Back to Journals » Journal of Asthma and Allergy » Volume 13
MP-AzeFlu Improves the Quality-of-Life of Patients with Allergic Rhinitis
Authors van Weissenbruch R , Klimek L, Gálffy G , Emmeluth M, Koltun A , Kopietz F , Nguyen DT, Kuhl HC, Pohl W, Scadding GK , Price D , Mullol J
Received 29 August 2020
Accepted for publication 29 October 2020
Published 2 December 2020 Volume 2020:13 Pages 633—645
DOI https://doi.org/10.2147/JAA.S277734
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Luis Garcia-Marcos
Ranny van Weissenbruch,1 Ludger Klimek,2 Gabriella Gálffy,3 Melanie Emmeluth,4 Arkady Koltun,5 Ferdinand Kopietz,4 Duc Tung Nguyen,6 Hans Christian Kuhl,4 Wolfgang Pohl,7 Glenis K Scadding,8 David Price,9,10 Joaquim Mullol11
1Department of ENT Head and Neck Surgery, Wilhelmina Ziekenhuis, Assen, the Netherlands; 2Department of Otorhinolaryngology and Head and Neck Plastic Surgery, Zentrum für Rhinologie und Allergologie, Wiesbaden, Germany; 3Pulmonology Hospital, Torokbalint, Hungary; 4Global Medical Affairs, MEDA Pharma GmbH & Co. KG (A Mylan Company), Bad Homburg, Germany; 5Mylan, Inc., Canonsburg, PA, USA; 6GBK Clinical Affairs, MEDA Pharma GmbH & Co. KG (A Mylan Company), Bad Homburg, Germany; 7Department of Respiratory and Pulmonary Diseases, Karl Landsteiner Gesellschaft, Institute of Clinical and Experimental Pneumology, Vienna, Austria; 8Roy National Throat Nose and Ear Hospital, London, UK; 9Centre of Academic Primary Care, Division of Applied Health Sciences, University of Aberdeen, Aberdeen, UK; 10Observational and Pragmatic Research Institute, Singapore, Singapore; 11Rhinology Unit & Smell Clinic, ENT Department, Hospital Clinic Barcelona IDIBAPS University of Barcelona, CIBERES, Barcelona, Catalonia, Spain
Correspondence: Ranny van Weissenbruch
Wilhelmina Ziekenhuis, Europaweg-Zuid 1, Assen 9401 RK, the Netherlands
Tel +31 592 325229
Fax +31 592 325226
Email [email protected]
Purpose: Patients with poorly controlled allergic rhinitis (AR) experience nasal symptoms, sleep disturbances, activity impairment, and decreased quality-of-life (QoL). MP-AzeFlu is safe and effective for moderate-to-severe seasonal and perennial AR, but its impact on QoL requires investigation in the real-world, especially among phenotypes of immunoglobulin (Ig)E-mediated AR. This subanalysis of an observational study evaluated response to MP-AzeFlu via assessment of sleep quality and trouble with daily activities.
Patients and Methods: This multicenter, prospective, non-interventional, real-life study included a convenience sample of patients with a history of moderate-to-severe AR presenting with acute AR symptoms (visual analog scale [VAS] ≥ 50 mm). Over approximately 14 days of treatment with MP-AzeFlu (137 μg azelastine HCL and 50 μg fluticasone propionate administered via single 0.137-mL spray in each nostril twice daily), changes in sleep quality and trouble with daily work, school, social, and outdoor activities were evaluated using a VAS for the entire study population and for four subgroups based on IgE response phenotype. VAS scores ranged from “not at all troubled” (0 mm) to “extremely troubled” (100 mm).
Results: Following MP-AzeFlu treatment, mean VAS scores for sleep quality impairment and work or school impairment decreased from 55.2 mm at baseline to 22.1 mm and 57.6 mm at baseline to 23.0 mm, respectively, after ∼ 14 days. Similar results were observed for mean VAS scores for impairment of social activity (55.1 mm to 22.4 mm) and impairment of outdoor activity (64.4 mm to 25.0 mm). For all VAS scores, results were similar across populations, regardless of phenotype of IgE-mediated disease, comorbidity, age, and sex.
Conclusion: MP-AzeFlu relieves symptoms and improves patient-reported QoL, illustrated by better sleep quality and less impairment of work, school, social, and outdoor activities after 14 days. The QoL benefits of MP-AzeFlu were consistent regardless of the phenotype of IgE-mediated disease.
Registration: Clinical Trial Registration (CTR) Number: EUPAS23075. Trial Register Date: March 12, 2018. First patient visit; Last patient visit: February 2018; April 2019.
Keywords: azelastine hydrochloride, daily activities, fluticasone propionate, sleep
Introduction
Allergic rhinitis (AR) comprises a variety of nasal symptoms, including congestion, itching, rhinorrhea, sneezing, and loss of smell.1 AR is frequently accompanied by ocular symptoms, such as itchy or watery eyes and redness, which are referred to as allergic rhinoconjunctivitis.1–3 According to Allergic Rhinitis and its Impact on Asthma (ARIA) severity criteria, the majority of patients experience moderate-to-severe disease.4
Severity of disease can have a profound impact on quality-of-life (QoL; eg, sleep disturbances, emotional problems, impairment in activities of daily life or social functioning),1 and on work productivity and school performance.1,5 AR impairs work productivity to a greater degree than hypertension and type 2 diabetes.5 The coexistence of AR in children with asthma further increases the burden of sleep-related breathing disorders.6
A study of adults with allergic occupational rhinitis demonstrated impaired QoL and work productivity.7 In a study of 101 adolescents and 41 children with moderate and severe persistent AR, medical treatment failure was associated with worse QoL outcomes.8 Furthermore, there was a significant correlation between visual analog scale (VAS) scores for nasal symptoms and QoL questionnaires.8
Results from a systematic review demonstrate that approximately 2.3% of 1,666 participants from a pooled analysis of six studies using the Work Productivity and Activity Impairment Allergy Specific (WPAI-AS) questionnaire missed work time, with 35.5% of 6,536 participants from a pooled analysis of 11 studies using the WPAI-AS questionnaire experiencing impaired work performance resulting from AR.9 Symptom severity was associated with a greater impact of AR on work productivity. Pharmacologic treatment of AR had a beneficial effect on work productivity. A study of physical activity in 1,137 German teens (mean age=15.6 years; 47% male) using 1-week accelerometry revealed an independent association between asthma and rhinitis and low physical activity in boys, but not in girls.10
Using the Medical Expenditure Panel Survey, self-reported information on demographic and socioeconomic characteristics, and health conditions, insurance status, healthcare use, and missed workdays were collected.11 Among 225.1 million adults, the estimated prevalence of AR was 7.9±0.3%. AR was associated with significantly increased limitations in work, social, and cognitive activity.11 In a case-control study of 1,834 students aged 15–17 years sitting for examinations in mathematics, English, and science, those reporting AR symptoms on an examination day were 40% more likely to drop a grade between practice and final examinations compared with students who did not report AR symptoms.12 Furthermore, those who reported taking sedating antihistamines during examinations were 70% more likely to drop a grade.12 Uncontrolled AR has also been associated with a negative impact on sexual functioning and impaired driving ability.13–15
MP-AzeFlu is indicated for the relief of symptoms of moderate-to-severe seasonal and perennial AR and has proved effective for the relief of AR symptoms;16–20 however, its impact on patient QoL under real-world conditions has not been reported in the literature to date. The Rhinitis Quality-of-Life Questionnaire (RQLQ) was used previously in the categorization of AR severity, but the impact of treatment on RQLQ scores was outside the scope of the study.21
AR symptoms are often assessed with a VAS, a simple, validated, and widely used instrument.22 A VAS was used for assessment of QoL in this study. The primary purpose of this real-life observational study was to investigate associations between patient-reported changes in sleep quality and trouble with daily work and social activities, and ~14 days of treatment with MP-AzeFlu in routine clinical practice.
Patients and Methods
Design
This multinational, multicenter, prospective, non-interventional real-life observational study was conducted in six European countries (Austria, Germany, Czech Republic, Hungary, the Netherlands, and Ireland) to evaluate the use of MP-AzeFlu. The recruitment period lasted 14 months, from February 21, 2018 (recruitment of first patient), to April 30, 2019 (date of last electronic case report form submission).
Patients attended an inclusion visit (Day 0) and a control visit after ~14 days; alternatively, the patient card could be sent by mail following the treatment period. The inclusion decision had to be made independently from and after the decision to prescribe MP-AzeFlu to the patient. Symptom severity on days 0, 1, 3, 7, and ~14, and quality of sleep and daily activities on days 0, 7, and ~14 were assessed by the patient on the VAS printed on the patient card.
Patients
The treatment population for this study was a convenience sample of adolescent and adult patients who had a history of moderate-to-severe AR for which MP-AzeFlu had been prescribed for the first time. Physicians who routinely managed patients with AR and used a VAS for symptom assessment of patients with AR as recommended by MAladies Chroniques pour un VIeillissement Actif en Languedoc-Roussillon (MACVIA)/ARIA guidelines were invited to participate.
To be included in the study, all the following criteria had to be met:
- First time prescription of MP-AzeFlu.
- History of moderate-to-severe symptoms of AR.
- Age ≥12 years.
- Acute symptoms of AR on the day of inclusion (VAS score ≥50 mm).
- Written informed consent by patient and (if applicable) caregiver for patients aged ≤18 years.
- Ability to understand the instructions for use of the medication according to the summary of product characteristics and patient information leaflet.
- Possibility to return the completed patient card.
Patients were not eligible if at least one of the following exclusion criteria were met:
- Known allergic reactions to MP-AzeFlu nasal spray or any of its ingredients.
- Pregnancy (or planned pregnancy during the study) or breastfeeding.
- Inability to provide informed consent.
- Missing consent for the collection, archiving, or transfer of personal data in the context of this study and in accordance with the observational plan.
Study Treatments
All patients received MP-AzeFlu (Dymista®; Meda Pharmaceuticals, Inc., a Mylan Company). MP-AzeFlu was dosed as outlined in the country-specific summary of product characteristics: 1 spray in each nostril twice daily. Each 0.137-mL spray delivers 137 µg of azelastine hydrochloride and 50 µg of fluticasone propionate.17 Physicians ensured the patient properly understood the instructions for use, as specified in the summary of product characteristics and patient information leaflet.
Assessments of Effectiveness
On days 0, 1, 3, 7, and ~14, each patient recorded AR symptoms on the printed VAS form provided in a patient card, marking with a pencil the appropriate value on a printed, single-line VAS (0–100 mm), ranging from “not at all bothersome” (0 mm) to “extremely bothersome” (100 mm).
On days 0, 7, and ~14 after the start of treatment, each patient assessed sleep and troublesomeness in daily activities for the previous 7 days on the VAS for the following domains: impairment of sleep quality, impairment of daily school or work activity, impairment of social activity, and impairment of outdoor activity. VAS scores were printed on a patient card and included a range from “not at all troubled” (0 mm) to “extremely troubled” (100 mm).
Sleep quality and daily activities were assessed for the entire study population, as well as for four different phenotype subgroups (derived from the novel classification of immunoglobulin [Ig]E-mediated diseases provided by the MeDALL paper) to determine potential differences among heterogenous allergic phenotypes,23 including:
- Monoclonal IgE response (IgE response restricted to one environmental allergen without family history).
- Polyclonal IgE response (polyclonal IgE response to >5 environmental allergens with family history).
- Nonallergic IgE response (patients with IgE test but no increased total IgE value without family history).
- Intermediate phenotype (polyclonal IgE response to >5 environmental allergens without family history, or IgE response restricted to 2–5 allergens).
Statistical Methods
Statistical analyses were performed using the statistical software package SAS® (SAS Institute Inc.; Cary, NC, USA) version 9.4 or higher. Continuous variables were summarized by number (N), mean, and standard error. Categorical variables were presented in frequency distribution tables with N and percentage. Percentages are relative to the total number of patients, if not stated otherwise. For the subgroup analyses, the percentages are relative to the total number of patients in the respective subgroup. Data analyses were explorative. Analysis of covariance for repeated measurements was used to assess post-baseline changes of VAS regarding overall symptoms of AR and activity impairments. The primary endpoint was displayed using the 95% Wilson confidence interval (CI). P-values<0.05 were considered statistically significant.
Results
Patients
Overall, 1,154 patients were enrolled; 51 were excluded because complete data were not submitted by the investigator. A total of 1,103 patients were included in the analysis (male, n=474; female, n=624 [56.6%]; Table 1). Of these, 82 were aged from 12–17 years, 937 were aged from 18–65 years, and 84 were older than 65 years. The mean age was 40.0 years (range=12–84 years).
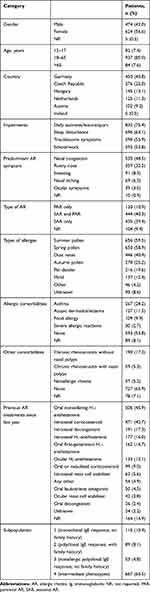 |
Table 1 Demographic and Baseline Characteristics |
A total of 96.7% of patients had moderate-to-severe AR (3.3% had mild AR) according to ARIA classification. The majority of patients (83%) had used at least one treatment for symptomatic AR in the past year, and 62% used two or more allergy medications in the past year. A total of 115 patients were included in subpopulation 1, 89 made up subpopulation 2, 53 made up subpopulation 3, and 667 patients were included in subpopulation 4.
Patient cards were evaluable for 1,098 patients at Day 0, 1,012 patients on the last day (~Day 14) when assessing sleep quality, and 1,013 patients on the last day (~Day 14) when assessing other domains.
Effectiveness of MP-AzeFlu
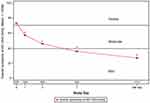
The mean VAS scores of overall AR symptoms were 73.2 mm at Day 0, 57.2 mm at Day 1, 46.3 mm at Day 3, 36.1 mm at Day 7, and 27.2 mm on the last day (Figure 1). Patients reported severe disease at baseline (>70 mm), which improved to mild disease (<40 mm) following treatment with MP-AzeFlu.24 The responder rate, defined as a documented AR-VAS score of <50 mm at least once through the end of the study, was 86.6% (95% CI=84.5–88.5; 944 patients). These patients were regarded as responders with controlled symptoms.
The mean patient-reported baseline VAS scores were 55.2 mm for impairment of sleep quality, 57.6 mm for impairment of daily work/school activity, 55.1 mm for impairment of social activity, and 64.4 mm for impairment of outdoor activity. Day 7 and Day 14 patient cards revealed substantial improvements in all QoL metrics. The mean impairment of sleep quality (mean VAS change) decreased from 55.2 mm to 29.8 mm (Day 7) to 22.1 mm at 14 days. Significant changes were found from baseline for Day 7 and the last day (P<0.0001; Figure 2A). Similar results were seen for all subpopulations (P<0.0001; Figure 2B).
The mean impairment of daily work or school activity decreased from 57.6 mm to 30.4 mm (Day 7) to 23.0 mm at 14 days. Significant changes were found from baseline for Day 7 and the last day (P<0.0001; Figure 3A). Similar results were seen among all subpopulations (P<0.0001; Figure 3B).
The mean impairment of social activity decreased from 55.1 mm to 29.0 mm (Day 7) to 22.4 mm at 14 days. Significant changes were found from baseline for Day 7 and the last day (P<0.0001; Figure 4A). Similar results were seen among all subpopulations (P<0.0001; Figure 4B).
The mean impairment of outdoor activity decreased from 64.4 mm to 32.6 mm (Day 7) to 25.0 mm at 14 days. Significant changes were found from baseline for Day 7 and the last day (P<0.0001; Figure 5A). Similar results were seen among all subpopulations (P<0.0001; Figure 5B).
Moderate correlations were found between the change in general AR symptoms from baseline and sleep quality, activities at work or school, social activities, and outdoor activities (Pearson correlation coefficient=0.59–0.65; all P<0.0001).
Safety
Overall, 20 adverse drug reactions were reported in 14 patients (1.3%) throughout the study, including epistaxis (n=4; 0.4%), impairment of sense of smell and taste (eg, dysgeusia; n=3; 0.3%), headache (n=2; 0.2%), and dyspnea (n=2; 0.2%). Other events were reported in one patient each. The duration of adverse events ranged from 2–14 days, which resulted in recovery/resolution. All events were labeled as possibly related to treatment. For 15 events, there was no impact on the administration of MP-AzeFlu, whereas, for the other five, it was unknown.
Discussion
In this study of 1,103 patients with AR, 86.6% responded to treatment with MP-AzeFlu nasal spray, which was defined as a VAS score <50 mm at least once during the study period. The severity of AR symptoms significantly decreased from the start of treatment (severe) through the last day of the study period (mild). VAS scores related to QoL, including sleep quality, daily activities at work/school, daily social activities, and daily outdoor activities, also significantly improved from baseline. Of importance, these benefits were also seen in all subpopulations based on phenotypes of IgE-mediated disease. These results are consistent with randomized controlled studies of MP-AzeFlu in which patients treated with MP-AzeFlu experienced a statistically significant overall reduction on the RQLQ, as well as on each individual domain.25,26
In the current study, patients with AR reported significantly decreased severity of AR symptoms by an average of 46.2 mm from baseline through the last day of the study period. A VAS score improvement of 10.0 mm was reported following 1 day of treatment in half of the patients, which has been defined as a clinically relevant improvement in symptoms and QoL by Bousquet et al.27 By Day 3, approximately 50% of patients reported an improvement of 23.0 mm or greater, which has been defined as a clinically relevant change in QoL independent of initial AR severity by Demoly et al.28 On the last day, over 75% of patients exhibited a clinically relevant improvement in VAS scores from baseline of greater than 23.0 mm, with a median change of 30.0 mm.
Baseline VAS scores indicated that participating patients with moderate-to-severe AR suffered from relatively poor QoL despite previous AR treatment, including co-medication. With MP-AzeFlu, patients reported substantial improvements in all QoL metrics assessed. MP-AzeFlu not only relieves AR symptoms but also improves patient QoL, as indicated by better sleep quality and less impairment of work, school, social, and outdoor activities after 7 and 14 days of treatment. The results suggest that patient QoL improvements were the result of fewer AR symptoms, which is supported by significant correlations between the reported change in general AR symptoms from baseline and QoL metrics. The benefits of MP-AzeFlu on QoL were consistent, regardless of the phenotype of IgE-mediated disease, suggesting that MP-AzeFlu is effective at improving QoL across IgE subgroups. These findings provide support to previous studies demonstrating improved olfaction and sleep quality following MP-AzeFlu treatment in patients with AR.18,29
Current ARIA recommendations are to use either an intranasal corticosteroid (INCS), intranasal H1-antihistamine (INAH), or the combination of INCS and azelastine in patients with seasonal or perennial AR.1,30 These data provide an important new addition to the evidence base supporting improved QoL with MP-AzeFlu in patients with moderate-to-severe AR taking MP-AzeFlu as a first-line therapy as recommended by ARIA or later in the continuum of care.
Based on real-world evidence, the combination of oral H1-antihistamines plus INCS is not more effective than INCS treatment alone.27 Furthermore, the combination of INCS and INAH has been shown to be more effective than INCS treatment alone. Medications containing H1-antihistamines, such as MP-AzeFlu, have been shown to be effective within minutes. When considering the level of control and co-medication, MP-AzeFlu has been shown to be more effective than INCS treatment.
Limitations to an observational study in a real-life setting are inherent, including the lack of randomization and the potential presence of confounding bias; however, the effect of MP-AzeFlu on QoL was consistent with randomized controlled trials. Pollen counts were not assessed during the study period; however, no relevant changes in exposure are expected during the 2-week treatment duration. In addition, there was no use of a control or placebo. However, the results of this study are not intended to be comparative with other treatments, and the current results demonstrate QoL improvements for patients taking MP-AzeFlu. Advantages of this study include the ability to gather large amounts of data quickly and to explore current clinical practice patterns.
Conclusion
The use of MP-AzeFlu improved severity of AR symptoms and patient QoL by improving the impact on sleep and daily activities. The first-line use of MP-AzeFlu as recommended by ARIA results in clinically significant improvements for patients with AR, regardless of phenotype.
Abbreviations
AR, allergic rhinitis; ARIA, Allergic Rhinitis and Its Impact on Asthma; CI, confidence interval; Ig, immunoglobulin; INAH, intranasal H1-antihistamine; INCS, intranasal corticosteroid; QoL, quality-of-life; RQLQ, Rhinoconjunctivitis Quality-of-Life Questionnaire; VAS, visual analog scale; WPAI-AS, Work Productivity and Activity Impairment Allergy Specific.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval
This investigation represented a non-interventional study as defined by European regulations (ie, the rules imposed for this observational plan did not interfere with the physician’s common therapy). The study was carried out in accordance with the national laws and guidelines current at that time for conducting non-interventional studies and was approved by local ethics committees (Germany, Ethik-Kommission bei der der Landesärztekammer Hessen FF76/2017; Netherlands, Dutch Clinical Research Foundation 17327.dcr; Austria, Ethikkommission der Stadt Wein EK 17-159-VK-NIS; Czech Republic, Eticka Komise FN Hradec Kralove 2018-2-I-16-O; Hungary, OGYEI 37066-9/2017; Ireland, ICGP Research Ethics Committee [reference number not applicable]). The trial was registered on March 12, 2018 (clinical trial registration number: EUPAS23075).
Acknowledgments
We would like to thank the subjects who participated in the trial.
The abstract of this paper was presented at the EAACI Congress 2020 as an oral presentation. The presentation’s abstract was published in Allergy: Van Weissenbruch R, Klimek L, Galffy G, et al. MP-Azeflu improves quality of life of patients with allergic rhinitis: a real-world study [Abstract OAS0249]. Allergy. 2020;75(Suppl 109):7.
Author Contributions
All authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Technical, editorial, and medical writing assistance were provided under the direction of the authors by Erin Burns, PhD, and Strategix, an affiliate of The Lynx Group, LLC. Funding for this support was provided by Mylan Inc.
Disclosure
RVW has nothing to disclose.
LK worked as a paid consultant for Allergopharma, MEDA/Mylan, HAL Allergy, ALK Abello, and LET! Pharma; has received financial grants from Allergopharma, ALK Abello, Allergy Therapeutics, Stallergenes, Quintiles, HAL Allergy, LET! Pharma, Sanofi, AstraZeneca, GSK, ASIT Biotech, and Lofarma; reports grants and personal fees from Allergopharma, MEDA/Mylan, and Sanofi; personal fees from HAL Allergy, LETI Pharma, and Allergy Therapeutics; grants from ASIT biotech, ALK Abelló, Stallergenes, Quintiles, Lofarma, AstraZeneca, GSK, and Inmunotek, outside the submitted work; and membership in the following: AeDA, DGHNO, Deutsche Akademie für Allergologie und klinische Immunologie, HNO-BV, GPA, and EAACI.
GG was a paid consultant and speaker for Astra-Zeneca, Chiesi, Bristol Myers Squibb, MSD, Berlin Chemi, Boehringer Ingelheim, Roche, Novartis, Pfizer, Orion, including Ipsen, and Mylan as speaker.
ME is an employee of MEDA Pharma GmbH & Co. KG (a Mylan Company).
AK is a Mylan, Inc. employee and shareholder, an employee of Mylan/MEDA Pharmaceuticals, and has been employed at Novartis and Lundbeck pharmaceutical companies.
FK is an employee of MEDA Pharma GmbH & Co. KG (a Mylan Company) and reports personal fees from MEDA Pharma GmbH & Co KG (A Mylan Company) during the conduct of the study and outside the submitted work.
DTN is an employee of MEDA Pharma GmbH & Co. KG (a Mylan Company).
HCK is an employee of MEDA Pharma GmbH & Co. KG and worked as a paid consultant for AstraZeneca, Boehringer lngelheim, Chiesi, GSK, and Novartis.
WP has been a paid speaker for and worked as a paid consultant for AstraZeneca, Boehringer lngelheim, Chiesi, GSK, Novartis, and TEVA, and reports personal fees from AstraZeneca, Chiesi, GSK, Menarini, Boehringer Ingelheim, and Sanofi outside the submitted work.
GS has received financial grants from GSK for the mepolizumab study, has worked as a paid consultant and speaker for Meda/Mylan and ALK-Abello, reports personal fees from Mylan and ALK outside the submitted work, and is/was the lead for Allergic Rhinitis education in EUFOREA, lead on BSACI Rhinitis Management guidelines, and scientific chief editor of the Rhinology section of Frontiers in Allergy.
DP has board membership with Amgen, AstraZeneca, Boehringer Ingelheim, Chiesi, Circassia, Mylan, Mundipharma, Napp, Novartis, Regeneron Pharmaceuticals, Sanofi Genzyme, and Teva Pharmaceuticals; consultancy agreements with Amgen, AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Mylan, Mundipharma, Napp, Novartis, Pfizer, Teva Pharmaceuticals, and Theravance; grants and unrestricted funding for investigator-initiated studies (conducted through Observational & Pragmatic Research Institute Pte Ltd) from AKL Research and Development Ltd, AstraZeneca, Boehringer Ingelheim, British Lung Foundation, Chiesi, Circassia, Mylan, Mundipharma, Napp, Novartis, Pfizer, Regeneron Pharmaceuticals, Respiratory Effectiveness Group, Sanofi Genzyme, Teva Pharmaceuticals, Theravance, UK National Health Service, and Zentiva (Sanofi Generics); payment for lectures/speaking engagements from AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, GlaxoSmithKline, Kyorin, Mylan, Merck, Mundipharma, Novartis, Pfizer, Regeneron Pharmaceuticals, Sanofi Genzyme, and Teva Pharmaceuticals; payment for manuscript preparation from Mundipharma and Teva Pharmaceuticals; payment for the development of educational materials from Mundipharma and Novartis; payment for travel/accommodation/meeting expenses from AstraZeneca, Boehringer Ingelheim, Circassia, Mundipharma, Napp, Novartis, and Teva Pharmaceuticals; funding for patient enrollment or completion of research from Chiesi, Novartis, Teva Pharmaceuticals, and Zentiva (Sanofi Generics); stock/stock options from AKL Research and Development Ltd, which produces phytopharmaceuticals; owns 74% of the social enterprise Optimum Patient Care Ltd (Australia and United Kingdom) and 74% of Observational & Pragmatic Research Institute Pte Ltd (Singapore); and is peer reviewer for grant committees of the Efficacy and Mechanism Evaluation Programme and Health Technology Assessment. In addition, DP reports personal fees from Amgen, Cipla, GlaxoSmithKline, Kyorin, Merck, and Zentiva (Sanofi Generics), grants from AKL Research and Development Ltd, British Lung Foundation, Respiratory Effectiveness Group, UK National Health Service; grants and personal fees from AstraZeneca, Boehringer Ingelheim, Chiesi, Circassia, Mylan, Mundipharma, Napp, Novartis, Pfizer, Regeneron Pharmaceuticals, Sanofi Genzyme, Teva, and Theravance; and non-financial support from Efficacy and Mechanism Evaluation Programme and Health Technology Assessment outside the submitted work; and owns 5% shareholding in TimeStamp, which develops adherence monitoring technology.
JM has conducted research/received research grant support from Mylan/MEDA Pharma, URIACH Group, GSK, MSD, FAES, and UCB; received consultancy fees from Mylan/MEDA Pharma, URIACH Group, Allakos, ALK-Abelló, Genentech–Roche, Novartis, Regeneron, Sanofi Genzyme, GSK, MSD, Hartington Pharmaceuticals, and UCB; was a paid instructor for Novartis; was a speaker for Mylan/MEDA Pharma, URIACH Group, Genentech–Roche, Novartis, Regeneron, Sanofi Genzyme, GSK, MSD, Hartington Pharmaceuticals, UCB, and Glenmark; reports grants and personal fees from URIACH Group; was on the speakers bureau/advisory board for Mylan/MEDA Pharma, Sanofi-Genzyme & Regeneron, and Genentech-Novartis; advisory board for AstraZeneca and GSK; and speakers bureau for MENARINI and MSD outside the submitted work.
The authors report no other potential conflicts of interest for this work.
References
1. Bousquet J, Khaltaev N, Cruz AA, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy. 2008;63(Suppl 86):8–160.
2. Canonica GW, Mullol J, Pradalier A, Didier A. Patient perceptions of allergic rhinitis and quality of life: findings from a survey conducted in Europe and the United States. World Allergy Organ J. 2008;1(9):138–144. doi:10.1097/WOX.0b013e3181865faf
3. Canonica GW, Bousquet J, Mullol J, Scadding GK, Virchow JC. A survey of the burden of allergic rhinitis in Europe. Allergy. 2007;62(Suppl 85):17–25.
4. Bousquet PJ, Combescure C, Neukirch F, et al. Visual analog scales can assess the severity of rhinitis graded according to ARIA guidelines. Allergy. 2007;62(4):367–372. doi:10.1111/j.1398-9995.2006.01276.x
5. de la Hoz Caballer B, Rodriguez M, Fraj J, Cerecedo I, Antolín-Amérigo D, Colás C. Allergic rhinitis and its impact on work productivity in primary care practice and a comparison with other common diseases: the cross-sectional study to evaluate work productivity in allergic rhinitis compared with other common diseases (CAPRI) study. Am J Rhinol Allergy. 2012;26(5):390–394. doi:10.2500/ajra.2012.26.3799
6. Perikleous E, Steiropoulos P, Nena E, et al. Association of asthma and allergic rhinitis with sleep-disordered breathing in childhood. Front Pediatr. 2018;6:250. doi:10.3389/fped.2018.00250
7. Maoua M, Maalel OE, Kacem I, et al. Quality of life and work productivity impairment of patients with allergic occupational rhinitis. Tanaffos. 2019;18(1):58–65.
8. Valls-Mateus M, Marino-Sanchez F, Ruiz-Echevarría K, et al. Nasal obstructive disorders impair health-related quality of life in adolescents with persistent allergic rhinitis: a real-life study. Pediatr Allergy Immunol. 2017;28(5):438–445. doi:10.1111/pai.12724
9. Vandenplas O, Vinnikov D, Blanc PD, et al. Impact of rhinitis on work productivity: a systematic review. J Allergy Clin Immunol Pract. 2018;6(4):1274–1286 e9. doi:10.1016/j.jaip.2017.09.002
10. Smith MP, Berdel D, Bauer CP, et al. Asthma and rhinitis are associated with less objectively-measured moderate and vigorous physical activity, but similar sport participation, in adolescent German boys: gINIplus and LISAplus cohorts. PLoS One. 2016;11(8):e0161461. doi:10.1371/journal.pone.0161461
11. Bhattacharyya N. Functional limitations and workdays lost associated with chronic rhinosinusitis and allergic rhinitis. Am J Rhinol Allergy. 2012;26(2):120–122. doi:10.2500/ajra.2012.26.3752
12. Walker S, Khan-Wasti S, Fletcher M, Cullinan P, Harris J, Sheikh A. Seasonal allergic rhinitis is associated with a detrimental effect on examination performance in United Kingdom teenagers: case-control study. J Allergy Clin Immunol. 2007;120(2):381–387. doi:10.1016/j.jaci.2007.03.034
13. Benninger MS, Benninger RM. The impact of allergic rhinitis on sexual activity, sleep, and fatigue. Allergy Asthma Proc. 2009;30(4):358–365. doi:10.2500/aap.2009.30.3244
14. Su VY, Liu CJ, Lan MY, et al. Allergic rhinitis and risk of erectile dysfunction–a nationwide population-based study. Allergy. 2013;68(4):440–445. doi:10.1111/all.12100
15. Vuurman EF, Vuurman LL, Lutgens I, Kremer B. Allergic rhinitis is a risk factor for traffic safety. Allergy. 2014;69(7):906–912. doi:10.1111/all.12418
16. Berger WE. MP29-02 for the treatment of seasonal allergic rhinitis: a review of clinical pharmacology, efficacy and safety. Expert Rev Clin Immunol. 2013;9(9):803–811. doi:10.1586/1744666X.2013.828876
17. Electronic Medicines Compendium. Dymista 137 micrograms/50 micrograms per actuation nasal spray, summary of product characteristics [updated December 10, 2019]. Available from: www.medicines.org.uk/emc/product/9450/smpc.
18. Kaulsay R, Nguyen DT, Kuhl HC. Real-life effectiveness of MP-AzeFlu in Irish patients with persistent allergic rhinitis, assessed by visual analogue scale and endoscopy. Immun Inflamm Dis. 2018;6(4):456–464. doi:10.1002/iid3.237
19. Klimek L, Bachert C, Stjärne P, et al. MP-AzeFlu provides rapid and effective allergic rhinitis control in real life: a pan-European study. Allergy Asthma Proc. 2016;37(5):376–386. doi:10.2500/aap.2016.37.3979
20. Price D, Klimek L, Gálffy G, et al. Allergic rhinitis and asthma symptoms in a real-life study of MP-AzeFlu to treat multimorbid allergic rhinitis and asthma. Clin Mol Allergy. 2020;18:15. doi:10.1186/s12948-020-00130-9
21. Meltzer E, Ratner P, Bachert C, et al. Clinically relevant effect of a new intranasal therapy (MP29-02) in allergic rhinitis assessed by responder analysis. Int Arch Allergy Immunol. 2013;161(4):369–377. doi:10.1159/000351404
22. Klimek L, Bergmann KC, Biedermann T, et al. Visual analogue scales (VAS): measuring instruments for the documentation of symptoms and therapy monitoring in cases of allergic rhinitis in everyday health care: position Paper of the German Society of Allergology (AeDA) and the German Society of Allergy and Clinical Immunology (DGAKI), ENT Section, in collaboration with the working group on Clinical Immunology, Allergology and Environmental Medicine of the German Society of Otorhinolaryngology, Head and Neck Surgery (DGHNOKHC). Allergo J Int. 2017;26(1):16–24.
23. Bousquet J, Schünemann HJ, Hellings PW, et al.; MASK study group. MACVIA clinical decision algorithm in adolescents and adults with allergic rhinitis. J Allergy Clin Immunol. 2016;138(2):367–374.e2. doi:10.1016/j.jaci.2016.03.025.
24. Del Cuvillo A, Santos V, Montoro J, et al. Allergic rhinitis severity can be assessed using a visual analogue scale in mild, moderate and severe. Rhinology. 2017;55(1):34–38. doi:10.4193/Rhin16.025
25. Hampel FC, Ratner PH, Van Bavel J, et al. Double-blind, placebo-controlled study of azelastine and fluticasone in a single nasal spray delivery device. Ann Allergy Asthma Immunol. 2010;105(2):168–173. doi:10.1016/j.anai.2010.06.008
26. Carr W, Bernstein J, Lieberman P, et al. A novel intranasal therapy of azelastine with fluticasone for the treatment of allergic rhinitis. J Allergy Clin Immunol. 2012;129(5):1282–1289.e10. doi:10.1016/j.jaci.2012.01.077
27. Bousquet PJ, Combescure C, Klossek JM, Daurès JP, Bousquet J. Change in visual analog scale score in a pragmatic randomized cluster trial of allergic rhinitis. J Allergy Clin Immunol. 2009;123(6):1349–1354. doi:10.1016/j.jaci.2009.02.033
28. Demoly P, Bousquet PJ, Mesbah K, Bousquet J, Devillier P. Visual analogue scale in patients treated for allergic rhinitis: an observational prospective study in primary care: asthma and rhinitis. Clin Exp Allergy. 2013;43(8):881–888. doi:10.1111/cea.12121
29. Klimek L, Poletti SC, Sperl A, et al. Olfaction in patients with allergic rhinitis: an indicator of successful MP-AzeFlu therapy. Int Forum Allergy Rhinol. 2017;7(3):287–292. doi:10.1002/alr.21877
30. Bousquet J, Schünemann HJ, Togias A, et al. Next-generation Allergic Rhinitis and Its Impact on Asthma (ARIA) guidelines for allergic rhinitis based on Grading of Recommendations Assessment, Development and Evaluation (GRADE) and real-world evidence. J Allergy Clin Immunol. 2020;145(1):70–80.e3. doi:10.1016/j.jaci.2019.06.049
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.