Back to Journals » Neuropsychiatric Disease and Treatment » Volume 15
Mindfulness-Based Intervention For Nurses In AIDS Care In China: A Pilot Study
Authors Pan C , Wang H , Chen M , Cai Y , Xiao C , Tang Q , Koniak-Griffin D
Received 12 July 2019
Accepted for publication 17 October 2019
Published 8 November 2019 Volume 2019:15 Pages 3131—3141
DOI https://doi.org/10.2147/NDT.S223036
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yuping Ning
Chen Pan,1 Honghong Wang,2 Minzhen Chen,3 Yu Cai,1 Changgen Xiao,4 Qiuping Tang,1 Deborah Koniak-Griffin5
1Department of Clinical Psychology, The Third Xiangya Hospital of Central South University, Changsha, Hunan 410013, People’s Republic of China; 2Department of Fundamental Nursing, Xiangya School of Nursing, Central South University, Changsha, Hunan 410013, People’s Republic of China; 3AIDS Department of the First Hospital of Changsha, Hunan 410005, People’s Republic of China; 4Department of Applied Psychology, School of Humanities and Management, Hunan University of Chinese Medicine, Changsha, Hunan 410208, People’s Republic of China; 5School of Nursing of University of California Los Angeles, Los Angeles, CA 90095-1702, USA
Correspondence: Qiuping Tang
Department of Clinical Psychology, The Third Xiangya Hospital of Central South University, Changsha, Hunan 410013, People’s Republic of China
Tel +86 13787256418
Fax +86 731 88618487
Email [email protected]
Background/purpose: Workplace stress among nurses providing care for people living with human immunodeficiency virus is a serious problem in China that may increase rates of job burnout and affect quality of care. Mindfulness-based intervention has been shown to be effective in relieving stress and burnout in nurses. Therefore, we designed a mixed-method pilot study to evaluate a mindfulness-based intervention for nurses providing care for people living with human immunodeficiency virus.
Methods: Twenty nurses caring for people living with human immunodeficiency virus in the First Hospital of Changsha, China participated in a mindfulness-based intervention for 2 hr sessions weekly for 6 weeks. The Perceived Stress Scale, Maslach Burnout Inventory, Five Facets Mindfulness Questionnaire, State-Trait Anxiety Inventory, and the Beck Depression Inventory were used to collect data before and after the mindfulness-based intervention. Participants were invited to attend an in-depth interview 1 week after the end of the mindfulness-based intervention to give feedback.
Results: The quantitative analyses revealed a significant change in Five Facets Mindfulness Questionnaire scores. There were no significant differences between pre- and post-intervention measures of any other variables. Qualitative results showed nurses experienced a decrease in work and daily life pressures; improvements in communications with patients, colleagues and families, with better regulation of negative emotions, and acceptance of other people and attention.
Conclusion: This study supports the acceptability and potential benefits of the mindfulness-based intervention in helping nurses caring for people living with human immunodeficiency virus to manage stress and emotions, and improve their acceptance of others and attention. A larger study with a randomized controlled trial design is warranted to confirm the effectiveness of this mindfulness-based intervention.
Keywords: human immunodeficiency virus, stress, emotions, job burnout, mindfulness-based intervention
Introduction
Nursing professionals encounter great stresses in our present healthcare environment.1 Stress may result in increased burnout, defined as continuous work pressure without effective handling, and commonly manifested in three aspects, including depersonalization, emotional exhaustion, and low personal achievement.2 In addition to enduring the common stresses associated with caring for patients with severe illnesses (such as progressive deterioration, discouraging prognosis, and high mortality rates), health professionals caring for people living with human immunodeficiency virus (HIV, PLWH) often confront other unique problems. These problems include fear of contagion, stigma, anxiety in dealing with patients’ emotional disorder, or even over-identification with the patient. Thus, unsurprisingly, they may more easily suffer from stress and burnout.3 Studies show that burnout, with moderate to high levels of morbidity, is a major challenge in the HIV care area.4 In China, the enormous population base and number of patients compared to available nurses have led to the many exhausting and stressful tasks being assumed by nurses that further place them at high risk for burnout.5 One recent study in China reported an overall burnout syndrome prevalence of 76.9% among HIV healthcare professionals.6
Burnout has negative impacts on healthcare professionals, including nurses, as well as their patients and the organization.7 Studies show that individuals affected by burnout often demonstrate emotional issues such as anxiety and depression; psychosomatic problems such as insomnia; attitude problems such as aggression, impassiveness, and mistrust; behavioral problems such as aggression, fussiness, and isolation; and interpersonal difficulties.8 In addition, research has revealed that burnout has a negative effect on the quality of care, patient safety, and productivity of employees.7
Mindfulness helps people bring their thoughts, feelings, and body sensations to existing moment experiences.9 Studies report that mindfulness can effectively and economically help nursing professionals to deal with burnout and stress,10 work with compassion in stressful and demanding environments,11 develop greater self-kindness and care for themselves,12 improve physical, psychosocial, and spiritual well-being,12 and enhance self-actualization and quality of care.13 There is a series of psychological interventions based on mindfulness, known as Mindfulness-Based Interventions (MBIs), including Mindfulness-Based Stress Reduction (MBSR) and Mindful Awareness Practices (MAPs), which aim at relieving stress and mental and physical health concerns.14 MBSR is an eight-session intervention with 2.5 hr weekly meetings that provide intensive training in mindfulness meditation, created by Kabat-Zinn at the University of Massachusetts Medical Center.15 MBSR has been found to decrease stress and burnout in nurses16,17 and may potentially enhance the quality of patient care.16 Similarly, MAPs, a six-session intervention with 2 hr weekly meetings that provides intensive training in mindfulness meditation, has been reported to have many positive outcomes. Findings of studies examining the effects of MAPS, which was developed by the UCLA Mindful Awareness Research Center, show short-term therapeutic effects in the reduction of behavioral symptoms, stress, and pro-inflammatory signals in younger women with breast cancer18 and the promotion of sleep quality in elderly suffering from moderate sleep disturbances.19
In China, few studies have been conducted to evaluate mindfulness-based interventions for nurses. Findings suggest that mindfulness-based intervention can reduce burnout among nurses working in emergency departments,10 regulate negative emotions among nurses working in a senior cadre ward for aged patients,20 improve sleep quality among nurses working in an internal medicine department,21 and effectively predict the achievement motivation of nurses working in rheumatism immunity departments and cardiology departments.22,23 However, studies to explore the effect of mindfulness-based interventions for nurses caring for PLWH are scarce in China.
Mindful Living With Stress (MLWS), the intervention evaluated in this study, integrates components of MBSR, MAPs, and Chinese cultural practices, especially Tai Chi, a primary form of mindfulness-based intervention.24 Therefore, we designed a mixed-method pilot study to evaluate MLWS in nurses caring for PLWH. The findings of this pilot study will increase our understanding about the acceptability and effects of the MLWS Intervention on stress and burnout of nurses caring for PLWH.
Materials And Methods
Study Design
This is a mixed-method study using both quantitative and qualitative methods. The quantitative data were collected at two different time points: pre-intervention and post-intervention. The qualitative data were collected at post-intervention.
Setting And Participants
This study was conducted in the AIDS Department of the First Hospital of Changsha, China from December 15, 2017, to February 15, 2018. The First Hospital of Changsha is a public, first-level tertiary care hospital that has the largest HIV care department in Hunan, with two wards, a clinic and a research center. Forty-three nurses provide care to the PLWH in this facility.
Nurses in the AIDS Department of the First Hospital of Changsha were recruited through flyers posted in the wards of the AIDS Department. Inclusion criteria included: (a) having a license to practice as a nurse in the People’s Republic of China, (b) being employed as a nurse in the AIDS department of the First Hospital of Changsha for at least half a year, (c) Chinese speaking, and (d) being at least 18 years old. Other healthcare professionals (eg, doctors, pharmacists, social workers) and nursing supervisors and managers were excluded. As the participation is voluntary, we recruited 43 nurses and a total of 20 nurses agreed to participate in the study, giving a response rate of 46.5%. A convenience sample of 20 nurses caring for PLWH was recruited. Written informed consent was obtained from these nurses at the time of recruitment.
Procedures
Participants were asked to complete a pre-intervention assessment packet 1 week before the first session of the MLWS intervention; this packet was composed of a background questionnaire and five questionnaires assessing stress, burnout, mindfulness, anxiety, and depression. One week following the last session, participants completed a post-intervention assessment that included all of the previously administered measures except the background questionnaire. Participants also were invited to attend an in-depth interview following completion of the written questionnaires. Using the interview guide as shown in Table 1, a specially trained research assistant (RA) conducted interviews for the purpose of obtaining participants’ feedback and reactions to the MLWS Intervention.
 |
Table 1 Qualitative Interview Guide |
In order to ensure the small group size needed for quality assurance in delivering the intervention, participants were divided into groups of 10 according to the convenience of clinical scheduling. The MLWS intervention was facilitated by the Principal Investigator (PI) with the assistance of the RA. At least four sessions of the MLWS intervention were attended by 80% of the participants. Sixteen participants attended four to six sessions, and two or three sessions were attended by three participants. One participant attended one session and then withdrew from this study because of time constraints related to personal responsibilities.
Confidentiality of the participants’ personal identity and data collected were assured by asking participants not to discuss the information shared during the MLWS intervention with anyone outside of their assigned sessions and not to identify colleagues’ names in in-depth interviews. Participants were informed of their right to refusal of or withdrawal from the study at all times without a negative impact on their work.
Data Collection Procedures
At the pre- and post-intervention assessments, the RA provided individual guidance to participants on how to fill out questionnaires, in a private office of the AIDS Department of the First Hospital of Changsha. Participants completed self-administered questionnaires by themselves. Completion of the questionnaires required approximately 45–60 mins.
Post-intervention in-depth interviews were conducted by the RA in a private conference room and lasted approximately 30 mins. The interview followed a semi-structured interview guide with open-ended probes. Interview topics included feedback on the MLWS intervention and the influence of the intervention on life, work, and living with stress. The interview was audio-recorded with all participants’ signed consent.
MLWS Intervention
Based on a multifactorial consideration of the MBSR and MAP protocol, practicality on the ground of the local nurses and our qualitative findings, the MLWS intervention consisted of six weekly 2 hr small group sessions. The content included: (a) stress and mindfulness; (b) mindful awareness of stress through listening to the body; (c) mindful awareness of stress through listening to the breath; (d) mindful living with challenges; (e) mindful interactions and mindful movement; and (f) review of the mindfulness practices included in the program.
Mindfulness skill-building practices in the MLWS intervention included mindful breathing, mindful body scan, sitting meditation, mindful listening, mindful movement (tai chi and yoga) and daily life meditation. The implementation plan for every session included: (a) initially presenting a short lecture on different components of mindfulness (25 mins), (b) practicing mindfulness meditation (50 mins), (c) sharing experiences and discussing feelings (40 mins), and (d) providing instructions on homework assignments (5 mins). In every new session, mindfulness practice skills learned in previous sessions were reviewed. WeChat, the most popular social media app in China, was established to provide opportunities for participants to have discussions and share videos and audios after every session. Sessions of the MLWS intervention were conducted in a private and quiet room in the evening (7:00 pm–9:00 pm).
Measures
Quantitative Data Collection
Five written questionnaires were administered at baseline and post-intervention.
Stress
Thoughts, feelings, and stressful situations that professionals may have experienced at the workplace or elsewhere during the previous month were evaluated with the Chinese Version of the Perceived Stress Scale (CPSS). The CPSS evaluates both negative and positive feelings. An example of a CPSS item is: “In the last month, how often have you been upset because of something that happened unexpectedly?” CPSS comprises 14 Likert-type items that range from 0 = never to 4 = very often. The higher the total score, the greater the perceived level of stress and score; ≥25 means severe stress. Cronbach’s α for the CPSS is 0.78.25
Burnout
Maslach Burnout Inventory (MBI) has been culturally adapted and validated in Chinese. The Chinese Version of the Maslach Burnout Inventory (CMBI) assessed the major components of burnout with three sub-scales: Emotional Exhaustion (EE), Depersonalization (DP) and Personal Accomplishment (PA). An example of a CMBI item is: “I feel emotionally drained from my work.” The CMBI is comprised of 22 Likert-type items (EE, nine items; DP, five items; PA, eight items), with a response scale ranging from 0 = never to 6 = every day. Scores of EE ≥27 indicate high burnout, scores of DP ≥10 indicate high burnout, and scores of PA ≤33 indicate low burnout. Cronbach’s α for the total CMBI is 0.84. Cronbach’s α for the EE, DP, and PA subscales is 0.85, 0.78, and 0.82, respectively.2
Mindfulness
The Chinese version of the Five Facets Mindfulness Questionnaire (Ch-FFMQ) was used to assess five facets of a general tendency to be mindful in daily life: (a) observing: paying attention to internal and external experiences, including sensation, emotion, cognition, and visual perception; (b) describing: labeling inner experiences with words; (c) acting with awareness: focusing on one’s activities of the present; (d) nonjudging of inner experience: adopting a non-evaluative attitude toward thoughts and feelings; and (e) nonreactivity to inner experience: permitting thoughts and feelings to come and go, without being caught up or denying them. An example of Ch-FFMQ is “I notice the smells and aromas of things.” Ch-FFMQ consists of 39 Likert-type items that range from 1 (never or very rarely true) to 5 (very often or always true). The higher the total score, the more mindful the individual is in daily life. Cronbach’s α for observing, describing, acting with awareness, non-judging, non-reactivity sub-scales is 0.75, 0.84, 0.79, 0.66, 0.45.26,27
Anxiety Symptoms
State and trait anxiety was evaluated with the Chinese version of the State-Trait Anxiety Inventory (C-STAI). The C-STAI includes 20 items that assess trait anxiety and 20 items for state anxiety. An Example of C-STAI is: “I worry too much over something that really doesn’t matter.” All items are rated on a 4-point scale (e.g., from “Almost Never” to “Almost Always”). The higher the total score, the greater the anxiety. Test–retest reliabilities for the Chinese versions of the State Anxiety Inventory (C-SAI) and the Trait Anxiety Inventory (C-TAI) are 0.88 and 0.90, respectively.28
Depression Symptoms
Depression was evaluated by the Chinese version of the Beck Depression Inventory (C-BDI). C-BDI is a 21-item, self-report rating inventory. An example of BDI is: 1 – I do not feel sad; 2 - I feel sad; 3 - I am sad all the time and I cannot snap out of it; 4 - I am so sad and unhappy that I cannot stand it.” A score of ≤4 indicates no depression or very mild depression, 5–13 indicates mild depression, 14–20 indicates moderate depression, ≥21 indicates severe depression. Cronbach’s α for the C-BDI is 0.89.29
Qualitative Data
The audio-recorded interview followed a semi-structured interview guide with open-ended probes, shown in Table 1. The draft of the interview guide was developed by the PI through literature review and consulting research team members. The PI revised the draft according to the suggestions from research team members and developed the final version of the interview guide.
Statistical Methods
Quantitative Study
Statistical analysis was conducted using SPSS22.0. Descriptive analyses were performed on sociodemographic data using percentages and frequencies. Comparison between the pre- and post-intervention scores for stress, burnout, mindfulness, anxiety, and depression were performed by paired-samples t-test (two-sided), with p< 0.05 considered significant.
Qualitative Study
The data were coded and analyzed using a thematic analysis. A first draft of the theme framework was developed based on the in-depth interview guide. The theme framework was modified according to the themes that emerged from the transcripts during analysis. The PI and RA read all transcripts one by one, analyzed the semantics, coded the transcripts and incorporated them into the corresponding themes. Saturation was reached in the qualitative discourse analysis. Data management and analysis were assisted by software (NVIVO 8.0).
Results
Sociodemographic Characteristics
Table 2 presents the participants’ sociodemographic characteristics. The mean age was 27.68 years (range = 21–41). The majority of participants (94.7%) were female. The average length of employment in nursing was 6.84 years (range = 2–23), with an average of 3.45 years of employment caring for PLWH (range = 0.5–10). Only 4 participants (21.1%) had prior mindfulness practice experiences (Yoga).
 |
Table 2 Sociodemographic Characteristics |
Quantitative Results
Nineteen nurses participated in MLWS intervention and completed pre- and post-intervention questionnaires.
Table 3 displays the comparisons of the pre- and post-intervention results. The intervention was associated with change in the observing domain of mindfulness (change: −3.53; 95% confidence interval (−5.74, −1.31); p=0.004) and the domain of acting with awareness of mindfulness (Change: 2.74; 95% confidence interval (0.53, 4.94); p=0.018) of the FFMQ scores. There were no significant differences among other variables.
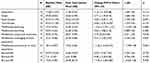 |
Table 3 Pre- And Posttest Comparisons Of Scores On Measures |
Qualitative Results
Acceptance Of And Satisfaction With MLWS Intervention
In general, the acceptability of the MLWS intervention was relatively high. Most participants were satisfied with the intervention design, group style, and atmosphere. They considered the intervention relaxing and appropriate for nurses caring for PLWH, and expressed willingness to recommend it to other nurses. The average satisfaction score was 7.3 (range: 1 lowest to 10 highest).
Effect Of MLWS Intervention On Stress, Communications, Emotional State, Acceptance, And Attention
Many benefits of the MLWS intervention were described by participants. The intervention reportedly decreased stress associated with work and daily life. Participants explained how their communications with patients, colleagues and families. They were better able to manage their emotions, were more accepting of other people, and had improved attention.
I have better communications with patients and colleagues. After calming down, I will pay-attention to my speaking speed, intonation, eyesight and facial expression in communication. [Nurse 4]
I will not be so hot-tempered with my family as I used to be. Now I can listen carefully to my family. [Nurse 2]
When mindfulness is used in life, quarrels with my mom are reduced and relationships with her are improved. [Nurse 7]
Mindfulness is helpful to my emotional stability. [Nurse 16]
I used to handle my negative emotions by avoidance or other means, but now I face and accept them. [Nurse 15]
There is a change in the acceptance of others. It is necessary to forgive others and put oneself in another person’s position. Before, I only complained about the patients, but after thinking, I realize that they have their own difficulties. [Nurse 11]
There is an improvement in concentration. For example, when changing shifts in the morning, I Sometimes cannot focus and pay attention to what other colleagues say. After learning mindfulness, I can basically follow from beginning to end. [Nurse 4]
The most commonly expressed impact of the MLWS intervention was on emotions and communications, helping nurses to calm down, step back, and adjust their cognition. The MLWS intervention also helped them to adjust their mood and coping style through mindful breathing so that they would not communicate in an unstable emotional state.
After attending the mindfulness course, I am not as anxious as before. When I encounter something, I don’t get angry immediately and calm down gradually. It is helpful to think before deciding how to say things. [Nurse 11]
When you are very upset, you will consciously take a deep breath. Whatever you do, you should first calm down and take a deep breath, then slowly calm down and do other things. Although it takes less than half a minute, your attitude, tone of voice and quality and effect of work will be better. [Nurse 13]
In the past, when patients were noisy and couldn’t accept the hospitalization cost, I would talk to them all the time. Now I listen to them. I breathe deeply and listen to them all the time. After adjusting my breathing slowly, I talk to them slowly. [Nurse 14]
Helpful Components Of MLWS Intervention
Nearly 90% of nurses reported that mindful breathing was the most helpful component of the MLWS intervention.
Mindfulness breathing is the most useful element for me. [Nurse 10]
My deepest impression is mindful breathing, which I use every night when I cannot sleep. [Nurse 8]
Body scan and mindful movement were the most helpful components of the MLWS reported by more than half of nurses.
I think the biggest help in attending this course was mindful body scanning. I have a habit of not sleeping until late in the evening and lying in bed for a long time before falling asleep. Practicing mindful body scan helps me to fall asleep easily. [Nurse 16]
I like mindfulness movement better than the sitting meditation. [Nurse 13]
Mindfulness movement is most useful to me. I don’t want to go out or move after I go home from work every day. It’s great to do practice of mindfulness movement at home. I feel relaxed and comfortable after practicing. [Nurse 18]
At the same time, body scan and mindful movement were also the least helpful components of the MLWS reported by one-third of nurses.
I rarely practice body scan and have the feeling that it is not easy to concentrate during body scan. [Nurse 14]
The least helpful practice is mindfulness movement because I always forgot how to practice it. [Nurse 16]
Challenges Of MLWS Intervention
The greatest challenge was being busy at work which caused nurses great fatigue and low energy.
The daily work is too busy and energy consuming, so at night I would prefer to rest not attend the MLWS intervention. [Nurse 18]
There are 2-3 night shifts every week. It is very tiring after a night shift and the only thing I would like to do is rest. [Nurse2]
Another challenge identified was not having an instructor at home for practice and so easily becoming distracted from mindfulness practices. It is difficult to insist on mindfulness practice without guidance of a therapist at home. [Nurse 15]
Discussion
The findings of this study demonstrate that most participants accepted the MLWS intervention and believed that it helped them to improve communications with patients, colleagues, and families; increase acceptance of other people; regulate negative emotions; and cultivate better attention. Our findings are consistent with previous studies which show that mindfulness-based intervention can enhance interpersonal relationships with patients experiencing generalized anxiety disorders,30,31 cultivate the forgiveness of other people among social work students,32 improve emotional regulation in nurses working in senior cadre wards for aged patients20 and nurse leaders,33 and improve concentration ability of social work and healthcare students.32,34,35
Most participants believed that the MLWS intervention helped them to calm down, step back, and adjust their cognition and mood. This finding was most likely due to the mindfulness skill called “STOP” and “RAIN” shared in the MLWS intervention. The acronym “STOP” means remind yourself to STOP, take a breath, observe what is happening in this moment, then continue on with whatever you were doing before you come to a STOP.9 The acronym “RAIN” means recognition (recognize and label your emotion), acceptance (whatever you are experiencing is okay), investigation (feel in your body how emotion manifests itself), and non-identification (not taking emotions so personally and allowing space around them).9 “STOP” and “RAIN” may have helped participants to deal with thoughts and emotions in an efficient way.
Nearly all participants expressed the belief that mindful breathing was the most helpful component of the MLWS intervention. The probable reason was that practice played an important role in mindfulness-based intervention. Breath is always present, free and available to everyone, and can pretty much reflect mood before we even know it, which makes it become a handy tool for mindfulness meditation.9 Participants could easily practice and apply mindful breathing within a short time frame. Future mindfulness-based programs should consider including mindfulness breathing, mindfulness movement and mindfulness body scanning as part of their intervention.
The MLWS intervention was a useful approach for increasing observing in the FFMQ, associated with a significant decrease in acting with awareness but unassociated with significant differences in describing, nonjudging of inner experience, and nonreactivity to inner experience. This finding is inconsistent with previous research which reports that levels of mindfulness assessed by five sub-scales of FFMQ increased significantly from pre- to post-8-weekly MBSR in the moderate-to-large range (eg, observing).36 Mindfulness helps people bring thoughts, feelings, and body sensations to existing moment experiences.9 Observing means paying attention to inner and exterior stimuli, including sensation, emotion, cognition, visual perception. So observing is a very fundamental and important facet in the five facets of FFMQ. Consider that if we cannot notice the internal and external stimuli, it is impossible for us to possess the quality of other facets of mindfulness, including describing, acting with awareness, nonjudging, and nonreactivity to inner experience. The increase in observing in this study means that participants have taken the first step in mindfulness training. Our findings related to the facets of the FFMQ may differ from other studies because of the length of the intervention and relatively short time frame for the post-evaluation. Observing may more easily improve through mindfulness practices in a short-term training intervention; however, long-time mindfulness training may be needed for the other four facets of mindfulness to show improvement. Another probable reason may be related to stressful events occurring at the end of the MLWS intervention. Post-intervention evaluations that were conducted in the last month of the lunar calendar (February) may result in confounders as the nurses were involved in taking a variety of examinations and completing yearly final reports before Spring Festival. Potential personal events before and after the completion of this type of program and prior yoga experience could have a confounding effect and should be noted in future studies.
The absence of significant findings related to the effects of the MLWS intervention on perceived stress, burnout, anxiety, and depression differs from previous studies.10,13 Factors that may have contributed to these differences include the small sample size and short follow-up period that limited potential for behavior change. More time may have been required for participants to experience changes in their scores on the measures of stress, burnout, emotions, and mindfulness state through bringing mindfulness practices into work and daily life. Nonetheless, in their interviews participants reported benefits of the MLWS intervention such as decreased stress and improved emotion regulation.
There were some challenges in implementing the MLWS intervention with nurses caring for PLWH. Nurses experienced difficultly in attending all of the sessions of the MLWS intervention due to the pace and expectations of their work schedules and the impossibility of conducting the MLWS intervention during daily working hours. Therefore, the MLWS intervention had to be arranged after work hours. Other factors influencing attendance at individual sessions included frequent assignment to night shifts (2–3 night shifts every week), nurses’ fatigue brought by heavy workload, family emergencies, and role conflicts associated with expectations of being a daughter, wife, and/or mother. Implementation of MLWS into a healthcare system will be needed to involve the management of the nurses or digital devices to improve the uptake of the MLWS.
Several recommendations are made based on our findings. At the organizational level, support from hospital administration is needed so that nurses caring for HIV-infected patients may attend MLWS interventions. MLWS interventions need to be scheduled during daily work time, making attendance more feasible and personal conflicts less likely to be experienced. We also recommend use of social media such as WeChat to facilitate practice of skills learned and review of content in sessions that may have been missed or require reinforcement. A scheduled supervisory program for nurses during the first weeks after the completion of the MLWS intervention should be tested in a future study.
The results of this study should be considered in relation to the limitations. Most importantly, the one-group design, while appropriate for intervention development and examination of feasibility and acceptability, prevents the determination of whether the pre- and post-test changes are the result of the experimental treatment. A variety of factors, including history and maturation, may result in changes in post-test scores. Further, the use of a volunteer sample raises concerns about participants being highly motivated and biased, or having background characteristics that may interact with the treatment. Small sample size is another limitation. The findings of this study are not generalizable to other groups of nurses or nurses caring for PLWH in other regions in China or other countries. To address some of these limitations, conducting a randomized controlled trial with a larger sample and longer follow-up period is recommended.
Despite these limitations, there are several strengths of this study. Pilot studies play a critical role in new intervention development. Well designed and implemented pilot studies decrease the probability of problems that may arise in clinical trials.37 The data from this study will enhance understanding about strategies that may be successful in implementing a mindfulness intervention with nurses caring for PLWH within a busy and stressful work environment in China. Supporting research to advance nursing science about the effects of mindfulness interventions offers numerous potential benefits for the health and quality of nurses’ work lives, PLWH, and healthcare organizations.
Conclusion
In conclusion, this mindfulness-based intervention for nurses caring for PLWH in China, integrating components of MBSR, MAPs and Chinese cultural practices, was found to be an acceptable intervention with multiple benefits for this population, particularly in managing stress from work and daily life. Moreover, qualitative findings suggest benefits for handling emotion, accepting others, and improving attention. A larger trial should be planned to confirm the findings of this study. The potential implementation of this mindfulness-based intervention may result in greater mindfulness, therefore potentially reducing the burnout rate of our nurses caring for PLWH.
Consent For Publication
All data published here are under the consent for publication.
Ethics Approval And Informed Consent
This study has been approved by The Institutional Review Board of the University of California, Los Angeles (IRB#16-001305) and The Ethics Committee of School of Nursing, Central South University (2017 Ethics Approval File NO.2017004). Written informed consent forms were obtained from these nurses at the time of recruitment.
Abbreviations
PLWH, People Living with HIV; MBIs, Mindfulness-Based Interventions; MBSR, Mindfulness-Based Stress Reduction; MAPs, Mindful Awareness Practices; MLWS, Mindful Living With Stress; RA, Research Assistant; PI, Principal Investigator; CPSS, Chinese Version of the Perceived Stress Scale; CMBI, Chinese Version of the Maslach Burnout Inventory; EE, Emotional Exhaustion; DP, Depersonalization; PA, Personal Accomplishment; Ch-FFMQ, Chinese version of the Five Facets Mindfulness Questionnaire; C-STAI, Chinese version of the State-Trait Anxiety Inventory; C-BDI, Chinese version of the Beck Depression Inventory.
Data Availability
The datasets generated and analyzed during the present study are available from the corresponding author on reasonable request.
Acknowledgments
This research was supported by the NIH-FIC Fogarty International Center (Grant # D43 TW009579, PI: Deborah Koniak-Griffin) and the Hunan Science and Technology Commission Foundation (Grant No 2017SK50133).
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Disclosure
Dr. Deborah Koniak-Griffin reports grant from NIH-FIC Fogarty International Center and Dr. Chen Pan reports grant from Hunan Science and Technology Commission Foundation, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. Ezenwaji IO, Eseadi C, Okide CC, et al. Work-related stress, burnout, and related sociodemographic factors among nurses: implications for administrators, research, and policy. Medicine. 2019;98(3):e13889. doi:10.1097/MD.0000000000013889
2. Jiang H, Li C, Gu Y, Lu H. Nurse satisfaction and burnout in Shanghai Neurology Wards. Rehabil Nurs. 2016;41(2):120–127. doi:10.1002/rnj.174
3. Lopez-Castillo J, Gurpegui M, Ayuso-Mateos JL, Luna JD, Catalan J. Emotional distress and occupational burnout in health care professionals serving HIV-infected patients: a comparison with oncology and internal medicine services. Psychother Psychosom. 1999;68(6):348–356. doi:10.1159/000012354
4. Gueritault-Chalvin V, Kalichman SC, Demi A, Peterson JL. Work-related stress and occupational burnout in AIDS caregivers: test of a coping model with nurses providing AIDS care. AIDS Care. 2000;12(2):149–161. doi:10.1080/09540120050001823
5. Ding Y, Yang Y, Yang X, et al. The mediating role of coping style in the relationship between psychological capital and burnout among Chinese Nurses. PLoS One. 2015;10(4):e0122128. doi:10.1371/journal.pone.0122128
6. Qiao Z, Chen L, Chen M, et al. Prevalence and factors associated with occupational burnout among HIV/AIDS healthcare workers in China: a cross-sectional study. BMC Public Health. 2016;16:335. doi:10.1186/s12889-016-2890-7
7. Nantsupawat A, Nantsupawat R, Kunaviktikul W, Turale S, Poghosyan L. Nurse burnout, nurse-reported quality of care, and patient outcomes in Thai Hospitals. J Nurs Scholarship. 2016;48(1):83–90. doi:10.1111/jnu.2015.48.issue-1
8. Canadas-De la Fuente GA, Vargas C, San LC, Garcia I, Canadas GR, De la Fuente EI. Risk factors and prevalence of burnout syndrome in the nursing profession. Int J Nurs Stud. 2015;52(1):240–249. doi:10.1016/j.ijnurstu.2014.07.001
9. Amouretti M, Le Pen C, Gaudin AF, et al. Impact of irritable bowel syndrome (IBS) on health-related quality of life (HRQOL). Gastroenterol Clin Biol. 2006;30(2):241–246. doi:10.1016/S0399-8320(06)73160-8
10. Zhang LH, Xiang L, Deng XF. Influence of mindfulness decompression intervention on job burnout of emergency nurses. Chin Nurs Res. 2015;29:954–955.
11. Hunter L. Making time and space: the impact of mindfulness training on nursing and midwifery practice. A critical interpretative synthesis. J Clin Nurs. 2016;25(7–8):918–929. doi:10.1111/jocn.2016.25.issue-7pt8
12. White L. Mindfulness in nursing: an evolutionary concept analysis. J Adv Nurs. 2014;70(2):282–294. doi:10.1111/jan.12182
13. Dos Santos TM, Kozasa EH, Carmagnani IS, et al. Positive effects of a stress reduction program based on mindfulness meditation in brazilian nursing professionals: qualitative and quantitative evaluation. Explore. 2016;12(2):90–99. doi:10.1016/j.explore.2015.12.005
14. Wang YX, Jiang CL. The biological mechanisms of mindfulness meditation and relationship between mindfulness meditation and psychosomatic health. Chin Ment Health J. 2016;30:105–108.
15. Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. New York: Delta; 1990.
16. Smith SA. Mindfulness-based stress reduction: an intervention to enhance the effectiveness of nurses’ coping with work-related stress. Int J Nurs Knowl. 2014;25(2):119–130. doi:10.1111/2047-3095.12025
17. Bazarko D, Cate RA, Azocar F, Kreitzer MJ. The impact of an innovative mindfulness-based stress reduction program on the health and well-being of nurses employed in a corporate setting. J Workplace Behav Health. 2013;28(2):107–133. doi:10.1080/15555240.2013.779518
18. Bower JE, Crosswell AD, Stanton AL, et al. Mindfulness meditation for younger breast cancer survivors: a randomized controlled trial. Cancer. 2015;121(8):1231–1240. doi:10.1002/cncr.v121.8
19. Black DS, O’Reilly GA, Olmstead R, Breen EC, Irwin MR. Mindfulness meditation and improvement in sleep quality and daytime impairment among older adults with sleep disturbances: a randomized clinical trial. JAMA Intern Med. 2015;175(4):494–501. doi:10.1001/jamainternmed.2014.8081
20. Yu T. Effect of mindfulness-based cognitive therapy on negative emotion of nurses in senior cadre ward for elderly patients. J Nurs. 2015;22(19):63–65.
21. Zhang XY, Yang R, Xie JL. The effect of group mindfulness therapy on sleep quality and job burnout among Nurses. J Nurses Train. 2014;29:1419–1420.
22. Gu XY, Ye YS, Yan-Sheng YE. Influence of mindfulness on achievement motivation of nurses in department of cardiology. Nurs Prac Res. 2011;11(1):35.
23. Guan YL, Yuan JY. Influences of samyaksmrti on chievement motivation in nurses of rheumatism immunity department. J Nurs Admin. 2013;13(11):765–766.
24. Buric I, Farias M, Jong J, Mee C, Brazil IA. What is the molecular signature of mind-body interventions? A systematic review of gene expression changes induced bymeditation and related practices. Front Immunol. 2017;8:670. doi:10.3389/fimmu.2017.00670
25. Yang T, Wu D, Zhang W, Cottrell RR, Rockett IR. Comparative stress levels among residents in three Chinese provincial capitals, 2001 and 2008. PLoS One. 2012;7(11):e48971. doi:10.1371/journal.pone.0048971
26. Deng YQ, Xia CY. The five facet mindfulness questionnaire: psychometric properties of the chinese version. Mindfulness. 2011;2(2):123–128. doi:10.1007/s12671-011-0050-9
27. Bohlmeijer E, Ten Klooster PM, Fledderus M, Veehof M, Baer R. Psychometric properties of the five facet mindfulness questionnaire in depressed adults and development of a short form. Assessment. 2011;18(3):308–320. doi:10.1177/1073191111408231
28. Wang XD, Wang XL, Ma H. Rating Scales for Mental Health (Updated version). Beijing: Chinese Mental Health Journal Club; 1999.
29. Zhang YX, Wang Y, Qian MY. Reliability and validity of Beck Depression Inventory (BDI) examined in Chinese samples. Chin Ment Health J. 1990;4:164–192.
30. Millstein DJ, Orsillo SM, Hayes-Skelton SA, Roemer L. Interpersonal problems, mindfulness, and therapy outcome in an acceptance-based behavior therapy for generalized anxiety disorder. Cogn Behav Ther. 2015;44(6):491–501. doi:10.1080/16506073.2015.1060255
31. Penque S. Mindfulness to promote nurses’ well-being. Nurs Manage. 2019;50(5):38–44. doi:10.1097/01.NUMA.0000557621.42684.c4
32. Birnbaum L. The use of mindfulness training to create an ‘accompanying place’ for social work students. Social Work Education. 2008;27(8):837–852. doi:10.1080/02615470701538330
33. Pipe TB, Bortz JJ, Dueck A, Pendergast D, Buchda V, Summers J. Nurse leader mindfulness meditation program for stress management: a randomized controlled trial. J Nurs Adm. 2009;39(3):130–137. doi:10.1097/NNA.0b013e31819894a0
34. Jain S, Shapiro SL, Swanick S, et al. A randomized controlled trial of mindfulness meditation versus relaxation training: effects on distress, positive states of mind, rumination, and distraction. Ann Behav Med. 2007;33(1):11–21. doi:10.1207/s15324796abm3301_2
35. Gilmartin H, Goyal A, Hamati MC, Mann J, Saint S, Chopra V. Brief mindfulness practices for healthcare providers - a systematic literature review. Am J Med. 2017;130(10):
36. Carmody J, Baer RA. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. J Behav Med. 2008;31(1):23–33. doi:10.1007/s10865-007-9130-7
37. Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res. 2011;45(5):626–629. doi:10.1016/j.jpsychires.2010.10.008
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
