Back to Journals » Journal of Pain Research » Volume 15
Migraine Attacks and Relevant Trigger Factors in Undergraduate Nursing Students in Hong Kong: A Cross-Sectional Study
Authors Xie YJ, Lin M, Wong YT, Yan L , Zhang D , Gao Y
Received 15 September 2021
Accepted for publication 27 February 2022
Published 10 March 2022 Volume 2022:15 Pages 701—713
DOI https://doi.org/10.2147/JPR.S337465
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Alexandre F DaSilva
Yao Jie Xie,1 Meijuan Lin,1 Yuen Ting Wong,2 Linjia Yan,3 Dexing Zhang,4 Yang Gao5
1School of Nursing, The Hong Kong Polytechnic University, Hung Hom, Kowloon, Hong Kong Special Administrative Region; 2Faculty of Social Science, The University of Hong Kong, Pokfulam, Hong Kong Special Administrative Region; 3Yibin Health School of Sichuan, Yibin City, Sichuan Province, People’s Republic of China; 4JC School of Public Health and Primary Care, The Chinese University of Hong Kong, Shantin, N.T., Hong Kong Special Administrative Region; 5Department of Sport, Physical Education and Health, Hong Kong Baptist University, Kowloon Tong, Kowloon, Hong Kong Special Administrative Region
Correspondence: Yao Jie Xie, School of Nursing, The Hong Kong Polytechnic University, Hung Hom, Kowloon, Hong Kong Special Administrative Region, Tel +852 3400-3798, Fax +852 2364-9663, Email [email protected]
Objective: This study aimed to examine the prevalence and features of migraine and explore the possible migraine triggers in a sample of university nursing students in Hong Kong.
Methods: A cross-sectional study using self-administered questionnaires was conducted in the Hong Kong Polytechnic University in 2016. The questionnaire included ID Migraine™ for migraine screening and items measuring the frequency, duration, severity, associated symptoms, and trigger factors of migraine. Years 2– 5 undergraduate nursing students from the university completed the questionnaires. Binary logistic regression was conducted to examine the migraine-associated factors.
Results: A total of 702 nursing students, including 168 males and 534 females, were successfully screened. Their mean age was 20.8 ± 1.4 years. The overall prevalence of migraine reached 11.8%. Over half (67.5%) of the students with migraine experienced attacks at least once per month. Each attack had a median duration of 3 h (interquartile range: 1– 4 h) and the mean pain intensity score of 6.4 ± 1.6. Students with a family history of migraine (adjusted odds ratio [OR]: 1.89; 95% confidence interval [CI]: 1.10, 3.25; p < 0.05) and poor general health status (Adjusted OR: 3.41, 95% CI: 1.05, 11.09; p < 0.05) were more likely to suffer from migraine than those without. The three most common migraine triggers were the lack of sleep (94.0%), change in sleep schedule (83.1%), and noise (81.9%). Female students were more likely to experience fatigue-triggered migraine than male students (85.9% vs 63.2%, p < 0.05).
Conclusion: Migraine prevalence was relatively high among undergraduate nursing students in Hong Kong. Sleep problem was the most frequent trigger factor. The students’ awareness of migraine attacks should be increased, and migraine management must be improved by avoiding common trigger factors in this population.
Keywords: migraine, prevalence, trigger factor, nursing student, Hong Kong
Introduction
Migraine, a primary headache disorder, is characterized by recurrent headache attacks and associated gastrointestinal symptoms, such as nausea, vomiting, photophobia, and phonophobia.1,2 A systematic review of 302 studies found that the prevalence of migraine ranged from 9.7% to 16.4% worldwide and was thrice higher in females than in males.3 Headache disorders including migraine was the 15th cause of disability-adjusted life-years (DALYs) among the all-age population and the second cause of DALYs among people aged 10–24 years.4 This condition contributes to the heavy financial burden and economic losses caused by high medical costs and impaired productivity.5
Various trigger factors may lead to migraine attacks. Changes in sleeping patterns, such as the lack of sleep and changes in sleep schedule;6 substantial emotional changes and psychological influences, such as stress;7,8 vigorous exercise;9 foods, including milk, cheese, alcohol, coffee, and chocolate;10 and external environmental changes, for example, cold and hot weather changes, noise, and strong smells,6,11 can all trigger the onset of migraine. In addition, hormonal factors, such as menstruation and pregnancy, are predominant migraine triggers in females.6,12 Migraine attacks could be prevented by avoiding these triggers. The prevention then alleviates the negative health impact of attacks on individuals.
Migraine are a common health condition among University students. Wang et al reported that the pooled migraine prevalence among university students is 16.1% worldwide with rates of 11.3% and 21.7% in male and female students, respectively.13 Migraine are a common psychosomatic complaint among medical students, especially those frequently exposed to physical and psychological stressors from their studies.14 A study conducted on medical students with migraine in Turkey indicated that 30% of the medical students would miss classes and clinical practicum during migraine attacks.15 Frequent attacks negatively influence the medical students’ daily lives and academic performance, thus leading to emotional suffering, lack of satisfaction, reduced vitality and concentration, and sleep disturbances.16,17 A similar situation was observed among nursing students from the discipline of health science. Previous studies reported a migraine prevalence of 12% to 18.9% for this population.18–20 The characteristics of the nursing curriculum may lead to high exposure to certain trigger factors. Nursing students must complete multiple examinations and assignments during their college life. They might be more anxious about tests than non-nursing students21 and might feel stressed due to their frequent clinical assessments22 and placements.23 High stress levels might lead to increased migraine intensity and frequency.24 The sleep quality of nursing students is also poorer than that of non-nursing students.25 Frequent shift work with sleep disturbances could trigger migraine attacks.26 Moreover, fatigue, sickness, and hunger are typical migraine trigger factors among nursing students.19
The special learning experiences of nursing students in college life relative to those of general university students may lead to an increased risk of migraine attacks. Thus, knowing the situation of migraine attacks in this population is important to help improve migraine awareness, avoid trigger factors, and reduce migraine attacks accordingly. However, no evidence has shown the migraine status of nursing students in Hong Kong. Given their distinct cultural background, environmental factors, and lifestyle, migraine attacks in this population in Hong Kong may differ from those in other countries. Therefore, we conducted this study to investigate the prevalence and features of migraine and explored the typical migraine triggers in a sample of Hong Kong undergraduate nursing students.
Methods
Study Design and Ethical Consideration
A cross-sectional study using self-administered questionnaires was designed to collect the data of nursing students from The Hong Kong Polytechnic University (PolyU). The Human Subjects Ethics Subcommittee of PolyU approved this study (Reference Number: HSEARS20160502001). A written informed consent form was received from each participant before questionnaire administration. Students participated in the study on a voluntary basis. The study was conducted in accordance with the Declaration of Helsinki.
Study Population
The target population was university nursing students studying for a full-time bachelor’s degree in Hong Kong. The accessible population comprised nursing students studying general nursing or are in a mental nursing program in PolyU. The inclusion criteria were as follows: 1) full-time Years 2–5 undergraduate students, 2) Hong Kong Chinese, and 3) willing to participate in the study and provide informed consent. Considering that this study was conducted within the first 2 weeks of the academic year, it excluded Year 1 students, who supposedly experience less exposure to the potential trigger factors related to university studies than students in other years.
Sample Size and Sampling Method
Sample size was calculated by using the Power Analysis and Sample Size Software. A sample size of 593 was needed to achieve 90% power and 0.05 significance level when the prevalence of migraine was 10%, which was estimated in accordance with previous studies conducted in mainland China (9%)27 and Hong Kong (12.5%).28 Given the response rate of 80% and potential incomplete questionnaire rate of 5%, the sample size was then adjusted to 780. In consideration of accessibility and availability at a given time, convenience sampling was adopted in this study, and nursing students in PolyU were selected.
Measurement
A self-administered questionnaire was designed to collect data. The questionnaire included four parts: 1) basic participant characteristics, 2) migraine screening, 3) migraine features, and 4) possible trigger factors.
Basic Participant Characteristics
The characteristics included gender, nursing program, study year, age, body weight and height, residence district, migraine family history, and cumulative grade point average (GPA). The GPA is the cumulative average grade point calculated for all subjects taken by the university student (maximum GPA: 4.00). The participants were also asked to rate their levels of general health and quality of life separately by using a four-point Likert scale as “excellent”, “good”, “fair”, or “poor”.
Migraine Screening
The second part of the questionnaire was used to identify possible migraine cases. The participants were initially screened by asking if they had experienced two or more headaches in the past 1 year. If they had, the participants would continue completing the ID Migraine™ test. ID Migraine™ is a quick screening tool for identifying migraine cases. This tool includes questions regarding the frequency of headache attacks, the effect of headaches on work and life, willingness to seek a physician for headache treatment, and the signs and symptoms of migraine (photophobia, nausea, and inability to work) in the past 3 months.29 In the study, the Chinese version of ID Migraine™ was adopted; the sensitivity and specificity of this tool have been found to be acceptable among Chinese university students and were 84% and 64%, respectively.30 The students with positive screening results were asked to continue answering the migraine-related items. The students without positive screening results were considered to have already finished the survey.
Migraine Features
The third part of the questionnaire was used to measure the features of migraine, including the frequency, duration, severity, characteristics, and associated symptoms of headaches and pain-relieving methods.31 The participants were also asked about their medications for migraine attacks. Frequency was measured by asking the participants the following question: “How many times have you had migraine attacks in the last year?” The options for responses included “almost every day,” “1–3 time(s) per week,” “4–6 times per week,” “every 2 weeks,” “every month,” “every 2–3 months,” and “every half a year.” The duration of headache was recorded as the average hours for a typical headache attack in the last 3 months. Headache severity was measured by using a visual analog scale with a 0–10 numeric pain rating, where 0 indicates no pain and 10 denotes the highest pain level.
Possible Migraine Trigger Factors
Seven categories of trigger factors were classified in accordance with the previous experiences reported by migraine studies and the literature:32–34 diet (hunger, drinking alcohol, drinking coffee, eating/drinking dairy products, and eating chocolate), environment (bright light, odor, changes in weather, hot weather, cold weather, cigarette smoking, and noise), sleep (over-sleeping, lack of sleep, and changes in sleep schedule), stress (from academics, from clinical work, from social life, from the work environment, and from family), menstruation (for female students), physical activity (daily exercise, head movements, and fatigue), and changes in emotion. The students with migraine were required to report the trigger factors that they had experienced and indicate frequency as follows: “never”, “infrequent”, “approximately half of the time,” “often”, and “always”.
Validity and Reliability of the Questionnaire
The questionnaires were distributed to 32 Years 2–5 students in the mental and general nursing programs, among which four students from each year and each program were invited. The students commented that the overall wording was understandable and readable. Minor modifications were made to the wording of items in accordance with the students’ comments. Content validity was examined by consulting six experts from different professional fields, including two neurological doctors, two neurological nurses, and two researchers. The experts were invited to rate each item of the questionnaire by using a four-point Likert scale (1 = not relevant, 2 = somewhat relevant, 3 = quite relevant, and 4 = highly relevant)35 and to give their opinions on the relevance of an item to the study purpose. Detailed reasons were required for the items that were scored 2 or below. The item–content validity index (I-CVI) was calculated. In total, 98% of the items received a score over 0.833, indicating the good content validity of the questionnaire. An item with a low I-CVI (0.667), ie, queries regarding “place of birth,” was deleted. Minor changes in wording were made to several items in accordance with the experts’ comments. Finally, the examination for test–retest reliability was conducted. A total of 30 Year 5 general nursing students were invited to complete the questionnaires twice with an interval of 1 week.36 The results showed that 56 out of 63 items showed high correlations (coefficient > 0.5, all p < 0.05) between the first and second tests, demonstrating that the questionnaire had the optimal level of the reliability.
Data Collection Procedure
Data collection was conducted during eight nursing lessons in September 2016 with one lesson from each year level (Year 2 to Year 5) and each nursing program (general or mental). Email approval for the distribution of questionnaires during lecture was received from the lecturers in advance. The research team then went to a lecture room 10 min before the start of a lesson. A brief introduction of the study was given to the students. The paper questionnaires and informed consent forms were distributed to the students thereafter. The research team provided concurrent explanations to the students when they had any queries about the questionnaire. The time required to complete the questionnaire was approximately 10 min. The questionnaires were collected at the end of the lesson. Questionnaires with less than 5% missing data were considered as valid.
Data Analysis
Descriptive statistics were used to describe basic participant characteristics, migraine situation, and features. Numbers and percentages were used to describe categorical variables, and median and interquartile range (IQR) or mean and standard deviation (SD) were used to describe the continuous variables with or without normal distribution where appropriate. Pearson’s chi-squared test or Fisher’s exact test was applied to compare the differences in the distribution of categorical variables regarding the different demographics and characteristics of the students. One-way analysis of variance (ANOVA) was performed to test the differences in normally distributed continuous variables across groups. The nonparametric test was adopted for variables with non-normal distribution. Binary logistic regression was conducted to examine the association between participant characteristics and migraine prevalence. All data were analyzed by using IBM SPSS Statistics software 26.0 version. All statistical tests were two-tailed, and p < 0.05 was considered to be statistically significant.
Results
The questionnaires were distributed to 766 students. In total, 707 students returned the questionnaires. Except for five blank questionnaires, 702 were valid questionnaires with a response rate of 91.6%.
Participants’ Characteristics
Table 1 shows the basic characteristics of the participants. In total, 168 male students (23.9%) and 534 female students (76.1%) participated in the study. The mean age of the participants was 20.8 ± 1.4 years. Male students exhibited significantly higher body weight (62.6 vs 51.7 kg, p < 0.001), body height (1.7 vs 1.6 m, p < 0.001), and body mass index (BMI) (21.0 vs 20.2 kg/m2, p = 0.001) than female students. The majority of the nursing students were studying a general program (69.1%). More female students reported a cumulative GPA greater than 3.00 than male students (43.6% vs 33.9%, p = 0.026). Most of the students (65.8%) lived in the New Territories. Over 18% of the students claimed a family history of migraine. A total of 2.3% and 1.3% of the participants reported poor general health and poor quality of life, respectively.
 |
Table 1 Basic Characteristics of Participants by Gendera |
Migraine Prevalence According to the Participants’ Characteristics
The migraine situation of nursing students is presented in in Table 2. Migraine was detected in 83 students in accordance with the ID Migraine™ screening test. The overall prevalence of migraine was 11.8%. Students who had a family history of migraine were more likely to present a higher prevalence of migraine than those without (19.0% vs.10.3%, p = 0.006). Students who considered themselves to have poor general health status and poor quality of life presented a significantly higher prevalence of migraine than those with good self-ratings (health status: 37.5% vs 11.2%, p = 0.001; quality of life: 44.4% vs 11.4%, p = 0.014). No statistically significant differences were found in terms of gender, nursing program, study year, cumulative GPA, residence district, and obesity status.
 |
Table 2 Prevalence of Migraine by Participants’ Characteristics |
Table 3 depicts the association of participant characteristics with migraine condition. The variables, including the family history of migraine, general health status, and quality of life, that showed significant associations with migraine in univariate analysis were involved in the logistic regression analysis. In the simple regression model, all three variables showed significant associations with migraine. The crude odds ratio (OR) was 2.04 (95% confidence interval [CI]: 1.21, 3.43; p = 0.007), 4.75 (95% CI: 1.68, 13.42; p = 0.003), and 6.22 (95% CI: 1.64, 23.64; p = 0.007) for the history of migraine, general status of health, and poor quality of health, respectively. When the age, gender, BMI and cumulative GPA were adjusted in the model, a significant association with migraine existed for the family history of migraine and general status of health. The odds of having migraine were 1.89 and 3.41 times higher among students who had a family history of migraine (adjusted OR: 1.89; 95% CI: 1.10, 3.25, p = 0.022) and poor general health status (adjusted OR: 3.41, 95% CI: 1.05, 11.09, p = 0.041), respectively, than in those without.
 |
Table 3 Odds Ratios (ORs) of Migraine Experience in Accordance with the Family History of Migraine, Health Status, and Quality of Life |
Migraine Features of Nursing Students
Among the 83 students identified with migraine in the whole sample, 56 (67.5%) experienced migraine attacks at least once per month in the past 1 year (Figure 1). The median duration of each attack was 3 h (IQR: 1–4 h), and the mean pain intensity was 6.4 (SD = 1.6). Figure 2 shows the headache characteristics of students with migraine. The most common characteristics of headaches were pressure (49.4%), dullness (41.0%), and pain (33.7%). Depression (59.0%), hypoactivity (57.8%), fatigue (54.2%), and nausea (50.6%) were the most common symptoms of headaches found in this sample (Figure 3). The most common pain-relieving method was sleeping (73.5%), followed by deep breathing (18.1%), bathing (15.7%) and listening to music (15.7%) (Figure 4).
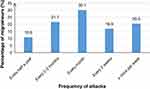 |
Figure 1 Frequency of migraine attacks among nursing students with migraine. |
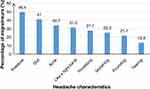 |
Figure 2 Headache characteristics among nursing students with migraine. |
 |
Figure 3 Symptoms during attack among nursing students with migraine. |
 |
Figure 4 Pain relieving methods among nursing students with migraine. |
Trigger Factors of Migraine
Table 4 shows the trigger factors experienced by the students with migraine. Male and female students were compared. In general, the most five common trigger factors were “lack of sleep” (94.0%), “change in sleep schedule” (83.1%), and “noise” (81.9%), followed by “academic stress” (80.7%) and “fatigue” (80.7%). Compared with male students, female students were more likely to experience migraine triggered by “fatigue” (85.9% vs 63.2%, p = 0.027). Menstruation was also one of the common migraine triggers for female students (68.8%).
 |
Table 4 Trigger Factors of Migraine in Students with Migraine (n = 83)a |
Discussion
Prevalence of Migraine
The overall prevalence of migraine found by our study was similar to that found by a study on university students in India20 but lower than that reported by studies conducted on nursing students in South East Nigeria18 and Turkey,19 where the prevalence reached 13.1% and 18.9%, respectively. The differences in the migraine prevalence rates of different populations might be due to inherited ethnic differences or external factors, such as environmental factors and dietary habits, which could be trigger factors of migraine.37 Furthermore, the findings might be partially explained by the study period. The data in our study were collected in early September immediately after the summer holidays, whereas the data in the study from Turkey were collected in May, which was close to the final examinations and assignment deadlines.19 Given that the migraine screening test is based on the occurrence of migraine attacks in the last 3 months, the prevalence of migraine would be high when the data are collected during a stressful period.37
In this study, the students who reported poor general health status were more likely to have migraine than those who did not. Terwindt et al38 indicated that subjects with migraine reported lower scores for the aspect of general health perception than those without migraine. Self-reported general health status was significantly associated with the students’ satisfaction with their School experiences.39 High stress in learning may result in a negative effect on the students’ school experiences; this negative effect subsequently influences the students’ perception of health status. Stress itself is a trigger factor of migraine.8,19 Nursing students in Hong Kong experience a moderate level of stress mostly from assignments and their clinical workload.23 In Hong Kong, undergraduate nursing students are required to complete at least 1238 h of theoretical instruction and 1400 h of clinical and field experience for a 5-year curriculum.40 Such a heavy school load might be an original reason for migraine occurrence. Students with a family history of migraine also showed high migraine prevalence. Similar results were observed in previous studies.41,42 These findings could be attributed to genetic etiology given that several studies have indicated that certain genetic factors increase migraine susceptibility, especially in people with first-degree relatives suffering from migraine.43,44
Characteristics of Migraine
The majority of students with migraine (67.5%) had one or more attacks per month. This proportion was slightly higher than that in medical students (49.5%) in the United States (US).45 Similar to that in students in India20 and Turkey,19 medium headache intensity was observed in the nursing students in our study. Most students with migraine in our study described their headache as exerting pressure, dullness, and pain in contrast to those in previous studies, who reported pulsating/throbbing as the major characteristic of the headache experienced.18,46,47 This finding may be due to the characterization of headaches in accordance with subjective feelings and different understandings and interpretations of the descriptive words used in the questionnaire. The most common symptoms of headache reported in our study were depression, hypoactivity, fatigue, neck stiffness, or pain and nausea. These symptoms present commonly in migraine attacks.1 Most of the students in our study selected sleeping as the method to relieve headache. Sleeping was also the most common nonpharmacological pain releasing strategy of the medical students in previous studies.19,48
Trigger Factors of Migraine
The lack of sleep and change in sleep schedule were the most selected migraine triggers of the nursing students in our study. Similar results have been found in other studies.20,42,45 University students, especially students from the faculty of medicine, were more likely to be poor sleepers and prone to suffer from insufficient sleep.49 The shortened sleeping times of nursing students may be due to the heavy academic workload and clinical placement of the nursing curriculum. During clinical placement, excessive time for after-work preparation, such as case studies, clinical skill practice, and preparation for clinical assessments, is required and may therefore decrease sleeping time. Involvement in shift work during clinical placement could also lead to changes in sleeping patterns. Given that certain hospitals may not offer overnight dormitory to students, sleeping time may also decline due to long travel times from the students’ homes to the hospital. Previous studies showed that stress is the most prevalent trigger factor of migraine.18,19,37 In the present study, academic stress was ranked as the fourth most prevalent trigger factor. Although it was not the most selected trigger, significant stress status is a noticeable mental health issue among nursing students. Fatigue was also indicated as one of the prevalent triggers of migraine in this study. Similar results were identified in a previous research.19 In our study, female students were more likely to experience fatigue-triggered migraine than male students. Given that female students had higher cumulative GPA than male students, they may exert more effort in studying and preparing for clinical placement than male students. Increased workload may lead to the increased chance of experiencing fatigue among female students, thus raising the probability of triggering migraine.
Noise was one of the major migraine trigger factors in this study. This variable is a typical environmental migraine trigger factor in the literature.50 However, noise was not indicated as a common migraine trigger in several previous studies conducted in Croatia51 and the US.8 This discrepancy may be due to geographical differences. Living areas in Hong Kong are overcrowded. This condition may exacerbate the mental stress and irritation induced by excessive noise from traffic, construction, intruder alarm systems, and neighbors.52
Strengths and Limitations of the Study
To our knowledge, this study was the first to investigate the migraine situation of nursing students in Hong Kong. The myths and misconceptions of headaches and the presumptive diagnosis of patients would lead to misdiagnosis and delay the proper treatment of migraine.53 Our study, which included the screening of migraine and the identification of trigger factors, could raise students’ awareness of preventing migraine attacks and undergoing prompt medical consultation.
This study had several limitations. First, the self-reported measures might lead to certain biases. However, we believe our assessment is acceptable The undergraduate nursing students in this study could understand the questionnaire items well and identify their own migraine triggers easily because they have medical knowledge. Second, due to time and manpower limits, we only used the ID MigraineTM and self-reported doctor diagnosis to identify migraine cases. This approach may lead to the underestimation of migraine prevalence. Furthermore, the ID MigraineTM cannot discern between primary and secondary migraine. Nevertheless, our study provides the first evidence for the migraine situation of the Hong Kong youth population under unique academic pressure. Third, nursing students were recruited from only one university, thus limiting the generalizability of our results to a certain extent. However, the nursing programs of universities in Hong Kong have similar gender distributions, study durations, and main components (theory and clinical practicum). Thus, recruiting subjects from one university is still acceptable, and these students are representative of the university nursing students in Hong Kong. Lastly, only two items were used to assess the self-perceived general health and quality of life. Given that these aspects were not the main outcomes of this study and due to time limitation, the standard questionnaires for evaluating the general health and quality of life were not used in our study. However, the significant associations found among migraine, general health, and quality of life in our study suggest that future studies could be conducted to explore how migraine attacks influence the health-related quality of life in different aspects.
Conclusions
The prevalence of migraine was relatively high among undergraduate nursing students in Hong Kong. The students’ awareness of migraine attacks and migraine management must be enhanced. The lack of sleep, changes in sleep schedule, noise, academic stress, and fatigue are modifiable trigger factors of migraine attacks that could be avoided. Increasing the awareness of how to avoid typical trigger factors, as well as the prophylactic strategies for reducing migraine attacks, are suggested.
Acknowledgments
We thank Dr. Ya Shuang Zhao to provide us the Chinese version of ID Migraine™.
We are also grateful to our team members (Kong Lai Lam, Elaine Yi Lam Cheng, Yuen Mei Wong, Phoebe Ngai Yan Chan, Chui Yuk Yu, Hoi Ying Ho, Sin Ki Lau and Ching Han Fung) for their important contributions to the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Ettlin DA. The international classification of headache disorders, (beta version). Cephalalgia. 2013;33:629–808.
2. World Health Organization. Headache disorders; 2016. Available from: http://www.who.int/mediacentre/factsheets/fs277/en/.
3. Woldeamanuel YW, Cowan RP. Migraine affects 1 in 10 people worldwide featuring recent rise: a systematic review and meta-analysis of community-based studies involving 6 million participants. J Neurol Sci. 2017;372:307–315. doi:10.1016/j.jns.2016.11.071
4. Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi:10.1016/S0140.6736(20)30925-9
5. Linde M, Gustavsson A, Stovner L, et al. The cost of headache disorders in Europe: the Eurolight project. Eur J Neurol. 2012;19(5):703–711. doi:10.1111/j.1468-1331.2011.03612.x
6. Fukui PT, Gonçalves TRT, Strabelli CG, et al. Trigger factors in migraine patients. Arq Neuropsiquiatr. 2008;66(3A):494–499. doi:10.1590/S0004-282X2008000400011
7. Hauge AW, Kirchmann M, Olesen J. Characterization of consistent triggers of migraine with aura. Cephalalgia. 2011;31(4):416–438. doi:10.1177/0333102410382795
8. Kelman L. The triggers or precipitants of the acute migraine attack. Cephalalgia. 2007;27(5):394–402. doi:10.1111/j.1468-2982.2007.01303.x
9. Pavlovic JM, Buse DC, Sollars CM, Haut S, Lipton RB. Trigger factors and premonitory features of migraine attacks: summary of studies. Headache. 2014;54(10):1670–1679. doi:10.1111/head.12468
10. Finocchi C, Sivori G. Food as trigger and aggravating factor of migraine. Neurol Sci. 2012;33(1):77–80. doi:10.1007/s10072-012-1046-5
11. Wang J, Huang Q, Li N, Tan G, Chen L, Zhou J. Triggers of migraine and tension‐type headache in C hina: a clinic‐based survey. Eur J Neurol. 2013;20(4):689–696. doi:10.1111/ene.12039
12. Stewart W, Wood C, Reed M, Roy J, Lipton RB. Cumulative lifetime migraine incidence in women and men. Cephalalgia. 2008;28(11):1170–1178. doi:10.1111/j.1468-2982.2008.01666.x
13. Wang X, Zhou H, Sun J, Xing Y, Zhu Y, Zhao Y. The prevalence of migraine in university students: a systematic review and meta‐analysis. Eur J Neurol. 2016;23(3):464–475. doi:10.1111/ene.12784
14. Balaban H, Semiz M, Şentürk İA, et al. Migraine prevalence, alexithymia, and post-traumatic stress disorder among medical students in Turkey. J Headache Pain. 2012;13(6):459. doi:10.1007/s10194-012-0452-7
15. Bicakci S, Over F, Aslan K, Bozdemir N, Saatci E, Sarica Y. Headache characteristics in senior medical students in Turkey. Tohoku J Exp Med. 2007;213(3):277–282. doi:10.1620/tjem.213.277
16. Adams AM, Serrano D, Buse DC, et al. The impact of chronic migraine: the Chronic Migraine Epidemiology and Outcomes (CaMEO) Study methods and baseline results. Cephalalgia. 2015;35(7):563–578. doi:10.1177/0333102414552532
17. Chaushev N, Milanov I. Impact of migraine and migraine treatment on patient”s capacity to work and quality of life. J Clin Med. 2009;2(3):26–31.
18. Ezeala-Adikai B, Ekenze O, Onwuekwe I. Frequency and pattern of migraine among medical and nursing students at Enugu, South East Nigeria. J Headache Pain. 2013;14(1):5. doi:10.1186/1129-2377-14-S1-P5
19. Saritas S, Saritas SC, Erci B, Karabulut N. Nursing student”s behaviours and attitude towards headache. Int J Med Investig. 2015;4(4):368–373.
20. Sujitha ERR. A multi method approach to measure the migraine distress among students. J Sci. 2014;4(9):583–586.
21. Driscoll R, Evans G, Ramsey G, Wheeler S. High test anxiety among nursing students. Online submission. 2009.
22. Watson R, Deary I, Thompson D, Li G. A study of stress and burnout in nursing students in Hong Kong: a questionnaire survey. Int J Nurs Stud. 2008;45(10):1534–1542. doi:10.1016/j.ijnurstu.2007.11.003
23. Chan CK, So WK, Fong DY. Hong Kong baccalaureate nursing students” stress and their coping strategies in clinical practice. J Prof Nurs. 2009;25(5):307–313. doi:10.1016/j.profnurs.2009.01.018
24. Schramm SH, Moebus S, Lehmann N, et al. The association between stress and headache: a longitudinal population-based study. Cephalalgia. 2015;35(10):853–863. doi:10.1177/0333102414563087
25. Kim G-H, Yoon HS. Factors influencing sleep quality in nursing students and non nursing students. J Korean Acad Psychiatr Ment Health Nurs. 2013;22(4):320–329. doi:10.12934/jkpmhn.2013.22.4.320
26. Kuo W-Y, Huang -C-C, Weng S-F, et al. Higher migraine risk in healthcare professionals than in general population: a nationwide population-based cohort study in Taiwan. J Headache Pain. 2015;16(1):102. doi:10.1186/s10194-015-0585-6
27. Wang X, Sun J, Xing Y, Zhu Y, Zhu Y, Zhu Y. The prevalence and awareness of migraine among university students in Harbin, China. J Oral Facial Pain Headache. 2015;29(4):384–389. doi:10.11607/ofph.1521
28. Cheung RT. Prevalence of migraine, tension‐type headache, and other headaches in Hong Kong. Headache. 2000;40(6):473–479. doi:10.1046/j.1526-4610.2000.00071.x
29. Lipton RB, Dodick D, Sadovsky R, et al. A self-administered screener for migraine in primary care: the ID Migraine™ validation study. Neurology. 2003;61(3):375–382. doi:10.1212/01.WNL.0000078940.53438.83
30. Wang X, San Y, Sun J, et al. Validation of the Chinese version of ID-migraine in medical students and systematic review with meta-analysis concerning its diagnostic accuracy. J Oral Facial Pain Headache. 2015;29(3):265–278. doi:10.11607/ofph.1341
31. Lapworth T, Cook D. Nursing & Health Survival Guide: Clinical Assessment. Routledge; 2014.
32. Rist PM, Buring JE, Kurth T. Dietary patterns according to headache and migraine status: a cross-sectional study. Cephalalgia. 2015;35(9):767–775. doi:10.1177/0333102414560634
33. Zebenholzer K, Frantal S, Pablik E, et al. Reliability of assessing lifestyle and trigger factors in patients with migraine–findings from the PAMINA study. Eur J Neurol. 2016;23(1):120–126. doi:10.1111/ene.12817
34. Gu X, Xie Y. Migraine attacks among medical students in Soochow University, Southeast China: a cross-sectional study. J Pain Res. 2018;11:771–781. doi:10.2147/JPR.S156227
35. DeVon HA, Block ME, Moyle‐Wright P, et al. A psychometric toolbox for testing validity and reliability. J Nurs Scholarsh. 2007;39(2):155–164. doi:10.1111/j.1547-5069.2007.00161.x
36. Roach KE. Measurement of health outcomes: reliability, validity and responsiveness. JPO. 2006;18(6):8–12.
37. Al-Hashel JY, Ahmed SF, Alroughani R, Goadsby PJ. Migraine among medical students in Kuwait University. J Headache Pain. 2014;15(1):26. doi:10.1186/1129-2377-15-26
38. Terwindt G, Ferrari M, Tijhuis M, Groenen S, Picavet H, Launer L. The impact of migraine on quality of life in the general population: the GEM study. Neurology. 2000;55(5):624–629. doi:10.1212/WNL.55.5.624
39. Sawatzky R, Ratner PA, Johnson JL, Kopec JA, Zumbo BD. Self-reported physical and mental health status and quality of life in adolescents: a latent variable mediation model. Health Qual Life Outcomes. 2010;8(1):17. doi:10.1186/1477-7525-8-17
40. The Nursing Council of Hong Kong Kong. A reference guide to the syllabus of subjects and requirements for the preparation of registered nurse (general) in the Hong Kong Special Administrative Region. Available from: http://www.nchk.org.hk/filemanager/en/pdf/syllabus_of_subjects_MS.pdf.
41. Adoukonou T, Tognon-Tchegnonsi F, Philomène K, Alabi A, Houinato D, Preux P-M. Prevalence of migraine among university students at Parakou, Benin: a cross-sectional study. World J Neurosci. 2014;4(1):18. doi:10.4236/wjns.2014.41003
42. Menon B, Kinnera N. Prevalence and characteristics of migraine in medical students and its impact on their daily activities. Ann Indian Acad Neurol. 2013;16(2):221. doi:10.4103/0972-2327.112472
43. De Vries B, Frants RR, Ferrari MD, van den Maagdenberg AM. Molecular genetics of migraine. Hum Genet. 2009;126(1):115. doi:10.1007/s00439-009-0684-z
44. Gardner KL. Genetics of migraine: an update. Headache. 2006;46:S19–S24. doi:10.1111/j.1526-4610.2006.00486.x
45. Johnson H, Guhl G, Arora J, Walling A. Migraine in students of a US medical school. Fam Med. 2014;46(8):615–619.
46. Nandha R, Chhabra M. Prevalence and clinical characteristics of headache in dental students of a tertiary care teaching dental hospital in Northern India. Int J Basic Clin Pharmacol. 2013;2(1):51–55. doi:10.5455/2319-2003.ijbcp20130110
47. Yazdanparast M, Abrishamizadeh AA, Mahboobi H, et al. Prevalence of and factors associated with migraine in medical students at BandarAbbas, Southern Iran, in 2012. Electron Physician. 2013;5(3):679. doi:10.14661/2013.679-684
48. Ojini FI, Okubadejo NU, Danesi MA. Prevalence and clinical characteristics of headache in medical students of the University of Lagos, Nigeria. Cephalalgia. 2009;29(4):472–477. doi:10.1111/j.1468-2982.2008.01766.x
49. Suen LK, Hon KL, Tam WW. Association between sleep behavior and sleep-related factors among university students in Hong Kong. Chronobiol Int. 2008;25(5):760–775. doi:10.1080/07420520802397186
50. Friedman DI, De Ver Dye T. Migraine and the environment. Headache. 2009;49(6):941–952. doi:10.1111/j.1526-4610.2009.01443.x
51. Galinović I, Vuković V, Trošelj M, Antić S, Demarin V. Migraine and tension-type headache in medical students: a questionnaire study. Coll Antropol. 2009;33(1):169–173.
52. Environmental Protection Department. An overview on noise pollution and control in Hong Kong. Available from: http://www.epd.gov.hk/epd/tc_chi/environmentinhk/noise/noise_maincontent.html.
53. Ravishankar K. Barriers to headache care in India and efforts to improve the situation. Lancet Neurol. 2004;3(9):564–567. doi:10.1016/S1474-4422(04)00855-5
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
