Back to Journals » Cancer Management and Research » Volume 10
Moderating effects of sleep duration on diabetes risk among cancer survivors: analysis of the National Health Interview Survey in the USA
Authors Seixas AA, Gyamfi L, Newsome V, Ranger-Murdock G, Butler M, Rosenthal DM , Zizi F , Youssef I, McFarlane SI , Jean-Louis G
Received 16 June 2018
Accepted for publication 2 August 2018
Published 12 October 2018 Volume 2018:10 Pages 4575—4580
DOI https://doi.org/10.2147/CMAR.S177428
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Antonella D'Anneo
Azizi A Seixas,1,2 Lloyd Gyamfi,1 Valerie Newsome,1 Gabrielle Ranger-Murdock,1 Mark Butler,1 Diana Margot Rosenthal,1 Ferdinand Zizi,1 Irini Youssef,3 Samy I McFarlane,3 Girardin Jean-Louis1,2
1Center for Healthful Behavior Change, Department of Population Health, NYU Langone Health, 2Department of Psychiatry, NYU Langone Health, New York, NY, USA; 3Division of Endocrinology, Department of Medicine, State University of New York (SUNY), Downstate Medical Center, Brooklyn, NY, USA
Background: Growing evidence suggests that cancer and diabetes may share common risk factors such as age, race/ethnicity, obesity, insulin resistance, sedentary lifestyle, smoking, and alcohol consumption. However, little is known about how habitual sleep duration (a known cardiometabolic risk factor) may affect the relationship between cancer and diabetes. The aim of this study was to investigate whether sleep duration moderated the relationship between history of cancer and diabetes.
Methods: Data were extracted from the National Health Interview Survey dataset from 2004 to 2013 containing demographics, chronic diseases, and sleep duration (N=236,406). Data were analyzed to assess the moderating effect of short and long sleep durations on cancer and diabetes mellitus.
Results: Our findings indicate that short sleep (odds ratio [OR] =1.07, 95% CI =1.03–1.11, P<0.001) and long sleep (OR =1.32, 95% CI =1.26–1.39, P<0.001) were associated with diabetes mellitus in fully adjusted models. However, only long sleep duration significantly moderated the relationship between cancer and diabetes (OR =0.88, 95% CI =0.78–0.98, P<0.05).
Conclusion: Our findings indicate that for cancer survivors, short sleep was associated with higher self-reported diabetes and long sleep duration may act as a buffer against diabetes mellitus, as the likelihood of self-reported diabetes was lower among cancer survivors who reported long sleep duration.
Impact: Findings from the current study have clinical and public health implications. Clinically, comprehensive sleep assessments and sleep interventions to improve sleep are needed for cancer survivors who have comorbid diabetes. Our findings can also spur public health reform to make sleep an important component of standard cancer survivorship care, as it reduces other chronic disease like diabetes.
Keywords: sleep duration, diabetes, cancer
Introduction
Individuals with diabetes mellitus (DM), otherwise known as type II diabetes, are at increased risk for cancer, and cancer patients are at increased risk for DM.1–3 To address this public health issue, both the American Diabetes Association and the American Cancer Society proposed to investigate the following: 1) whether there is a meaningful relationship between cancer and diabetes; 2) the risk factors common between cancer and diabetes; 3) the biological mechanisms between cancer and diabetes; and 4) whether diabetes treatment increases cancer risk or vice versa. Although all four questions remain relatively unsatisfactorily answered, to date progress has been limited to observations of biological mechanisms between cancer and diabetes.3 While the exact mechanisms linking diabetes and cancer remain largely unclear, two categories of possible underlying hypothesis include behavioral/lifestyle (eg, alcohol, diet, obesity, smoking, and physical activity) and biological (eg, insulin resistance, inflammatory cytokines, and oxidative stress) roots.4 Of the possible biological mechanisms, a decrease in cell mitochondrial metabolic activity as well as mitochondrial dysfunction represent the most robust mechanisms linking DM to cancer.5 However, since our understanding of these mechanisms is incomplete at best, the translation of these targets into actual interventions has been slow. These limitations highlight the need for better understanding of the potentially modifiable behavioral factors that are associated with DM and cancer and how behavior influences pathophysiological mechanisms (mainly hypoxia and cell mitochondrial dysfunction and damage) that undergird DM and cancer.
Little is known about behavioral/lifestyle factors that influence the pathophysiology of cancer and DM and which behavioral factors affect the hypoxia and mitochondrial cell damage that are commonly observed among individuals with cancer and/or DM. Adequate hydration is one potentially effective behavioral strategy that may address or prevent mitochondrial cell inactivity and dysfunction. Adequate hydration optimizes and regulates homeostatic cell function and potentially mitigates the harmful effects of oxidative stress by binding to free radicals that would produce mitochondrial disease, a precursor to DM (ie, deterioration of β cell functioning) and cancer.5–9 Mitochondrial dysfunction caused by cell dehydration may be due to oxygen desaturation, hypoxia, and poor oxidative metabolism.6 Laboratory investigations indicate that chronic sleep deprivation in mice may also be responsible for mitochondrial dysfunction, specifically impairment of the mitochondrial electron transport chain in the brain.7 In human studies, patients with obstructive sleep apnea, a sleep disorder marked by chronic sleep deprivation, are susceptible to mitochondrial DNA damage and dysfunction induced by the increase of oxidative stress caused by hypoxia (intermittent loss of oxygen during sleep).8,9
Despite initial evidence linking cancer to diabetes, as well as sleep deprivation to cancer and to DM, the relationship among cancer, diabetes, and sleep duration in humans remains largely underexplored (Figure 1). The purpose of the current study is to investigate whether short or long sleep duration moderates the relationship between cancer and DM. We hypothesize that short sleep duration would strengthen the relationship between cancer and DM diagnosis, while long sleep duration would weaken/attenuate the relationship between cancer and DM diagnosis.
  | Figure 1 Conceptual framework for the moderating effects of sleep duration on the relationship between cancer and DM. Abbreviation: DM, diabetes mellitus. |
Materials and methods
The study was approved by the Centers for Disease Control and Prevention (CDC) ethical review board, and all participants signed informed consents before participating. Data for this study emanated from a total of 236,406 Americans (age range: 18–85 years) who participated in the 2004–2013 National Health Interview Survey (NHIS). The NHIS is conducted annually by the National Center for Health Statistics, CDC. The NHIS comprises a complex multistage area probability design providing a representative sample of US households from all 50 states and the District of Columbia. Data are stored in a public repository that is freely accessible online and can be downloaded and coded by an experienced biostatistician using available coding and analytic instructions provided by the CDC.
Procedures and measures
Data for the 2004–2013 NHIS was obtained through face-to-face interviews and questionnaires, including self-reported sociodemographic data (e.g., age, sex, race/ethnicity, average family income, and education) and physician-diagnosed chronic conditions or diseases such as hypertension, diabetes, coronary heart disease, cancer, kidney disease, stroke, and myocardial infarction. In the present analysis, we included several variables including sleep duration, race/ethnicity, and history of physician-diagnosed cancer and DM.
Sleep duration
Sleep duration was assessed by asking participants the following question: “On average, how many hours of sleep do you get in a 24-hour period?” Participants estimated habitual sleep duration using full hour units, i.e., 5, 6, and 7 hours. Sleep duration was categorized into two groups: short sleep duration (≤6 hours)10 and long sleep duration (≥9 hours);11,12 individuals reporting 7–8 hours of sleep were used as the reference group (“healthy sleep duration”).
Covariates
Several important covariates were adjusted in our analyses. They included information about participants’ annual family income and body mass index (BMI; measured in kg/m2). Additionally, analyses also considered history of chronic diseases or health conditions, such as hypertension and depression as covariates.
Statistical analyses
Analyses included adults aged ≥18 years with complete data. Frequency and measures of central tendency were used to describe the sample. In preliminary analyses, Pearson and Spearman correlations were used to explore relationships between variables of interest – sleep duration, self-reported cancer history, and potential covariates (age, race/ethnicity, sex, BMI, smoking history, and habitual alcohol beverage consumption). Only factors that were significantly associated with sleep duration (a P-value <0.05) – age, race/ethnicity, and sex – were considered in the final regression models. We utilized multivariable logistic regression modeling to test the relationship between sleep duration (short or long sleep duration) and DM adjusting for covarying effects of age, race/ethnicity, and sex, among individuals with and without a cancer history. Specifically, we created two models (one for short sleepers and the other for long sleepers) investigating the relationship between short sleep duration in model 1 and long sleep duration in model 2 and DM. The IBM Corporation released 2013 SPSS Statistics for Windows, Version 23.0, (IBM Corporation, Armonk, NY, USA), was used for all statistical analyses.
Results
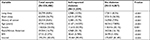
Descriptive statistical analyses indicate that of the participants who reported DM: 53.9% were female, 23.1% identified as Black/African American, had a mean age of 61.67 years, 13.9% reported long sleep duration, 27.9% reported short sleep duration, 15.7% had a history of cancer, 90.4% had medical insurance coverage, and had an average BMI of 30.63 kg/m2 (which is considered within the obesity range) (Table 1). All abovementioned prevalence factors were statistically significant compared to individuals who reported no history of DM. This indicates that individuals with DM are more likely to have long sleep, short sleep, and a history of cancer than individuals without DM. Individuals with DM in the sample were also older, less likely to be female, more likely to be black, had higher BMI, and were more likely to be insured compared to individuals without DM.
In our regression analyses, a history of cancer, short and long sleep durations were associated with DM. Specifically in our fully adjusted models (controlling for age, sex, and race/ethnicity), participants with a cancer history were 9% more likely to report DM, compared to participants who did not have a history of cancer. Additionally, short sleep (odds ratio [OR] =1.07, 95% CI =1.03–1.11, P<0.001) and long sleep (OR =1.32, 95% CI =1.26–1.39, P<0.001) were associated with DM in fully adjusted models. We also found that the interaction between cancer and short sleep duration was not significantly associated with DM (OR =1.08, 95% CI =0.98–1.19, P=0.101) (Table 2). However, there was a significant interaction between long sleep and cancer history on the presence of DM (Table 3). Looking at the conditional effects of cancer on DM, individuals without long sleep were 13% more likely to report diabetes (OR = 1.13, 95% CI = 1.07–1.18; P≤ 0.001). In individuals with a cancer history and long sleep, the conditional effect of cancer on DM is not significant (OR =0.99, 95% CI =0.89–1.10; P=0.811). Therefore, individuals with a cancer history who did not report long sleep had 12% greater odds of having DM compared to individual with a cancer history who had long sleep.
Discussion
Our findings that short sleep duration, long sleep duration, and cancer history are independently associated with DM are consistent with previous evidence.13–16 These findings make two significant contributions to the literature. First, though short and long sleep durations are associated with DM, our finding that long sleep has a greater association with DM compared to short sleep is novel. Previous studies have indicated a U-shape relationship between sleep duration (short and long sleep) and DM. Second, our finding that long sleep was a stronger moderator in the cancer-DM relationship, as opposed to short sleep duration and cancer, is inconsistent with our a priori hypothesis, since short sleep is generally associated with adverse health outcomes. Plausibly, these anomalous findings might be explained by clinical, biological/etiological, and methodological factors.
Although the strong association between long sleep duration and DM is novel, previous studies have found a similar relationship between sleep duration and stroke.17 It is important however to note that DM is an important underlying risk factor for stroke, and many patients with stroke have either insulin resistance, dysglycemia/prediabetes, or undiagnosed DM.18 Though we are unable to espouse any casual mechanisms linking long sleep with DM, it is likely that long sleep may be a consequence of DM or an underlying cardio-metabolic condition (eg, metabolic syndrome). Also, the relationship between long sleep duration and DM may be attributed to an underlying sleep disorder, emotional distress, or mental health issues, which have been linked to DM.19,20 It is also important to note that the magnitude of the association between long sleep and DM was only greater than the magnitude of the association between short sleep and DM in models adjusted for cancer history.
Based on our findings, long sleep duration marginally moderated the relationship between cancer and DM, such that cancer survivors who reported long sleep duration had a 12% lower likelihood of reporting DM. This finding is novel because previous studies indicate that long sleep duration is associated with increased cardiovascular disease and DM risk.14 There are two possible interpretations for our findings. First, long sleep duration may buffer the relationship between cancer and DM. Specifically, long sleep duration among cancer survivors may have unique cardiovascular health benefits. Prior evidence indicating that cancer survivors are at increased risk for short sleep duration, which in turn increases their risk for cardiovascular disease and mortality supports our argument that long sleep duration, may have health benefits for cancer survivors, specifically in DM risk reduction.21 Second, some of the inconsistencies observed in our study may be attributed to the nuances of how sleep impacts certain types of cancers, where several studies have found that long sleep duration is positively associated with colorectal cancer and inversely associated with hormone-derived cancers (like breast cancer).22 Perhaps for our study, long sleep only confers health benefits for individuals who suffer from a hormone-related cancer, and therefore reducing the likelihood of developing DM.23
Our findings that cancer and short sleep duration increased an individual’s risk for DM are consistent with previous work, as mentioned earlier. However, our finding that short sleep duration did not significantly moderate the relationship between cancer and DM is not consistent with our hypothesis, which we hypothesized would exacerbate the relationship. These findings can be interpreted in two ways. First, they reinforce the main effects of cancer and short sleep duration on DM. Second, the nonsignificance of the interaction between cancer and short sleep could be attributed to effects confounders, such as obesity and sleep disorders (eg, sleep apnea).24,25
Limitations and future directions
Although our study found several interesting results, there are a few limitations that should be noted. First, the cross-sectional design of the NHIS prohibits establishing any causal links between cancer and diabetes. Second, the lack of objective sleep duration, diabetes and cancer diagnosis and clinical (insulin resistance) data are subject to self-report bias and prevented us from testing biological mechanisms that undergird the relationship among cancer, sleep, and DM. Third, we did not account for whether our main findings vary by type of cancer through subgroup analyses, which could provide nuanced insight on how certain cancers are related to short or long sleep durations and how the interaction of these specific types of cancers with sleep duration is associated with DM.
To address some of these limitations, future studies should: 1) investigate the longitudinal effects of cancer and sleep duration on DM; 2) utilize objective data to assess whether and how short or long sleep durations affect the shared biological etiology of cancer and DM; 3) investigate if our findings vary across different cancer types; and 4) check whether long sleep duration has a similar protective effect on other cardiovascular or cardiometabolic conditions other than DM.
Conclusion
Our findings demonstrate that cancer history as well as short or long sleep durations are independently associated with DM and might increase an individual’s likelihood of having DM. However, short sleep did not significantly moderate the relationship between cancer and DM, while long sleep duration did suggest that cancer survivors who reported long sleep duration were less likely to report DM. Although these findings do not provide mechanistic insights into glucose homeostasis derangements and DM development and maintenance among cancer survivors, they highlight the importance of sleep as a preventive strategy to stave off DM among cancer survivors. We expect that these findings will help clinicians, interventionists, and health policymakers to integrate sleep as a core feature in cancer survivorship care to reduce risk of comorbid conditions such as DM. A tangible and easy-to-adapt method is to include sleep as part of standard medical screening, assessment, and treatment for cancer survivors, especially individuals at high risk for DM.
The abstract of this paper was presented at the 2016 SLEEP Conference as a poster presentation with interim findings. The poster’s abstract was published in “Poster Abstracts” in SLEEP. Please see reference: Sleep. 2016:39:A271-A271.DOI: EMBASE:72303638.
Acknowledgment
This work was supported by funding from the NHLBI (K01HL135452) and NIMHD (R01MD007716).
Disclosure
The authors report no conflicts of interest in this work.
References
de Nunzio C, Tubaro A. Prostate cancer: Diabetes and prostate cancer--an open debate. Nat Rev Urol. 2013;10(1):12–14. | ||
Singer M. Management of comorbid diabetes and cancer. Oncology. 2007;21(8 Suppl):26–29. | ||
Pandey A, Forte V, Abdallah M, et al. Diabetes mellitus and the risk of cancer. Minerva Endocrinol. 2011;36(3):187–209. | ||
Giovannucci E, Harlan DM, Archer MC, et al. Diabetes and cancer: A consensus report. Diabetes Care. 2010;33:1674–1685. | ||
Klimova T, Chandel NS. Mitochondrial complex III regulates hypoxic activation of HIF. Cell Death Differ. 2008;15(4):660–666. | ||
Solaini G, Baracca A, Lenaz G, Sgarbi G. Hypoxia and mitochondrial oxidative metabolism. Biochim Biophys Acta. 2010;1797(6-7):1171–1177. | ||
Andreazza AC, Andersen ML, Alvarenga TA, et al. Impairment of the mitochondrial electron transport chain due to sleep deprivation in mice. J Psychiatr Res. 2010;44(12):775–780. | ||
Bell EL, Klimova T, Chandel NS. Targeting the mitochondria for cancer therapy: regulation of hypoxia-inducible factor by mitochondria. Antioxid Redox Signal. 2008;10(3):635–640. | ||
Lacedonia D, Carpagnano GE, Crisetti E, et al. Mitochondrial DNA alteration in obstructive sleep apnea. Respir Res. 2015;16(1):47. | ||
Seixas AA, Nunes JV, Airhihenbuwa CO, et al. Linking emotional distress to unhealthy sleep duration: analysis of the 2009 National Health Interview Survey. Neuropsychiatr Dis Treat. 2015;11(2425–2430):2425. | ||
Patel SR, Blackwell T, Ancoli-Israel S, Stone KLOsteoporotic Fractures in Men-MrOS Research Group. Sleep characteristics of self-reported long sleepers. Sleep. 2012;35(5):641–648. | ||
Youngstedt SD, Kripke DF. Long sleep and mortality: rationale for sleep restriction. Sleep Med Rev. 2004;8(3):159–174. | ||
Grandner MA, Seixas A, Shetty S, Shenoy S, Duration S. Sleep Duration and Diabetes Risk: Population Trends and Potential Mechanisms. Curr Diab Rep. 2016;16(11):106. | ||
Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010;71(5):1027–1036. | ||
Holliday EG, Magee CA, Kritharides L, Banks E, Attia J. Short sleep duration is associated with risk of future diabetes but not cardiovascular disease: a prospective study and meta-analysis. PLoS One. 2013;8(11):e82305. | ||
Renehan A, Smith U, Kirkman MS. Linking diabetes and cancer: a consensus on complexity. Lancet. 2010;375(9733):2201–2202. | ||
Leng Y, Cappuccio FP, Wainwright NW, et al. Sleep duration and risk of fatal and nonfatal stroke: a prospective study and meta-analysis. Neurology. 2015;84(11):1072–1079. | ||
Mcfarlane SI, Sica DA, Sowers JR. Stroke in patients with diabetes and hypertension. J Clin Hypertens. 2005;7(5):286–294. | ||
Grandner MA, Drummond SP. Who are the long sleepers? Towards an understanding of the mortality relationship. Sleep Med Rev. 2007;11(5):341–360. | ||
Patel SR, Malhotra A, Gottlieb DJ, White DP, Hu FB, Fb H. Correlates of long sleep duration. Sleep. 2006;29(7):881–889. | ||
Yoon HS, Yang JJ, Song M, et al. Short Sleep Duration and Its Correlates among Cancer Survivors in Korea: the Korea National Health and Nutrition Examination Surveys. Asian Pac J Cancer Prev. 2015;16(11):4705–4710. | ||
Zhao H, Yin JY, Yang WS, et al. Sleep duration and cancer risk: a systematic review and meta-analysis of prospective studies. Asian Pac J Cancer Prev. 2013;14(12):7509–7515. | ||
Lambadiari V, Mitrou P, Maratou E, et al. Thyroid hormones are positively associated with insulin resistance early in the development of type 2 diabetes. Endocrine. 2011;39(1):28–32. | ||
Knutson KL, van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci. 2008;1129:287–304. | ||
Kendzerska T, Leung RS, Hawker G, Tomlinson G, Gershon AS. Obstructive sleep apnea and the prevalence and incidence of cancer. CMAJ. 2014;186(13):985–992. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.