Back to Journals » International Journal of General Medicine » Volume 15
Monocyte-to-Lymphocyte Ratio in the Diagnosis of Lymphoma in Adult Patients
Authors Kamiya N, Ishikawa Y , Kotani K , Hatakeyama S, Matsumura M
Received 7 January 2022
Accepted for publication 6 April 2022
Published 20 April 2022 Volume 2022:15 Pages 4221—4226
DOI https://doi.org/10.2147/IJGM.S357468
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Naoko Kamiya,1 Yukiko Ishikawa,1 Kazuhiko Kotani,2 Shuji Hatakeyama,1,3 Masami Matsumura1
1Division of General Internal Medicine, Jichi Medical University Hospital, Shimotsuke-shi, Tochigi, Japan; 2Division of Community and Family Medicine, Center for Community Medicine, Jichi Medical University, Shimotsuke-shi, Tochigi, Japan; 3Division of Infectious Diseases, Jichi Medical University Hospital, Shimotsuke-shi, Tochigi, Japan
Correspondence: Naoko Kamiya, Division of General Internal Medicine, Jichi Medical University Hospital, 3311-1 Yakushiji, Shimotsuke-shi, Tochigi, 329-0498, Japan, Tel +81-285-58-7498, Fax +81-285-40-5160, Email [email protected]
Background: Lymphomas, including Hodgkin lymphoma and non-Hodgkin lymphoma, are one of the differentials for peripheral lymphadenopathy and are difficult to diagnose clinically. Biopsy is essential for diagnosing lymphoma, although it is invasive. Non-invasive methods are required to identify patients with suspected lymphoma who should undergo a biopsy. The relevance of the monocyte-to-lymphocyte ratio has recently been reported to be a useful diagnostic marker in children with lymphoma and a prognostic marker of various other diseases. This study aimed to determine the relevance of the monocyte-to-lymphocyte ratio in the diagnosis of lymphoma in adults.
Methods: The study included 246 adult outpatients (median age of 49.0 years) presenting with peripheral lymphadenopathy. The final diagnosis was determined by reviewing the medical records. We categorized all patients into either the lymphoma group or the non-lymphoma group. The lymphoma group included patients who underwent biopsy and were diagnosed with lymphoma by histopathology, while the non-lymphoma group included those diagnosed with disease excluding lymphoma. The monocyte-to-lymphocyte ratios were compared between the two groups.
Results: Of the participants, 33 (13.4%) were assigned to the lymphoma group. The median age of the lymphoma and non-lymphoma groups were 67.0 years (interquartile range [IQR] 55.5– 75.5 years) and 46.0 years (IQR 36.0– 61.0 years), respectively. The lymphocyte and monocyte levels showed no significant differences between the two groups individually. Nonetheless, the monocyte-to-lymphocyte ratio was significantly higher in the lymphoma group (median, 0.36; IQR, 0.24– 0.73) than in the non-lymphoma group (median, 0.29; IQR, 0.21– 0.43; P = 0.022), independent of lymph node diameter ≥ 1 cm and C-reactive protein levels.
Conclusion: This study suggests that the monocyte-to-lymphocyte ratio can be a helpful diagnostic marker for lymphoma in adults with peripheral lymphadenopathy when the etiology is unclear even after a medical interview and physical examination.
Keywords: lymphadenopathy, lymphoma, monocyte-to-lymphocyte ratio, diagnostic marker
Introduction
Peripheral lymphadenopathy is a common sign encountered in daily clinical practice and is caused by various diseases, including neoplasms.1 The etiology of peripheral lymphadenopathy is generally determined after a medical interview and physical examination.1 However, additional evaluation is required when the etiology is unclear even after a medical interview and physical examination, particularly when neoplasms are included in the differential diagnosis.
Lymphomas are one of the causes of lymphadenopathy and are more prevalent in adults compared to children.2,3 Although fever, night sweats, and weight loss are known to be characteristic symptoms of lymphoma, they are nonspecific symptoms and signs.4,5 Furthermore, patients with lymphoma typically present with painless and slowly enlarging lymph nodes. Furthermore, a lymphoma might occur in any organ other than the lymph nodes.4,5 Hence, reaching the clinical diagnosis of lymphoma is difficult.
Biopsy is essential for the diagnosis of lymphoma. However, performing this invasive examination is inapplicable to all patients with lymphadenopathy. Whether a biopsy should be performed must be carefully considered in patients who do not present with the typical lymphoma features or in those whose enlarged lymph nodes are located in a difficult to reach area. In contrast, delayed diagnosis of lymphoma caused by withholding biopsy must be avoided. The clinicians are often faced with the decision of whether to perform a biopsy or follow up evaluation, when examining patients with peripheral lymphadenopathy. Therefore, non-invasive methods to identify patients with a high risk of lymphoma should be identified for use in daily practice. Although serum C-reactive protein (CRP) and soluble interleukin-2 receptor (sIL-2R) have been reported as useful prognostic markers for lymphoma,6,7 reports on their use as diagnostic markers are scarce. The monocyte-to-lymphocyte ratio, which reflects the presence of inflammation, has recently been used as a new marker for various diseases. Since tumors also evoke inflammatory responses, the monocyte-to-lymphocyte ratio has been reported as a prognostic marker in myeloma, lymphoma, and several solid tumors.8–14 Conversely, to the best of our knowledge, the monocyte-to-lymphocyte ratio has been reported as a diagnostic marker only in children with lymphoma.15 Lymphoma is epidemiologically common in adults, and new diagnostic methods for lymphoma are desired for use in daily practice.2,3 The objective of this study was to determine whether the monocyte-to-lymphocyte ratio can be a diagnostic marker for lymphoma in adult patients with peripheral lymphadenopathy.
Patients and Methods
Study Design, Setting, and Participants
We conducted a cross-sectional study of patients with a chief complaint of swelling in the neck, axilla, or inguinal regions. The data were retrospectively collected from new outpatients aged ≥30 years who visited or were referred to the Division of General Internal Medicine, Jichi Medical University Hospital, Japan, between June 2010 and December 2019. We enrolled only patients ≥30 years. We chose the 30 years cut-off point since most patients with lymphoma in our General Internal Medicine Division were ≥30 years.
Measurements
All patients suspected of metastatic lymphadenopathy or lymphoma had fine-needle aspiration cytology or biopsy. Histopathologic examination included immunostaining when necessary. From the medical records, we extracted age, sex, lymph node diameter on physical examination, and laboratory data, including white blood cell (WBC) count, lymphocyte count, neutrophil count, monocyte count, and CRP levels. The monocyte-to-lymphocyte ratio was then calculated. The final diagnosis was determined by reviewing medical records more than 12 months after the initial visit. In patients with fine-needle aspiration cytology or biopsy, the final diagnosis was determined by the histopathological findings. All patients were classified into either the lymphoma or non-lymphoma group. We defined the lymphoma group as patients who underwent biopsy and were diagnosed with lymphoma by histopathology, while we defined the non-lymphoma group as those diagnosed with disease excluding lymphoma.
Statistical Analysis
Statistical analyses were performed using SPSS (version 21.0; IBM Corporation, Tokyo, Japan). The chi-squared test was used for nominal variables, and the Student’s t-test was used for continuous variables to compare characteristics, physical findings, and laboratory parameters between the lymphoma and non-lymphoma groups. Variables such as age, CRP, and monocyte-to-lymphocyte ratio were analyzed after log-transformation due to their skewed distribution. A general linear model was employed with three models to evaluate the independent contribution of the monocyte-to-lymphocyte ratio when adjusted for other variables: Model 1, adjusted for age and sex; Model 2, adjusted for age, sex, and CRP level; Model 3, adjusted for age, sex, CRP level, and lymph node diameter ≥ 1 cm.16 A value of P < 0.05 was considered significant.
Ethics
The Institutional Review Board of Jichi Medical University approved this study (approval number A20-005). This study was conducted in accordance with the Declaration of Helsinki. All data were collected anonymously without including information that identifies the patient, and patient data confidentiality is guaranteed. The requirement for informed consent was waived owing to the retrospective study design, non-identification, and confidentiality. This study was carried out using the opt-out method.
Results
Among the 441 participants enrolled, we excluded patients with missing laboratory data (139 patients), those with enlarged organs other than lymph nodes (51 patients), and no detectable lymph node enlargement (5 patients). The final number of eligible participants for the study was 246 (152 women and 94 men), and their median age was 49.0 years (interquartile range [IQR] 37.0–63.0 years).
Of the 246 participants, 33 (13.4%) were assigned to the lymphoma group. All of patients in the lymphoma group underwent biopsy and immunohistochemical staining in histopathological examination. The lymphoma group included B-cell lymphoma (n = 28), T-cell lymphoma (n = 4), and Hodgkin lymphoma (n = 1). The non-lymphoma group included normal or reactive lymph nodes (n = 166), metastatic lymphadenopathy (n = 26), necrotizing lymphadenitis (n = 14), tuberculous lymphadenitis (n = 5), plasmacytoma (n = 1), and Castleman’s disease (n = 1).
Table 1 shows the characteristics, physical findings, and laboratory parameters in the lymphoma and non-lymphoma groups. There was no sex difference between the lymphoma and non-lymphoma groups. The patients in the lymphoma group were significantly older than those in the non-lymphoma group (67.0 years vs 46.0 years, P < 0.001). The percentage of patients with lymph node diameter ≥ 1 cm was significantly higher in the lymphoma group than in the non-lymphoma group (81.8% vs 52.1%, P = 0.001). In the laboratory parameters, WBC, neutrophil, lymphocyte, monocyte, and CRP levels showed no significant differences between the two groups. Nonetheless, the median value of the monocyte-to-lymphocyte ratio was significantly higher in the lymphoma group than in the non-lymphoma group (0.36 [IQR 0.24–0.73] vs 0.29 [IQR 0.21–0.43], P = 0.022). The values of the monocyte-to-lymphocyte ratio were not significantly different between patients with B-cell lymphoma (median, 0.35; IQR, 0.24–0.74) and T-cell lymphoma (median, 0.43; IQR, 0.13–0.73; P = 0.608). The value of the monocyte-to-lymphocyte ratio for Hodgkin lymphoma was 0.42.
 |
Table 1 Comparison of Clinical Characteristics in the Lymphoma and Non-Lymphoma Groups |
Table 2 presents the results of the general linear modeling. Lymphoma was significantly associated with the monocyte-to-lymphocyte ratio in all adjusted models (model 1, P = 0.012; model 2, P = 0.014; and model 3, P = 0.035). This indicated that the difference in the monocyte-to-lymphocyte ratio between the lymphoma and non-lymphoma groups remained significant after considering the other confounders.
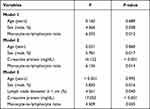 |
Table 2 General Linear Models for Lymphoma |
Discussion
In this study, the monocyte-to-lymphocyte ratio was significantly higher in the lymphoma group, which was independent of lymph node diameter ≥ 1 cm and CRP levels, indicating its potential as a diagnostic marker for lymphoma in adults with peripheral lymphadenopathy. Although a monocyte-to-lymphocyte ratio higher than 0.29 in children with lymphadenopathy can reportedly differentiate between lymphoma and reactive lymphadenopathy,15 our findings in this study suggest the monocyte-to-lymphocyte ratio can be used as a diagnostic marker of lymphoma in adults. Since the incidence of lymphoma is higher in adults than in children, the results of this study are valuable.
Biopsy is essential for the diagnosis of lymphoma. However, it is an invasive examination. The WBC count is a simple laboratory test that can be easily performed at the initial point-of-care testing center. The monocyte-to-lymphocyte ratio can be easily calculated using WBC count. If the palpation of lymph nodes and CRP levels are not enough to determine whether a biopsy is required, a high monocyte-to-lymphocyte ratio may help identify patients who require a biopsy in cases where lymphoma is suspected. Thus, the monocyte-to-lymphocyte ratio may be useful in confirming the diagnosis of lymphoma in the early phase of the diagnostic process.
This study showed the relevance of the monocyte-to-lymphocyte ratio in lymphoma diagnosis in patients with peripheral lymphadenopathy. Similarly, the monocyte-to-lymphocyte ratio has been reported to be useful in bacterial infection diagnosis when used in patients with liver cirrhosis or fever and influenza diagnosis when used in patients with influenza-like symptoms.17–19 The monocyte-to-lymphocyte ratio has also been a marker related to tumor growth because it has been reported as a prognostic marker in myeloma, lymphoma, and several solid tumors.8–10,13,14 Considering the relation with tumor growth, it is consistent for the monocyte-to-lymphocyte ratio to be useful in lymphoma diagnosis.
The tumor microenvironment consists of non-tumor cells, including tumor-associated macrophages (TAMs) and lymphocytes. The monocyte-to-lymphocyte ratio represents a combination balanced by an increase in monocytes and a decrease in lymphocytes, which can be caused by an inflammatory response against tumor growth.20–22 TAMs are peripheral monocytes recruited to the tumor area, which promote tumor progression.23 Peripheral monocyte counts have been high in patients with solid tumors or hematological malignancies.24–26 Peripheral monocyte count reportedly represents the abundance of TAMs in the tumor microenvironment and can be considered a potential biomarker for TAMs.27,28 Peripheral lymphocytes are reportedly lower in malignant tumors than in benign tumors,29 probably because lymphocytes infiltrate the tumor area to suppress tumor cells,20 resulting in a decrease in the peripheral lymphocyte count. These mechanisms may support the results of this study.
In this study, the elevation of the monocyte-to-lymphocyte ratio was related to lymphoma and independent of CRP levels. The tumor microenvironment secretes cytokines that are involved in the synthesis of CRP, such as interleukin (IL)-1 beta, IL-6, and tumor necrosis factor alpha.22,30 The monocyte-to-lymphocyte ratio directly estimates infiltrating cells reacting to tumor progression, while CRP reflects indirect reactions through a complex network of cytokines in the tumor area. These differences might have resulted in the monocyte-to-lymphocyte ratio being independent of CRP levels.
Our study has some limitations. First, we used a cross-sectional design; thus, the causal relationship between the monocyte-to-lymphocyte ratio and lymphoma cannot be established. Second, lymph node biopsy, which is the gold standard for diagnosis, was not performed in all the cases included in this study. Third, patients with severe lymphoma or typical lymphoma might have been excluded from this study as we only included the outpatients of the General Internal Medicine department. Finally, this study was conducted in a single university hospital. Participants in this study were patients who visited without a referral or were referred from other medical institutions. The generalizability of the result might need to be considered due to selection bias.
Conclusion
This study reveals that the monocyte-to-lymphocyte ratio is independently and significantly associated with adult patients with lymphoma diagnosed with Hodgkin and non-Hodgkin lymphomas. The monocyte-to-lymphocyte ratio can be a useful diagnostic marker in adult patients with peripheral lymphadenopathy when the etiology is unclear even after a medical interview and physical examination. Prospective studies with more patients are warranted.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analyses, interpretation of the results, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported in part by the Foundation for Development of the Community (research grant). The funder had no role in the study design, data collection, data analysis, data interpretation, writing of the manuscript, or decision to submit the manuscript for publication.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Habermann TM, Steensma DP. Lymphadenopathy. Mayo Clin proc. 2000;75(7):723–732.
2. Urquhart A, Berg R. Hodgkin’s and non-Hodgkin’s lymphoma of the head and neck. Laryngoscope. 2001;111(9):1565–1569.
3. Roman E, Smith AG. Epidemiology of lymphomas. Histopathology. 2011;58(1):4–14.
4. Townsend W, Linch D. Hodgkin’s lymphoma in adults. Lancet. 2012;380(9844):836–847.
5. Armitage JO, Gascoyne RD, Lunning MA, Cavalli F. Non-Hodgkin lymphoma. Lancet. 2017;390(10091):298–310.
6. Cao Y, Shi YX, Chen JO, et al. Serum C-reactive protein as an important prognostic variable in patients with diffuse large B cell lymphoma. Tumour Biol. 2012;33(4):1039–1044.
7. Morito T, Fujihara M, Asaoku H, et al. Serum soluble interleukin-2 receptor level and immunophenotype are prognostic factors for patients with diffuse large B-cell lymphoma. Cancer Sci. 2009;100(7):1255–1260.
8. Nishijima TF, Muss HB, Shachar SS, Tamura K, Takamatsu Y. Prognostic value of lymphocyte-to-monocyte ratio in patients with solid tumors: a systematic review and meta-analysis. Cancer Treat Rev. 2015;41(10):971–978.
9. Xiang J, Zhou L, Li X, et al. Preoperative Monocyte-to-Lymphocyte Ratio in Peripheral Blood Predicts Stages, Metastasis, and Histological Grades in Patients with Ovarian Cancer. Transl Oncol. 2017;10(1):33–39.
10. Tian Y, Zhang Y, Zhu WQ, Chen XL, Zhou HB, Chen WM. Peripheral Blood Lymphocyte-to-Monocyte Ratio as a Useful Prognostic Factor in Newly Diagnosed Multiple Myeloma. BioMed Res Int. 2018;2018:9434637.
11. Markovic O, Popovic L, Marisavljevic D, et al. Comparison of prognostic impact of absolute lymphocyte count, absolute monocyte count, absolute lymphocyte count/absolute monocyte count prognostic score and ratio in patients with diffuse large B cell lymphoma. Eur J Intern Med. 2014;25(3):296–302.
12. Lee SF, Ng TY, Spika D. Prognostic value of lymphocyte-monocyte ratio at diagnosis in Hodgkin lymphoma: a meta-analysis. BMC Cancer. 2019;19(1):338.
13. Gao F, Hu J, Zhang J, Xu Y. Prognostic Value of Peripheral Blood Lymphocyte/monocyte Ratio in Lymphoma. J Cancer. 2021;12(12):3407–3417.
14. Wang J, Gao K, Lei W, et al. Lymphocyte-to-monocyte ratio is associated with prognosis of diffuse large B-cell lymphoma: correlation with CD163 positive M2 type tumor-associated macrophages, not PD-1 positive tumor-infiltrating lymphocytes. Oncotarget. 2017;8(3):5414–5425.
15. Tezol O, Bozlu G, Sagcan F, Tuncel Daloglu F, Citak C. Value of neutrophil-to-lymphocyte ratio, monocyte-to-lymphocyte ratio, platelet-to-lymphocyte ratio and red blood cell distribution width in distinguishing between reactive lymphadenopathy and lymphoma in children. Bratisl Lek Listy. 2020;121(4):287–292.
16. Oguz A, Karadeniz C, Temel EA, Citak EC, Okur FV. Evaluation of peripheral lymphadenopathy in children. Pediatr Hematol Oncol. 2006;23(7):549–561.
17. Naess A, Nilssen SS, Mo R, Eide GE, Sjursen H. Role of neutrophil to lymphocyte and monocyte to lymphocyte ratios in the diagnosis of bacterial infection in patients with fever. Infection. 2017;45(3):299–307.
18. Piotrowski D, Sączewska-Piotrowska A, Jaroszewicz J, Boroń-Kaczmarska A. Lymphocyte-To-Monocyte Ratio as the Best Simple Predictor of Bacterial Infection in Patients with Liver Cirrhosis. Int J Environ Res Public Health. 2020;17(5):85.
19. Zhu R, Chen C, Wang Q, Zhang X, Lu C, Sun Y. Routine blood parameters are helpful for early identification of influenza infection in children. BMC Infect Dis. 2020;20(1):864.
20. Balkwill FR, Capasso M, Hagemann T. The tumor microenvironment at a glance. J Cell Sci. 2012;125(Pt 23):5591–5596.
21. Komohara Y, Niino D, Ohnishi K, Ohshima K, Takeya M. Role of tumor-associated macrophages in hematological malignancies. Pathol Int. 2015;65(4):170–176.
22. Solinas G, Germano G, Mantovani A, Allavena P. Tumor-associated macrophages (TAM) as major players of the cancer-related inflammation. J Leukoc Biol. 2009;86(5):1065–1073.
23. Liu Y, Cao X. The origin and function of tumor-associated macrophages. Cell Mol Immunol. 2015;12(1):1–4.
24. Lee YY, Choi CH, Sung CO, et al. Prognostic value of pre-treatment circulating monocyte count in patients with cervical cancer: comparison with SCC-Ag level. Gynecol Oncol. 2012;124(1):92–97.
25. Wang YQ, Zhu YJ, Pan JH, et al. Peripheral monocyte count: an independent diagnostic and prognostic biomarker for prostate cancer - a large Chinese cohort study. Asian J Androl. 2017;19(5):579–585.
26. Wilcox RA, Ristow K, Habermann TM, et al. The absolute monocyte count is associated with overall survival in patients newly diagnosed with follicular lymphoma. Leuk Lymphoma. 2012;53(4):575–580.
27. Shibutani M, Maeda K, Nagahara H, et al. The peripheral monocyte count is associated with the density of tumor-associated macrophages in the tumor microenvironment of colorectal cancer: a retrospective study. BMC Cancer. 2017;17(1):404.
28. Koh YW, Kang HJ, Park C, et al. The ratio of the absolute lymphocyte count to the absolute monocyte count is associated with prognosis in Hodgkin’s lymphoma: correlation with tumor-associated macrophages. Oncologist. 2012;17(6):871–880.
29. Damar M, Dinç AE, Erdem D, et al. Pretreatment Neutrophil-Lymphocyte Ratio in Salivary Gland Tumors Is Associated with Malignancy. Otolaryngol Head Neck Surg. 2016;155(6):988–996.
30. Lin WW, Karin M. A cytokine-mediated link between innate immunity, inflammation, and cancer. J Cnin Invest. 2007;117(5):1175–1183.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
