Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 10 » Issue 1
Misidentification of airflow obstruction: prevalence and clinical significance in an epidemiological study
Authors Pothirat C , Chaiwong W , Phetsuk N, Liwsrisakun C
Received 11 January 2015
Accepted for publication 23 February 2015
Published 11 March 2015 Volume 2015:10(1) Pages 535—540
DOI https://doi.org/10.2147/COPD.S80765
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Chaicharn Pothirat, Warawut Chaiwong, Nittaya Phetsuk, Chalerm Liwsrisakun
Division of Pulmonary, Critical Care and Allergy, Department of Internal Medicine, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand
Background: The fixed threshold criterion for the ratio of forced expiratory volume in the first second to forced vital capacity (FEV1/FVC) <0.7 is widely applied for diagnosis of airflow obstruction (AO). However, this fixed threshold criterion may misidentify AO, because thresholds below the fifth percentile of normal FEV1/FVC (lower limit of normal; LLN) vary with age. This study aims to identify the prevalence of AO misidentification and its clinical significance.
Materials and methods: A cross-sectional population-based study was conducted to identify the prevalence of chronic respiratory diseases in adults older than 40 years of age who live in municipal areas of Chiang Mai province, Thailand. All randomly selected subjects underwent face-to-face interviews and examinations by pulmonologists, and received chest radiographs and post-bronchodilator spirometry. AO misidentification was classified into under- or overestimated AO subgroups. Underestimated AO was defined as ratio of FEV1/FVC greater than the fixed threshold, but below the LLN criteria. Overestimated AO was defined as the ratio of FEV1/FVC below the fixed threshold but greater than the LLN criteria. The clinical significance of each misidentified subject was then explored.
Results: There were 554 subjects with a mean age of 52.9±10.1 years and a percent predicted FEV1 of 85.5%±15.4%. The prevalence of AO misidentification was 5.6% (31/554), and all subjects belonged to the underestimated subgroup. Clinical significance of underestimated subjects included clinical AO disease of 22.6% (7/31) (three subjects with chronic obstructive pulmonary disease [COPD] and four subjects with asthma); chronic respiratory symptoms of 54.8% (17/31) (mostly associated with chronic rhinitis, 70.6% [12/17]); and only 12.9% (4/31) were identified as non-ill subjects.
Conclusion: The prevalence of AO misidentification in this population was significant, and all were underestimated subjects. Most underestimated subjects had clinical significance as related to obstructive airway diseases and chronic respiratory symptoms, mostly associated with rhinitis.
Keywords: spirometry, airflow obstruction, chronic obstructive pulmonary disease, asthma
Introduction
Previous studies have shown marked variation in the prevalence of chronic obstructive airway disease due to differences in survey methods, diagnostic criteria, and analytic approaches.1–4 A number of different diagnostic criteria were used in these studies, including self-reporting, physician diagnosis, diagnosis based on the presence of respiratory symptoms, and diagnosis based on the presence of airflow obstruction (AO) either by pre- or post-bronchodilator spirometric values. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria5 defines chronic obstructive pulmonary disease (COPD) as a ratio of post-bronchodilator forced expiratory volume in the first second to forced vital capacity (FEV1/FVC) of <0.7, which is in agreement with both the American Thoracic Society (ATS) and the European Respiratory Society (ERS).6 As FEV1/FVC ratio varies with age, using a fixed threshold criterion may result in over- or underestimation of COPD, especially in advancing or young age groups.7–9 GOLD guidelines also suggest defining AO by a reduced FEV1/FVC below the statistically defined fifth percentile of normal (lower limit of normal; LLN) in order to minimize potential misclassification.10 By using a different criterion for diagnosis of AO, there are two possible discordant results in reference to misidentified AO subjects. Subjects with LLN ≤ FEV1/FVC <0.7 are identified as overestimated subjects, and those subjects with 0.7< FEV1/FVC ≤ LLN are identified as underestimated subjects. As FEV1/FVC declines with age, overestimated subjects should be found in advancing age groups, and underestimated subjects should be found in younger age groups.9 The most appropriate criterion to define AO remains controversial.5 Although many studies evaluate AO by using the LLN criterion,11–16 only a few have attempted to determine the clinical impact of overestimated and underestimated subjects.11,12 A study by Mannino et al11 that enrolled 4,965 elderly patients (age ≥65 years) for 11 years found that overestimated subjects were more likely to die and to have COPD-related hospitalizations compared to subjects who had normal spirometry. In contrast, Cerveri et al12 followed up 6,249 young participants aged between 20 and 44 years for 9 years and discovered that underestimated subjects had a significantly higher risk of developing FEV1 below 80% predicted and a significantly higher use of health care resources due to respiratory problems. Therefore, over- or underestimated subjects may not be a truly positive or negative phenomenon. In the current study, we analyzed data from our population-based study to identify the prevalence of AO misidentification (over- and underestimated subjects) and explored its clinical significance.
Materials and methods
This study was one part of a cross-sectional population-based study, known as the Chiang Mai Lung Health Study, which was set up to identify the prevalence of chronic respiratory diseases in adults older than 40 years of age living in municipal areas of Chiang Mai province. Sample size was calculated using Slovin’s formula,17 based on a total population of 60,000 people. A minimal sample size of 398 was determined, and with 60% of patients expected to deny participation, we planned to enroll approximately 560 subjects. Subjects were randomly selected from those residing in detached houses (1:3) and only one subject per house was enrolled.
All relevant data including age, sex, smoking history, family history of atopic diseases, respiratory symptoms, and previous diagnosis of respiratory diseases was reviewed from written questionnaires. The respiratory questionnaire was adapted from the European Community Respiratory Health Survey (ECRHS)18 (for information on general health, chronic respiratory symptoms, and previous physician-diagnosed respiratory diseases) as well as from the International Study of Asthma and Allergy in Childhood (ISAAC)19 (for chronic rhinitis and asthma screening). Subjects were invited to the pulmonary administrative office at the hospital to confirm their information by face-to-face interviews, and to be physically checked by pulmonologists from the study team. Each subject underwent a chest radiograph and post-bronchodilator pulmonary function test in the form of a standard chest radiograph and standard ATS/ERS post-bronchodilator spirometry.6 Interpretation of AO in each subject was independently based on two standard criteria: 1) a fixed threshold criterion (a ratio of post-bronchodilator FEV1/FVC <0.7); and 2) a LLN criterion (a ratio of post-bronchodilator FEV1/FVC below the cut-off value set at the fifth percentile of the normal distribution derived from healthy lifetime non-smokers in Thailand).20,21 Only data from misidentified AO subjects were analyzed in the current study. Ethics approval was granted by the Ethics Committees of the Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand.
Clinical definitions
Classification of AO based on two criteria is shown in Table 1. Definite AO subjects were defined as those whose lung function met both fixed threshold and LLN criteria. Misidentified AO subjects were defined as those whose lung function met only one criterion (either fixed threshold or LLN criterion). The latter category was further classified into two subgroups: 1) overestimated subjects, defined as those whose lung function met only the fixed threshold criterion; and 2) underestimated subjects, defined as those whose lung function met only the LLN criterion. Non-ill subjects referred to subjects without chronic respiratory symptoms, no previous diagnosis of any chronic respiratory diseases, normal general physical examination, and normal chest radiographs. Asthma subjects were defined as subjects with a positive history of wheezing in the past year (a current wheezer), with a post-bronchodilator FEV1/FVC >0.7 (for chronic smokers >5 pack-years) or any FEV1/FVC ratio (for a non-smoker or a person smoking <5 pack-years) and no pulmonary infiltration, pleural effusion, bronchiectasis, or mass on chest radiographs, which were possible causes of wheezing. A subset of COPD subjects in misidentified AO was defined as subjects with abnormal chest radiographs compatible with the COPD (pulmonary hyperinflation with a flattened diaphragm). Chronic rhinitis subjects were defined by the presence of recurrent or chronic symptoms of nose blockage, posterior nasal drip, sneezing, or an intermittently runny nose without fever in the past year. Pulmonary tuberculosis (TB) subjects were defined as those with physician-diagnosed pulmonary TB or abnormal chest radiographs compatible with the disease (fibrotic scar with or without bronchiectasis, or fibronodular or patchy infiltration with or without thin-wall cavitation in the apicoposterior segment of the upper lobe). Undetermined subjects were subjects with chronic respiratory symptoms but no previous diagnosis of any chronic pulmonary diseases who presented with a normal general physical examination and normal chest radiographs.
Statistical analysis
Results for numerical values were expressed as means ± standard deviation (SD) and those for categorical data were expressed as absolute frequencies and percentages. Unpaired t-tests and chi-square tests were used to compare differences between groups for numerical values and categorical data, respectively. Statistical significance was set at P<0.05. All analyses were carried out with the SPSS statistical package, version 16 for Windows.
Results
A total of 574 subjects were screened for the study; 20 were excluded, three due to absence of spirometric data and 17 due to unacceptable spirometry. Almost half the subjects were in the middle age group (48.2%), whereas only 7.8% were elderly with an age of ≥70 years (Figure 1). Baseline demographic and spirometric data of all subjects is shown in Table 2. Males and females were equally represented, with no differences in age and body mass index (BMI). However, FEV1, FVC, and FEV1/FVC ratios were significantly different. Prevalence of AO increased from 5.4% (30/554) by using the fixed threshold criterion to 11.0% (61/554) by using the LLN criterion. Prevalence rates of definite AO and misidentified AO subjects were 5.4% (30/554) and 5.6% (31/554), respectively, and all misidentified AO subjects belonged to the underestimated subgroup (Table 3). Underestimated subjects were further explored and determined to be non-ills 12.9% (4/31), clinical AO disease 22.6% (7/31), and undetermined subjects 64.5% (20/31) (Table 4). Based on smoking history in undetermined subjects, 15 out of 20 were non-smokers or smoking <5 pack-years and five subjects were chronic smokers. Among the 15 non-smokers, 13 had chronic respiratory symptoms and two had systemic co-morbidities (hypertension and other diseases). Among the five chronic smokers, four had chronic respiratory symptoms and one had no respiratory symptoms other than diabetes mellitus and hypertension as co-morbidities. Investigating the clinical diagnoses of clinical AO disease subjects revealed three cases with COPD (two cases related to cigarette smoking, one case related to post-pulmonary TB) and four cases with chronic asthma (Table 5). Most subjects in the undetermined group had chronic respiratory symptoms 85.0% (17/20) and 60.0% (12/20) had a diagnosis of chronic rhinitis.
  | Figure 1 Age distribution of entire study population based on sex. |
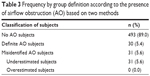  | Table 3 Frequency by group definition according to the presence of airflow obstruction (AO) based on two methods |
  | Table 4 Classification of underestimated subjects (n=31) |
Discussion
Overestimated subjects could have been in the early phase of the disease with the possibility of arresting further disease progression through intervention such as smoking cessation and underestimated subjects may have been those with late detection that missed the chance to receive appropriate intervention to improve their quality of life and reduce consumption of health care resources. All of the misidentified AO subjects in our current study were proved to be underestimated AO, because most of them were in the young age group, which supported results from earlier studies that showed how overestimated AO is frequently found in advanced age groups.12,17
Most of underestimated subjects in our current study had clinical AO disease and chronic respiratory symptoms, which need to be further discussed. Three subjects with clinical AO disease were diagnosed as COPD based on diffuse pulmonary hyperinflation with flattened diaphragms on chest radiographs compatible with COPD. Two of those three had a smoking history of more than 5 pack-years compatible with smoking-related COPD. The other had a history of pulmonary TB with post-TB bronchiectasis revealed by chest radiography and without significant smoking history compatible with post-TB-related COPD. If COPD were to be diagnosed by a fixed threshold criterion alone, a chest radiograph revealing diffuse pulmonary hyperinflation with a flattened diaphragm would turn out to be a false positive, a result which would be quite unlikely. In clinical practice, diagnosis of COPD should be based on multimodalities of evidence and not only on a single tool to achieve the highest probability. The other four subjects with clinical AO disease were diagnosed as asthma based on our clinical criteria, which was concordant with previous physicians’ diagnoses in three of them. All had concomitant chronic allergic rhinitis positive to at least one aeroallergen on skin prick tests. These asthma subjects were underestimated AO by the fixed threshold criterion but not LLN criterion. Undetermined subjects were the largest group of underestimated subjects and had clinically significant findings. Most of undetermined subjects had chronic respiratory symptoms, mostly shown to be chronic rhinitis, which is a well-known precedent for asthma.22
This study revealed that underestimated subjects had relevant AO diseases including smoking-related COPD, post-TB bronchiectasis, and asthma. The two latter diseases could potentially be significant confounding AO diseases other than smoking-related COPD in large epidemiological studies such as the current one. Moreover, we found that approximately two-thirds of underestimated subjects had chronic respiratory symptoms and that most of them were due to chronic rhinitis. If untreated, chronic rhinitis may have a considerable financial effect and impact quality of life.23,24 Furthermore, it is one of the most important risk factors in asthma development.25
There are two major advantages to the current study. Firstly, post bronchodilator spirometry was conducted in all study patients, both symptomatic and asymptomatic, and independently interpreted by two criteria. Secondly, our study had sufficient relevant clinical data to make a diagnosis and to determine the clinical significance of misidentified AO. However, our study was limited as it was based on data from municipal areas only, and it therefore may not be reliably extrapolated to the entire Chiang Mai province. In addition, spirometry was performed as a post-bronchodilator test, and was therefore unable to be used to evaluate reversibility in each tested subject.
Conclusion
Most underestimated subjects in this epidemiological study had conditions of clinical significance, including clinical AO disease and chronic respiratory symptoms, mostly associated with rhinitis. Therefore, subjects meeting the LLN but not fixed threshold criteria should not be considered as false positive AO. The LLN criterion may be considered as a useful supplementary tool for detection of possible AO in prevalence studies for a population cohort. In addition, each underestimated subject should be clinically evaluated and should undergo further investigation by physicians.
Acknowledgments
The authors wish to thank the patients who kindly took part in this study and to acknowledge staff members from the Division of Pulmonary, Critical Care and Allergy, Department of Internal Medicine, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand for their contributions to this study.
Author contributions
CP developed study design and carried out acquisition and interpretation of data, statistical analysis, manuscript preparation, and critical revision of intellectual contents. The remaining authors contributed to acquisition and interpretation of data, revision of the article for important intellectual content, and final approval of the version to be published.
Disclosure
The authors report no conflicts of interest in this work.
References
Shirtcliffe P, Weatherall M, Marsh S, et al. COPD prevalence in a random population survey: a matter of definition. Eur Respir J. 2007;30:232–239. | ||
Halbert RJ, Natoli JL, Gano A, Badamgarav E, Buist AS, Mannino DM. Global burden of COPD: systematic review and meta-analysis. Eur Respir J. 2006;28:523–532. | ||
Halbert RJ, Isonaka S, George D, Iqbal A. Interpreting COPD prevalence estimates: what is the true burden of disease? Chest. 2003;123:1684–1692. | ||
Roche N, Dalmay J, Perez T, et al. FEV1/FVC and FEV1 for the assessment of chronic airflow obstruction in prevalence studies: do prediction equations need revision? Respir Med. 2008;102:1568–1574. | ||
Global initiative for chronic obstructive lung disease: global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease [webpage on the Internet]. Bethesda, MD: National Heart, Lung, and Blood Institute, National Institutes of Health; 2014 [updated 2014]. Available from: http://www.goldcopd.org. Accessed June 25, 2014. | ||
Celli BR, MacNee W; ATS/ERS Task Force. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23:932–946. | ||
Hankinson JL, Odencratz JR, Fedan KB. Spirometric reference values from a sample of the general US population. Am J Respir Crit Care Med. 1999;159:179–187. | ||
Hardie JA, Buist AS, Vollmer WM, Ellingsen I, Bakke PS, Mørkve O. Risk of over-diagnosis of COPD in a symptomatic elderly never-smokers. Eur Respir J. 2002;20:1117–1122. | ||
Aggarwal A, Gupta D, Agarwal R, Jindal S. Comparison of lower confidence limit to the fixed-percentage method for assessing airway obstruction in routine clinical practice. Respir Care. 2011;56:1778–1784. | ||
Global initiative for chronic obstructive lung disease: global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease [webpage on the Internet]. Bethesda, MD: National Heart, Lung, and Blood Institute, National Institutes of Health; 2006 [updated 2006]. Available from: http://www.goldcopd.org. Accessed June 25, 2014. | ||
Mannino DM, Sonia Buist A, Vollmer WM. Chronic obstructive pulmonary disease in the older adult: what defines abnormal lung function? Thorax. 2007;62:237–241. | ||
Cerveri I, Corsico AG, Accordini S, et al. Underestimation of airflow obstruction among young adults using FEV1/FVC <70% as a fixed cut-off: a longitudinal evaluation of clinical and functional outcomes. Thorax. 2008;63:1040–1045. | ||
Robert SD, Farber MO, Knox KS, et al. FEV1/FVC ratio of 70% misclassifies patients with obstruction at the extremes of age. Chest. 2006;130:200–206. | ||
Aggarwal AN, Gupta D, Behera D, Jindal SK. Comparison of fixed percentage method and lower confidence limits for defining limits of normality for interpretation of spirometry. Respir Care. 2006;51:737–743. | ||
Celli BR, Halbert RJ, Isonaka S, Schau B. Population impact of different definitions of airway obstruction. Eur Respir J. 2003;22:268–273. | ||
Swanney MP, Ruppel G, Enright PL, et al. Using the lower limit of normal for the FEV1/FVC ratio reduces the misclassification of airway obstruction. Thorax. 2008;63:1046–1051. | ||
Cochran W. Sampling Techniques. 3rd ed. New York: John Wiley and Sons Inc; 1977. | ||
Burney PGJ, Luczynska C, Chinn S, Jarvis D. The European Community respiratory health survey. Eur Respir J. 1994;7:954–960. | ||
Asher MI, Keil U, Anderson HR, et al. International study of asthma and allergies in childhood (ISAAC): rationale and methods. Eur Respir J. 1995;8:483–491. | ||
Dejsomritrutai W, Nana A, Maranetra KN, et al. Reference spirometric values for healthy lifetime nonsmokers in Thailand. J Med Assoc Thai. 2000;83:457–466. | ||
Dejsomritrutai W, Wongsurakiat P, Chierakul N, Charoenratanakul S, Nana A, Maranetra KN. Comparison between specified percentage and fifth percentile criteria for spirometry interpretation in Thai patients. Respirology. 2002;7:123–127. | ||
Guerra S, Sherrill DL, Martinez FD, Barbee RA. Rhinitis as an independent risk factor for adult-onset asthma. J Allergy Clin Immunol. 2002;109:419–425. | ||
Fineman SM. The burden of allergic rhinitis: beyond dollars and cents. Ann Allergy Asthma Immunol. 2002;88(4 Suppl 1):S2–S7. | ||
Schoenwetter WF, Dupclay L Jr, Appajosyula S, Botteman MF, Pashos CL. Economic impact and quality of life burden of allergic rhinitis. Curr Med Res Opin. 2004;20:305–317. | ||
Shaaban R, Zureik M, Soussan D, et al. Rhinitis and onset of asthma: a longitudinal population-based study. Lancet. 2008;372:1049-1057. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



