Back to Journals » Journal of Inflammation Research » Volume 14
Models Based on Dynamic Clinicopathological Indices for Predicting Prognosis During the Perioperative Period for Patients with Colorectal Cancer
Authors Ma Y, Lu P, Liang X , Wei S
Received 20 January 2021
Accepted for publication 19 March 2021
Published 21 April 2021 Volume 2021:14 Pages 1591—1601
DOI https://doi.org/10.2147/JIR.S302435
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Ning Quan
Yifei Ma,1 Ping Lu,2 Xinjun Liang,2 Shaozhong Wei1
1Department of Gastrointestinal Oncology Surgery, Hubei Cancer Hospital, The Seventh Clinical School Affiliated of Tongji Medical College, Huazhong University of Science and Technology, Wuhan, People’s Republic of China; 2Department of Abdominal Oncology, Hubei Cancer Hospital, The Seventh Clinical School Affiliated of Tongji Medical College, Huazhong University of Science and Technology, Wuhan, People’s Republic of China
Correspondence: Xinjun Liang
Department of Abdominal Oncology, Hubei Cancer Hospital, The Seventh Clinical School Affiliated of Tongji Medical College, Huazhong University of Science and Technology, 116 Zhuodaoquan South Road, Wuhan, Hubei, 430079, People’s Republic of China
Tel/Fax +86-27-87671663
Email [email protected]
Shaozhong Wei
Department of Gastrointestinal Oncology Surgery, Hubei Cancer Hospital, The Seventh Clinical School Affiliated of Tongji Medical College, Huazhong University of Science and Technology, 116 Zhuodaoquan South Road, Wuhan, Hubei, 430079, People’s Republic of China
Tel/Fax +86-27-87671663
Email [email protected]
Background: Recent studies have found that clinicopathological indices, such as inflammatory and biochemical indices, play a significant role in the prognosis of colorectal cancer (CRC) patients. However, few studies have focused on the effect of dynamic changes in these indicators. In our study, we studied the influence of dynamic changes in inflammatory and biochemical indices on patient outcomes during the perioperative period.
Methods: We enrolled 551 patients from Hubei Cancer Hospital who had undergone radical resection of CRC and collected the results of laboratory examinations performed within 1 week before surgery and at the first admission after surgery. The whole population was randomly divided into the training (386) and testing (185) cohorts. We used postoperative inflammatory and biochemical indices/preoperative inflammatory and biochemical indices (ΔX) to reflect the dynamic changes. Chi-square tests, Kaplan–Meier survival analyses, and univariate and multivariate Cox regression analyses were used to evaluate the prognosis. The prediction accuracies of models for overall survival (OS) and disease-free survival (DFS) were estimated through Harrell’s concordance index (the C-index) and Brier scores. Nomograms of the prognostic models were plotted for evaluations of individualized outcomes.
Results: The median follow-up time of the 551 patients was 35.6 (range: 1.1– 73.8) months. Ultimately, the prognostic models based on age, sex, TNM stage, pathological conditions, inflammatory and biochemical indices, CEA, and CA199 were found to have exceptional performance for OS and DFS. The C-index of the nomogram for OS was 0.806 (95% CI, 0.75– 0.86) in the training cohort and 0.921 (95% CI, 0.87– 0.96) in the testing cohort. The C-index of the nomogram for DFS was 0.781 (95% CI, 0.74– 0.82) in the training cohort and 0.835 (95% CI, 0.78– 0.88) in the testing cohort.
Conclusion: We successfully established a novel model based on inflammatory and biochemical indices to guide clinical decision-making for CRC.
Keywords: colorectal cancer, prognosis, time-dependent receiver operating characteristic curve, nomogram, inflammatory indices, biochemical indices
Introduction
Colorectal cancer (CRC) is the world’s second most deadly cancer.1 For newly diagnosed patients with CRC, clinicians often make decisions about whether to operate based on TNM stage and general condition. The traditional TNM staging system (based on the degree of tumor invasion, lymph node status, and distant metastasis status) has been widely used to predict the prognosis of CRC patients.2,3 However, it represents the biological behavior of tumors and cannot accurately predict the risk of death and recurrence in cancer patients. In fact, the prognosis of tumors is affected not only by TNM stage but also by the systemic inflammatory response.
Although previous studies4–7 have demonstrated a correlation between the preoperative inflammatory response and the prognosis of CRC, few studies have considered the postoperative inflammatory response. The ability of nomograms to visualize predictive models has been shown to be effective in many cancers, and nomograms are superior to the traditional TNM staging system, having personalized predictive power that can quickly guide clinical practice.8,9
Therefore, we attempted to explore the prognostic significance of perioperative inflammatory cells in patients with resectable CRC by jointly considering these factors and other routine biochemical and blood indicators that influence the treatment of CRC and to develop a novel prognostic model incorporating relevant perioperative inflammatory and biochemical markers for the prediction of individual survival outcomes in patients with resectable CRC.
Materials and Methods
Study Population
Overall, 551 patients with histopathologically confirmed CRC who had undergone resection of primary lesions at Hubei Cancer Hospital, Hubei, China, from January 2013 to December 2016 were enrolled in this retrospective analysis. The following clinical parameters were retrieved from medical records: age, sex, body mass index (BMI), family history, history of smoking or drinking, TNM stage and some pathological factors, including degree of tumor differentiation, tumor location, nerve infiltration status, circumferential margin, and vascular cancer embolus status. Laboratory test results, including the results of neutrophil (NEU), lymphocyte (LYM), monocyte (MON), white blood cell (WBC), hemoglobin (HGB), alkaline phosphatase (ALP), lactate dehydrogenase (LDH), direct bilirubin (DBIL), γ-transglutaminase (GGT), carcinoembryonic antigen (CEA), and carbohydrate antigen 19–9 (CA199) tests, were also collected. The inclusion criteria were as follows: (1) age ≥18 years; (2) patients first identified to have primary CRC; and (3) patients who had already undergone eradication of CRC. The exclusion criteria were as follows: (1) previous diagnosis of malignancy; (2) cooccurrence of other cancers; (3) lack of clinical parameters and laboratory results; and (4) other diseases that would have serious impacts on prognosis, such as ischemic heart disease and stroke. This study was supported by the Ethics Committee and Institutional Review Board of Hubei Cancer Hospital, and all patients provided informed consent. This study was conducted in accordance with the Declaration of Helsinki.
Laboratory Parameters
Routine preoperative blood tests and serum biochemical examinations were performed within one week before the surgery. There is no standard for determining the appropriate time for postoperative inflammatory and biochemical profiling. To exclude the influence of postoperative complications, postoperative laboratory tests were obtained after the first postoperative inpatient admission. The median time between postoperative data collection and surgery was 19 (range: 10–39) days, and the mean interval was 24.6 days. To correlate preoperative and postoperative indices, we defined ΔX as the postoperative X value/the preoperative X value (where X stands for one of any of the inflammatory or biochemical indicators).
Follow-Up
Patients were followed up regularly until death or September 1, 2019, according to the 7th edition of the TNM-UICC/AJCC classification system for CRC (which recommends follow-up every 3–6 months for the first 2 years and then every 6 months for the third to fifth years).10 Disease-free survival (DFS) was defined as the period after successful treatment in which there was no appearance of the symptoms or effects of the disease,11 and overall survival (OS) was defined as the time from the date of diagnosis to death or last follow-up.12 Follow-up data for patients were obtained from medical records, laboratory examinations, or telephone follow-up.
Statistical Analyses
Differences between groups were analyzed using the chi-square test or Fisher’s exact test for dichotomous parameters. For clinical parameters, we changed the continuous variables to categorical variables by determining cutoff values via receiver operating characteristic (ROC) curve analyses and utilized these classifications in further statistical analysis. The survival curves were established according to the Kaplan–Meier method, and the differences were analyzed by the Log-rank test. To identify independent prognostic factors, multivariate Cox regression analyses were performed by forward stepwise selection of variables. The efficacy of the prognostic models was estimated by Harrell’s concordance index (the C-index) and the Brier score. Time-dependent ROC curves and calibration curves were plotted to visualize the performance of the models. Nomograms of the prognostic models were plotted for individualized evaluation of OS and DFS. The training set was applied to plot the nomogram based on the results of the multivariable Cox analysis. Differences with a two-tailed P <0.05 were considered to be statistically significant. The time-dependent ROC curve, calibration curve, and nomogram were generated using the “survival ROC”, “time ROC”, “pec” and “regplot” packages of R 3.6.0 (The R Foundation for Statistical Computing, Vienna, Austria). Other statistical analyses were performed using SPSS software, version 23.0 (IBM SPSS, Chicago, IL, USA).
Results
The Optimal Cutoff Values for Variables
According to the ROC curve, the optimal cutoff values for ΔNEU, ΔWBC, ΔMON, ΔLYM, ΔHGB, ΔALP, ΔLDH, ΔDBIL, and ΔGGT were 1.39, 1.11, 1.06, 1.27, 1.32, 1.14, 1.16, 1.86, and 1.83, respectively. In addition, the cutoff values for CEA, CA199, and BMI were 3.5 ng/mL, 35.5 ng/mL, and 25 kg/m2, respectively, which were taken from the reference ranges reported by the Clinical Laboratory Department in Hubei Cancer Hospital. For age, we used the median (65) as the cutoff value. Furthermore, other clinical baseline characteristics are described in Table 1.
 |
Table 1 Demographic and Tumor Characteristics of Colorectal Cancer Patients |
Relationships of Inflammatory and Biochemical Indices with the Prognosis of Patients with Resectable Colorectal Cancer
All included indicators were dichotomized with the cutoffs of the corresponding ROC curves. We found that high levels of ΔNEU (P=0.003), ΔALP (P<0.001), ΔLDH (P=0.001), ΔDBIL (P=0.006), and ΔGGT (P<0.001) were related to poor DFS of patients with resectable CRC in the Kaplan-Meier survival analysis. In addition, high levels of ΔLYM (P<0.001), ΔHGB (P=0.002), ΔNEU (P<0.001), ΔALP (P<0.001), ΔLDH (P<0.001), and ΔGGT (P=0.002) were related to poor OS of patients with resectable CRC in the Kaplan-Meier survival analysis. Next, we performed univariate Cox regression analysis for each of the included indicators and put those indicators with P< 0.1 into the multivariate Cox regression model. In the whole population, after adjusting for differentiation, circumferential margin status, vascular cancer embolus status, nerve infiltration status, TNM stage, CEA, CA199, ΔNEU, ΔLMR, ΔLDH, ΔMON, ΔALP, ΔGGT, and ΔDBIL, we found that ΔMON, ΔALP, and ΔDBIL maintained significant associations with DFS, with HRs (95% CI) of 1.725 (1.228–2.425), 1.589 (1.171–2.157), and 2.325 (1.525–3.547), respectively. After adjusting for age, circumferential margin status, vascular cancer embolus status, nerve infiltration status, TNM stage, CEA, CA199, ΔWBC, ΔMON, ΔLYM, ΔHGB, ΔALP, ΔLDH, ΔGGT, and ΔNEU, we found that ΔNEU still had a presented significant association with OS, with an HR of 1.843 (1.030–3.300) (Table 2).
 |
Table 2 Univariate and Multivariate Analyses of the Factors Affecting Overall Survival and Disease-Free Survival by Cox Proportional Hazard Model |
Predictive Models for Patients with Colorectal Cancer
We constructed prognostic prediction models based on the changes in inflammatory and biochemical indices as well as other baseline indicators. In training cohort, we performed a univariate Cox regression analysis for each indicator, inflammatory cell ratio and routine blood tests, with blood biochemical indicators and related pathological indicators included. Ultimately, age, sex, TNM stage, circumferential margin status, vascular cancer embolus status, nerve infiltration status, ΔWBC, ΔMON, ΔLYM, ΔALP, ΔLDH, ΔGGT, ΔDBIL, ΔNEU, CEA, and CA199 were included in our models. The C-indices of the prognostic models for OS and DFS were 0.806 (95% CI, 0.75–0.86) and 0.781 (95% CI, 0.74–0.82), respectively. One- and 3-year time-dependent ROC curves were generated to determine the performance of the two models (Figure 1). Evaluations of the 1-year and 3-year overall survival rates illustrated the predictive power of the nomogram, as measured by area under the curve (AUC) values, which were 0.883 and 0.823 in the training set and 0.965 and 0.954 in the testing set, respectively. Meanwhile, evaluations of the 1-year and 3-year disease-free survival rates revealed AUCs of 0.836 and 0.811 in the training set and 0.857 and 0.910 in the testing set, respectively. The AUC values (95% CIs) of the two models were stable over time (Figure 2), and the calibration curves also showed good agreement between the prediction and observation in the 1-year and 3-year survival probabilities of OS and DFS, with Brier scores of 0.023 and 0.062 for OS and 0.069 and 0.115 for DFS, respectively (Figures 3 and 4).
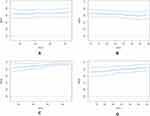 |
Figure 2 Time–AUC curves of the model. Time–AUC curves from the nomograms for the prediction of OS and DFS rates in the training (A and B) and testing (C and D) sets, respectively. |
We further performed a sensitivity analysis excluding patients with advanced CRC. The results show that the prognostic model maintained good performance for OS prediction [C-index: 0.818 (95% CI, 0.74–0.89) and Brier score: 0.009 for 1-year and 0.036 for 3-year OS], and the prognostic model based for DFS prediction [C-index: 0.752 (95% CI, 0.70–0.81) and Brier score: 0.040 for 1-year and 0.095 for 3-year OS]. Nomograms for OS and DFS were plotted based on the models, as shown in Figures 5 and 6, respectively.
 |
Figure 5 Nomogram of prognostic model for OS of colorectal cancer. |
 |
Figure 6 Nomogram of prognostic model for DFS of colorectal cancer. |
Discussion
We not only assessed the impact of dynamic changes in clinicopathological indices on a retrospective series of resectable CRC patients but also built a high-quality prediction model presenting exceptional performance for OS [C-index: 0.806 (95% CI, 0.75–0.86)] and DFS prediction [C-index: 0.781 (95% CI, 0.74–0.82)].
Recent studies have focused on the impact of preoperative inflammatory markers on the outcomes of CRC patients. A high preoperative NLR (neutrophils/lymphocytes) represents a poor prognosis,13 and a low preoperative PLR (platelets/lymphocytes) represents a superior prognosis.14 Few studies have focused on the prognostic significance of postoperative inflammatory indicators, which may be related to the influence of postoperative complications on changes in inflammatory indicators. Xie Ya14 combined preoperative and postoperative NLR and PLR and divided patients into four groups. They found that perioperative NLR/PLR might be a good predictor for prognosis in CRC patients undergoing curative surgery. Joseph C.Y15 also studied the changes in NLR and LMR before and after surgery and identified an optimal period of remeasurement at 21 to 56 days postoperation. Naoki Ashizawa16 investigated the prognostic value of the change in NLR (postoperative NLR/preoperative NLR) and found that it might be a good predictor for prognosis. You W17 found positive that postoperative CEA and CEA increase were independent prognostic factors for stage II and III CRC.
Our study was inspired by the abovementioned studies and included less-researched prognostic markers of inflammation as well as conventional laboratory findings (for example, WBC, platelets, HGB, etc.). These results guide the treatment of patients clinically. For example, low WBC or platelet counts will affect the patient’s chemotherapy. Abnormal liver function will also affect the treatment of patients, so we included not only routine transaminases but also positive indicators in the univariate Cox regression analysis, such as γ-transglutaminase, lactate dehydrogenase, alkaline phosphatase, and direct bilirubin. The ΔNLR was not included in the nomogram because it did not show good predictive performance in our univariate Cox analysis. The changes in perioperative indicators were replaced by the ratio of the value after to before surgery, and the nomogram was drawn from this, and it was found that the nomograms showed good prediction of OS and DFS. A prognostic model based on age, sex, TNM stage, circumferential margin, ΔNEU, ΔWBC, ΔMON, ΔLYM, ΔALP, ΔLDH, ΔDBIL, ΔGGT, ΔCEA, and ΔCA199 was found to present exceptional performance for OS prediction [C-index: 0.806 (95% CI, 0.75–0.86) and Brier score: 0.023]. Another model based on age, sex, TNM stage, circumferential margin, vascular cancer embolus status, ΔLMR, ΔNEU, ΔWBC, ΔMON, ΔLYM, ΔALP, ΔLDH, ΔDBIL, ΔGGT, ΔCEA, and ΔCA199 also presented exceptional performance for DFS prediction [C-index: 0.781 (95% CI, 0.74–0.82) and Brier score: 0.069]. More encouragingly, the model showed better predictive performance after the removal of stage IV patients, with C-indices of 0.818 for OS and 0.752 for DFS. A predictive model considering mutation status (BRAF and KRAS mutation status), sex, performance status, BMI, and laboratory values presented C-indices of 0.68 and 0.62 for progression-free survival.18
In recent years, studies have found that blood-based liquid biopsies can quickly detect some substances in the blood that are shed or released by tumor tissue, which often play an important role in the treatment, diagnosis, and prognosis of tumors. Tumor-derived circulating endothelial cell clusters (ECCs), the serum DNA concentration may play a role in the early diagnosis of tumors. Elevated miR-6803-5p and serum exosomal miR-21 have been associated with the poor prognosis of CRC. There is also a low association between E1317Q and the risk of CRC.19 In addition, mutations in certain genes can be used to determine treatment strategies. For example, KRAS mutations indicate a poor prognosis but can be used to determine whether patients can undergo anti-EGFR therapy.20 Patients with MSI have a better prognosis and respond better to treatment. However, due to the lack of clinical validation, regulatory approval and other issues, its inclusion in routine cancer diagnostics is limited, so it should be included in the establishment of predictive models in future studies. In addition, the conventional inflammatory indicator C reactive protein (CRP) is related to the prognosis of colorectal cancer. The prognostic model with CRP also showed good predictive performance, with a C index of 0.762 for DFS.21 In addition, preoperative lymphocyte-C-reactive protein ratio is a useful marker for perioperative and postoperative treatment of CRC patients.22 As this was a retrospective study with considerable amount of missing relevant data and the clinical accessibility, CRP was not included in our model. Therefore, the identification of a more simple and efficient comprehensive prediction model for colorectal cancer is needed in the future.
Our study also has limitations. Most importantly, we did not know how many days after surgery would be the optimal time to predict prognosis. The changes caused by the stress response and related inflammatory response after surgery cannot be ignored within a few days after surgery. If the time window was extended, the occurrence of postoperative complications and related uncontrollable factors would inevitably interfere with the results. In addition, mutation status (BRAF and KRAS mutation status) and MSI status were not included in this study due to the lack of relevant data. Besides, there lacks a comparison study with other prognosis models from literature applied to the same dataset.
The strengths of this study include the fact that we jointly considered changes in postoperative versus preoperative indicators and incorporated a variety of inflammatory markers that influence clinical decision-making to establish a nomogram that has a high predictive performance, which has never been done before.
In summary, postoperative inflammatory and biochemical indices have significant prognostic value in patients with resectable CRC. Our novel prognostic model incorporating both postoperative and preoperative markers provides superior prognostic prediction. These results provide a new approach to search for prognostic biomarkers in patients with CRC. However, the main findings of the current study need to be interpreted with caution and require external validation in future studies.
Data Availability Statement
The datasets used and/or analyzed during this study are available from the corresponding author upon reasonable request.
Acknowledgments
The authors would like to thank all participants who volunteered to provide data and samples in this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the National Natural Sciences Foundation of China (Grants No. 81772499), the National Key R&D Program of China (Grant No. 2017YFC0908204), the Health commission of Hubei Province scientific research project (Grant No. WJ2017Z020, Grant No. WJ2019H121, Grant No. WJ2017M142, Grant No. WJ2021Z001), the Natural Science Foundation of Hubei Province (Grant No. 2019ACA135), Applied Basic Research Program of Wuhan Science and Technology Bureau (Grant No. 2020020601012250).
Disclosure
The authors report no conflicts of interest related to this work.
References
1. Siegel RL, Miller KD, Goding SA, et al. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020;70(3):145–164. doi:10.3322/caac.21601
2. Weitz J, Koch M, Debus J, Höhler T, Galle PR, Büchler MW Colorectal cancer. Lancet. 2005;365(9454):153–165. (). doi:10.1016/S0140-6736(05)17706-X
3. Balkwill F, Mantovani A Inflammation and cancer: back to Virchow? Lancet. 2001;357(9255):539–545. (). doi:10.1016/S0140-6736(00)04046-0
4. Murata M. Inflammation and cancer. Environ Health Prev Med. 2018;23(1):50. doi:10.1186/s12199-018-0740-1
5. de Visser KE, Eichten A, Coussens LM Paradoxical roles of the immune system during cancer development. Nat Rev Cancer. 2006;6(1):24–37. (). doi:10.1038/nrc1782
6. Jamieson NB, Glen P, McMillan DC Systemic inflammatory response predicts outcome in patients undergoing resection for ductal adenocarcinoma head of pancreas. Br J Cancer. 2005;92(1):21–23. (). doi:10.1038/sj.bjc.6602305
7. Lamb GW, McArdle PA. The connection between the local and systemic inflammatory responses and survival in patients undergoing resection for localized renal cancer. BJU Int. 2008;102(6):756–761. doi:10.1111/j.1464-410X.2008.07666.x
8. Ogino S, Nosho K, Irahara N. Lymphocytic reaction to colorectal cancer is associated with longer survival, independent of lymph node count, microsatellite instability, and CpG island methylator phenotype. Clin Cancer Res. 2009;15(20):6412–6420. doi:10.1158/1078-0432.CCR-09-1438
9. Rozek LS, Schmit SL, Greenson JK. Tumor-infiltrating lymphocytes, crohn’s-like lymphoid reaction, and survival from colorectal cancer. J Natl Cancer Inst. 2016;108(8):. doi:10.1093/jnci/djw027
10. Hu X, Li YQ, Ma X-J, Zhang L, Cai S-J, Peng -J-J. A Risk Signature With Inflammatory and T Immune Cells Infiltration in Colorectal Cancer Predicting Distant Metastases and Efficiency of Chemotherapy. Front Oncol. 2019;9:704. doi:10.3389/fonc.2019.00704
11. Gryfe R, Kim H, Hsieh ETK Tumor microsatellite instability and clinical outcome in young patients with colorectal cancer. N Engl J Med. 2000;342(2):69–77. (). doi:10.1056/NEJM200001133420201
12. Hutchins G, Southward K, Handley K. Value of Mismatch Repair, KRAS, and BRAF Mutations in Predicting Recurrence and Benefits From Chemotherapy in Colorectal Cancer. J Clin Oncol. 2011;29(10):1261–1270. doi:10.1200/JCO.2010.30.1366
13. Pine JK, Morris E. Systemic neutrophil-to-lymphocyte ratio in colorectal cancer: the connection to patient survival, tumour biology and local lymphocytic response to tumour. Br J Cancer. 2015;113(2):204–211. doi:10.1038/bjc.2015.87
14. Haram A. The prognostic value of neutrophil-to-lymphocyte ratio in colorectal cancer: a systematic review. J Surg Oncol. 2017;9999:1–10.
15. Dolan RD, Lim J, McSorley ST, Horgan PG, McMillan DC. The role of the systemic inflammatory response in predicting outcomes in patients with operable cancer: systematic review and meta-analysis. Sci Rep. 2017;7:16717.
16. Ya X, Wenbin F, Wenfeng Y. Perioperative changes of inflammation-based biomarker for predicting the prognosis in colorectal cancer patients: a retrospective analysis. Prz Gastroenterol. 2019;14(4):258–267. doi:10.5114/pg.2019.90252
17. Ashizawa N, Furuya S. Clinical significance of dynamic neutrophil-lymphocyte ratio changes in patients with colorectal cancer. Anticancer Res. 2020;40(4):2311–2317. doi:10.21873/anticanres.14197
18. You W, Yan L, Cai Z, et al. Clinical significances of positive postoperative serum CEA and Post-preoperative CEA Increment in Stage II and III Colorectal Cancer: a Multicenter Retrospective Study. Front Oncol. 2020;10:671. doi:10.3389/fonc.2020.00671
19. Vacante M, Ciuni R, Basile F, Biondi A. The Liquid Biopsy in the Management of Colorectal Cancer: an Overview. Biomedicines. 2020;8(9):308. doi:10.3390/biomedicines8090308
20. Vacante M, Borzì AM, Basile F, Biondi A. Biomarkers in colorectal cancer: current clinical utility and future perspectives. World J Clin Cases. 2018;6(15):869–881. doi:10.12998/wjcc.v6.i15.869
21. Fujino S, Myoshi N. The inflammation-nutrition score supports the prognostic prediction of the TNM stage for colorectal cancer patients after curative resection. Surg Today. 2020;50(2):163–170. doi:10.1007/s00595-019-01861-2
22. Okugawa Y, Toiyama Y, Yamamoto A. Lymphocyte-C-reactive protein ratio as promising new marker for predicting surgical and oncological outcomes in colorectal cancer. Ann Surg. 2020;272(2):342–351. doi:10.1097/SLA.0000000000003239
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



