Back to Journals » OncoTargets and Therapy » Volume 9
Mutations in hepatitis B virus small S genes predict postoperative survival in hepatocellular carcinoma
Authors Peng L, Yang G, Wu C, Wang WS, Wu J, Guo Z
Received 7 September 2016
Accepted for publication 9 November 2016
Published 2 December 2016 Volume 2016:9 Pages 7367—7372
DOI https://doi.org/10.2147/OTT.S121785
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Carlos E Vigil
Li Peng,1 Guang Yang,2 Chensi Wu,3 Wenshuai Wang,1 Jianhua Wu,4 Zhanjun Guo3
1Department of Hepatobiliary Surgery, 2Department of Radiology, 3Department of Gastroenterology and Hepatology, 4Animal Center, Fourth Hospital of Hebei Medical University, Shijiazhuang, People’s Republic of China
Abstract: Hepatitis B virus (HBV) DNA is prone to mutations due to proofreading deficiencies of HBV polymerase. We have previously identified hepatocellular carcinoma (HCC) survival–associated HBV mutations in the X, precore, and core regions. In the present study, we extended our research to assess HCC survival–associated HBV mutations in the small S gene of HBV genome in 115 HCC patients including 60 patients with HBV B genotype, 52 patients with HBV C genotype, and 3 patients with other genotypes. The overfrequencies of mutations at nucleotides 529 and 735 are 8.5% and 91.5%, respectively, but the distribution frequencies of these mutations are not different between HBV genotypes B and C. Mutational sites 529 (relative risk: 3.611, 95% confidence interval [CI]: 1.414–9.221, P=0.007) and 735 (relative risk: 1.905, 95% CI: 1.101–3.297, P=0.021) were identified as statistically significant independent predictors for HCC survival by multivariate survival analysis using a Cox proportional hazards model. Moreover, the mutated 529A and 735T were associated with both short survival time and high HBV DNA load score in HCC patients. The analysis of DNA mutations in the HBV S gene may help identify HCC subgroups with poor prognosis and may provide reference for therapeutic decisions.
Keywords: HCC, HBV, survival, S gene, mutations
Introduction
Hepatocellular carcinoma (HCC) is responsible for more than half a million cancer-related deaths annually, making it the third leading cause of cancer deaths worldwide.1 A number of clinical characteristics including tumor size, tumor quantity, cell differentiation, venous invasion, and inflammation degree have been identified as predictors for HCC, but the prognosis of HCC patients is still poor due to a high recurrence rate.2–5
Hepatitis B virus (HBV) is a hepatotropic virus that chronically infects approximately 400 million people worldwide and is thought to be responsible for a million deaths annually. HBV infection may be associated with a large spectrum of liver diseases including chronic hepatitis, cirrhosis, and HCC.6,7 In the People’s Republic of China, HBV infection is a challenging health issue with approximately 93 million people being HBV carriers and 30 million people being chronic hepatitis B patients.8 Eight geography-related HBV genotypes (genotypes A–H) have been identified with genotypes B and C predominant in eastern Asia.9
The HBV genome is a relaxed, circular, partially double-stranded DNA (rcDNA) with approximately 3,200 nucleotides and comprises four partially overlapping open reading frames (ORFs) that encode the surface protein (PreS/S), the core protein (preC/C), a polymerase (pol), and a multifunctional nonstructural protein (HBx).7 The PreS/S ORF has one long ORF with three in-frame “start” (ATG) codons and different aminoterminal extensions that encodes the three structurally related envelope proteins termed large, middle, and short proteins. The small S protein (HBsAg) contains 226 amino acids (aa), the middle protein (PreS2 + S) contains an extra N-terminal extension of 55 aa, whereas the large protein (PreS1 + PreS2 + S) has a further extensional N-terminal aa of 108 or 119.10 HBV DNA is prone to mutations due to the proofreading deficiencies of HBV polymerase.11,12 The HCC risk-associated HBV mutations have been well studied in HBV-related HCC (HBV-HCC) patients in recent years;13–18 furthermore, we and other researchers have found the prognostic value of the X and PreC/C region mutations for HCC outcome.19–21 The potential role of HBV preS mutations on HCC pathogenesis had been identified previously;7,22,23 we have now extended our research to assess HCC survival–associated HBV mutations in small S gene.
Materials and methods
Tissue specimens and DNA extraction
HBV-HCC tissue specimens were collected from patients who underwent tumor resection in the Department of Hepatobiliary Surgery in the Fourth Hospital of Hebei University between 2007 and 2010. The Wizard Genomic DNA extraction kit (Promega, Madison, WI, USA) was used to extract genomic DNA. This study and all procedures were supervised and approved by the Human Tissue Research Committee of the Fourth Hospital of Hebei Medical University. Written informed consent was obtained from all patients.
Virological assay
The HBV DNA concentration in the HBV-HCC tissue was quantified as copies per microgram of genomic DNA with ABI 7300 TaqMan platform (Life Technologies, Carlsbad, CA, USA) by real-time PCR. HBV genotypes were determined by multiplex-PCR as described previously.18 The DNA sequences flanking the small S region were amplified with the primer pairs listed in Table 1 according to the NCBI database (http://www.ncbi.nlm.nih.gov/genome/5536). Cyclic sequencing was performed with a BigDye Terminator v3.1 Cycle Sequencing Kit (Life Technologies) by ABI PRISM 3100 Genetic Analyzer (Life Technologies). Mutations were confirmed by repeating the analysis on both the strands.
  | Table 1 Primer pairs used in amplifying and sequencing the small S gene |
Statistical analysis
Survival curves were plotted with the log-rank test using Kaplan–Meier method. Cox proportional hazards model was used for multivariate survival analysis and χ2 test to analyze dichotomous values among the genotypes and HBV DNA copy numbers. All statistical analyses were performed using SPSS 18.0 software package (IBM Corporation, Armonk, NY, USA), and a P-value <0.05 was considered statistically significant.
Results
Clinical characteristics of HBV-HCC patients
A total of 115 HBV-HCC patients including 60 patients with B genotype, 52 patients with C genotype, 2 patients with D genotype, and 1 patient with A + C genotype were enrolled in this study. The relationships between the clinical characteristics and postoperative overall survival in HBV-HCC patients were analyzed with the log-rank test using Kaplan–Meier method. The portal vein thrombosis, tumor size, tumor stage, and HBV DNA load score were identified for their association with survival by univariate analysis (Table 2). After adjusting for clinical characteristics with the Cox proportional hazards model, the portal vein thrombosis and HBV load score were identified as independent predictors of postoperative survival in HBV-HCC patients.
Mutation of small S gene is associated with postoperative survival in HCC patients
The DNA sequences flanking the small S gene were sequenced in 47 HBV-HCC patients. Firstly, a total of 88 mutations were identified (Figure 1). The mutation sites with mutation distribution frequency higher than 5% were analyzed for their association with HCC survival by Kaplan–Meier method for patients with HBV genotypes B and C (Table 3). The potentially HCC survival–associated mutations sites of 529 and 735 were further analyzed in the remaining HCC patients; these two sites were identified for their association with HCC survival (Figure 2). After adjusting for clinical characteristics with the Cox proportional hazards model, the mutated 529A and 735T were associated with short survival time of HCC patients: 529 (RR: 3.611, 95% confidence interval [CI]: 1.414–9.221, P=0.007); 735 (RR: 1.905, 95% CI: 1.101–3.297, P=0.021). The overfrequencies of mutations at nucleotide 529 and 735 were 8.5% and 91.5%, respectively, but the distribution frequencies of these mutations were not different between HBV genotypes B and C. We evaluated the relationships between HBV replication and these two mutated sites, and the mutations were associated with higher HBV DNA load score (Table 4).
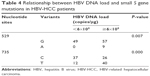  | Table 4 Relationship between HBV DNA load and small S gene mutations in HBV-HCC patients |
Discussion
HBV has a mutation rate that is more than 10-fold higher than that of other DNA viruses due to the deficiency of the proofreading function for HBV polymerase.7,11,12 Accumulation of mutations reflects both the activity of virus infection and the strength of the immune response. Some of these mutations could provide a survival advantage for HBV while the others are detrimental.7 The HBV mutations are clustered in a particular region of the HBV genome such as the basal core promoter (BCP)/preCore region and the preS/S region.24 We have identified previously the HBV-HCC survival–associated HBV mutations in the X protein region and preCore regions.20,21 Now we have extended our research to evaluate the mutations in the HBV DNA sequences flanking the small S gene and identified two mutations associated with HBV-HCC survival by multivariate analysis.
The specific preS/S gene mutations may induce both the intracellular accumulation of envelope proteins in the endoplasmic reticulum (ER), resulting in liver damage, and the activation of ER stress-signaling pathways, resulting in oxidative DNA damage and genomic instability; all these contribute to HCC development.7,23,25,26 The “a” determinant, that is the immunodominant determinant for the anti-HBs neutralization, is located in the aa 99–170 of the S protein.10,27 Nonsense mutations in the “a” determinant induce antigenically modified S proteins that may escape from the specific anti-HBs neutralizing antibody.28–30 The 529 mutation site was located in the “a” determinant region; this mutation does not induce aa substitution in the S gene, but the complete overlapping of PreS/S ORF with polymerase has made it possible to induce aa substitution of rtD134N in the HBV polymerase which may result in an altered function of the HBV polymerase so as to effect the viral replication. Our data did show that the 529G-A mutation might increase HBV DNA replication. Laboratory-based functional study for the role of 735 C-T which induces Ala-Val substitution on HCC development should be performed. The other mutations in the S gene were also analyzed for their association with the viral DNA load score, but statistical difference could not be found. These data implied that the 529- and 735-mutation-related alterations of the viral DNA scores should be responsible, at least partly, for the outcome of HCC.
In conclusion, we found survival-associated S gene mutations in HCC patients. The detection of outcome-associated HBV variants may help identify those HCC patients with poor prognosis for appropriate treatment.
Acknowledgment
This work was supported by the Key Basic Research Program of Hebei (14967713D).
Disclosure
The authors report no conflicts of interest in this work.
References
Gomaa AI, Khan SA, Toledano MB, Waked I, Taylor-Robinson SD. Hepatocellular carcinoma: epidemiology, risk factors and pathogenesis. World J Gastroenterol. 2008;14(27):4300–4308. | ||
Maki A, Kono H, Gupta M, et al. Predictive power of biomarkers of oxidative stress and inflammation in patients with hepatitis C virus-associated hepatocellular carcinoma. Ann Surg Oncol. 2007;14(3):1182–1190. | ||
Okada S, Shimada K, Yamamoto J, et al. Predictive factors for postoperative recurrence of hepatocellular carcinoma. Gastroenterology. 1994;106(6):1618–1624. | ||
Minagawa M, Makuuchi M, Takayama T, Kokudo N. Selection criteria for repeat hepatectomy in patients with recurrent hepatocellular carcinoma. Ann Surg. 2003;238(5):703–710. | ||
Wang C, Zhang F, Fan H, et al. Sequence polymorphisms of mitochondrial D-loop and hepatocellular carcinoma outcome. Biochem Biophys Res Commun. 2011;406(3):493–496. | ||
Dienstag JL. Hepatitis B virus infection. N Engl J Med. 2008;359(14):1486–1500. | ||
Pollicino T, Cacciola I, Saffioti F, Raimondo G. Hepatitis B virus PreS/S gene variants: pathobiology and clinical implications. J Hepatol. 2014;61(2):408–417. | ||
Lu FM, Zhuang H. Management of hepatitis B in China. Chin Med J (Engl). 2009;122(1):3–4. | ||
Yu MC, Yuan JM, Govindarajan S, Ross RK. Epidemiology of hepatocellular carcinoma. Can J Gastroenterol. 2000;14(8):703–709. | ||
Seeger C, Mason WS. Hepatitis B virus biology.Microbiol Mol Biol Rev. 2000;64(1):51–68. | ||
Yang HI, Yeh SH, Chen PJ, et al; REVEAL-HBV Study Group. Associations between hepatitis B virus genotype and mutants and the risk of hepatocellular carcinoma. J Natl Cancer Inst. 2008;100(16):1134–1143. | ||
Tsai WL, Chung RT. Viral hepatocarcinogenesis. Oncogene. 2010;29(16):2309–2324. | ||
Chan HL, Tse CH, Mo F, et al. High viral load and hepatitis B virus subgenotype ce are associated with increased risk of hepatocellular carcinoma. J Clin Oncol. 2008;26(2):177–182. | ||
Yu MW, Yeh SH, Chen PJ, et al. Hepatitis B virus genotype and DNA level and hepatocellular carcinoma: a prospective study in men. J Natl Cancer Inst. 2005;97(4):265–272. | ||
Liu CJ, Chen BF, Chen PJ, et al. Role of hepatitis B viral load and basal core promoter mutation in hepatocellular carcinoma in hepatitis B carriers. J Infect Dis. 2006;193(9):1258–1265. | ||
Lin CL, Liu CH, Chen W, et al. Association of pre-S deletion mutant of hepatitis B virus with risk of hepatocellular carcinoma. J Gastroenterol Hepatol. 2007;22(7):1098–1103. | ||
Kao JH, Chen PJ, Lai MY, Chen DS. Basal core promoter mutations of hepatitis B virus increase the risk of hepatocellular carcinoma in hepatitis B carriers. Gastroenterology. 2003;124(2):327–334. | ||
Kim DW, Lee SA, Hwang ES, Kook YH, Kim BJ. Naturally occurring precore/core region mutations of hepatitis B virus genotype C related to hepatocellular carcinoma.PLoS One. 2012;7(10):e47372. | ||
Yeh CT, So M, Ng J, et al. Hepatitis B virus-DNA level and basal core promoter A1762T/G1764A mutation in liver tissue independently predict postoperative survival in hepatocellular carcinoma. Hepatology. 2010;52(6):1922–1933. | ||
Xie Y, Liu S, Zhao Y, Guo Z, Xu J. X protein mutations in hepatitis B virus DNA predict postoperative survival in hepatocellular carcinoma. Tumour Biol. 2014;35(10):10325–10331. | ||
Xie Y, Liu S, Zhao Y, et al. Precore/core region mutations in hepatitis B virus DNA predict postoperative survival in hepatocellular carcinoma. PLoS One. 2015;10(7):e0133393. | ||
Raimondo G, Costantino L, Caccamo G, et al. Non-sequencing molecular approaches to identify preS2-defective hepatitis B virus variants proved to be associated with severe liver diseases. J Hepatol. 2004;40(3):515–519. | ||
Wang HC, Huang W, Lai MD, Su IJ. Hepatitis B virus pre-S mutants, endoplasmic reticulum stress and hepatocarcinogenesis. Cancer Sci. 2006;97(8):683–688. | ||
Locarnini S, McMillan J, Bartholomeusz A. The hepatitis B virus and common mutants. Semin Liver Dis. 2003;23(1):5–20. | ||
Hagen TM, Huang S, Curnutte J, et al. Extensive oxidative DNA damage in hepatocytes of transgenic mice with chronic active hepatitis destined to develop hepatocellular carcinoma. Proc Natl Acad Sci U S A. 1994;91(26):12808–12812. | ||
Wang LH, Huang W, Lai MD, Su IJ. Aberrant cyclin A expression and centrosome overduplication induced by hepatitis B virus pre-S2 mutants and its implication in hepatocarcinogenesis. Carcinogenesis. 2012;33(2):466–472. | ||
Norder H, Couroucé AM, Magnius LO. Molecular basis of hepatitis B virus serotype variations within the four major subtypes. J Gen Virol. 1992;73(Pt 12):3141–3145. | ||
Weber B. Genetic variability of the S gene of hepatitis B virus: clinical and diagnostic impact.J Clin Virol. 2005;32(2):102–112. | ||
Pawlotsky JM. The concept of hepatitis B virus mutant escape. J Clin Virol. 2005;34(Suppl 1):S125–S129. | ||
Yamamoto K, Horikita M, Tsuda F, et al. Naturally occurring escape mutants of hepatitis B virus with various mutations in the S gene in carriers seropositive for antibody to hepatitis B surface antigen. J Virol. 1994;68(4):2671–2676. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.