Back to Journals » Patient Preference and Adherence » Volume 14
Modeling Lay People’s Ethical Attitudes to Organ Donation: A Q-Methodology Study
Authors Hammami MM , Hammami MB, Aboushaar R
Received 8 September 2019
Accepted for publication 18 December 2019
Published 29 January 2020 Volume 2020:14 Pages 173—189
DOI https://doi.org/10.2147/PPA.S230286
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Muhammad M Hammami, 1, 2 Muhammad B Hammami, 3 Reem Aboushaar 4
1Clinical Studies and Empirical Ethics Department, King Faisal Specialist Hospital and Research Centre, Riyadh, Saudi Arabia; 2Alfaisal University College of Medicine, Riyadh, Saudi Arabia; 3Division of Gastroenterology, Department of Medicine, John Hopkins University, Baltimore, MD, USA; 4MS IV, Florida Atlantic University, Boca Raton, FL, USA
Correspondence: Muhammad M Hammami
Clinical Studies and Empirical Ethics Department, King Faisal Specialist Hospital and Research Centre, P O Box # 3354 (MBC 03), Riyadh 11211, Saudi Arabia
Tel +966-11-442-4527
Fax +966-11-442-7894
Email [email protected]
Background: Organ donation is commonly evaluated by biomedical ethicists based largely on principlism with autonomy at the top of the “moral mountain.” Lay people may differ in the way they invoke and balance the various ethical interests. We explored lay people’s ethical attitudes to organ donation.
Methods: Respondents (n=196) ranked 42 opinion-statements on organ donation according to a 9-category symmetrical distribution. Statements’ scores were analyzed by averaging-analysis and Q-methodology.
Results: Respondents’ mean (SD) age was 34.5 (10.6) years, 53% were women, 69% Muslims (30% Christians), 29% Saudis (26% Filipinos), and 38% healthcare-related. The most-agreeable statements were “Acceptable if benefit to recipient large,” “Explicit donor consent and family approval for live donation,” “Acceptable if directed to family member,” and “Explicit donor consent and family approval for postmortem donation.” The most-disagreeable statements were “Donor consent and family approval not required for postmortem donation,” “Acceptable with purely materialistic motivation,” and “Only donor no-known objection for postmortem donation.” Women, Christians, and healthcare respondents gave higher rank to “Explicit donor consent and family approval for live donation,” “Only donor family consent required for postmortem donation,” and “Acceptable if organ distribution equitable,” respectively, and Muslims gave more weight to donor/family harm (p ≤ 0.001). Q-methodology identified various ethical resolution models that were associated with religious affiliation and included relatively “motives-concerned,” “family-benefit-concerned,” “familism-oriented,” and “religious or non-religious altruism-concerned” models. Of 23 neutral statements on averaging-analysis, 48% and 65% received extreme ranks in ≥ 1 women and men Q-methodology models, respectively.
Conclusion: 1) On average, recipient benefit, requirement of both explicit donor consent and family approval, donor-recipient relationship, and motives were predominant considerations; 2) ranking of some statements was associated with respondents’ demographics; 3) Q-methodology identified various ethical resolution models that were partially masked by averaging-analysis; and 4) strong virtue and familism approaches in our respondents provide some empirical evidence against principlism adequacy.
Keywords: organ donation, familism, virtue, ethics of care, principlism, Q-methodology
Background
Organ transplantation has allowed longer and better quality of life while organ donation remains inadequate.1,2 The decision to donate an organ involves balancing various ethical interests that have been widely debated by biomedical ethicists.3–26 However, it is not clear which interests ordinary people invoke and how they weigh them.
Ethical/philosophical issues relevant to postmortem organ donation include: 1) choosing among the various consenting systems12,27 including, mandated “donation,”18,19 mandated choice,4,28 explicit consent by donor and/or their family,21 and presumed consent with a spectrum of enforcement and family involvement.29–32 Lay people opinion regarding the consenting systems is crucial and expected to be culture and religion-specific;7,8,12,27,31,33 2) offering financial and/or medical incentives that may increase donation rates1,9,10 but are potentially connected to commercial trade;23,26,27 3) whether people own their bodies the way they own their property and thus have similar rights to non-interference, donation, and selling13,34 or that body ownership represents a legal relation between the owner and non-owners (rather than between the owner and the owned) and does not have to be a simple binary issue;14,18,19 4) the legitimacy and weight of critical interests (as opposed to experiential interests) that living people may have when they cease to exist.11,35 Does one’s critical interest in the disposition of their organs trump the experiential interests of their family members and/or organ recipients?; 5) whether the body of the diseased is “owned” by the diseased, the family, or the “biomass;”18 and 6) whether an act that is freely chosen has a greater moral value than an act that is not.36 It has been suggested that the ethics of organ donation should be founded on autonomy and non-maleficence37 and the ethics of organ allocation on equity and efficiency.38
Ethicists have generally addressed medical ethical dilemmas directly through deontic (consequentialism and deontology) or aretaic (virtue) approaches39 or through principlism, ie, the four principles of respect for autonomy, beneficence, non-maleficence, and justice.40 Principlism advocates argue that provided application scope and specification41,42 are carefully deliberated, the four principles are the only principles required for ethical resolution,40 which has been criticized by communitarian43 and virtue ethicists.39,44,45
Previous empirical studies on public attitudes toward organ donation27,46–49 have not adequately addressed the underlying thinking process and have usually used independent rating and averaging-analysis, which tend to obscure individual differences. Q-methodology has been used to overcome such limitations.50–53 A type of by-person factor analysis, Q-methodology uses forced-ranking of opinion statements to produce grouping of respondents based on their thinking patterns.54
The aim of this study was to explore how lay people invoke and balance the four ethical principles of principlism and whether they use other principles to achieve ethical resolution in relation to organ donation.
Methods
As part of a series of studies,53 this exploratory cross sectional study was designed to model the ethical decision-making of common people in regard to controversial issues in contemporary medicine. The study was conducted in accordance with the Declaration of Helsinki and was approved by the Research Ethics Committee (REC) of the King Faisal Specialist Hospital and Research Center (KFSH&RC). Written informed consents were provided by all respondents.
Study Instrument Development and Validation
The instrument (Q-set) was author-developed and underwent three rounds of pilot-testing, validation, and revision as previously described.53 The final Q-set (Supplementary material Additional File 1, Q-set statements) consisted of 42 opinion statements divided into four major domains: 1) Consequentialism: a) recipient (3 statements covering graded health benefit to recipient), b) donor (3 statements covering graded social benefit and 3 statements covering graded risk of harm to donor), c) common good (3 statements covering graded benefit to community), and d) ethics of care (3 statements covering graded benefit to donor family, 3 statements covering graded harm to donor family, and 5 statements covering organ allocation choices). 2) Justice (2 statements covering cost-bearing and 2 statements covering State involvement). 3) Rights (7 statements covering various types of consenting options). 4) Virtue (4 statements covering graded moral-materialistic motives and 4 statements covering graded materialistic demand by donor). The statements were randomly numbered and presented to respondents together with instructions and a sorting sheet (Supplementary material Additional File 2, Instructions and sorting sheet). There were nine categories in the sorting sheet, ranging from 1 = strongly disagree to 9 = strongly disagree. The numbers of slots under each category were symmetrically distributed.
Study Instrument Administration
The instrument was self-administered. We first asked respondents to rank the Q-set statements and to comment on their extreme selections. Then, study coordinators checked the sorting sheet to confirm that each statement number was recoded and only once, and asked respondents to correct any copying mistakes of statements numbers onto the sorting sheet. We also collected data on sex, age, degree and place of general education, specific education in ethics (informal, formal), nationality, religious affiliation, occupation (non-healthcare, healthcare), and time used on Q-sorting.
Sample Size and Sampling
Sample size and sampling were based on convenience, in accordance with Q-methodology exploratory nature. Recruitment was via advertising within KFSH&RC as well as in other public places. Adults with at least high school education were eligible to participate if they demonstrated understanding of study purpose and procedures.
Analysis
Q-methodology analysis was performed independently for men and women using PCQ for Windows (PCQ Software, Portland, OR, USA), which has a limit of 120 Q-sorts. The program extracted 6 factors that were then graphically rotated. It considered Q-sorts with significant (p <0.01) loading of ≥ 0.40 as definer Q-sorts and used them to create a model Q-sort for each factor. Model Q-sort denotes how a respondent with 100% loading on a factor would have sorted all the statements. Factors (or ethical attitude models) were construed according to their seven most agreeable and seven most disagreeable statements, post-sorting comments by respondents, and variation of statement scores among and within factors.53 We considered statements to have “neutral” score on averaging-analysis, if the average score was ≥4 and ≤6. We considered statements to be strongly agreed with or strongly disagreed with if they were assigned a Q-methodology score of 8 to 9 or 1 to 2, respectively. In studying the association between attitude models and respondents’ demographics, because of the relatively small number of definer Q-sorts, we grouped respondents who loaded significantly on one factor only together with confounded respondents who loaded more significantly on the same factor. We compared the groups by Analysis of Variance (ANOVA) and Fisher Exact test. We compared individual statements’ mean scores by independent t-test and considered p ˂0.01 as significant. Two-sided p-value and 95% confidence interval are reported. IBM SPSS Statistics version 21 software was used to conduct statistical analysis.
Results
One hundred ninety six respondents participated in the study. Mean (SD) age and sorting time were 34.5 (10.6) years and 28.7 (10.3) minutes, respectively. As shown in Table 1, 53% were women and most were Muslims or Christians and had their general education in Saudi Arabia or the Philippines, which mirrors visitors mix and employees mix of the institution.
 |
Table 1 Demographics of Study Respondents |
Averaging-Analysis
Figure 1 shows mean (SD) scores of the 42 statements. Nine statements were given mean ranking scores of >6. The four most agreeable statements were “42. Acceptable if benefit to recipient large,” “20. Explicit donor consent and family approval for live donation,” “25. Acceptable if directed to family member,” and “3. Explicit donor consent and family approval for postmortem donation.” Their mean (SD) ranking scores were 7.4 (2.1), 6.9 (2.2), 6.9 (2.0), and 6.9 (2.0), respectively. Ten statements were given mean ranking scores of <4. The three most-disagreeable statements were “14. Donor consent and family approval not required for postmortem donation,” “27. Acceptable with purely materialistic motivation,” and “33. Only donor no-known objection for postmortem donation.” Their mean (SD) ranking scores were 2.3 (1.8), 3.0 (2.0), and 3.0 (2.1), respectively.
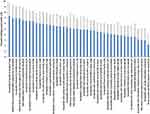 |
Figure 1 Forced-ranking scores of 42 organ donation-related opinion statements, arranged according to ranks. Bars and error bars represent mean and SD of ranking scores on a scale of 1 (strongly disagree) to 9 (strongly agree). For full description of the statements, see Supplementary material Additional File 1, Q-set statements. |
Figure 2 shows the 42 statements grouped according to the most relevant underlying ethical interest. It reveals the graded and overlapping nature of the perceived importance of the various interests. Interestingly, organ donation was as acceptable with “small” benefit to recipient as with “moderate” harm to donor, and as acceptable with “moderate” benefit to donor as with “small” harm to donor. Further, organ donation was most acceptable if directed to a family member and least acceptable if directed to people of the same race, state, or religion; explicit donor consent and family approval for postmortem donation took precedence over other types of consenting; and materialistic motivation reduced acceptability of organ donation when it is stronger (but not when it is weaker) than moral co-motivation.
 |
Figure 2 Forced-ranking scores of 42 organ donation-related opinion statements, arranged according to the most relevant underlying ethical approach. Bars and error bars represent mean and SD of ranking scores on a scale of 1 (strongly disagree) to 9 (strongly agree). For full description of the statements, see Supplementary material Additional File 1, Q-set statements. |
Respondents’ demographics were significantly associated with scores of some of the statements. Women assigned higher mean ranking score to “20. Explicit donor consent and family approval for live donation” (7.5 (2.0) vs 6.4 (2.4) in men, mean (95% confidence interval) difference 1.1 (0.5 to 1.7), p =0.001). Healthcare respondents assigned higher mean ranking score to “13. Acceptable if organ distribution equitable” (6.3 (1.7) vs 5.4 (1.7) in non-healthcare respondents, mean difference 0.9 (0.4 to 1.4), p ˂0.001) and “35. Acceptable with small social benefit to donor family” (4.6 (1.7) vs 3.7 (1.6) in non-healthcare respondents, mean difference 0.9 (0.4 to 1.3), p =0.001), and lower mean ranking score to “31. Acceptable with donor mandating large materialistic self-benefit” (3.1 (1.8) vs 4.0 (2.0) in non-healthcare respondents, mean difference −0.8 (−1.4 to −0.3), p =0.004).
There was a significant association (p ˂0.001) between nationality (Saudis vs Filipinos), place of general education (Saudi Arabia vs the Philippines), and religious affiliation (Muslims vs Christians) but not between these three variables and profession (p ≥0.8). Compared to Christians, Muslims assigned significantly higher mean ranking score to “5. Acceptable if directed to same-religion people” (4.2 (2.3) vs 3.2 (1.9), mean difference 0.9 (0.3 to 1.6), p =0.006) and lower mean ranking score to “32. Acceptable with large harm to donor” (3.1 (2.3) vs 4.8 (2.0), mean difference −1.7 (−2.4 to −1.0), p <0.001), “16. Only donor family consent required for postmortem donation” (4.6 (2.4) vs 6.1 (2.4), mean difference −1.5 (−2.2 to −0.7), p <0.001), “24. Acceptable with moderate harm to donor family” (3.4 (1.5) vs 4.4 (1.7), mean difference −1.3 (−1.8 to −0.8), p <0.001), and “28. Acceptable if harm to donor family small” (4.0 (1.7) vs 5.0 (1.6), mean difference −1.0 (−1.5 to −0.5), p <0.001). The differences in ranking statements 5, 32, 16, 24, and 28 between respondents who had their general education in Saudi Arabia vs the Philippines were in the same direction (ie, Muslims vs Christians) and were also significant (except for statement 5). In addition, compared to their counterparts, respondents who had their general education in Saudi Arabia gave significantly higher mean ranking score to “3. Explicit donor consent and family approval for postmortem donation” (7.2 (1.9) vs 6.2 (2.1), mean difference 1.0 (0.3 to 1.7), p =0.007) and lower mean ranking score to “19. Acceptable if directed to same-race people” (3.4 (1.8) vs 4.6 (1.9), mean difference −1.2 (−1.8 to −0.5), p = 0.001). The differences between Muslims and Christians in ranking these two statements were in the same direction but not significant.
Q-Methodology Analysis
We extracted six factors for women and six for men. The factors were graphically rotated to reduce negative loading and confounding (loading significantly on more than one factor). Extracting more factors did not notably increase the percentage of explained variance and complicated factor interpretation.
Ethical Resolution Models in Women
The six-factor solution accounted for 55% of the total variance and 64 (62%) of the Q-sorts; 13 Q-sorts did not have significant loading on any factor and 27 were confounded. Statements’ score correlation ranged from 0.38 (between models D and E) to 0.56 (between models A and B, A and F, and B and F). Respectively, models A, B, C, D, E, and F had 23, 13, 6, 5, 11, and 6 defining Q-sorts (Q-sorts used by the program to create a model Q-sort); had 15.8, 8.9, 9.2, 5.5, 8.9, and 8.5 eigenvalue, and explained 15%, 9%, 9%, 5%, 9%, and 8% of the variance. Program-generated model Q-sorts, which assign idealized score to each of the 42 statements to indicate how a hypothetical respondent with perfect loading on a factor would order the statements, are presented in Table 2. There were two consensus statements among the six factors, “35. Acceptable with social benefit to donor family” (ranked 3 or 4) and “42. Acceptable if benefit to recipient large” (ranked 8 or 9). There were three differentiating statements, “20. Explicit donor consent and family approval for live donation” (ranked 9, 9, 9, 5, 8, and 9 in factors A to F, respectively), “5. Acceptable if directed to same-religion people (ranked 1, 3, 5, 3, 9, and 2 in factors A to F, respectively), and “13. Acceptable if organ distribution equitable (ranked 8, 6, 6, 7, 7, and 2 in factors A to F, respectively).
 |
Table 2 Idealized Statement Scores for Six Ethical Resolution Models in Women |
Figure 3 shows the idealized scores of the 42 statements for the six factors (models) along with mean statements’ score for all women in the study. None of the models was mono-principled. All models assigned rank 8 or 9 to “42. Acceptable if benefit to recipient large”, indicating a consequentialist orientation that emphasized the recipient over donor, donor family, and community at large. However, ranking score of “40. Acceptable with moderate benefit to recipient” ranged from 4 to 7, and ranking score of “29. Acceptable with small benefit to recipient” ranged from 1 to 5, indicating different degrees of consequentialism. Further, “41. Acceptable if health benefit to donor family large” was among the most agreeable statements for 2 models (B and D), “38. Acceptable with moderate harm to donor” was among the most disagreeable statements for one model (B) and the most agreeable statements for 2 models (D and F), and “39. Acceptable with small benefit to community” was among the most disagreeable statement for one model (F), suggesting different scopes of consequentialism.
 |
Figure 3 Organ donation-related ethical resolution models in women. Data represent mean or program-generated idealized ranking scores on a scale of 1 (strongly disagree) to 9 (strongly agree) of 42 organ donation-related opinion statements, arranged according to the most relevant underlying ethical approach. (A) Models A (gray triangle, “relatively justice-concerned”) and B (light brown circle, “relatively non-maleficence-concerned”). (B) Models C (blue square, “relatively motives-concerned”) and D (dark brown circle, “relatively family-benefit-concerned”). (C) Models E (green diamond, “relatively religious altruism-concerned”) and F (red circle, “relatively familism-oriented”). For reference, mean scores for the entire women cohort are represented by the blue plus symbol in a, b, and c. For description of the resolution models see text. For full description of the statements, see Supplementary material Additional File 1, Q-set statements. |
Women model A was unique in strongly agreeing with “13. Acceptable if organ distribution equitable.” and strongly disagreed with “19. Acceptable if directed to same-race people”, “5. Acceptable if directed to same-religion people”, and “6. Acceptable if directed to same-State people.” It can be classified as “relatively justice-concerned.”
Women model B was unique in strongly disagreeing with “38. Acceptable with moderate harm to donor” and “28. Acceptable if harm to donor family small.” Consistently, it strongly disagreed with “32. Acceptable with large harm to donor” and “24. Acceptable with moderate harm to donor family.” Interestingly, it agreed with “11. Acceptable with donor mandating moderate materialistic self-benefit” which was justified in some of the post-sorting comments as “to be on the safe side if there is healthcare need later.” It can be classified as “relatively non-maleficence-concerned.”
Women model C was unique in strongly disagreeing with “11. Acceptable with donor mandating moderate materialistic self-benefit.” Consistently, it strongly disagreed with “31. Acceptable with donor mandating large materialistic-benefit”, “30. Acceptable with materialistic motivation stronger than moral”, and “27. Acceptable with purely materialistic motivation” and strongly agreed with “8. Acceptable if motivation purely moral” and “4. Acceptable if moral motivation stronger than materialistic.” Interestingly, it strongly agreed with “3. Explicit donor consent and family approval for postmortem donation” and strongly disagreed with “16. Only donor family approval for postmortem donation.” The justification in some of the post-sorting comments was “so that the donor would be rewarded for his/her intentions,” It can be classified as “relatively motives-concerned.”
Women model D was unique in strongly disagreeing with “29. Acceptable with small benefit to recipient.” It strongly agreed with “23. Acceptable if no harm to donor family.”, “25. Acceptable if directed to family member”, “38. Acceptable with moderate harm to donor”, and “41. Acceptable if health benefit to donor family large.” Interestingly, it did not strongly agree/agree with any of the statements related to consenting and assigned rather neutral ranks to “3. Explicit donor consent and family approval for postmortem donation”, “21. Only explicit donor consent for postmortem donation”, and “20. Explicit donor consent and family approval for live donation” (a differentiating statement for this model), suggesting that although explicit donor consent is favored, it is not the most important consideration. It can be classified as “relatively family benefit-concerned.”
Women model E was unique in strongly agreeing with “5. Acceptable if directed to same-religion people” (a differentiating statement for this model) and “17. Acceptable if donor doesn’t mandate materialistic self-benefit.” It strongly disagreed with “27. Acceptable with purely materialistic motivation,” “31. Acceptable with donor mandating large materialistic self-benefit,” and “30. Acceptable with materialistic motivation stronger than moral.” Interestingly, this model was unique in strongly agreeing with “18. Only donor no-known objection and family approval for postmortem donation.” The justification in some of the post-sorting comment was “it is the family religious right to decide.” It can be classified as “relatively religious altruism-concerned.”
Finally, women model F was unique in strongly disagreeing with “13. Acceptable if organ distribution equitable” (a differentiating statement for this model) and “39. Acceptable with small benefit to community.” It strongly disagreed with “6. Acceptable if directed to same-State people” and “5. Acceptable if directed to same-religion people” but strongly agreed with “25. Acceptable if directed to family member”, “38. Acceptable with moderate harm to donor”, and “23. Acceptable if no harm to donor family”, suggesting that family benefit is a high priority. In addition, model F was unique in strongly agreeing with “16. Only donor family approval for postmortem donation”, favoring a family-based decision-making. It can be classified as “relatively familism-oriented.”
Ethical Resolution Models in Men
The six-factor solution accounted for 48% of the total variance and 50 (54%) of the Q-sorts; 19 Q-sorts did not have significant loading on any factor and 23 were confounded. Statements’ score correlation ranged from 0.07 (between models A and F) to 0.65 (between models B and E, and C and E). Respectively, models A, B, C, D, E, and F had 4, 7, 14, 10, 9, and 6 defining Q-sorts; had 4.2, 8.1, 12.4, 8.7, 6.5, and 4.5 eigenvalue, and explained 5%, 9%, 13%, 9%, 7%, and 5% of the variance. Program-generated model Q-sorts are presented in Table 3. There was one consensuses statement, “42. Acceptable if benefit to recipient large.” (ranked 8 or 9). There were no differentiating statements.
 |
Table 3 Idealized Statement Scores for Six Ethical Resolution Models in Men |
Figure 4 shows the idealized scores of the 42 statements for the six models along with mean statements’ score for all men in the study. Similar to women’s models, none of the men models was mono-principled and all six models assigned high rank to “42. Acceptable if benefit to recipient large” (rank 8 or 9). Similarly, ranking score of “40. Acceptable with moderate benefit to recipient” ranged from 5 to 8 and ranking score of “29. Acceptable with small benefit to recipient” ranged from 3 to 7, again indicating a varying degree of consequentialism. Further, “12. Acceptable if benefit to community large” was among the most agreeable statements for 2 models (B and E) and among the most disagreeable statements for one model (F), “41. Acceptable if health benefit to donor family large” was among the most agreeable statements for 3 models (C, D, and F), and “38. Acceptable with moderate harm to donor” was among the most disagreeable statements for one model (E), yet again suggesting different scopes of consequentialism.
 |
Figure 4 Organ donation-related ethical resolution models in men. Data represent mean or program-generated idealized ranking scores on a scale of 1 (strongly disagree) to 9 (strongly agree) of 42 organ donation-related opinion statements, arranged according to the most relevant underlying ethical approach. (A) Models A (gray triangle, “relatively non-religious altruism-concerned”) and B (light brown circle, “relatively common good and rights-concerned”). (B) Models C (blue square, “relatively motives, family benefit, and rights-concerned”) and D (dark brown circle, “relatively ethics of care and rights-concerned”). (C) Models E (green diamond, “relatively motives-concerned”) and F (red circle, “relatively familism-oriented”). For reference, mean scores for the entire men cohort are represented by the blue plus symbol in a, b, and c. For description of the resolution models see text. For full description of the statements, see Supplementary material Additional File 1, Q-set statements. |
Men model A was unique in strongly disagreeing with “6. Acceptable if directed to same-State people.” It strongly disagreed with “5. Acceptable if directed to same religion people” and “19. Acceptable if directed to same-race people”, agreed with “12. Acceptable if benefit to community large” and “13. Acceptable if organ distribution equitable,” and disagreed with “25. Acceptable if directed to family member.” Consistently, it strongly agreed with “17. Acceptable if donor doesn’t mandate materialistic self-benefit” and “8. Acceptable if motivation purely moral” and strongly disagreed with “30. Acceptable with materialistic motivation stronger than moral” and “31. Acceptable with donor mandating large materialistic self-benefit.” It can be classified as “relatively non-religious altruism-concerned.”
Men model B was not unique in its ranking of any of the statements. However, it strongly agreed with “12. Acceptable if benefit to community large” and agreed with “15. Acceptable with moderate benefit to community,” suggesting a common good orientation. On the other hand, it strongly disagreed with “16. Only donor family approval for postmortem donation” and “33. Only donor no-known objection for postmortem donation” and strongly agreed with “21. Only explicit donor consent for postmortem donation.” and “3.Explicit donor consent and family approval for postmortem donation,” suggesting rights orientation. It can be classified as “relatively common good and rights-concerned.”
Men model C was unique in strongly disagreeing with “11. Acceptable with donor mandating moderate materialistic self-benefit.” It strongly disagreed with “30. Acceptable with materialistic motivation stronger than moral” and “27. Acceptable with purely materialistic motivation,” disagreed with “31. Acceptable with donor mandating large materialistic self-benefit,” and agreed with “8. Acceptable if motivation purely moral.” This suggests emphasis on motivation. On the other hand, it strongly agreed with “25. Acceptable if directed to family member” and “41. Acceptable if health benefit to donor family large,” indicating that family benefit is a high priority. Lastly, it equally strongly agreed with “3. Explicit donor consent and family approval for postmortem donation” and “21. Only explicit donor consent for postmortem donation” and strongly disagreed with “33. Only donor no-known objection for postmortem donation,” suggesting rights orientation. It can be classified as “relatively motives, family benefit, and rights-concerned”.
Men model D was unique in strongly agreeing with “23. Acceptable if no harm to donor family” and “7. Acceptable if directed to friend.” It also strongly agreed with “25. Acceptable if directed to family member” and “41. Acceptable if health benefit to donor family large,” suggesting an ethics of care orientation (regarding both family and friends). On the other hand, it was unique in strongly agreeing with “40. Acceptable with moderate benefit to recipient,” and in strongly disagreeing with “37. Acceptable if social benefit to donor large” and it strongly disagreed with “35. Acceptable with social benefit to donor family”, indicating a focus on health (but not social) benefits. In the same vein, it was unique in strongly disagreeing with “18. Only donor no-known objection and family approval for postmortem donation” and it strongly agreed with “21. Only explicit donor consent for postmortem donation.” It can be classified as “relatively ethics of care and rights-concerned.”
Men model E was unique in strongly agreeing with “4. Acceptable if moral motivation stronger than materialistic.” It strongly agreed with “8. Acceptable if motivation purely moral” and strongly disagreed with “27. Acceptable with purely materialistic motivation,” “31. Acceptable with donor mandating large materialistic self-benefit” and “30. Acceptable with materialistic motivation stronger than moral.” It can be classified as “relatively motives-concerned.”
Finally, men model F was unique in strongly disagreeing with “12. Acceptable if benefit to community large.” It also disagreed with “15. Acceptable with moderate benefit to community.” Further, it strongly disagreed with “5. Acceptable if directed to same-religion people” and “19. Acceptable if directed to same-race people” and disagreed with “6. Acceptable if directed to same-State people.” However, it strongly agreed with “41. Acceptable if health benefit to donor family large,” was unique in strongly agreeing with “10. Acceptable if recipient covers cost” and “34. Acceptable if State covers cost,” and agreed with “25. Acceptable if directed to family member,” suggesting that family benefit is a high priority. In addition, model F was unique in strongly agreeing with “16. Only donor family approval for postmortem donation,” favoring a family-based decision-making. It can be classified as “relatively familism-oriented.”
Association Between Ethical Resolution Models and Respondents Demographics
In women, the numbers of Q-sorts that loaded, only or with a higher loading score, on model A, B, C, D, E, or F were 32, 15, 11, 6, 15, and 8, respectively. The corresponding numbers in men were 5, 11, 21, 13, 11, and 6, respectively.
In women, type of resolution models was not significantly associated with occupation (p =0.38), mean age (p =0.65), or mean sorting time (p =0.52). However, it was associated with religious affiliation (p =0.007) and place of education (p =0.04). Most Q-sorts by Muslims loaded on either model A, ie, “relatively justice-concerned” (35%) or model B, ie, “relatively non-maleficence-concerned” (24% compared to 4% by Christians). Most Q-sorts by Christians loaded on either model A (44%) or model C, ie, “relatively motives-concerned” (30% compared to 5% by Muslims). Loading was 5% and 7% on model D, 19% and 11% on model E, and 12% and 4% on model F, by Muslims and Christians, respectively. Similarly, most Q-sorts by respondents who completed their general education in Saudi Arabia loaded on model A (40% compared to 23% by their counterparts) and most Q-sorts by respondents who completed their general education in the Philippines loaded on model C (31% compared to 3% by their counterpart). Loading was 23% and 8% on model B, 0% and 8% on model D, 23% and 23% on model E, and 11% and 8% on model F, by Saudi Arabia-educated and Philippines-educated respondents, respectively.
In men, type of resolution models was not significantly associated with place of education (p =0.13), occupation (p =0.27), mean age (p =0.06), or mean sorting time (p =0.61). However, it was associated with religious affiliation (p =0.03). Loading was 10% and 0% on model A, 19% and 11% on model B, 27% and 42% on model C, 23% and 11% on model D, 19% and 11% on model E, and 2% and 26% on model F, by Muslims and Christians, respectively.
Averaging-Analysis vs Q-Methodology
Out of the 23 statements that had neutral scores on averaging-analysis (defined as mean ranking score ≥4 and ≤6), 11 (48%) and 15 (65%) had extreme scores (defined as idealized score <3 or ˃7) in one or more of the women (Table 2) and men (Table 3) resolution models, respectively.
On the other hand, out of the 14 statements with extreme scores in women’s resolution models A to F, 14%, 29%, 14%, 36%, 21%, and 36%, respectively, had neutral scores on averaging-analysis (Table 2). The corresponding percentages for men’s resolution models A to F were 43%, 29%, 29%, 36%, 29%, and 64%, respectively (Table 3). In fact, some statements were ranked among the most seven agreeable by some models and among the seven most disagreeable by others (statements 5, 13, 16, 18, and 38 in women models and statements 12, 16, 18, and 34 in men models).
There were only four statements that had neutral scores on averaging-analysis and in all women and men models, “9. Acceptable with moderate health benefit to donor family,” “15. Acceptable with moderate benefit to community,” “22. Acceptable with small social benefit to donor,” and “36. Acceptable with moderate social benefit to donor.”
Using Principles Other Than the Four Principles of Principlism
One or more of the eight statements related to motives (statements 4, 8, 11, 17, 26, 27, 30, 31) were among the seven most agreeable and seven most disagreeable statements in 5 (83%) women and 6 (100%) men models (Tables 2 and 3). Further, two of these statements were ranked among the nine most agreeable and three among the ten most disagreeable statements on averaging-analysis.
In addition, one or more of the seven statements related to familism (statements 9, 23, 24, 25, 28, 35, 41) were among the seven most agreeable and seven most disagreeable statements in 5 (83%) women and 4 (67%) men models (Tables 2 and 3). Further, two of these statements were ranked among the nine most agreeable and one among the ten most disagreeable statements on averaging-analysis.
Finally, one or more of the four statements related to communitarianism (statements 6, 12, 15, 39) were among the seven most agreeable and seven most disagreeable statements in 2 (33%) women and 4 (67%) men models (Tables 2 and 3). Further, statement 6 was ranked among the ten most disagreeable statements on averaging-analysis.
Discussion
The aim of this study was to explore how lay people invoke and balance the four ethical principles of principlism and whether they use other principles to achieve ethical resolution in relation to organ donation.
Predominance of Consequentialism
A consequentialist attitude was rather predominant among our respondents. “Acceptable if benefit to recipient large” received the highest mean rank on averaging-analysis and was ranked 8 or 9 in all women and men models, “Acceptable if no harm to donor family” and “Acceptable with moderate benefit to recipient” were among the nine statements with the highest ranks, and “Acceptable with large harm to donor” and “Acceptable with moderate harm to donor family” were among the ten statements with the lowest ranks. This is consistent with the results of a previous study on acceptance of placebo treatment,53 the notion that “good” may be more basic than “right,” and the precedence of “care/harm” over other psychological foundations of morality.55
Individuals with a consequentialist attitude may differ in what they consider the best consequence. Our respondents focus was on recipient’s health benefit. In fact, “Acceptable if directed to same-State people” received the eighth lowest rank and “Acceptable if benefit to community large” received a rather neutral rank, suggesting that communitarian and utilitarian consequentialism were on average less prominent. However, Q-methodology analysis did reveal interesting heterogeneity. For example, women model B was relatively non-maleficence-concerned, women model D was relatively family benefit-concerned, and men model B was relatively common good-concerned. Further, compared to Christians, Muslims put significantly more weight on harms to donor and donor family and more Muslim women loaded on the relatively non-maleficence-concerned model, indicating more harm-aversion. Furthermore, healthcare respondents assigned significantly higher rank to “Acceptable if organ distribution equitable” and “Acceptable with small social benefit to donor family,” consistent with professional organizations’ positions.
Islam shares many social values with Judaism and Christianity.56,57 In the Quran, saving life is praised, “and if any one saved a life, it would be as if he saved the life of the whole people” (Chapter 5, verse 32); not helping others when the cost is trivial is condemned, “So woe to the worshippers, Who are neglectful of their prayers, Those who (want but) to be seen (of men), But refuse (to supply) (even) neighborly needs (Al-Ma’un, small kindnesses)” (Chapter 107, verses 4–7); and consequentialist thinking is acknowledged,
They ask thee concerning wine and gambling. Say: ‘In them is great sin, and some profit, for men; but the sin is greater than the profit.’ They ask thee how much they are to spend; Say: ‘What is beyond your needs.’ Thus doth Allah Make clear to you His Signs: In order that ye may consider- (Their bearings) on this life and the Hereafter. (Chapter 4, verses 219–220)58
Thus, the predominance of consequentialism found in the current study would be expected.
Respect to Autonomy and Acceptance of the Various Consenting Systems
Although consequentialism was the predominant approach by our respondents, respect to autonomy followed closely. Out of the eight consent-related statements, five were among the most agreeable or most disagreeable statements. The most agreeable statement in relation to consenting for postmortem donation was “Explicit donor consent and family approval for postmortem donation” followed by “Only explicit donor consent for postmortem donation,” and the most disagreeable statement was “Donor consent and family approval not required for postmortem donation” followed by “Only donor no-known objection for postmortem donation” “Only donor no-known objection and family approval for postmortem donation,” and “Only donor family approval for postmortem donation” received neutral ranks. This indicates recognition of critical interests and of “ownership” of the body of the diseased by the diseased/family, a demand for explicit consent (opt-in or contracting-in) system, rejection of presumed consent (opt-out or contracting-out) system, and acceptance of a role for donor family veto.
In a previous study on Saudis, we also found that a presumed consent system was less favorable compared to an explicit consent system.27 The presumed consent system raises a conflict between a consequentialist approach (may or may not increase donation rate2,29–32) on one hand and rights and justice approaches on the other (may represent violation of autonomy especially for vulnerable populations5,6), unless one accepts that actual consent is not essential16 or even moral18 for postmortem organ donation.16
The disfavoring of presumed consent could be due to a perceived importance of willing the good act,21,36 which was reflected in the comments of some of our respondents (Women model C). However, “Acceptable if equitably State-forced after death,” which represents a mandated “donation” system, received a neutral rank, suggesting that the preference for an explicit consent system may be due in part to distrust in the medical establishment, and more a preference for being informed than a preference for self-decision-making.
Q-methodology revealed subtle differences. For example, women model F and men model F were relatively familism-oriented, favoring a family-based consenting/decision-making, and men models B, C, and D were relatively more rights-concerned.
Ethics of Care and Familism
A family ethics of care orientation was apparent in our study. “Acceptable if directed to family member” received the third highest rank, whereas “Acceptable if directed to same-race people,” “Acceptable if directed to same-State people,” and “Acceptable if directed to same-religion people” were among the 10 statements with the lowest ranks. “Acceptable if directed to friend” and “Acceptable if organ distribution equitable” received rather neutral ranks. Moreover, “Acceptable with no harm to donor family” received the eighth highest rank and “Acceptable with moderate harm to donor family” received the ninth lowest rank. Of note, the concept of ethics of care (moral actions centers on interpersonal relationship) is clearly recognized in the Quran,
Serve Allah, and join not any partners with Him; and do good - to parents, kinsfolk, orphans, those in need, neighbours who are near, neighbours who are strangers, the companion by your side, the wayfarer (ye meet), and what your right hands possess: For Allah loveth not the arrogant, the vainglorious. (Chapter 4, verse 36)58
Familism, a prevalent ethos in East Asia, involves more than caring for the family. In familism, individuals are family-centered, depend on their family for identity and various needs, and regard their lives to belong to their family.7,59 Consequently, there is a family rather than individual autonomy and the family makes decisions collectively in a way that promotes its interest. In the People's Republic of China, families are given the legal option to over-rule an individual’s wish to donate.7 Our respondents assigned slightly higher rank to “Explicit donor consent and family approval for postmortem donation” than to “Only explicit donor consent for postmortem donation,” indicating a perceived importance of involving donor family in decision-making. Q-methodology revealed models that were relatively more concerned about donor family benefit (women model D and men model C) or family and friends benefits (men model D) and models that were fully familism-oriented (women model F and men model F).
Interestingly, familism orientation appeared stronger in Christians/Philippines-educated than Muslims/Saudi Arabia-educated respondents (giving higher mean rank to “Only donor family consent required for postmortem donation” and lower mean rank to “Explicit donor consent and family approval for postmortem donation,” respectively, and relatively more Christian men loaded on familism-oriented model) and stronger in women than men (women gave higher mean rank to “Explicit donor consent and family approval for live donation”).
Virtue Approach and Importance of Motives
Principlism has been criticized for neglecting emotional and personal factors39 and for being narrow and giving autonomy the place of honor.43 Our empirical data support such a view. “Acceptable if motivation purely moral” and “Acceptable if moral motivation stronger than materialistic” received the sixth and seventh highest ranks, respectively, and “Acceptable with purely materialistic motivation” and “Acceptable with materialistic motivation stronger than moral” the second and fourth lowest ranks, respectively. This is in line with previous results showing that judgment of an action’s wrongness/permissibility by lay people depends partly on the agent’s mental status60 and provides some evidence against the argument that the four principles of principlism are sufficient for universalizable normative morality.40–42
Organ donation has long relied on altruism, wherein the moral value of an action is focused on its beneficial impact to others, without regards to self-interest consequences.16 However, certain kinds of regulated financial incentives have been considered7,9,16,22 as they may increase organ supply based on basic economics,9 out of fairness to donors, and recognizing that even with altruism there is usually some gain such as intrinsic satisfaction, expectation of reciprocation, reputation gain, and reward in life after death. Arguments against incentives include that they can negatively affect an altruistic culture, exploit vulnerable people, reduce respect for human body sanctity, and crowd out altruistic donation. Our previous study on Saudis showed disfavoring of both medical and monetary incentives.27 In the current study, “Acceptable with donor mandating large materialistic self-benefit” received the sixth lowest rank, with lower mean rank by healthcare respondents compared to their counterpart. However, our respondents were rather silent in regard to mandating moderate, small, and no materialistic self-benefit, which is consistent with a supererogatory (rather than obligatory) altruism, wherein demanding material benefits for one’s organ would not be wrong but would be non-supererogatory.16
Q-methodology revealed models that were relatively motives-concerned (women model C and men models C and E) and models that were not only concerned about motives but also about organ allocation. The latter could be classified into religious altruism-concerned (women model E) and non-religious altruism-concerned (men model A) models. Interestingly, relatively more Christians and Philippines-educated women loaded on the motives-concerned model, relatively more Muslim women loaded on the religious altruism-concerned model, and Muslims in general assigned higher mean rank to “Acceptable if directed to same-religion people,” which may be due to some degree of in-group favoritism or some necessary religious observances.
Given the overall picture of consequentialist orientation, the relatively motives-concerned models are consistent with a utilitarianism version that only considers intended consequences.
Finally, one advantage of Q-methodology is its tendency to avoid the depersonalization of averaging-analysis.50–53 This was obvious in this study. Out of the 23 statements that received neutral ranks on averaging-analysis, 48–65% received extreme ranks in one or more of the women and men models, and out of the 14 statements with extreme ranks in a women or men model, 14-64% received neutral ranks on averaging-analysis. The causes underlying the observed variability in ethical attitudes are likely multifactorial. People may have different interpretations, prioritization, scope,41 or specification42,61,62 of the same ethical principles due in part to the circumstances they were raised in. Alternatively, moral reasoning may be based on analogical reasoning, in which paradigm cases not ethical principles are more influential42 or may be a post hoc construct that functions to justify judgements automatically reached by moral intuition.63
Study Strengths and Limitations
The study instrument’s design minimized the order effect and the tendency to respond in an overall way and/or assign maximum value to a huge number of items, by using shuffled statements and forced-ranking, respectively. It also allowed minimizing the influence of assertiveness seen with complete rank-ordering, the influence of proclivity to categorize seen with dichotomization, and moral credentialing bias, ie, affirming one’s pro-social values may affect subsequent choices.
The study has several limitations. First, convenience sampling, restricting recruitment to educated individuals, and the fact that most respondents happened to be Saudi or Filipinos and Muslims or Christians limit study generalizability. Further, different individuals may assign different values to organ donation and may have different understanding of the process. Second, the Q-set did not include all of the statements related to organ donation discourse. As an example, the mandated choice consenting system was not covered. Third, it is likely that there are ethical attitude models that were not identified in our study, consistent with the fact that Q-methodology is exploratory and not exhaustive. Fourth, as Q-methodology gives impressionistic conclusions, there is overlap among the identified models and some subjectivity in their interpretation.
Conclusions
In exploring lay people’s ethical attitudes to organ donation, using forced-ranking of 42 opinion statements, we found that: 1) on average, recipient benefit, requirement of both explicit donor consent and family approval, donor-recipient relationship, and motives were the predominant considerations; 2) ranking of some opinion statements was associated with respondents’ demographics; 3) Q-methodology identified several ethical resolution models that were partially masked by averaging-analysis, were associated with religious affiliation, and included relatively “motives-concerned,” “family-benefit-concerned,” “familism-oriented,” and “religious or non-religious altruism-concerned” models; 4) strong virtue and familism approaches in our respondents provide some empirical evidence against the adequacy of principlism. The results enrich the organ donation debate and shed light on potential differences between how ethicists and lay people invoke and balance the various ethical interests/principles.
Abbreviations
ANOVA, Analysis of variance; KFSH&RC, King Faisal Specialist Hospital and Research Center; REC, Research Ethics Committee; SD, Standard deviation.
Ethics Approval and Consent to Participate
The study complied with the Declaration of Helsinki and was approved by the Research Ethics Committee (REC) of the King Faisal Specialist Hospital and Research Center (KFSH&RC). Written informed consents were provided by all respondents.
Data Sharing Statement
Additional data are available under Supplementary Material-Additional File 1 and Additional File 2. Raw data are available for the corresponding author upon request.
Acknowledgments
The authors would like to thank the staff of the Clinical Studies and Empirical Ethics Department for their help in collecting data.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Langone AJ, Helderman H. Disparity between solid-organ supply and demand. N Eng J Med. 2003;349:704–706. doi:10.1056/NEJMe038117
2. Abadie A, Gay S. The impact of presumed consent legislation on cadaveric organ donation: a cross-country study. J Health Econ. 2006;25(4):599–620. doi:10.1016/j.jhealeco.2006.01.003
3. English V, Sommerville A. Presumed consent for transplantation: a dead issue after Alder Hey? J Med Ethics. 2003;29:147–152. doi:10.1136/jme.29.3.147
4. Chouhan P, Draper H. Modified mandated choice for organ procurement. J Med Ethics. 2003;29:157–162. doi:10.1136/jme.29.3.157
5. Pierscionek BK. What is presumed when we presume consent? BMC Med Ethics. 2008;9:8. doi:10.1186/1472-6939-9-8
6. Lawson A. Presumed consent for organ donation in the United Kingdom. JICS. 2008;9(2):116–117.
7. Wu Y, Elliott R, Li L, Yang T, Bai Y, Ma W. Cadaveric organ donation in China: a crossroads for ethics and sociocultural factors. Medicine (Baltimore). 2018;97(10):e9951. doi:10.1097/MD.0000000000009951
8. Golmakani MM, Niknam MH, Hedayat KM. Transplantation ethics from the Islamic point of view. Med Sci Mont. 2005;11(4):RA105–109.
9. Clark PAC. Financial incentives for cadaveric organ donation: an ethical analysis. Internet J Law Healthcare Ethics. 2006;4(1).
10. Larijani B, Sadeghi S, Jessri M, Zahedi F. Financial incentives in organ transplantation: ethical views. Iran J Allergy Asthma Immunol. 2007;6(Suppl. 5)):39–45.
11. Glannon W. Do the sick have a right to cadaveric organs? J Med Ethics. 2003;29:153–156. doi:10.1136/jme.29.3.153
12. Simpson PJ. What are the issues in organ donation in 2012? Br J Anaesth. 2012;108(Suppl 1):i3–i6. doi:10.1093/bja/aer352
13. Fabre C. Whose Body Is It Anyway? Justice and the Integrity of the Person. Oxford: Oxford University Press; 2006:72–96.
14. Björkman B, Hansson SO. Bodily rights and property rights. J Med Ethics. 2006;32:209–214. doi:10.1136/jme.2004.011270
15. Dunstan GR. The ethics of organ donation. B Med Bull. 1997;53(4):921–939. doi:10.1093/oxfordjournals.bmb.a011659
16. Dalal AR. Philosophy of organ donation: review of ethical facets. World J Transplant. 2015;5(2):44–51. doi:10.5500/wjt.v5.i2.44
17. Saunders B. Normative consent and opt-out organ donation. J Med Ethics. 2010;36(2):84–87. doi:10.1136/jme.2009.033423
18. Emson HE. It is immoral to require consent for cadaver organ donation. J Med Ethics. 2003;29:125–127. doi:10.1136/jme.29.3.125
19. Harris J. Organ procurement: dead interests, living needs. J Med Ethics. 2003;29:130–134. doi:10.1136/jme.29.3.130
20. Truog RD. Consent for organ donation–balancing conflicting ethical obligations. N Engl J Med. 2008;358(12):1209–1211. doi:10.1056/NEJMp0708194
21. Zink S, Werlieb SL. Forced altruism is not altruism. Am J Bioethics. 2004;4:29–31. doi:10.1080/15265160490906727
22. Arnold R, Barlett S, Bernat J. Financial incentives for cadaver organ donation: an ethical reappraisal. Transplantation. 2002;73(8):1361–1367. doi:10.1097/00007890-200204270-00034
23. Bruzzone P. Financial incentives for organ donation: a slippery slope toward organ commercialism? Transplant P. 2010;42(4):1048–1049. doi:10.1016/j.transproceed.2010.03.058
24. Byrne MM, Thompson P. A positive analysis of financial incentives for cadaveric organ donation. J Health Economics. 2001;20:69–83. doi:10.1016/S0167-6296(00)00065-5
25. Haddow G. “Because you’re worth it?” The taking and selling of transplantable organs. J Med Ethics. 2006;32:324–328. doi:10.1136/jme.2005.013805
26. Delmonico FL, Arnold R, Scheper-Hughes N, Siminoff LA, Kahn J, Youngner SJ. Ethical incentives – not payment – for organ donation. N Engl J Med. 2002;346:2002–2005. doi:10.1056/NEJMsb013216
27. Hammami MM, Abdulhameed HM, Concepcion KA, et al. Consenting options for posthumous organ donation: presumed consent and incentives are not favored. BMC Med Ethics. 2012;13:32. doi:10.1186/1472-6939-13-32
28. Spital A. Mandated choice: the preferred solution to the organ shortage? Arch Intern Med. 1992;152:2421–2424. doi:10.1001/archinte.1992.00400240045007
29. English V. Is presumed consent the answer to organ shortage? Yes. BMJ. 2007;334:1088. doi:10.1136/bmj.39199.492894.AD
30. Wright L. Is presumed consent the answer to organ shortage? No. BMJ. 2007;334:1089. doi:10.1136/bmj.39199.492894.AD
31. Rithalia A, McDaid C, Suekarran S, Myers L, Sowden A. Impact of presumed consent for organ donation on donation rates: a systematic review. BMJ. 2009;338:a3162. doi:10.1136/bmj.a3162
32. Horvat LD, Cuerden MS, Kim SJ, Koval JJ, Young A, Garg AX. Informing the debate: rates of kidney transplantation in nations with presumed consent. Ann Intern Med. 2010;153:641–649. doi:10.7326/0003-4819-153-10-201011160-00006
33. Morgan M, Adams OP, Seed PT, Jones R. Ethnicity and attitudes to deceased kidney donation: a survey in Barbados and comparison with black Caribbean people in United Kingdom. BMC Public Health. 2010;10:266. doi:10.1186/1471-2458-10-266
34. Kass LR. Bioethics. In: Shannon TA, editor. Organs for Sale? Propriety, Property and the Price of Progress. Vol. 4. New Jersey: Paulist Press; 1993:468–488.
35. Dworkin R. Life’s Dominion. New York: Vintage Books; 1993:199–213.
36. Young L, Saxe R. It’s not just what you do, but what’s on your mind: a review of Kwame Anthony Appiah’s “experiments in ethics”. Neuroethics. 2010;3:201–207. doi:10.1007/s12152-010-9066-4
37. Truog RD, Miller FG, Halpern SD. The dead-donor rule and the future of organ donation. N Engl J Med. 2013;369(14):1287–1289. doi:10.1056/NEJMp1307220
38. Halpern SD, Goldberg D. Allocating organs to cognitively impaired patients. N Engl J Med. 2017;376(4):299–301. doi:10.1056/NEJMp1613858
39. Campbell A. The virtues (and vices) of the four principles. J Med Ethic. 2003;29:292–296. doi:10.1136/jme.29.5.292
40. Gillon R. Ethics needs principles – four can encompass the rest – and respect for autonomy should be “first among equals”. J Med Ethics. 2003;29:307–312. doi:10.1136/jme.29.5.307
41. Gillon R. Medical Ethics: four Principles plus attention to scope. BMJ. 1994;309:184. doi:10.1136/bmj.309.6948.184
42. Beauchamp T. Methods and principles in biomedical ethics. J Med Ethics. 2003;29:269–274. doi:10.1136/jme.29.5.269
43. Callahan D. Principlism and communitarianism. J Med Ethics. 2003;29:287–291. doi:10.1136/jme.29.5.287
44. Cowley C. The dangers of medical ethics. J of Med Ethics. 2005;31:739–742. doi:10.1136/jme.2005.011908
45. Gardiner P. A virtue ethics approach to moral dilemmas in medicine. J Med Ethics. 2003;29:297–302. doi:10.1136/jme.29.5.297
46. Alam AA. Public opinion on organ donation in Saudi Arabia. Saudi J Kidney Dis Transplant. 2007;18(1):54–59.
47. Naçar M, Cetinkaya F, Baykan Z, Poyrazoğlu S. Attitudes and behaviors of students from the faculty of theology regarding organ donation: a study from Turkey. Transplant Proc. 2009;41(10):4057–4061. doi:10.1016/j.transproceed.2009.09.084
48. Saleem T, Ishaque S, Habib N, et al. Knowledge, attitudes and practices survey on organ donation among a selected adult population of Pakistan. BMC Med Ethics. 2009;10:5. doi:10.1186/1472-6939-10-5
49. Altraif IH, Al Sebayel MI, Nondo H. knowledge and attitude towards organ donation among males in Riyadh, Saudi Arabia. Saudi J Kidney Dis Transpl. 1996;7(2):135–138.
50. Hammami MM, Al Gaai E, Hammami S, Attala S. Exploring end of life priorities in Saudi males: usefulness of Q-methodology. BMC Palliat Care. 2015;14:66. doi:10.1186/s12904-015-0064-5
51. Hammami MM, Hammami S, Amer HA, Khodr NA. Typology of end-of-life priorities in Saudi females: averaging analysis and Q-methodology. Patient Prefer Adherence. 2016;10:781–794. doi:10.2147/PPA.S105578
52. Hammami MM, Abuhdeeb K, Hammami MB, De Padua SJS, Al-Balkhi A. Prediction of life-story narrative for end-of-life surrogate’s decision-making is inadequate: a Q-methodology study. BMC Med Ethics. 2019;20:28. doi:10.1186/s12910-019-0368-8
53. Hammami MM, Hammami S, Aboushaar R, AlJomah A. Lay people’s ethical attitudes to placebo treatment: a Q-methodology study. Patient Prefer Adherence. 2019. doi:10.2147/PPA.S216565
54. Brown S. Q Methodology and Qualitative research. Qual Health Res. 1996;6(4):561–567. doi:10.1177/104973239600600408
55. Graham J, Haidt J, Nosek B. Liberals and conservatives rely on different moral foundations. J Pers Soc Psychol. 2009;96(5):1029–1046. doi:10.1037/a0015141
56. Daar SA, Khitamy A. Bioethics for clinicians: 21. Islamic Bioethics CMAJ. 2001;164(1):60–63.
57. Randhawa G, Brocklehurst A, Pateman R, Kinsella S, Parry V. Faith leaders united in their support for organ donation: findings from the UK organ donation taskforce study. Transpl Int. 2010;23(2):140–146. doi:10.1111/j.1432-2277.2009.00952.x
58. The meanings of The Holy Qur’an by Abdullah Yusufali. Available from: http://www.islam101.com/quran/yusufAli/index.htm.
59. Nagai H. Blood ties and trust: a comparative history of policy on family consent in Japan and the United States. Monash Bioeth Rev. 2017;34:226–238. doi:10.1007/s40592-017-0069-3
60. Cushman F. Crime and punishment: distinguishing the roles of causal and intentional analyses in moral judgment. Cognition. 2008;108:353–380. doi:10.1016/j.cognition.2008.03.006
61. Macklin R. Applying the four principles. J Med Ethics. 2003;29:275–280. doi:10.1136/jme.29.5.275
62. Macklin R. Can one do good medical ethics without principles? J Med Ethics. 2015;41(1):75–78. doi:10.1136/medethics-2014-102354
63. Haidt J. The emotional dog and its rational tail: a social intuitionist approach to moral judgment. Psychol Rev. 2001;108(4):814–834. doi:10.1037/0033-295X.108.4.814
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
