Back to Journals » Orthopedic Research and Reviews » Volume 14
Minimally Invasive Inferior Intra-Articular Sacroiliac Joint Fusion: Successful Application of Osseous Stabilization Using Allograft Bone
Authors Lynch PJ, Tubic G, Foster JM, Puri S, Burnette CA, Block JE
Received 22 August 2022
Accepted for publication 8 November 2022
Published 16 November 2022 Volume 2022:14 Pages 429—435
DOI https://doi.org/10.2147/ORR.S387104
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Clark Hung
Paul J Lynch,1 Goran Tubic,2 Jeffrey M Foster,3 Shawn Puri,4 Candice A Burnette,5 Jon E Block6
1Arizona Pain, Scottsdale, AZ, USA; 2Chicagoland Pain Management, Bolingbrook, IL, USA; 3Saint Luke’s Hospital Pain Management Clinic, Kansas City, MO, USA; 4Relievus Pain Management, Havertown, PA, USA; 5Modern Pain Management, Sugar Land, TX, USA; 6Private Practice, San Francisco, CA, USA
Correspondence: Jon E Block, Email [email protected]
Abstract: Minimally invasive sacroiliac joint (SIJ) fusion is the preferred surgical method for managing patients with recalcitrant, chronically severe SIJ pain and dysfunction refractory to conservative medical measures. The primary surgical objective of all minimally invasive SIJ fusion procedures is to provide immediate stabilization within the joint space to support osseous consolidation and the development of a mechanically solid arthrodesis. The intra-articular surgical approach to the SIJ with allograft bone placement utilizes a trajectory and easily identifiable landmarks that allow the surgeon to control the risk of violating important neuro-vascular structures. The intra-articular approach can employ a superior or inferior operative trajectory, with the former restricted to allograft placement in the ligamentous portion of the SIJ. The inferior approach utilizes decortication to surgically create a channel originating in the purely articular portion of the joint space allowing for truly intra-articular implant placement within the osseous confines of the ilium and sacrum. Positioning the implant along the natural joint line and securing it within the underlying sub-chondral bone, mortise and tenon fashion provides stabilization and large surface area contact at the bone implant interface. The inferior, intra-articular approach also places the implant perpendicular to the S1 endplate, near the sacral axis of rotation, which addresses the most significant biomechanical forces across the joint. Short-term, post-surgical observational data from a 57 patient multi-center registry using the inferior, intra-articular approach show uniform and statistically significant improvement in all clinical outcomes (p < 0.001 for all comparisons), including an average 3-point improvement in back pain severity from 6.8 preoperatively to 3.8 at 6 months. Further clinical evaluation with longer-term follow-up of the inferior, intra-articular SIJ fusion procedure is encouraged.
Keywords: sacroiliac, fusion, intra-articular, minimally invasive, allograft
Introduction
Orthograde posture and bipedal locomotion, uniquely human anatomical and functional characteristics, place unusually high axial compressive loads on the weight-bearing joints of the human body, resulting in arthritic deterioration with aging.1 In fact, our widely curving, “S-shaped”, flexible spinal column markedly amplifies the adverse biomechanical effects in the lumbosacral spine, resulting in chronic pain and dysfunction.2,3 The junction of the sacrum and pelvis, the sacroiliac joint (SIJ), is particularly susceptible to deleterious compressive loading during normal ambulation that leads to osseo-ligamentous degeneration.4
Once clinically unappreciated, extensive empirical research has established that the SIJ serves as a potent pain generator that can act as both a primary and a contributing source of chronically severe low back pain.5–11 While differential diagnosis of this condition can be challenging, SIJ pain and dysfunction are frequently encountered sequelae among patients with new onset or reemergent low back pain subsequent to lumbar spine fusion surgery.12–14 The degree of impairment and the diminution in quality of life in SIJ patients that require surgical intervention are worse than in many chronic health conditions, and similar in symptom severity to other orthopedic conditions requiring surgery.5
Minimally invasive SIJ arthrodesis is the preferred surgical intervention in patients with unremitting symptoms refractory to conservative measures.15,16 This paper elucidates the biomechanical and clinical correlations associated with SIJ dysfunction and discusses the evolution of minimally invasive surgical procedures to address this condition. Lastly, we highlight the current surgical paradigm which adopts an inferior, intra-articular approach to the implant placement. This inferior corridor provides the most direct access to the articular region of the SIJ for placement of allogeneic bone graft which works in conjunction with the natural joint architecture to stabilize the SIJ to facilitate a mechanically solid arthrodesis.
Biomechanical and Clinical Correlates
The diarthrodial articulations of the sacrum and ilium represent an extensive anatomical complex consisting of an anterior articular portion coupled with posterior osseo-ligamentous structures (Figure 1).8 As such, the SIJ is the largest axial joint in the body, and serves as the primary junction for the transfer of loads from the lumbar spine to the lower extremities.17,18 The SIJ has six degrees of freedom, but motion in any axis is highly constrained, amounting to ≤3°.19
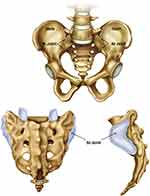 |
Figure 1 Anatomical rendering of the sacroiliac joint shown in anterior (top), posterior (bottom left) and lateral (bottom right) views. |
As noted previously, the SIJ complex is part of the kinetic chain that transfers loads from the axial to the lower appendicular skeleton and, as such, is subject to osteoarthritic degeneration and associated dysfunction with aging.4 Repetitive microtrauma, as with arthritis, and acute trauma are strongly associated with chronically severe SIJ dysfunction requiring fusion surgery.20
It is also well recognized that the likelihood of developing SIJ dysfunction is markedly increased as a result of adjacent segment disease following lumbar spine fusion surgery.12–14 In fact, as many as 40% of patients undergoing instrumented lumbar fusion report SIJ pain within 12 months of surgery,21 and this proportion may be higher among patients undergoing multi-level fusion procedures.22 To underscore this association, it has recently been reported that spontaneous SIJ ankylosis, which represents the highest level of SIJ degeneration, has different phenotypes in patients after fusion procedures versus non-surgical patients.23 Specifically, it was noted that among patients with spontaneous SIJ ankyloses on CT imaging, the anterior-type ankylosis was present in 92% of patients who had undergone lumbar spine fusion surgery, versus only in 48% of control patients, who did not have any spine surgery.
The magnitude of biomechanical loads and strains across the joint complex can be quite variable and strongly associated with gender.19,24 Indeed, the SIJ complex represents one of the most pronounced areas of anatomical sexual dimorphism among humans. To facilitate childbirth, the female sacrum is wider and more backward tilted compared to the long and narrow pelvis in males.8 These anatomical distinctions in joint form have been found to be associated with an increased risk of SIJ pain and dysfunction in females.25 Ziegeler et al26 reported that, in a cohort of over 800 patients without documented SIJ disease, atypical joint forms were over four times more likely to occur among females, with an almost five times greater risk of radiographic evidence of dorsal osteophytes formation compared to males.
Although SIJ pain and dysfunction are characteristically linked to osteoarthritic degeneration, postpartum pelvic girdle pain has recently been appreciated as an antecedent to chronic SIJ problems.27 It has been estimated that almost 10% of women continue to have chronically severe pelvic pain of SIJ origin two years postpartum.27 A number of studies suggest that minimally invasive SIJ fusion is effective in attenuating the impact of pelvic pain on function and quality of life in these patients.27,28 Ongoing research in this key area is being undertaken to optimize clinical outcomes using a patient-tailored approach in selecting the appropriate surgical option for this important sub-population.
Evolution and Current Surgical Treatment Paradigm
Due to significant iatrogenic injury, residual pain secondary to autograft harvesting and a lengthy period of post-operative hospitalization and rehabilitation, open surgical arthrodesis of the SIJ has been considered an intervention of “last resort” and uncommonly undertaken.29 Minimally invasive SIJ fusion was developed, in part, to obviate the iatrogenic injury associated with the open surgical approach and, thus, improve patient outcomes.30,31 However, in larger part, the advent, validation, rapid clinical adoption and commercialization of minimally invasive SIJ fusion occurred at the same time as the burgeoning awareness of the contributory effects of SIJ dysfunction on chronic low back pain, impaired physical functioning and reduced quality of life.10,11,32–34 The clinical benefit associated with minimally invasive SIJ fusion has been the subject of extensive investigation including two, open-label, randomized clinical trials that reported significantly better clinical outcomes after two years of follow-up compared to conservative care.35,36 An ongoing randomized, sham-controlled trial of SIJ fusion will provide a definitive estimate of the effect size associated with this procedure.37
The primary surgical objective of the minimally invasive SIJ fusion procedure is to provide immediate stabilization across the joint space to support osseous consolidation and the development of a mechanically solid arthrodesis.38 Surgical stabilization of the SIJ can be accomplished using an array of surgical approaches; however, it remains unclear as to whether true fixation has added benefit over stabilization across the joint, which is accomplished by intra-articular placement of allograft implants.15,31,39 While the overall surgical goal of all approaches is identical (solid arthrodesis), the intra-articular approach allows surgeons to utilize an operative corridor that permits extensive and direct decortication, and it provides fixation in all planes, as opposed to some approaches which fixate the joint mostly in flexion-extension.40
Inferior, Intra-Articular Arthrodesis Procedure
The SIJ can be approached intra-articularly from an operative trajectory at or above the posterior superior iliac spine (PSIS) (ie, superior) or under the PSIS (ie, inferior). While lateral SIJ fusion utilizes metallic instrumentation to achieve fixation, the intra-articular approach typically utilizes a bone allograft implant to provide osseous stabilization. The allograft implant occupies greater than three times the intra-articular spatial volume than the three metallic implants used in the lateral transfixing procedure, providing bone implant contact over a large surface area of the joint space (Figure 2).
Using a superior, intra-articular operative trajectory has the fundamental limitation of requiring allograft implantation in the ligamentous portion of the SIJ, essentially parallel to the S1 endplate which is orthogonal to the natural architectural of the joint. In contrast, the inferior, intra-articular surgical approach, referred to as the Omnia approach, avoids having to contend with the PSIS in the operative corridor, and places the allograft bone implant inferior and ventral to the PSIS within the purely articular portion of the joint, nearly perpendicular to the S1 endplate. Decortication and preparation of the bony bed with a drill and broach to create a defined “channel” within the underlying sub-chondral bone allows for the structural allograft to be implanted truly intra-articularly in a sturdy mortise and tenon fashion along the joint line. This has the theoretical advantage of providing joint stabilization. Additionally, placement of the implant under the PSIS and adjacent to the sacral axis of rotation may induce stabilization, and may minimize the biomechanical forces on the implant, particularly those due to sacral rotation and flexion-extension (Figure 3). Figure 4 illustrates radiographically the correct anatomical placement of the allograft bone implant within a surgically created channel in the articular portion of the SIJ.
 |
Figure 3 Schematic showing relevant SIJ functional motions and corresponding directions of biomechanical forces about the sacral axis of rotation. |
 |
Figure 4 Lateral, anteroposterior and oblique (left to right) radiographic views of proper implant placement within the sacroiliac joint. |
Preliminary Clinical Evidence from a Patient Registry
A post-market patient registry was established at 16 geographically dispersed clinical sites in the US with the primary objective to evaluate the real-world clinical utility of intra-articular arthrodesis with the PsiF™ Sacroiliac Joint Fusion System (Omnia Medical, Morgantown, WV, USA). A standardized set of peri-operative parameters as well as safety and clinical outcomes were collected across all sites. Briefly, adult patients were eligible to participate in this registry if they underwent the PsiF™ fusion procedure as a result of chronic pain of SIJ origin that had been confirmed by positive response to two diagnostic blocks with greater than 75% reported improvement in pain. Patients were evaluated pre-operatively and clinical follow-up occurred at 1, 3, 6 and 12 months, post-procedure and included assessments of adverse events, back pain severity by visual analog scale, and pain-tolerant standing time and walking distance.
Observational data were collected in 57 patients (mean age: 63 ± 15 years) with early follow-up at 6 months from this multi-center registry of patients undergoing intra-articular SIJ fusion with decortication and allograft bone implantation. All clinical outcomes showed improvement over pre-surgical values (mean ± SD) for back pain severity by 44% (6.8 ± 2 to 3.8 ± 3), pain-tolerant standing time by 183% (29 ± 53 mins. to 82 ± 36 mins.), and pain-tolerant walking distance by 55% (87 ± 267 steps to 135 ± 374 steps). All improvements were statistically significant (p < 0.001 for all comparisons). There were no serious adverse events reported in this registry population.
Interpretation and Conclusions
While all minimally invasive SIJ fusion procedures share the same surgical goal of achieving a mechanically solid ilio-sacral arthrodesis, there has been increasing recognition that use of an intra-articular approach offers an improved surgical option compared to SIJ fusion employing other approaches. As recently published in the AMA CPT® Editorial Summary of Panel Actions, September 2022, the CPT Editorial Panel approved a new Category I code for the intra-articular procedure and accepted the addition of code 2×000 to report percutaneous arthrodesis of the SIJ using placement of intra-articular implant(s) without placement of a transfixation; and deletion of Category III code 0775T. The new code will go into effect in January 2024. Additional real-world clinical evidence supporting the effectiveness of intra-articular SIJ fusion should be encouraged in order to fully characterize the potential advantages over other approaches.
Although the SIJ fusion procedure can be performed using several operative trajectories, the inferior, intra-articular trajectory has the advantage of avoiding the PSIS. It offers direct access to the articular portion of the joint for decortication and allograft bone placement within a surgically created channel in the sub-chondral bone, offering maximal stabilization and surface area contact at the bone implant interface. Approaching the joint from the inferior trajectory also places the implant perpendicular to the S1 endplate near a natural “pivot point” at the sacral axis of rotation, which addresses the most significant motion of the joint.
Short-term, post-surgical pragmatic data from a patient registry using the inferior, intra-articular approach show uniform and significant improvement in all clinical outcomes, including an average 3-point reduction in back pain severity. However, the average amount of amelioration in back pain in these patients represents short-term (6 month) follow-up and may not accurately reflect the degree of clinical improvement realized longer-term (12–24 months) after solid arthrodesis has been achieved. Additionally, the magnitude of pain reduction among patients treated in a real-world setting may be different than results achieved in open-label trials of SI joint fusion. Further clinical evaluation with longer-term follow-up of the inferior, intra-articular SIJ fusion procedure is recommended.
Data Sharing Statement
Requests for data sharing can be made by contacting the corresponding author. Individual participant data that underlie the results reported in this article will be made available (after deidentification) from 9 to 36 months after article publication. Data sharing will be limited to investigators whose proposed use of the data has been approved by an independent review committee identified for this purpose.
Acknowledgments
Financial support for this work was provided by Omnia Medical (Morgantown, WV, USA).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
JMF reports personal fees from Omnia Medical, during the conduct of the study; personal fees from Nevro Corp and Nalu Med, outside the submitted work. SP reports personal fees from Omnia Medical and Vertos Medical, outside the submitted work. CAB reports personal fees from Omnia Medical, outside the submitted work. JB is an independent advisor to Omnia Medical and was remunerated for assistance in manuscript development. The authors report no other conflicts of interest in this work.
References
1. Pennisi E. Evolutionary biology. The burdens of being a biped. Science. 2012;336(6084):974. doi:10.1126/science.336.6084.974
2. Latimer B. The perils of being bipedal. Ann Biomed Eng. 2005;33(1):3–6. doi:10.1007/s10439-005-8957-8
3. Filler AG. Emergence and optimization of upright posture among hominiform hominoids and the evolutionary pathophysiology of back pain. Neurosurg Focus. 2007;23(1):E4. doi:10.3171/FOC-07/07/E4
4. Toyohara R, Kurosawa D, Hammer N, et al. Finite element analysis of load transition on sacroiliac joint during bipedal walking. Sci Rep. 2020;10(1):13683. doi:10.1038/s41598-020-70676-w
5. Cher D, Polly D, Berven S. Sacroiliac joint pain: burden of disease. Med Devices. 2014;7:73–81. doi:10.2147/MDER.S59437
6. Le Huec JC, Bourret S, Thompson W, Daulouede C, Cloche T. A painful unknown: sacroiliac joint diagnosis and treatment. EFORT Open Rev. 2020;5(10):691–698. doi:10.1302/2058-5241.5.190081
7. Ou-Yang DC, York PJ, Kleck CJ, Patel VV. Diagnosis and Management of Sacroiliac Joint Dysfunction. J Bone Joint Surg Am. 2017;99(23):2027–2036. doi:10.2106/JBJS.17.00245
8. Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537–567. doi:10.1111/j.1469-7580.2012.01564.x
9. Schwarzer AC, Aprill CN, Bogduk N. The sacroiliac joint in chronic low back pain. Spine. 1995;20(1):31–37. doi:10.1097/00007632-199501000-00007
10. Weksler N, Velan GJ, Semionov M, et al. The role of sacroiliac joint dysfunction in the genesis of low back pain: the obvious is not always right. Arch Orthop Trauma Surg. 2007;127(10):885–888. doi:10.1007/s00402-007-0420-x
11. Sembrano JN, Polly DW. How often is low back pain not coming from the back? Spine. 2009;34(1):E27–32. doi:10.1097/BRS.0b013e31818b8882
12. DePalma MJ, Ketchum JM, Saullo TR. Etiology of chronic low back pain in patients having undergone lumbar fusion. Pain Med. 2011;12(5):732–739. doi:10.1111/j.1526-4637.2011.01098.x
13. Liliang PC, Lu K, Liang CL, Tsai YD, Wang KW, Chen HJ. Sacroiliac joint pain after lumbar and lumbosacral fusion: findings using dual sacroiliac joint blocks. Pain Med. 2011;12(4):565–570. doi:10.1111/j.1526-4637.2011.01087.x
14. Maigne JY, Planchon CA. Sacroiliac joint pain after lumbar fusion. A study with anesthetic blocks. Eur Spine J. 2005;14(7):654–658. doi:10.1007/s00586-004-0692-6
15. Kaye AD, Edinoff AN, Scoon L, et al. Novel Interventional Techniques for Chronic Pain with Minimally Invasive Arthrodesis of the Sacroiliac Joint: (INSITE, iFuse, Tricor, Rialto, and others). Rheumatol Ther. 2021;8(3):1061–1072. doi:10.1007/s40744-021-00350-8
16. Martin CT, Haase L, Lender PA, Polly DW. Minimally Invasive Sacroiliac Joint Fusion: the Current Evidence. Int J Spine Surg. 2020;14(Suppl 1):20–29. doi:10.14444/6072
17. Cohen SP. Sacroiliac joint pain: a comprehensive review of anatomy, diagnosis, and treatment. Anesth Analg. 2005;101(5):1440–1453. doi:10.1213/01.ANE.0000180831.60169.EA
18. Dietrichs E. Anatomy of the pelvic joints--A review. Scand J Rheumatol Suppl. 1991;88:4–6.
19. Kiapour A, Joukar A, Elgafy H, Erbulut DU, Agarwal AK, Goel VK. Biomechanics of the Sacroiliac Joint: anatomy, Function, Biomechanics, Sexual Dimorphism, and Causes of Pain. Int J Spine Surg. 2020;14(Suppl 1):3–13. doi:10.14444/6077
20. Dydyk AM, Forro SD, Hanna A. Sacroiliac Joint Injury. Treasure Island (FL): StatPearls; 2022.
21. Ha KY, Lee JS, Kim KW. Degeneration of sacroiliac joint after instrumented lumbar or lumbosacral fusion: a prospective cohort study over five-year follow-up. Spine. 2008;33(11):1192–1198. doi:10.1097/BRS.0b013e318170fd35
22. Colo G, Cavagnaro L, Alessio-Mazzola M, Zanirato A, Felli L, Formica M. Incidence, diagnosis and management of sacroiliitis after spinal surgery: a systematic review of the literature. Musculoskelet Surg. 2020;104(2):111–123. doi:10.1007/s12306-019-00607-0
23. Gahleitner A, Pamnani S, Huschbeck A, Petersein J, Dengler J, Lenga P. Spontaneous ankylosis of the sacroiliac joint: prevalence and risk factors. Eur J Orthop Surg Traumatol. 2022. doi:10.1007/s00590-022-03359-z
24. Joukar A, Shah A, Kiapour A, et al. Sex Specific Sacroiliac Joint Biomechanics During Standing Upright: a Finite Element Study. Spine. 2018;43(18):E1053–E1060. doi:10.1097/BRS.0000000000002623
25. Ziegeler K, Hermann KGA, Diekhoff T. Anatomical Joint Form Variation in Sacroiliac Joint Disease: current Concepts and New Perspectives. Curr Rheumatol Rep. 2021;23(8):60. doi:10.1007/s11926-021-01033-7
26. Ziegeler K, Kreutzinger V, Diekhoff T, et al. Impact of age, sex, and joint form on degenerative lesions of the sacroiliac joints on CT in the normal population. Sci Rep. 2021;11(1):5903. doi:10.1038/s41598-021-85303-5
27. Fiani B, Sekhon M, Doan T, et al. Sacroiliac Joint and Pelvic Dysfunction Due to Symphysiolysis in Postpartum Women. Cureus. 2021;13(10):e18619. doi:10.7759/cureus.18619
28. Capobianco R, Cher D, Group SS. Safety and effectiveness of minimally invasive sacroiliac joint fusion in women with persistent post-partum posterior pelvic girdle pain: 12-month outcomes from a prospective, multi-center trial. Springerplus. 2015;4:570. doi:10.1186/s40064-015-1359-y
29. Buchowski JM, Kebaish KM, Sinkov V, Cohen DB, Sieber AN, Kostuik JP. Functional and radiographic outcome of sacroiliac arthrodesis for the disorders of the sacroiliac joint. Spine J. 2005;5(5):520–528. doi:10.1016/j.spinee.2005.02.022
30. Al-Khayer A, Hegarty J, Hahn D, Grevitt MP. Percutaneous sacroiliac joint arthrodesis: a novel technique. J Spinal Disord Tech. 2008;21(5):359–363. doi:10.1097/BSD.0b013e318145ab96
31. Wise CL, Dall BE. Minimally invasive sacroiliac arthrodesis: outcomes of a new technique. J Spinal Disord Tech. 2008;21(8):579–584. doi:10.1097/BSD.0b013e31815ecc4b
32. Rudolf L. Sacroiliac Joint Arthrodesis-MIS Technique with Titanium Implants: report of the First 50 Patients and Outcomes. Open Orthop J. 2012;6:495–502. doi:10.2174/1874325001206010495
33. Sachs D, Capobianco R. One year successful outcomes for novel sacroiliac joint arthrodesis system. Ann Surg Innov Res. 2012;6(1):13. doi:10.1186/1750-1164-6-13
34. Kreiner DS, Matz P, Bono CM, et al. Guideline summary review: an evidence-based clinical guideline for the diagnosis and treatment of low back pain. Spine J. 2020;20(7):998–1024. doi:10.1016/j.spinee.2020.04.006
35. Dengler J, Kools D, Pflugmacher R, et al. Randomized Trial of Sacroiliac Joint Arthrodesis Compared with Conservative Management for Chronic Low Back Pain Attributed to the Sacroiliac Joint. J Bone Joint Surg Am. 2019;101(5):400–411. doi:10.2106/JBJS.18.00022
36. Polly DW, Swofford J, Whang PG, et al. Two-Year Outcomes from a Randomized Controlled Trial of Minimally Invasive Sacroiliac Joint Fusion vs. Non-Surgical Management for Sacroiliac Joint Dysfunction. Int J Spine Surg. 2016;10:28. doi:10.14444/3028
37. Randers EM, Gerdhem P, Dahl J, Stuge B, Kibsgard TJ. The effect of minimally invasive sacroiliac joint fusion compared with sham operation: study protocol of a prospective double-blinded multicenter randomized controlled trial. Acta Orthop. 2022;93:75–81. doi:10.1080/17453674.2021.1994185
38. Lee DW, Patterson DG, Sayed D. Review of Current Evidence for Minimally Invasive Posterior Sacroiliac Joint Fusion. Int J Spine Surg. 2021;15(3):514–524. doi:10.14444/8073
39. Belanger TA, Dall BE. Sacroiliac arthrodesis using a posterior midline fascial splitting approach and pedicle screw instrumentation: a new technique. J Spinal Disord. 2001;14(2):118–124. doi:10.1097/00002517-200104000-00005
40. Lindsey DP, Parrish R, Gundanna M, Leasure J, Yerby SA, Kondrashov D. Biomechanics of unilateral and bilateral sacroiliac joint stabilization: laboratory investigation. J Neurosurg Spine. 2018;28(3):326–332. doi:10.3171/2017.7.SPINE17499
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

