the study falling below 29, the minimum suggested by the sample size calculation, the success criterion was still met. This is attributable to the use of MERM methodology, which uses the available data from all study participants (missing data were imputed by projected outcomes), and the observed treatment effect being larger than that assumed in the sample size calculation. Shoulder replacement surgery was the primary reason for discontinuation in five cases and a further six patients who discontinued were on a waiting list for shoulder surgery. Although these 11 patients met the inclusion criteria, they should probably not have been included in the study because of the exclusion criterion “subjects not likely to avoid other therapies” (there was always a risk that they could discontinue at any time). A post-hoc analysis showed the percentage reduction from baseline in SPOM VAS score over 12 weeks was 38.8% in the 29 non-surgery patients within the full analysis set, compared with 19.2% in the 11 surgery patients. These results suggest that patients undergoing or planning shoulder surgery had GH-OA that was more advanced than in the other study participants, and this would have reduced the likelihood of an optimal response to viscosupplementation. This supposition is borne out by the adjusted SPOM, SPAN and PGA LSMeans showing slightly reduced improvements compared with the unadjusted means. It is possible that the 11 surgery patients participated in the study as a personal bridging strategy to help manage pain until the time of surgery.
Intra-articular HA has previously been shown to be efficacious in patients with GH-OA. The largest previous study was randomized, double-blind and placebo-controlled.3 A total of 660 patients were randomized to receive 5 weekly injections: all sodium hyaluronate, three sodium hyaluronate and two saline, or all saline. The primary endpoint (shoulder pain at 13 weeks) did not show a significant benefit with sodium hyaluronate. However, there were trends in favor of active treatment and significant improvements versus placebo were observed at Week 7 (all sodium hyaluronate), Week 17 (three and five sodium hyaluronate injections) and Week 26 (three sodium hyaluronate injections). In a second randomized, placebo-controlled trial, 300 patients received three, weekly injections of sodium hyaluronate or placebo.5 There were no significant overall between-group differences in VAS pain score or Outcome Measures in Rheumatoid Clinical Trials-Osteoarthritis Research Society International (OMERACT-OARSI) response rate, but significant benefits were observed with sodium hyaluronate in a subgroup of patients without concomitant pathologies. In both of these trials, AE rates were similar with sodium hyaluronate and placebo, and there were no serious treatment-related AEs. Three intra-articular injections of HA with 15-day intervals, combined with physiotherapy for 3 months, were compared with physiotherapy only in a third randomized trial, involving 78 patients.4 Six months after treatment was started, the Constant score was statistically significantly higher in the HA group versus physiotherapy only, indicating reduced pain, and no AEs were reported.
A retrospective study compared GH-OA patients treated with three, weekly injections of either hylan G-F 20 (n=51) or a corticosteroid (n=33).6 Significant benefits versus baseline were observed with sodium hyaluronate at 1, 3 and 6 months, with respect to VAS pain score and the Shoulder, Pain and Disability Index. Improvements versus baseline were also seen in the corticosteroid group, but only at 1 month post-treatment.
A number of single-arm, uncontrolled studies have also been published. Two such studies were performed with hylan G-F 20; one was a preliminary investigation of three, weekly injections in 30 patients9 and the other was a multicenter study in which 33 patients received a single injection, with a second injection available after 1, 2 or 3 months.7 Significant reductions in pain were reported in both of these studies; the multicenter study showed mean VAS pain score improving from 61 mm at baseline to 37 mm at 3 months. No serious or severe treatment-related AEs were reported in either of these studies. Three weekly injections of high molecular weight hyaluronan were assessed in a cohort of 27 patients.10 Significant improvements in VAS pain score were evident over 26 weeks and an OMERACT-OARSI response rate of 78% was reported. There were no treatment-related AEs. In a more recent study, HYADD4-G was administered as two injections, 1 week apart, and patients were followed up for 26 weeks.8 In the 41 study participants, SPOM VAS score improved from 66 mm at baseline to 38 mm at 6 months, with a greater improvement over the first 13 weeks than over the second 13 weeks post-treatment. There were no serious AEs.
NASHA was the first HA product to be administered routinely as a single injection, instead of multiple injections. It has a prolonged intra-articular residence time because a unique molecular cross-linking process is undertaken during manufacture.22 The efficacy of one NASHA injection appears to be broadly similar to that achieved with multiple injections of other HA products.16 Treatment with a single injection requires less health care professional time than multiple injections, lowering this dimension of treatment cost, and patients are likely to prefer having to undergo only one injection.
Treatment guidelines for GH-OA are lacking, but a UK patient care pathway was published in 2016.1 This publication includes consideration of a broad range of treatment options, from oral drug treatment to surgery. It is recommended that treatment be tailored to the patient’s needs, depending on symptom severity. Intra-articular sodium hyaluronate is suggested for temporary symptomatic relief in cases where treatment with analgesics/NSAIDs, acupuncture or physical therapy is inadequate, and surgery is contraindicated or needs to be delayed.
This study has several limitations apart from the high discontinuation rate. It was a preliminary study performed in a relatively small number of patients, in the absence of a comparator group and without blinding of either the patients or investigators. It is therefore not possible to determine the extent to which placebo effect might have contributed to the study outcomes. A larger dataset with a control group is now needed for robust characterization of the safety and efficacy of NASHA injection for treatment of GH-OA. Participants of the present study were allowed to have bilateral GH-OA but were only treated in one joint, and this could have reduced the sensitivity with which responses to NASHA were detectable. Injections were performed without visual guidance; therefore, it is possible that some treatments were not delivered to the intra-articular space of the GH joint as intended. Strengths of the study include the allowance of treatment only with acetaminophen apart from intra-articular NASHA, and the inclusion of several different efficacy variables.
Conclusions
In conclusion, this study provides preliminary evidence that a single injection of NASHA may be efficacious in patients with symptomatic GH-OA. Improvements in pain were clinically and statistically significant and sustained over the 6-month follow-up period, and the primary study success criterion was met. NASHA appeared to be well tolerated, and no new safety signals were identified. Evidence from larger, controlled studies is needed to confirm these findings.
Acknowledgments
The authors thank Ken Sutor who provided medical writing services on behalf of Bioventus LLC. This study was supported by Bioventus LLC, Durham, NC, USA.
Disclosure
AJH, TW and JJ are employees of Bioventus. MDK reports personal fees from Bioventus, royalties from Stryker, publishing royalties from Elsevier during the conduct of the study. RL reports grants, personal fees from Smith Nephew outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Thomas M, Bidwai A, Rangan A, et al. Glenohumeral osteoarthritis. Shoulder Elbow. 2016;8(3):203–214. doi:10.1177/1758573216644183
2. Millett PJ, Gobezie R, Boykin RE. Shoulder osteoarthritis: diagnosis and management. Am Fam Physician. 2008;78(5):605–611.
3. Blaine T, Moskowitz R, Udell J, et al. Treatment of persistent shoulder pain with sodium hyaluronate: a randomized, controlled trial. A multicenter study. J Bone Joint Surg Am. 2008;90(5):970–979. doi:10.2106/JBJS.F.01116
4. Di Giacomo G, de Gasperis N. Hyaluronic acid intra-articular injections in patients affected by moderate to severe glenohumeral osteoarthritis: a prospective randomized study. Joints. 2017;5(3):138–142. doi:10.1055/s-0037-1605389
5. Kwon YW, Eisenberg G, Zuckerman JD. Sodium hyaluronate for the treatment of chronic shoulder pain associated with glenohumeral osteoarthritis: a multicenter, randomized, double-blind, placebo-controlled trial. J Shoulder Elbow Surg. 2013;22(5):584–594. doi:10.1016/j.jse.2012.10.040
6. Merolla G, Bianchi P, Porcellini G. Ultrasound-guided subacromial injections of sodium hyaluronate for the management of rotator cuff tendinopathy: a prospective comparative study with rehabilitation therapy. Musculoskelet Surg. 2013;97(Suppl 1):49–56. doi:10.1007/s12306-013-0259-y
7. Noel E, Hardy P, Hagena FW, et al. Efficacy and safety of Hylan G-F 20 in shoulder osteoarthritis with an intact rotator cuff. Open-label prospective multicenter study. Joint Bone Spine. 2009;76(6):670–673. doi:10.1016/j.jbspin.2009.10.008
8. Porcellini G, Merolla G, Giordan N, et al. Intra-articular glenohumeral injections of HYADD®4-G for the treatment of painful shoulder osteoarthritis: a prospective multicenter, open-label trial. Joints. 2015;3(3):116–121. doi:10.11138/jts/2015.3.3.116
9. Silverstein E, Leger R, Shea KP. The use of intra-articular hylan G-F 20 in the treatment of symptomatic osteoarthritis of the shoulder: a preliminary study. Am J Sports Med. 2007;35(6):979–985. doi:10.1177/0363546507300256
10. Weil AJ. High molecular weight hyaluronan for treatment of chronic shoulder pain associated with glenohumeral arthritis. Med Devices (Auckl). 2011;4:99–105. doi:10.2147/MDER.S22423
11. Altman RD, Akermark C, Beaulieu AD, Schnitzer T. Durolane International Study G. Efficacy and safety of a single intra-articular injection of non-animal stabilized hyaluronic acid (NASHA) in patients with osteoarthritis of the knee. Osteoarthritis Cartilage. 2004;12(8):642–649. doi:10.1016/j.joca.2004.04.010
12. Arden NK, Akermark C, Andersson M, Todman MG, Altman RD. A randomized saline-controlled trial of NASHA hyaluronic acid for knee osteoarthritis. Curr Med Res Opin. 2014;30(2):279–286. doi:10.1185/03007995.2013.855631
13. Berg P, Olsson U. Intra-articular injection of non-animal stabilised hyaluronic acid (NASHA) for osteoarthritis of the hip: a pilot study. Clin Exp Rheumatol. 2004;22(3):300–306.
14. Conrozier T, Couris CM, Mathieu P, et al. Safety, efficacy and predictive factors of efficacy of a single intra-articular injection of non-animal-stabilized-hyaluronic-acid in the hip joint: results of a standardized follow-up of patients treated for hip osteoarthritis in daily practice. Arch Orthop Trauma Surg. 2009;129(6):843–848. doi:10.1007/s00402-008-0778-4
15. Leighton R, Akermark C, Therrien R, et al. NASHA hyaluronic acid vs. methylprednisolone for knee osteoarthritis: a prospective, multi-centre, randomized, non-inferiority trial. Osteoarthritis Cartilage. 2014;22(1):17–25. doi:10.1016/j.joca.2013.10.009
16. Zhang H, Zhang K, Zhang X, et al. Comparison of two hyaluronic acid formulations for safety and efficacy (CHASE) study in knee osteoarthritis: a multicenter, randomized, double-blind, 26-week non-inferiority trial comparing Durolane to Artz. Arthritis Res Ther. 2015;17:51. doi:10.1186/s13075-015-0557-x
17.
18. Schulz KF, Altman DG, Moher D. Group C. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332. doi:10.1136/bmj.c293
19. Dworkin RH, Turk DC, Wyrwich KW, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain. 2008;9(2):105–121. doi:10.1016/j.jpain.2007.09.005
20. Ehrich EW, Davies GM, Watson DJ, Bolognese JA, Seidenberg BC, Bellamy N. Minimal perceptible clinical improvement with the Western Ontario and McMaster Universities osteoarthritis index questionnaire and global assessments in patients with osteoarthritis. J Rheumatol. 2000;27(11):2635–2641.
21. Tubach F, Ravaud P, Baron G, et al. Evaluation of clinically relevant changes in patient reported outcomes in knee and hip osteoarthritis: the minimal clinically important improvement. Ann Rheum Dis. 2005;64(1):29–33. doi:10.1136/ard.2004.022905
22. Agerup B, Berg P, Akermark C. Non-animal stabilized hyaluronic acid: a new formulation for the treatment of osteoarthritis. BioDrugs. 2005;19(1):23–30. doi:10.2165/00063030-200519010-00003
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
