Back to Journals » Research Reports in Clinical Cardiology » Volume 10
Mycotic pseudoaneurysm in intravenous drug users: current insights
Authors Stevenson RP, Tolias C , Hussey K, Kingsmore DB
Received 4 September 2018
Accepted for publication 3 January 2019
Published 11 February 2019 Volume 2019:10 Pages 1—6
DOI https://doi.org/10.2147/RRCC.S161698
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Kones
Richard P Stevenson,1 Christos Tolias,1 Keith Hussey,2 David B Kingsmore2
1Department of Surgery, Glasgow Royal Infirmary, Glasgow G4 0SF, UK; 2Department of Vascular Surgery, Queen Elizabeth University Hospital, Glasgow G51 4TF, UK
Abstract: Mycotic pseudoaneurysms are rare, but potentially life threatening. They are challenging both from a diagnostic and surgical perspective. It is an area lacking in robust trial data, and current knowledge and evidence is represented only by retrospective case series. This review will summarize the current literature with regard to mycotic pseudoaneurysms consequent to illicit drug misuse.
Keywords: IVDU, mycotic, pseudoaneurysm
Introduction
A pseudoaneurysm (synonymous with false aneurysm) occurs when there is disruption of the arterial wall and may be defined anatomically as the presence of blood between the tunica media and the tunica adventitia. This differs from true aneurysm where all layers of the arterial wall (including the intima) are involved.
The term “mycotic” is used to define an aneurysm/pseudoaneurysm that occurs as a consequence of infection. When applied in this context, the term is a misnomer as it used to describe all arterial infections rather than fungal infection in isolation. However, it was not until the mid-19th century that mycotic pseudoaneurysms associated with other pathogens (specifically bacteria) were recognized and described.1–3 They represent a fulminant infectious process, which, if untreated, may result in systemic sepsis, rupture and exsanguination.
Historically, mycotic pseudoaneurysms were classified pathophysiologically based on the mode of arterial infection: direct arterial infection from an area of suppuration (primary), septic embolus with arterial occlusion (secondary) – frequently in the context of infective bacterial endocarditis, and finally, as a consequence of adherence of viable pathogens in the arterial wall in patients with systemic sepsis.4,5
However, in developed countries, the pathophysiology has changed as a consequence of access to and development of antibiotics, with changes in patterns of behavior. A review of 178 patients with 243 mycotic aneurysms published in 1984 described arterial trauma as being the most significant pathophysiological process. This is reflected in contemporary vascular surgical practice.6 In some cases, this may be iatrogenic following interventional radiological/cardiological procedures, although in these cases, hemorrhage is most frequently encountered on completion of the procedure and infection is rarely an issue.7 In Scotland, mycotic pseudoaneurysm is most frequently encountered in the population that uses heroin intravenously.
We have reviewed the world literature and summarize trends in current practice and critically evaluate surgical management strategies for mycotic pseudoaneurysm of the common femoral artery occurring as a consequence of inadvertent arterial self-injection in intravenous drug users (IVDU).
Epidemiology
Worldwide, it is estimated that 16 million people are IVDU. Drugs injected include opiates, cocaine, amphetamines and steroids. Although recent reports suggest a reduction in the population using opiates intravenously, recent evidence published by the European Monitoring Center for Drugs and Drug Addiction has estimated the number of problem opiate users across the continent to be 1.4 million (in Scotland, there are 20,000 IVDU).8
In the IVDU population, there has been a notable rise in those injecting into the groin. Historically, smaller peripheral veins were cannulated first and the groin was considered to be the last resort as peripheral access thrombosed. However, over the past 10 years, the groin appears to be used as the primary injection site more frequently (cited reasons for this include concealment, reliability, ease of access and even potentially for a perceived “bigger hit”).9
The annual incidence of mycotic pseudoaneurysm of the common femoral artery ranges from 0.03%9 to 1%.10,11 This figure is perhaps surprising, given that of 3,733 IVDU surveyed in England, Wales and Northern Ireland, 35% reported infection at injection sites within the previous 12 months.12 Features associated with infection include frequency of injection, duration of time injecting and those who had recently used a needle exchange program. Scottish national statistical data have shown an increase in the proportion of patients over the age of 40 years receiving specialist attention for heroin use,13 and an older group of patients are now presenting with mycotic pseudoaneurysm.10,14,15
The bacteria associated with mycotic pseudoaneurysm in IVDU differ from those reported in historical, non-IVDU series, which is unsurprising as the pathophysiological mechanisms differ. The most commonly encountered pathogens9 in contemporary series in this patient population are staphylococci (most common), streptococci, pneumococci and enterococci. Salmonella may be encountered, but is less common.16,17 In many cases, a polymicrobial field may be encountered,10,12 and consequently, initiation of broad-spectrum antibiotics is recommended until definitive culture results are available.
An important consideration for health care practitioners involved in the management of patients presenting with mycotic pseudoaneurysm is the presence of blood-borne viral infections (which include hepatitis B, hepatitis C and HIV).10 It is important for all health care workers to be aware of the high incidence of transmissible infections within this patient group and appropriate precautions should be taken. If patients have not been screened for viral infections, appropriate counseling with subsequent screening is required.
Diagnosis/investigation
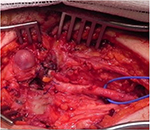
In the majority of cases, diagnosis of mycotic pseudoaneurysm is clear. There will be an antecedent history of IVDU. Often, there will be pain reported at the site of injection. In patients with bacteremia, there may be nonspecific prodromal symptoms and systemic sepsis may be seen. There is often a history of bleeding, and a herald bleed may often precede life-threatening hemorrhage. Hypotension may be encountered if there has been significant hemorrhage or if there is severe sepsis. There is often erythema around the injection site, and in the majority of cases, there is swelling. There may be a groin sinus, a sign of repeated intravascular injection (Figure 1). Often, the hip on the affected side will be held in flexion, a sign of psoas irritation and retroperitoneal extension of the infective/inflammatory component. An important aspect of the history is the occurrence of previous deep vein thrombosis, as this may critically impact on subsequent limb viability.
Duplex may have a role in the investigation of patients where the diagnosis is uncertain. The sensitivity and specificity of duplex is reported to be 94% and 97%, respectively, in patients with post-catheterization pseudoaneurysm.18 However, if arterial imaging is required in an IVDU, CT angiography is probably the better option (Figure 2).19 CT will also allow characterization of the retroperitoneum to confirm/exclude proximal extension of sepsis (this is an important part of preprocedural planning). However, if there is significant ongoing hemorrhage, the most appropriate course of action is to transfer the patient immediately to the operating theater for surgical exploration.
  | Figure 2 Reconstructed three-dimensional CT angiogram demonstrating a mycotic common femoral pseudoaneurysm at the level of the inguinal ligament. Abbreviation: CT, computed tomography. |
Management
If the diagnosis of mycotic pseudoaneurysm is confirmed, it is important to ensure that there is appropriate intravenous access for resuscitation and that the blood transfusion service is informed given the possibility of major hemorrhage. Empirical broad-spectrum antibiotic therapy should be administered in accordance with the local protocols for severe soft tissue infection. There should be appropriate cover for staphylococci.10
There is no evidence in the literature supporting a conservative strategy with antibiotic therapy in isolation, and in the majority of cases where the presentation has been with significant hemorrhage, this would clearly be inappropriate.
The central area of controversy in the management of mycotic pseudoaneurysm of the common femoral artery relates to the surgical strategy and, specifically, the requirement for arterial reconstruction. With each approach, debridement of necrotic tissue and drainage of sepsis must be performed (specimens must be sent for microbiological assessment).
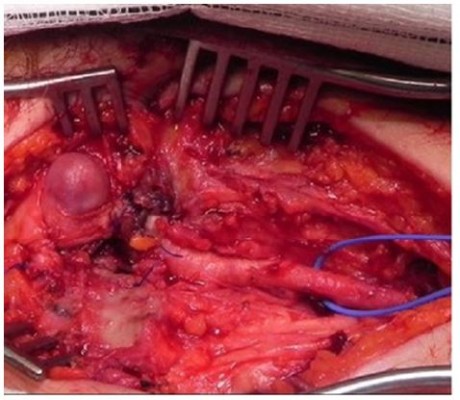
Primary arterial ligation without reconstruction has been well described. This should include ligation of the distal external iliac artery/proximal common femoral artery, superficial femoral artery and profunda femoris. Figure 3 demonstrates an intraoperative view of a common femoral artery with proximal incision for control of the external iliac artery. Those who advocate this approach argue that hemorrhage control is achieved and that the procedure is safe – following the procedure, the limb is rendered acutely ischemic and most patients will have symptoms as a consequence of this. However, in the majority of case series describing this approach, rates of subsequent major limb amputation are low (although when required, this is generally at the transfemoral level).10,13,14,19–21 Factors that may influence this include the degree of collateralization, pre-existing occlusive atherosclerotic artery disease and presence of occlusive deep venous pathology, although the relationship of these features to the outcome of the limb has not been defined. Long-term outcome in patients who do not lose the limb on index admission is less clear as these patients are frequently lost to follow-up as a consequence of chaotic lifestyle choices.10
Immediate arterial reconstruction at the time of the index procedure following arterial control has been described.22,23 Advocates argue that secondary hemorrhage is uncommon and that both limb salvage is improved and long-term symptoms (lifestyle-limiting claudication) are reduced. However, other series have described secondary hemorrhage occurring on the index admission as a consequence of infection, necessitating further surgical intervention (with graft ligation).
Perhaps a more pragmatic approach is to consider arterial reconstruction on an elective basis following wound healing (if the patient has symptoms which would warrant). Specific considerations include a lack of autologous conduit for bypass (in the majority of cases, there has been a long history of drug use with obliteration of the superficial venous system, and often, there may be thrombotic occlusion of the deep venous system, although in some cases, the basilic vein in the dominant arm may be preserved). Using prosthetic grafts in this context can be effective, but is associated with potential for graft infection. If considered, operative strategies such as tunneling the graft through the obturator foramen may be helpful to avoid a previously explored/inflammatory surgical field. Biosynthetic composite grafts may have a role with lower infection rates reported than with Dacron or polytetrafluroethylene.24,25 However, there is no long-term data to support the use of these grafts. Table 1 summarizes the outcomes reported by the larger case series reporting outcome measures following intervention for mycotic pseudoaneurysm in IVDU.
  | Table 1 Summary of published case series |
In the endovascular era, consideration must be given to possible endovascular interventions, although at present, there is limited data to support these strategies. Mycotic aneurysms have been managed with covered stent grafts and combined with antibiotic suppression for producing a good effect, but the data supporting this are very limited.25–27 Case reports and small series have suggested favorable outcomes with stent grafts used as a bridge to definitive surgical arterial reconstruction to allow adequate treatment of sepsis.28,29 This would seem to be an expensive strategy, which the authors do not advocate at present. Coil embolization and thrombin injection are suitable in the context of iatrogenic post-catheterization pseudoaneurysms (without infection). Neither strategy has a role in the management of mycotic pseudoaneurysm in IVDU.
Wound management in this patient group is challenging. Broadly speaking, there are two strategies, which include primary closure (with or without drainage) and leaving the wound open to heal by secondary intention with dressing therapy. The central advantage of the former is that it is more convenient for both the patient and the nursing team involved with wound management. A sartorius flap may be a useful adjunct, although it is the authors’ experience that often, there has been a chronic inflammatory response around the mycotic pseudoaneurysm that can make this challenging. If primary closure is employed, clinicians should have a low threshold to re-open the wound should there be evidence of wound infection/collection. If there is extensive sepsis/tissue loss as a consequence of necrosis, primary wound closure may not be possible. In cases like this, there may be significant lymphatic disruption. Both of these issues can contribute to protracted wound problems. In this context, there may be a role for negative wound pressure therapy (albeit applying this to an arterial bed is a relative contraindication). Alternative dressing therapies may also be used – there is no evidence to guide the medical and nursing management.
In the UK, the social care system seeks to help this patient group. Drug rehabilitation services seek to engage the patients while they are recovering from the surgical procedure. Rehabilitation and social services will then seek to ensure that safe and appropriate housing is available. This process is challenging and patient engagement with this is variable. A proportion of this patient population will take its own discharge and subsequently be lost to follow-up, unless there is symptomatic deterioration that forces a further presentation.
The evidence available to guide the clinician with the management of mycotic pseudoaneurysm in IVDU is limited. Often, patients present late are unwell with systemic inflammatory response and have organ dysfunction as a consequence of sepsis. Consequently, in this disparate group, a randomized controlled trial would be fraught with ethical dilemma and practically would be unrealistic. As such, the evidence that we have which is derived from case series must guide us. The institutional bias of the authors’ center for primary ligation has been influenced by previously published (albeit historical) work in Glasgow.21 Specifically, a small case series described six cases where immediate reconstruction was performed with prosthetic grafts – there were five graft infections with life-threatening hemorrhage in four.
Conclusion
Mycotic common femoral artery pseudoaneurysm as a consequence of inadvertent arterial self-injection in IVDU remains a common presentation in areas where there are significant populations using intravenous heroin. Diagnosis can be made on the basis of clinical grounds and is generally uncomplicated. Appropriate resuscitation with early administration of antibiotic therapy is essential. If arterial imaging is considered necessary, CT angiography is the modality of choice as it allows assessment of the retroperitoneum and allows exclusion of a significant proximal extension of sepsis. Surgical management involves drainage of sepsis and debridement of non-viable tissue. The evidence available suggests that arterial ligation is safe, although in a small proportion of patients, limbs may be lost with this strategy. It is reasonable to extrapolate from the limited data presented in the world literature with regard to endovascular techniques that these strategies may have a role, although as yet, they remain undefined.
Disclosure
The authors report no conflicts of interest in this work.
References
Finseth F, Abbott WM. One-stage operative therapy for Salmonella mycotic abdominal aortic aneurysm. Ann Surg. 1974;179(1):8–11. | ||
Tufnell J. On the influence of vegetations on the valves of the heart, in the production of secondary arterial disease. Q J Med Sci (Dublin). 1853;15(2):371–382. | ||
Stengel A, Wolferth CC. Mycotic (bacterial) aneurysms of intravascular origin. Arch Intern Med. 1923;31(4):527. | ||
Crane AR. Primary multilocular mycotic aneurysms of the aorta. Arch Pathol. 1937;24:634. | ||
Labardini MM, Dow RW. Primary mycotic aneurysm of the right common iliac artery. Arch Surg. 1968;96(3):373. | ||
Brown SL, Busuttil RW, Baker JD, Machleder HI, Moore WS, Barker WF. Bacteriologic and surgical determinants of survival in patients with mycotic aneurysms. J Vasc Surg. 1984;1(4):541–547. | ||
Mccready RA, Bryant MA, Divelbiss JL, Chess BA, Chitwood RW, Paget DS. Arterial infections in the new millennium: an old problem revisited. Ann Vasc Surg. 2006;20(5):590–595. | ||
European Monitoring Centre for Drugs and Drug Addiction. Trends in heroin use in Europe. Emcdda.europa.eu. 2013. Available from http://www.emcdda.europa.eu/publications/pods/trends-in-heroin-use_en. Accessed September 05, 2018. | ||
Senbanjo R, Strang J. Evaluation of femoral ultrasonography as a tool for promoting cessation of groin-injecting behaviour. Eur Addict Res. 2015;21(4):204–210. | ||
Tsao JW, Marder SR, Goldstone J, Bloom AI. Presentation, diagnosis, and management of arterial mycotic pseudoaneurysms in injection drug users. Ann Vasc Surg. 2002;16(5):652–662. | ||
Stevenson RP, Semple C, Hussey K, McGovern J, Stuart WP, Kingsmore DB. Changes in the demographics of intravenous drug users with mycotic common femoral artery pseudoaneurysm as a consequence of self-injection does not influence outcome following emergency ligation. Vascular. 2017;25(5):520–524. | ||
Hope VD, Marongiu A, Parry JV, Ncube F. The extent of injection site infection in injecting drug users: findings from a national surveillance study. Epidemiol Infect. 2010;138(10):1510–1518. | ||
A National Statistics Publication for Scotland. Scottish Drug Misuse Database: overview of individuals assessed in 2011/12. Available from: http://www.isdscotland.org/Health-Topics/Drugs-and-Alcohol-Misuse/Publications/2013-03-26/2013-03-26-SDMDS-Report.pdf. Accessed September 05, 2018. | ||
Gan JP, Leiberman DP, Pollock JG. Outcome after ligation of infected false femoral aneurysms in intravenous drug abusers. Eur J Vasc Endovasc Surg. 2000;19(2):158–161. | ||
Peirce C, Coffey JC, O’Grady H, Aly S, O’Malley K, O’Donohoe M. The management of mycotic femoral pseudoaneurysms in intravenous drug abusers. Ann Vasc Surg. 2009;23(3):345–349. | ||
Müller BT, Wegener OR, Grabitz K, Pillny M, Thomas L, Sandmann W. Mycotic aneurysms of the thoracic and abdominal aorta and iliac arteries: experience with anatomic and extra-anatomic repair in 33 cases. J Vasc Surg. 2001;33(1):106–113. | ||
Hsu R-B, Lin F-Y. Surgical pathology of infected aortic aneurysm and its clinical correlation. Ann Vasc Surg. 2007;21(6):742–748. | ||
Saad NE, Saad WE, Davies MG, Waldman DL, Fultz PJ, Rubens DJ. Pseudoaneurysms and the role of minimally invasive techniques in their management. Radiographics. 2005;25 Suppl 1:S173–S189. | ||
Behera A, Menakuru SR, Jindal R. Vascular complications of drug abuse: an Indian experience. ANZ J Surg. 2003;73(12):1004–1007. | ||
Hu ZJ, Wang SM, Li XX, Li SQ, Huang XL. Tolerable hemodynamic changes after femoral artery ligation for the treatment of infected femoral artery pseudoaneurysm. Ann Vasc Surg. 2010;24(2):212–218. | ||
Welch GH, Reid DB, Pollock JG. Infected false aneurysms in the groin of intravenous drug abusers. Br J Surg. 1990;77(3):330–333. | ||
Patel KR, Semel L, Clauss RH. Routine revascularization with resection of infected femoral pseudoaneurysms from substance abuse. J Vasc Surg. 1988;8(3):321–328. | ||
Georgiadis GS, Lazarides MK, Polychronidis A, Simopoulos C. Surgical treatment of femoral artery infected false aneurysms in drug abusers. ANZ J Surg. 2005;75(11):1005–1010. | ||
Bacourt F, Koskas F. Axillobifemoral bypass and aortic exclusion for vascular septic lesions: a multicenter retrospective study of 98 cases. French University Association for Research in Surgery. Ann Vasc Surg. 1992;6(2):119–126. | ||
Schneider PA, Abcarian PW, Leduc JR, Ogawa DY. Stent-graft repair of mycotic superficial femoral artery aneurysm using a Palmaz stent and autologous saphenous vein. Ann Vasc Surg. 1998;12(3):282–285. | ||
Callaert JR, Fourneau I, Daenens K, Maleux G, Nevelsteen A. Endoprosthetic treatment of a mycotic superficial femoral artery aneurysm. J Endovasc Ther. 2003;10(4):843–845. | ||
Kwon K, Choi D, Choi SH, et al. Percutaneous stent-graft repair of mycotic common femoral artery aneurysm. J Endovasc Ther. 2002;9(5):690–693. | ||
Antoniou G, Papas T, Tsagkos I, et al. Endovascular stent-graft repair of bleeding common femoral artery pseudoaneurysm in intravenous drug users: a bridge to surgical reconstruction. Vasa. 2014;43(6):473–477. | ||
Domanin M, Romagnoni G, Romagnoli S, Rolli A, Gabrielli L. Emergency Hybrid Approach to Ruptured Femoral Pseudoaneurysm in HIV-positive Intravenous Drug Abusers. Annals of Vascular Surgery. 2017;40:297.e5–297.e12. | ||
Arora S, Weber MA, Fox CJ, Neville R, Lidor A, Sidawy AN. Common femoral artery ligation and local debridement: a safe treatment for infected femoral artery pseudoaneurysms. J Vasc Surg. 2001;33(5):990–993. | ||
Naqi SA, Khan HM, Akhtar S, Shah TA. Femoral pseudoaneurysm in drug addicts—excision without revascularization is a viable option. Eur J Vasc Endovasc Surg. 2006;31(6):585–587. Naqi SA, Khan HM, Akhtar S, Shah TA. Femoral pseudoaneurysm in drug addicts—excision without revascularization is a viable option. Eur J Vasc Endovasc Surg. 2006;31(6):585–587. | ||
Yegane RA, Salehi NA, Ghaseminegad A, et al. Surgical approach to vascular complications of intravenous drug abuse. J Vasc Surg. 2006;44(4):907. | ||
Salimi J, Shojaeefar A, Khashayar P. Management of infected femoral pseudoaneurysms in intravenous drug abusers: a review of 57 Cases. Arch Med Res. 2008;39(1):120–124. | ||
Tan K, Chen K, Chia K, Lee C, Nalachandran S. Surgical management of infected pseudoaneurysms in intravenous drug abusers: single institution experience and a proposed algorithm. World J Surg. 2009;33(9):1830–1835. | ||
Mousavi SR, Saberi A, Tadayon N, Zeynalzadeh M, Kavyani A. Femoral artery ligation as treatment for infected pseudo-aneurysms, secondary to drug injection. Acta Chirurgica Belgica. 2010;110(2):200–202. | ||
Jayaraman S, Richardson D, Conrad M, Eichler C, Schecter W. Mycotic pseudoaneurysms due to injection drug use: a ten-year experience. Ann Vasc Surg. 2012;26(6):819–824. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.