Back to Journals » International Journal of Nanomedicine » Volume 12
mPEG-PLA/TPGS mixed micelles via intranasal administration improved the bioavailability of lamotrigine in the hippocampus
Authors Yu A, Lv J , Yuan F, Xia Z, Fan K, Chen G, Ren J, Lin C, Wei S, Yang F
Received 4 July 2017
Accepted for publication 17 September 2017
Published 21 November 2017 Volume 2017:12 Pages 8353—8362
DOI https://doi.org/10.2147/IJN.S145488
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Linlin Sun
Anan Yu,1,* Jieqiong Lv,1,* Fang Yuan,1 Zihua Xia,1 Kaiyan Fan,1 Gang Chen,1,2 Jialin Ren,1 Cuicui Lin,1 Shijie Wei,1,2 Fan Yang1,2
1Department of Pharmaceutics, 2Guangdong Provincial Engineering Center of Topical Precise Drug Delivery System, Guangdong Pharmaceutical University, Guangzhou, Guangdong, China
*These authors contributed equally to this work
Purpose: This study aimed to develop a novel methoxy poly(ethylene glycol)-poly(lactide) (mPEG-PLA)/D-α-tocopherol polyethylene glycol 1000 succinate (TPGS) mixed micelle drug delivery system to improve lamotrigine (LTG) distribution in the hippocampus.
Methods: LTG-loaded mPEG-PLA/TPGS mixed micelles and LTG-loaded mPEG-PLA micelles were formulated, and their characteristics, particle size, surface morphology, and release behavior in vitro were researched. Then, a microdialysis sampling technique coupled with two validated chromatographic systems was developed for the continuous measurement of the protein-unbound form of LTG in the rat plasma and hippocampus after administering two kinds of micelles and LTG solution intranasally.
Results: The drug loading and mean size of LTG-loaded micelles and LTG-loaded mixed micelles prepared with optimal formulation were 36.44%±0.14%, 39.28%±0.26%, 122.9, and 183.5 nm, respectively, with a core–shell structure. The cumulative release rate in vivo of LTG-loaded mixed micelles was 84.21% at 24 hours and showed more sustained release while that of LTG-loaded micelles was 80.61% at 6 hours. The Tmax and area under concentration-time curve from zero to time of last quantifiable concentration of LTG solution, LTG-loaded micelles, and LTG-loaded mixed micelles were 55, 35, and 15 minutes and about 5,384, 16,500, and 25,245 (min·µg)/L in the hippocampus, respectively.
Conclusion: The results revealed that LTG-loaded mPEG-PLA/TPGS mixed micelles enhanced the absorption of LTG at the nasal cavity and reduced the efflux of LTG in the brain, suggesting that the function of TPGS inhibited P-glycoprotein and LTG-loaded mPEG-PLA/TPGS mixed micelles had the potential to overcome refractory epilepsy.
Keywords: epilepsy, intranasal administration, lamotrigine, P-glycoprotein, blood brain barrier, TPGS
Introduction
Central neurological diseases seriously affect the health of people at all ages. Epilepsy is a common chronic central neurological disease with a high incidence, affecting about 65 million people worldwide,1,2 of which refractory epilepsy (RE) accounts for 30%.2 Appropriate antiepileptic drugs (AEDs) are used for reasonable and regular treatment of RE under the premise of a clear diagnosis. Although plasma concentration reaches an effective therapeutic value, the drug concentration in the pathogenic site of epilepsy remains lower than the effective therapeutic concentration, failing to satisfactorily control RE.3
The reason is that the distribution of the drug in the brain tissue is strictly controlled because the drug has to pass through the blood–brain barrier (BBB).4 Furthermore, the adenosine triphosphate (ATP)-dependent transporter protein produced by the endothelial cells of the BBB can exhaust the drugs outside the brain tissue against the concentration gradient,5 serving as a “second barrier” in the brain. According to the multidrug resistance gene theory, the main reason for the resistance of RE is that when the AEDs enter the brain, they are pumped out by these transporter proteins so that the concentration of the drugs in the brain decreases and fails to effectively suppress seizures.2 Terrell-Hall et al6 proved that the rate of permeability of rhodamine 123 across the BBB model increased 14-fold in the presence of P-glycoprotein (P-gp) inhibitor verapamil and 8-fold with the addition of cyclosporine A, indicating that P-gp limited the movement of the drug into the brain.
Intranasal administration has drawn much attention on account of the efficacy of nasal delivery of drugs to the central nervous system, as reported by many studies. After nasal delivery, drugs are taken up by the olfactory cell through the olfactory mucosa and transported into the brain, including the olfactory bulb, nucleus, amygdale, and hippocampus, along the olfactory beam, avoiding the obstruction of BBB and making it relatively easier to enter the brain.7,8 Serralheiro et al9 found that the bioavailability of lamotrigine (LTG) in brain was 116.5% comparing intranasal administration with intravenous administration in mice. Through the nasal route, drugs can avoid the obstruction of the BBB and enter the brain relatively easily.
Tocopherol polyethylene glycol 1000 succinate (TPGS) could inhibit the efflux effect of P-gp and promote drug permeation into the biofilm. Since P-gp is an ATP-dependent efflux pump, TPGS can directly affect the excretive function of P-gp by inhibiting the activity of ATP.10 TPGS not only inhibits the efflux of the brain drug but can also increase drug absorption through nasal administration because the efflux protein, such as P-gp, localized in the epithelial cells, glands, and vascular endothelial cells of nasal mucosa can decrease the drug transport from the nose to the brain.11 A study by Cho et al12 demonstrated that the speed of movement of drug lyophilized particles connected with TPGS into the nasal epithelial cells was nine times the speed of movement of particles not connected with TPGS. Therefore, suppressing P-gp in the nasal membrane to promote the transport of drugs into the brain has become an important research topic.
One of the most common REs is mesial temporal lobe epilepsy which is frequently accompanied by neurodegeneration in the hippocampus resulting in hippocampal sclerosis.13,14 LTG has been initially approved for the add-on treatment of patients with RE, but only a modest or no significant improvement has been effectively demonstrated on seizure control. Recently, several reports have identified LTG as a P-gp substrate, which may explain its limited access to the brain throughout the treatment.9
This study aimed to prepare LTG-loaded methoxy poly(ethylene glycol)-poly(lactide) (mPEG-PLA)/TPGS mixed micelles, taking advantage of TPGS to inhibit the exocytosis of P-gp and enhance the efficacy of drugs through nasal mucosa and prolong the residence time of the drug in the brain. The nasal administration route was used in this study to allow the mixed micelles to avoid BBB and enter the hippocampus and achieve effective therapeutic concentration.
Materials and methods
Drugs and reagents
LTG (with ≥99% purity) was purchased from Guangzhou Eastbang Pharmaceutical Technology Co, Ltd (Guangzhou, China). Jinan Daigang Co, Ltd (Jinan, China) provided monomethoxy-poly(ethylene glycol)-b-poly(d,l-lactide) (mPEG2000–PLA2000). TPGS was purchased from Melone Pharmaceutical Co, Ltd (Dalian, China). High-performance liquid chromatography (HPLC) grade acetonitrile and methanol were obtained from Merck KGaA (Darmstadt, Germany). An anticoagulant citrate dextrose15 (ACD) solution was prepared in the laboratory, containing 3.5 mM citric acid, 7.5 mM sodium citrate, and 13.6 mM glucose. Artificial cerebrospinal fluid16 (ACSF) consisted of 147 mM sodium chloride, 2.7 mM potassium chloride, 1.2 mM calcium chloride, and 0.85 mM magnesium chloride, and was also prepared in the laboratory. Other reagents mentioned in this study were all of analytical grade.
Experimental animals
Sprague Dawley rats, weighing 180–220 g, were of specific pathogen-free grade and obtained from Guangdong Medical Laboratory Animal Center (Guangzhou, China). The license number was SCXK (Yue) 2013–0002. The rats fasted for 12 hours before the experiment but had free access to water. All animal experiments complied with the requirements of the National Act on Experimental Animals (China) and were approved by Guangdong Pharmaceutical University Animal Ethics Committee.
Analytical method validation
The concentration of protein-unbound LTG in the blood and hippocampus dialysate was quantified accurately, and full validation of the analytical method was carried out according to the US Food and Drug Administration guidelines for the validation of bioanalytical methods,17 including limit of detection, lower limit of quantification (LLOQ), calibration curves, precision, accuracy, specificity, and stability. The specificity of LTG was evaluated by the contrast between blank dialysate, blank dialysate spiked with LTG, and samples collected after drug administration. The intraday and interday assay precisions were evaluated using samples of three different concentrations. The precisions were calculated in terms of their relative standard deviation after quantifying five replicates on the same day (intraday assay) or three consecutive days (interday assay). Accuracy was calculated by comparing the average measured concentration with the nominal concentration.
Preparation of LTG-loaded mPEG-PLA/TPGS mixed micelles
The preparation of LTG-loaded mPEG-PLA/TPGS mixed micelles was carried out by the solvent evaporation method.18 Eight factors of preparation, including stirring rate, stirring time, stirring temperature, evaporation temperature, ratio between methanol and water, ratio between mPEG-PLA and TPGS, concentration of mPEG-PLA, and drug dosage, were taken into consideration. The preparation of LTG-loaded mPEG-PLA micelles was similar to that of the mixed micelles.
Orthogonal experiment was conducted to optimize the formulation of LTG-loaded mPEG-PLA/TPGS mixed micelles according to the standard [L16(45)] table (Table 1). The drug-loading efficiency was used as an indicator to measure the quality of the preparation. Based on the results of the single-factor analysis (data not shown), five major factors, including drug dosage, concentration of mPEG-PLA, ratio of mPEG-PLA to TPGS, ratio of methanol to water, and stirring rate, and four levels for each factor were selected and arranged.
Characterization of micelles
Particle size determination
Dynamic light scattering19 (Delsa Nano C; Beckman Coulter, Inc, Brea, CA, USA) was used to measure the mean particle size and polydispersity index (PDI) of two kinds of micelles. The micelle solution was diluted with distilled water to have an appropriate intensity according to the limit of the instrument.
Surface morphology
The morphological detection of the two kinds of micelles was performed using a transmission electron microscope (TEM; JEM-100CXII; JEOL, Tokyo, Japan) after negative staining with a phosphotungstic acid solution (2.0% w/v).
Release in vitro
The in vitro release behavior of LTG-loaded micelles and LTG-loaded mixed micelles was monitored by the dialysis method. An appropriate amount of LTG-loaded micelles and LTG-loaded mixed micelles solution was introduced in a dialysis bag (molecular weight cutoff 500) that was tightened and immersed fully into the release medium at 37°C. According to the guidelines of the in vitro release of sustained release drug of Chinese pharmacopoeia, phosphate-buffered saline (pH =6.5) including 0.1% Tween 80 was chosen as the dissolution medium to reach the sink condition and sequentially stirred at 100 rpm for 24 hours. In a predetermined interval, 1 mL of the dissolution medium was taken out and replaced with an equal volume of fresh medium. An LTG stock solution was prepared under the same condition as control. The fit tests of five models, including zero-order equation, first-order equation, Higuchi equation, Ritger–Peppas equation, and biexponential and biphase equation, were performed using the data of release in vitro.
The concentration of LTG in the release medium was measured by HPLC. The HPLC system (Agilent 1260; Agilent Technologies, Santa Clara, CA, USA) consisted of a quaternary pump and an ultraviolet (UV) detector. LTG in the samples was separated using a Phenomenex C18 column (Phenomenex, Torrance, CA, USA; 25×4.6 mm internal diameter; particle size 5 μm) maintained at a temperature of 40°C. The mobile phase was composed of acetonitrile −20 mM ammonium acetate (pH 6.5) (28:72, v/v) and the flow rate was set at 0.8 mL/min. The UV detector was set at 310 nm and the injection volume at 20 μL.
LTG concentration in plasma sampled by microdialysis
Microdialysis is a neoteric sampling technique designed based on the principle of diffusion and permeability of the semipermeable membrane.20 The most important advantage of microdialysis for sampling and studying drug delivery into the brain is its ability to measure the unbound drug concentration in a single experimental animal over a period of time.21 Microdialysis could reduce the experimental errors caused by individual differences and be widely used in drug pharmacokinetic studies of blood, brain, and other tissues.
After anesthetizing the rats with 20% (g/mL) urethane (7 mL/kg) intraperitoneally, the blood microdialysis probe was implanted into the jugular vein toward the right atrium of rats and then perfused with ACD solution at a flow rate of 2 μL/min for 1.5 hours to stabilize. Then, LTG-loaded mPEG-PLA/TPGS mixed micelles, LTG-loaded mPEG-PLA micelles, and LTG solution (2 mg/kg) were administered intranasally. The sampling interval was 15 minutes, and the samples were preserved at 4°C before HPLC analysis. The analytical method for assessing drug concentration in plasma samples was the same as that of in vitro release analysis and the midpoints of the sampling times were used for plasma LTG concentration–time profiles.
LTG concentration in the hippocampus sampled by microdialysis
A probe with a dialyzing membrane of 2 mm was used for brain sampling. The rats were anesthetized with an intraperitoneal dose of 20% (g/mL) urethane (7 mL/kg) and then mounted on a stereotactic frame. An incision was made in the scalp, and a small hole was drilled for implanting the brain microdialysis probe. A guide cannula was implanted into the hippocampus according to the Paxinos and Watson atlas22 (coordinates: 5.1 mm posterior to bregma, 5.0 mm lateral to midline, and 7.0 mm lower to tip). A microdialysis probe was slowly implanted via the guiding cannula into the hippocampus of the rat. The brain microdialysis probe was then flushed with ACSF solution at a flow rate of 2.0 μL/min and continued for the duration of the experiment. Brain samples were drawn every 10 minutes after administration of LTG, until 8 hours. The midpoints of the sampling times were used for hippocampus LTG concentration–time profiles.
Hippocampus dialysate analysis was then performed on an ACQUITY Ultra Performance Liquid Chromatography (UPLC) System (Waters Corporation, Milford, MA, USA). Separation was carried out at 40°C on an ACQUITY UPLC C18 column (100×2.1 mm internal diameter, 1.8 μm; Waters Corporation) with gradient elution water (containing 5 mM ammonium acetate) and acetonitrile as the mobile phase. The flow rate was set at 0.3 μL/min. The injection volume was 2 μL.
Recovery assessment of blood and hippocampus microdialysis probes
The microdialysis system consisted of a microdialysis syringe (1 mL, MDN-0100; BASi, Mt Vernon, IN, USA), a Bee syringe pump, and a fraction collector (CULEX fraction collector; BASi). Commercially available microdialysis probes (MD-2200; BASi) with membrane lengths of 5 and 2 mm were used for plasma and hippocampus sampling, respectively.
In vivo recovery was evaluated using a retrodialysis method, which measured the loss (extraction ratio) of LTG via the probe.23 Microdialysis probes were implanted for plasma and hippocampus sampling as described in the “LTG concentration in plasma sampled by microdialysis” and “LTG concentration in the hippocampus sampled by microdialysis” sections; 1 μg/mL and 25 ng/mL of LTG were flushed via the blood probe and brain probe, respectively. The perfusate (Cperf) and dialysate (Cdial) concentrations of LTG were determined using HPLC and UPLC–mass spectrometry (MS). In vivo relative recovery (Rdial) of LTG across the microdialysis probe was calculated by the following equation: Rdial = (Cperf − Cdial)/Cperf.
Pharmacokinetic data and statistical analysis
Curves of various dialysate concentration data versus sampling time for LTG (Cm) were converted into protein-unbound concentrations (Cu) using the following equation: Cu = Cm/Rdial. The pharmacokinetic parameters of LTG were calculated by a non-compartmental method using Drug Analysis System 3.1.1 software package.
Results
Preparation of LTG-loaded mixed micelles and LTG-loaded micelles
The optimized formulation of LTG-loaded mixed micelles was determined by the result of the orthogonal test in Table 2. A total of 20 mg of mPEG-PLA and 15 mg of LTG were dissolved in 3 mL of methanol. Then, 8 mg of TPGS was dissolved in 18 mL of water. The organic mixture was then added to the TPGS solution dropwise and stirred at 1,200 rpm for 0.5 hours. Based on the results of variance analysis, the most significant factors were stirring speed, the ratio of methanol and water, mPEG-PLA concentration, drug dosage, the ratio of TPGS and mPEG-PLA, and there were significant differences among the five factors. The drug loadings of the optimal formulation of LTG-loaded mixed micelles and LTG-loaded micelles were 39.28%±0.26% and 36.44%±0.14%, respectively.
Characterization of the micelles
As shown in Figure 1, the average particle size of the optimal formulation of LTG-loaded micelles and LTG-loaded mixed micelles were 122.9 and 183.5 nm, respectively. Their PDIs were 0.168 and 0.238, respectively, with a single-peak distribution, indicating a uniform particle size distribution.
  | Figure 1 Particle size and the distribution of LTG-loaded micelles: (A) LTG-loaded micelles, (B) LTG-loaded mixed micelles. |
The morphology of the micelle was observed by a TEM. The TEM diagrams of the blank micelle, LTG-loaded micelle, blank mixed micelle, and LTG-loaded mixed micelle are shown in Figure 2. Whether it was a blank micelle or a drug-loaded micelle, a clear core–shell structure was formed. The black disk was the hydrophobic core of the micelle that acted as a container for the insoluble drug.
  | Figure 2 TEM images: (A) blank micelle, (B) LTG-loaded micelle, (C) blank mixed micelle, (D) LTG-loaded mixed micelle. |
The release behavior of LTG-loaded micelles and LTG-loaded mixed micelles is shown in Table 3 and Figure 3, which were most similar to the kinetic charateristics of biexponential and biphase equation, indicating that the release of LTG from micelles could be divided into two stages: the drug released rapidly in the first stage and then slowly in the second stage. The cumulative release rate of LTG-loaded micelles reached 80.61% at 6 hours, while that of the LTG-loaded mixed micelles was 84.21% at 24 hours. Both of them had some bursts, but the release of LTG-loaded micelles was faster than that of LTG-loaded mixed micelles. The reason for the burst release phenomenon was that some drugs were not distributed in the core of the micelle but in the palisade layer. The sustained release of LTG-loaded mixed micelle could decrease the fluctuation of plasma concentration and the side effect of drugs.
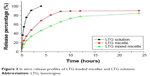  | Figure 3 In vitro release profiles of LTG-loaded micelles and LTG solution. |
Pharmacokinetics of LTG in plasma
The HPLC–UV detection method was employed to separate LTG from blood dialysate. The linearity of each calibration curve, ranging from 0.1 to 10 μg/mL, was verified in every trial, and the correlation coefficient (R2) was >0.995. For blood analysis, the overall precisions (reflex sympathetic dystrophy [RSD], %) ranged from 0.14% to 3.29% and accuracies (bias, %) from 2.2% to 8.34%. Accuracy and precision values within ±15% were acceptable. The LLOQ of LTG was determined to be 50 ng/mL.
The concentration–time curves of free form LTG in plasma after the administration of LTG (2 mg/kg, intranasal) in various groups, including the groups of LTG solution, LTG-loaded micelles, and LTG-loaded mixed micelles, are shown in Figure 4. The plasma concentration arrived at a peak of 0.75 μg/mL after intranasal administration of LTG solution for 7.5 minutes, followed by a sharp decline to about 0.17 μg/mL. The plasma concentration fluctuated at about 0.36 μg/mL 22.5–52.5 minutes after intranasal administration of LTG-loaded micelles, and the concentration did not appear to have a downward trend until 67.5 minutes. The plasma concentration fluctuated at about 0.45 μg/mL 15–55 minutes after intranasal administration of LTG-loaded mixed micelles. The concentration appeared to have a downward trend in 60 minutes, but it still remained higher than that of the LTG-loaded micelles. The pharmacokinetic parameters of LTG in the plasma of different groups are presented in Table 4. The area under the concentration–time curve (AUC0–t) of the groups of LTG solution, LTG-loaded micelles, and LTG-loaded mixed micelles was 23.04±1.42, 50.7303±0.86, and 62.51±0.84 (min·μg)/L and the terminal elimination half-life (t1/2z) was 52.8435±30.52, 106.7317±33.66, and 108.99±56 minutes, respectively.
  | Figure 4 Concentration–time profile of LTG in plasma after nasal administration. |
Pharmacokinetics of LTG in the hippocampus
The UPLC–MS detection method was adopted to separate LTG from brain samples. The linearity of each calibration curve, ranging from 1 to 100 ng/mL, was verified, and the coefficient of determination (R2) was found to be >0.995. For brain analysis, overall precisions (RSD, %) ranged from 0.28% to 5.91% and accuracies (bias, %) from 0.29% to 6.93%. The LLOQ of LTG was determined to be 0.5 ng/mL.
Figure 5 shows the concentration–time profiles of protein-unbound LTG in the hippocampus after LTG administration (2 mg/kg, intranasal) in various groups, including the groups of LTG solution, LTG-loaded micelles, and LTG-loaded mixed micelles. The curves showed that the concentration in the hippocampus reached a peak of 197.3 ng/mL after administering the LTG solution for 55 minutes, followed by a sharp decline to about 20 ng/mL. The concentration of LTG-loaded micelles in the hippocampus fluctuated at about 50 ng/mL 35–310 minutes after drug administration. The concentration in the hippocampus fluctuated at about 60 ng/mL 15–440 minutes after administering LTG-loaded mixed micelles. The pharmacokinetic parameters of LTG in the hippocampus of different groups are presented in Table 5. AUC0–t of the groups of LTG solution, LTG-loaded micelles, and LTG-loaded mixed micelles was 5,383.578, 16,500.479, and 25,245.019 (min·μg)/L, respectively.
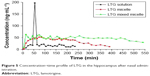  | Figure 5 Concentration–time profile of LTG in the hippocampus after nasal administration. |
In vivo recovery of LTG from microdialysis probes
The average in vivo recoveries (%) of microdialysis probes of LTG were 58.27%±0.62% in the blood and 15.79%±0.38% in the hippocampus (n=3).
Discussion
Intranasal administration can directly transport LTG from the nose to the brain by circumventing the BBB and TPGS in the nasal membrane could promote the transport of drugs into the brain, and in the endothelial cells of BBB, could inhibit the efflux of brain drug. Therefore, LTG-loaded micelles could be successfully prepared and delivered to the hippocampus by intranasal administration in this study. The result showed that mPEG-PLA/TPGS mixed micelles could improve the bioavailability of LTG in the hippocampus by increasing nasal drug absorption and decreasing brain drug efflux. The major findings of this study are as follows.
- Some differences existed between the LTG-loaded mPEG-PLA mixed micelles and the LTG-loaded mPEG-PLA micelles in terms of particle size and morphology. The reason why the particle size of the mixed micelles was larger than that of the micelles might be as follows. In the shell of the micelles, mPEG-PLA and TPGS were intertwined with each other to form a relatively thick shell layer. Moreover, TPGS contained aromatic rings that increased the volume of the nucleus. The difference between the blank micelles and the drug-loaded micelles lay in the shape of the core; when the micelle contained drugs, the interaction between drugs and polymers made the kernel more compact. The difference between micelles and mixed micelles was the boundary of the shell, and the shell of the mixed micelle was formed by the interaction of TPGS and mPEG-PLA, which made the shell compact and regular. Some LTG distribution was seen in the barrier layer of the micelle using TEM, which was because the solubility of LTG in water was 170 μg/mL. Compared with other highly lipid soluble drugs, such as nimodipine and curcumin, LTG was also soluble in water. Therefore, part of the drugs would be distributed between the micelle core and the shell. This phenomenon might also be a good interpretation for the reason why the release of drugs from the core of the micelle was faster than that in the case of the mixed micelle.
- The plasma and hippocampus concentrations showed that LTG-loaded mPEG-PLA/TPGS mixed micelles exhibited a rapid and enhanced penetration efficiency compared with the LTG-loaded mPEG-PLA micelles and free LTG. On comparing free LTG and LTG-loaded mPEG-PLA micelles, the micelle served as a sustained-release preparation. The drug concentration was stable for a certain period of time, followed by a slow decline. This action could reduce the production of side effects on one hand, and prolong the control of epilepsy on the other hand. On comparing LTG-loaded mPEG-PLA micelles and LTG-loaded mPEG-PLA/TPGS mixed micelles, mixed micelles showed a more profound effect. LTG could be absorbed faster by means of the mixed micelles. In the hippocampus of the brain, the concentration of LTG was stable for a relatively longer period of time with no downward trend.
- The increased blood and brain penetration of LTG might partially be attributed to the inhibition of efflux of LTG by P-gp located on the membrane of the BBB and the blood–cerebrospinal fluid barrier. Recently, the crucial role of efflux transporters in drug absorption and disposition has gained considerable attention.5,24,25 P-gp, the most extensively studied ATP-binding cassette transporter, serves as a biological barrier by eliminating toxic substances and xenobiotics out of the cells.5,26 The hypothesis that inhibition of P-gp improved the bioavailability of drugs, which were the substrates of this efflux transporter, has gained widespread recognition.25,27 The results indicated that intranasal administration of LTG-loaded mPEG-PLA/TPGS mixed micelles might serve as a promising drug delivery system to promote the brain delivery of AEDs.
Conclusion
AEDs could not achieve an effective therapeutic concentration in the hippocampus because of the presence of the BBB and the efflux of P-gp. Micelles could efficiently solubilize poorly soluble LTG and deliver it by intranasal administration, helping drugs to pass through the BBB. The results of the present study indicated that mPEG-PLA/TPGS mixed micelle exhibited significantly enhanced and rapid delivery of LTG to the brain. Testing data indicated that Tmax and the MRT0–t of mPEG-PLA/TPGS mixed micelle were the smallest and the largest, respectively, compared with those of the mPEG-PLA micelle and solution. Also, the bioavailability of mPEG-PLA/TPGS mixed micelle in the hippocampus was four times that of the solution, suggesting that TPGS could inhibit P-gp in the epithelial cells of nasal mucosa and the BBB to improve the absorption of LTG in the nasal cavity and reduce the excretion of LTG in the hippocampus. In conclusion, the mPEG-PLA/TPGS mixed micelle is a promising vehicle for targeting delivery of AEDs and other drugs to the brain, thereby having implications in treating central neurological diseases, especially RE.
Acknowledgments
This study was supported by grants from the Guangdong Provincial Science and Technology projects (2013B021800091) and Medical Scientific Research Foundation of Guangdong Province, China (A2015585).
Disclosure
The authors report no conflicts of interest in this work.
References
Rao G, Mashkouri S, Aum D, Marcet P, Borlongan CV. Contemplating stem cell therapy for epilepsy-induced neuropsychiatric symptoms. Neuropsychiatr Dis Treat. 2017;13:585–596. | ||
Chouchi M, Kaabachi W, Klaa H, Tizaoui K, Turki IB, Hila L. Relationship between ABCB1 3435TT genotype and antiepileptic drugs resistance in epilepsy: updated systematic review and meta-analysis. BMC Neurol. 2017;17(1):32. | ||
Xiong J, Mao DA. Research progress on the role of ABC transporters in the drug resistance mechanism of intractable epilepsy. Biomed Res Int. 2015;2015:194541. | ||
Ronaldson PT. Blood–brain barrier integrity and glial support: mechanisms that can be targeted for novel therapeutic approaches in stroke. Curr Pharm Des. 2012;18(25):3624–3644. | ||
Mesev EV, Miller DS. Ceramide 1-phosphate increases P-glycoprotein transport activity at the blood–brain barrier via prostaglandin E2 signaling. Mol Pharmacol. 2017;91(4):373–382. | ||
Terrell-Hall TB, Ammer AG, Griffith JIG, Lockman PR. Permeability across a novel microfluidic blood–tumor barrier model. Fluids Barriers CNS. 2017;14:3. | ||
Lochhead JJ. Intranasal delivery of biologics to the central nervous system. Adv Drug Deliv Rev. 2012;64:614–628. | ||
Renner DB, Svitak AL, Gallus NJ, Ericson ME, Frey WH 2nd, Hanson LR. Intranasal delivery of insulin via the olfactory nerve pathway. J Pharm Pharmacol. 2012;64:1709–1714. | ||
Serralheiro A, Alves G, Fortuna A. Direct nose-to-brain delivery of lamotrigine following intranasal administration to mice. Int J Pharm. 2015; 490:39–46. | ||
Collnot EM, Baldes C, Schaefer UF, Edgar KJ, Wempe MF, Lehr CM. Vitamin E TPGS P-glycoprotein inhibition mechanism: influence on conformational flexibility, intracellular ATP levels, and role of time and site of access. Mol Pharm. 2010;3:642–651. | ||
Molinas A, Sicard G. Functional evidence of multidrug resistance transporters (MDR) in rodent olfactory epithelium. PLoS One. 2012; 7(5):e36167. | ||
Cho HJ, Balakrishnan P, Chung SJ, Shim CK, Kim DD. Evaluation of protein stability and in vitro permeation of lyophilized polysaccharides-based microparticles for intranasal protein delivery. Int J Pharm. 2011; 416:77–84. | ||
Bencurova P, Baloun J, Musilova K, et al. MicroRNA and mesial temporal lobe epilepsy with hippocampal sclerosis: whole miRNome profiling of human hippocampus. Epilepsia. Epub 2017 Aug 16. | ||
Asadi-Pooya AA. Age at onset in patients with medically refractory temporal lobe epilepsy and mesial temporal sclerosis: impact on clinical manifestations and postsurgical outcome. Seizure. 2015;30:42–45. | ||
Giraldo CE, Álvarez ME, Carmona JU. Effects of sodium citrate and acid citrate dextrose solutions on cell counts and growth factor release from equine pure-platelet rich plasma and pure-platelet rich gel. BMC Vet Res. 2015;11:60. | ||
Tamano H, Nishio R, Shakushi Y, et al. In vitro and in vivo physiology of low nanomolar concentrations of Zn2+ in artificial cerebrospinal fluid. Sci Rep. 2017;7:42897. | ||
FDA, US Department of Health and Human Services, Center for Drug Evaluation and Research (CDER), Center for Veterinary Medicine (CVM). Draft guidance for industry: bioanalytical method validation (revised). 2013. Available at https://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm368107.pdf. Accessed October 9, 2017. | ||
Huang S, Yu X, Yang L, et al. The efficacy of nimodipine drug delivery using mPEG-PLA micelles and mPEG-PLA/TPGS mixed micelles. Eur J Pharm Sci. 2014;63:187–198. | ||
Sotoudegan F, Amini M, Faizi M, Aboofazeli R. Nimodipine-loaded Pluronic® block copolymer micelles: preparation, characterization, in-vitro and in-vivo studies. Iran J Pharm Res. 2016;15(4):641–661. | ||
Simmel F, Kirbs C, Erdogan Z, Lackner E, Zeitlinger M, Kloft C. Pilot investigation on long-term subcutaneous microdialysis: proof of principle in humans. AAPS J. 2013;15(1):95–103. | ||
Boddu SH, Gunda S, Earla R. Ocular microdialysis: a continuous sampling technique to study pharmacokinetics and pharmacodynamics in the eye. Bioanalysis. 2010;2(3):487–507. | ||
Paxinos G, Watson C. The Rat Brain in Stereotaxic Coordinates. 6th ed. San Diego: Elsevier Academic Press; 2007. | ||
Zhuang L, Xia H, Gu Y, Derendorf H, Li Y, Liu C. Theory and application of microdialysis in pharmacokinetic studies. Curr Drug Metab. 2015;16(10):919–931. | ||
Sasabe H, Shimokawa Y, Shibata M, et al. Antitubercular agent delamanid and metabolites as substrates and inhibitors of ABC and solute carrier transporters. Antimicrob Agents Chemother. 2016;60(6): 3497–3508. | ||
Mateus A, Treyer A, Wegler C, Karlgren M, Matsson P, Artursson P. Intracellular drug bioavailability: a new predictor of system dependent drug disposition. Sci Rep. 2017;7:43047. | ||
El-Awady R, Saleh E, Hashim A, et al. The role of eukaryotic and prokaryotic ABC transporter family in failure of chemotherapy. Front Pharmacol. 2016;7:535. | ||
Xu W, Ling P, Zhang T. Polymeric micelles, a promising drug delivery system to enhance bioavailability of poorly water-soluble drugs. J Drug Deliv. 2013;2013:340315. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





