Back to Journals » International Journal of Women's Health » Volume 8
Middlemore Hospital experience with tubo-ovarian abscesses: an observational retrospective study
Authors Habboub A
Received 5 February 2016
Accepted for publication 10 June 2016
Published 22 July 2016 Volume 2016:8 Pages 325—340
DOI https://doi.org/10.2147/IJWH.S105913
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Antoine Youssef Habboub
Middlemore Hospital, Counties Manukau District Health Board, Auckland, New Zealand
Aim: The aim of this paper was to study the characteristics of patients presenting to Middlemore Hospital with tubo-ovarian abscess (TOA) and to compare the outcomes of conservative medical management versus medical management with surgical drainage and medical management with radiological drainage.
Methods: All patients admitted with a radiologically or surgically proven TOA between January 01, 2008 and December 31, 2010, were included and followed up until June 30, 2011. The total number of patient/index admission was 174.
Results: The mean age of patients was 37.8 years. One hundred thirty patients had medical treatment only with hospitalization and antibiotics, and 44 patients were managed with antibiotics and surgical drainage. Complete resolution of TOA was 77.3% (99/128) for patients managed medically and 93.2% (41/44) for patients managed surgically. When the two groups were compared, patients who were managed surgically were more likely to have complete resolution of TOA within 6 months of index admission with an odds ratio (OR) of 4 and a P-value of 0.029. There was no statistically significant difference in the secondary outcomes namely of readmission with TOA (OR: 0.47) and the need for repeat surgical or radiological drainage (OR: 1.48). Nonetheless, the relative duration of hospitalization was longer for the surgical group with a P-value of <0.0001. The C-reactive protein and the size of TOA were the significant factors involved in the resolution of TOA.
Conclusion: The results of this study confirmed our initial hypothesis that we should consider surgical drainage more often, probably earlier, especially for the younger patients still desiring fertility preservation and for larger abscesses. Laparoscopic surgical drainage is safe and could be used as the procedure of choice. Conservative medical management is still acceptable with good cure rates of 77%. C-reactive protein and the size of the abscess were the important factors to consider when managing patients with TOA.
Keywords: tubo-ovarian abscess, pelvic inflammatory disease, antibiotics, surgical drainage
Introduction
Tubo-ovarian abscess (TOA) is a serious complication of pelvic inflammatory disease (PID). It occurs usually in women aged 20–49 years and carries a significant risk of morbidity, occasional mortality, and long-term sequelae, which may include chronic pelvic pain and infertility. Treatment of TOA historically was surgical, with most women having radical surgery with total abdominal hysterectomy (TAH) and bilateral salpingo-oophorectomy (BSO).1 Management of TOA has changed drastically in the past 4 decades with the advent of broad-spectrum antibiotics and continues to evolve with improved imaging and drainage techniques. Studies have demonstrated an overall 16%–95% success rate with conservative medical management, with the majority of studies demonstrating a success rate of ≥70%.1 Current practice is to start with broad-spectrum intravenous (IV) antibiotics for 48–72 hours and then resort to surgical or interventional radiology drainage, should no significant improvement be noted.1–3 Surgical and/or radiological drainage has been shown in recent studies to decrease the hospitalization period and rehospitalization with the same complaint within 3 months.4 Early resort to drainage has also been shown to hasten resolution of TOA and decrease scarring of pelvic organs and the long-term sequelae, especially for women with a desire for fertility preservation.5 The size of TOA should be taken into consideration when managing patients with large TOA (>10 cm) and early resort to drainage is advisable.
An audit at Middlemore Hospital conducted prior to this study had found a high incidence of recurrent admissions for patients with TOA. We therefore hypothesized that our department may have not been resorting to surgical drainage of TOAs as often as was ideally required; hence, this study aims to further investigate this issue.
Methods
This was a retrospective cohort study; all patients admitted with the diagnosis of TOA to Middlemore Hospital between January 01, 2008, and December 31, 2010, were included and were followed up until June 30, 2011. TOAs were coded as follows:
- N700: acute salpingitis and oophoritis,
- N701: chronic salpingitis and oophoritis,
- N709: salingitis and oophoritis unspecified.
The data of 277 patients were therefore reviewed. An application was lodged with the study protocol to the Northern Regional Health and Disability Ethics Committee with approval number NTX/11/EXP/078, dated April 26, 2011. The ethics committee also deemed that written patient consent was not needed as this was a retrospective study. Data were collected from individual patient’s notes, patient’s information systems including Concerto, and in certain instances general practitioners and/or patients were directly contacted to complete missing information. The National Health Index was used to identify individual patients and to follow them up, but another identifying number was assigned to each patient for confidentiality purposes. Covariate data recorded included demographic factors, risk factors, and clinical factors as described below:
- Demographic factors: age, marital status, gravidity, and parity.
- Risk factors (at time of index admission): self-reported sexually active status, history of current or previous PID/sexually transmitted disease (STD), recent insertion or removal of intrauterine device (IUD) (within 3 months), prolonged use of IUD (>5 years), and recent pelvic surgery (within 6 weeks).
- Clinical factors (at time of index admission): abdominal pain, vaginal discharge, fever, cervical motion tenderness, adnexal tenderness, white blood cell (WBC) and neutrophil counts, C-reactive protein (CRP), Chlamydia status on cervicovaginal swabs/urine, gonorrhea status on cervicovaginal swabs, bacterial vaginosis (BV) status on cervicovaginal swabs, bacterial culture when applicable, radiological diagnosis ultrasound scan (USS) or computer tomography (CT) scan or both, magnetic resonance imaging (MRI), unilaterality or bilaterality of TOA, and size of TOA.
- Management factors: duration of IV/oral antibiotics, duration of hospitalization, and management plan (medical, surgical, or interventional radiology). The following supplementary data were collected conditionally on the management strategy level:
- Medical management:
- Surgical management: team performing surgery (general surgery/obstetrics and gynecology; Obstetrics and Gynecology), type of surgery (laparoscopy or laparotomy), actual procedure (drainage only versus drainage and excision), surgical complications (primary surgery versus surgery after failure of medical or interventional radiology).
- Interventional radiology: type of drainage A (aspiration versus aspiration and drain placement), type of drainage B (CT versus USS drainage), site of drainage (transvaginal, transgluteal, or transabdominal), number of interventions, and complications.
Primary endpoint
Primary endpoint includes the clinical and radiological resolutions of TOA within 6 months of index admission with TOA.
Secondary endpoints
Secondary endpoints include duration of hospitalization, duration of IV and oral antibiotics, and readmission with the same complaint, repeat interventional radiology drainage, and repeat surgical intervention within 6 months of index admission with TOA.
Statistical analysis plan
Baseline characteristics were summarized according to mean and standard deviation, as well as median and interquartile range, for continuous covariates. Proportions were reported for categorical covariates.
Logistic regression was used to obtain odds ratios (ORs) for the outcomes considered associated with each management strategy. Propensity functions (Imai and van Dyk, 2004) based on the other observed covariates were used to appropriately reweight the outcomes according to the management strategy. Outcomes within a given management strategy were analyzed using the strategy-specific data as covariates.
Times to event (secondary outcomes) were analyzed similarly using survival analysis tools, including Cox regression and nonparametric inferential methods.
All data were entered on an Excel spreadsheet, and analysis was performed using SAS Version 9.2 and R Version 2.12.
Results
Descriptive statistical analysis
Of the 277 files reviewed, 158 patients fulfilled the inclusion criteria of the study, that is, those patients with either radiologically proven TOA or surgically proven TOA. Of those 158 patients, 15 patients represented after the follow-up period of 6 months with either a new TOA (three) or persistent and/or recurrent ipsilateral TOA (eleven, including one patient who had three index admissions over 18 months). The total number of patient/index admission with TOA was, therefore, 174. Two patients left the country after their index admission, could not be followed up, and were therefore removed from the assessment of primary and secondary outcomes but were included in the descriptive analysis. Early in the data analysis, we realized that there were only two cases that were managed with interventional radiology drainage and could not be set as a group apart; therefore, we decided that those two cases be included in the Medical Management Group for statistical purposes.
The mean age of patients in this study was 37.8 years, and 43% of patients were in the age group of 40–49 years, 20% were older than 30 years, and 6.9% of patients were older than 50 years. The mean gravidity was 2.55 and the mean parity was 1.82. One hundred sixteen (66%) patients were registered as married, 82% reported that they were sexually active, 37% had a prior history of PID/STD, two (1.1%) patients had a recent IUD inserted, 26 (15.1%) patients had prolonged use of IUD (>5 years), and 19 (10.9%) patients had recent pelvic surgery/intervention (Table 1).
Regarding clinical signs, 97.7% (170/174) of patients presented with abdominal pain, 33% (58/174) presented with abnormal vaginal discharge, and 48.3% (84/174) of patients presented with fever (Table 1).
Physical signs included abdominal tenderness 95.4% (166/174), cervical motion tenderness 32.2% (56/174), and adnexal tenderness 48.3% (84/174) (Table 1).
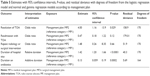
The mean WBC count was 16.1, and the mean neutrophil count was 13.4. The mean CRP taken for 144 patients was 152.6. The mean maximum size of the TOA was 7.2 cm with a right of 6.9 cm and a left of 6.8 cm (Table 2).
  | Table 2 Descriptive statistics of clinical measurements |
Diagnosis was confirmed at the time of surgery for 33 (18.9%) patients, by USS of pelvis for 147 (84.4%) patients, or by other radiological modalities including CT scan of abdomen and pelvis for 57 patients and MRI of pelvis for seven patients. Some patients had more than one imaging modality. Bilateral TOAs were found in 30.6% (53/173) of patients.
Ninety patients had negative cultures, and 80 patients had positive cultures with a mixture or a dominant pathogen (Table 3). Twenty-two patients had BV.
There were 130 patients who had medical treatment only (MP1) with hospitalization and IV antibiotics followed by oral antibiotics as per Middlemore Hospital guidelines for the management of PID/TOA and 44 patients who were managed with antibiotics and surgical drainage (MP2). This protocol for nonpregnant patients included cefoxitin 2 g IV q8h, doxycycline 100 mg BD PO 14 days, metronidazole 400 mg BD PO 14 days, and gentamycin if not settling after 24–48 hours for patients not allergic to penicillin and clindamycin 450–600 mg IV q8h, gentamycin 5 mg/kg (ideal body weight) IV daily followed by doxycycline 100 mg BD PO 14 days, and metronidazole 400 mg BD PO 14 days for patients with severe allergy to penicillin.
Forty-five (25.8%) patients did not have antibiotics according to protocol; of these patients, most of them had cefuroxime or augmentin (amoxicillin and clavulinic acid) instead of cefoxitine or had another combination of antibiotics as advised by infectious disease team.
Surgical procedures were done through laparoscopy for 23 of 44 patients and laparotomy for 21 of 44 patients with one case having a hymenotomy and drainage of an infected hematocolpos with TOA. Most laparoscopies (19/23) were performed by the general surgical team. Most laparotomies (11/20) were performed by the gynecological team. Procedures performed were lavage and drainage alone for 20 patients, excision for twelve patients, and appendicectomy for five patients. Five TAH and BSO were performed. No significant complications were noted for laparoscopies except one case of pulmonary embolus and one case of prolonged ileus. Laparotomies were associated with more complications including wound infection and dehiscence in six cases, two bowel injuries and two ureteral injuries, and one case of pneumonia likely due to sepsis (Table 4).
Patients were followed up for 6 months. Of the 128 patients who had medical management (MP1), patients excluding the two patients lost to follow-up, 99 (77.3%) patients had complete resolution of TOA and 29 (22.6%) patients had no resolution of TOA within 6 months of index admission. Of the 44 patients who had surgical management (MP2), 41 (93.2%) patients had complete resolution of TOA and only three (6.8%) patients had no resolution by the end of the 6 months following the index admission. Unfortunately, only 22.2% (38/172) of our study group had an imaging modality to confirm radiological resolution. Nonetheless, those patients and/or their general practitioners were contacted confirming the complete clinical resolution of their symptoms. Some of them even opted not to have the follow-up imaging and/or the clinical follow-up. Instead of excluding those patients from the study, we decided to keep them and consider that since those patients had no further complaints relating to their TOAs, we could also presume that those patients had complete radiological resolution. This could probably be the most important limitation of this study.
The mean overall duration of IV antibiotics was 4.5 days, and the mean overall duration of oral antibiotics was 20.1 days. The overall mean duration of hospitalization was 6 days. The overall duration of IV antibiotics was 4.3 days for medical management and 4.9 days for surgical management. The overall duration of oral antibiotics was 21.7 days for medical management and 15.4 days for surgical management. Hospitalization duration was 7.6 days for surgical management and 5.3 days for medical management.
Overall, 38 (21.8%) patients were readmitted with TOA within 6 months of index admission, of whom 32 of 130 (24%) patients were from the medical management group (MP1) and six of 44 (13.6%) patients were from the surgical treatment group (MP2). Overall, three of the 174 (1.7%) patients needed subsequent radiological drainage; all patients were from the medical management group. Overall, three of the 174 patients needed subsequent/repeat surgical intervention, of whom one patient was from the medical management group and two patients were from the surgical management group.
Inferential statistical analysis
When the surgical management group (MP2) was compared with the medical management group (MP1), it appeared that patients who were managed surgically were more likely to have complete resolution of TOA within 6 months of index admission with an OR of 4 and a P-value of 0.029, which is statistically significant. There was no statistically significant difference in the secondary outcomes namely of readmission with TOA (OR: 0.47) and the need for repeat surgical or radiological drainage (OR: 1.48). Nonetheless, the relative duration of hospitalization was longer for the surgical group (MP2) with a P-value of <0.0001. The relative duration on antibiotics was shorter for the surgical group (MP2), with a statistically significant additive duration and P-value of 0.0002 (Table 5).
Several models were fitted on each group of the clinical factors, and further analyses were carried out on the resolution of TOA outcome only.
CRP and the size of the TOA were found to be significant factors in the resolution of the TOA within 6 months of index admission. Every unit increase in the CRP increased the chance of resolution of TOA by ~10%; this was not very well understood but may likely be due to the fact that patients who had raised CRP were more likely to have surgery, although this was barely statistically significant with a P-value of 0.037. The size of the TOA was also a significant covariate; with every increase of 1 cm in the overall size of the TOA, there was a 23% reduction in the resolution of TOA (Table 6).
Patients with larger TOA size were more likely to be readmitted to hospital within 6 months of index admission (OR: 1.2 [1.04–1.39] and P-value 0.02) (Table 7).
Every unit increase in the CRP count was noted to be associated with ~2% reduction in the repeat surgical or radiological drainage of TOA (Table 8).
Gamma regression analysis was carried out on the duration of hospital stay by age group. Comparison was made in the younger age group patients aged <30 years, and this was found to be statistically significant at the 10% level. This indicated that the older the patient was, the more likely she would have to stay longer when compared with the younger group of patients aged <30 years (Table 9, Model 10).
It appeared that patients who reported to be sexually active were more likely to have shorter hospital stay after adjusting for all age groups (Table 9, Model 1). Patients who had fever were more likely to have a longer hospital stay (Table 9, Model 5). Patients with a higher CRP were more likely to have longer hospital stay. Every unit rise in the CRP count increased hospital stay by ~0.2% (Table 9, Model 6). Patients with bilateral TOA compared to those with unilateral TOA were more likely to have a longer hospital stay (Table 9, Model 8). The size of the TOA was also an important covariate influencing hospital stay; in fact, with every 1 cm increase in the size of TOA, there was ~6% increase in the duration of hospitalization. In other words, with every 2 cm increase in the size of the TOA, the duration of hospitalization was increased by 1 day (Table 9, Model 9).
Normal regression was carried out on the duration of antibiotics according to age group at index admission. The age category was found to be not significant at the 10% level, and it was not included in all the analyses of the outcome. Patients who were sexually active were noted to be more likely to have a shorter duration of antibiotics (P-value =0.0002) when compared with those who were not sexually active. In addition, patients who presented with abdominal pain were more likely to have a shorter duration of antibiotic treatment (P-value =0.015) when compared with those who had no pain on admission. Patients who presented with fever were more likely to have a longer duration of antibiotics (P-value =0.0033) when compared with those who had no fever. Again those patients with higher CRP count and those patients with larger size TOA were more likely to have a longer antibiotic treatment, with the P-values of 0.0096 and 0.009, respectively.
Discussion and review of literature
PID usually occurs because of an ascending infection affecting the uterus (endometritis and myometritis), fallopian tubes (salpingitis) and surrounding structures, ovary (oophoritis), broad ligaments (parametritis), and abdomen (peritonitis). The anatomy of the abdomen is significant in the development of PID and sepsis. In men, the peritoneal cavity is a closed cavity. In contrast, in women, the peritoneal cavity is perforated by the free ends of the fallopian tubes.6 Peritoneal reflections and mesenteric attachments compartmentalize the intraperitoneal space and facilitate the spread of exudates to sites that are often distant leading to more risk of disseminated peritoneal infection compared to men.6 One in ten women suffers from PID during her reproductive years.7 Approximately 60% of PID cases may be triggered by a sexually transmitted infection (STI), such as chlamydia, gonorrhea, or Mycoplasma genitalium, and ~30% are not caused by an STI.1,8 There is also a known association between BV and PID.9 Because of varying degrees of clinical appearance and the lack of specific laboratory tests, medical therapy is often delayed and almost one in four women with PID experiences long-term sequelae, such as chronic abdominal pain, ectopic pregnancy, and infertility.7 It has been demonstrated that no single subjective complaint, physical examination finding, or laboratory test is highly sensitive or specific for the diagnosis of PID. Thus, the diagnosis of PID requires careful consideration of the combination of patient’s risk factors, physical examination findings, laboratory findings, and overall clinical presentation. Because of this, the diagnosis of PID is imprecise with the clinical diagnosis of PID having a positive predictive value of 65%–90% in even the most experienced practitioners’ hands.1 That is why the US Center for Disease Control and Prevention recommends a low threshold for treating patients if they are at risk of PID and if on physical examination they exhibit any signs of uterine, adnexal, or cervical tenderness without other apparent causes.10 If PID is inadequately treated a pelvic abscess, typically a TOA develops. TOAs are generally reported as complicating 10%–15% of hospitalized cases of PID.7,11 TOA is the most common cause of an intraabdominal abscess in premenopausal women.12
Risk factors for TOA are similar to those of PID and include a previous history of PID, multiple sexual partners, IUD, and immunosuppression.7 In our study, two patients with TOA had a recent IUD insertion and 15.1% (26/174) of patients had prolonged use of IUCD for >5 years. The percentage of IUD users diagnosed with TOA ranges from 20% to 54%.7 It is well known in the literature that recent insertion of IUD is associated with a short-term increased risk of PID.6 A recent Swedish study has demonstrated that the use of a copper IUD for a period of >5 years may be a risk factor for TOA, therefore challenging the current Swedish Medical Products Agency recommendation that a woman nearing her reproductive phase could safely use the same IUD for a period of >5 years.13,14
The mechanisms by which TOAs are formed have been difficult to establish due to various presentations and degrees of tubo-ovarian damage present when the infection is diagnosed. It seems clear that TOAs are often the consequence of PID. However, in many women with TOA, no symptoms or signs of STI/STD can be traced.7 In our study, only 12 patients had chlamydia and only two patients had gonorrhea present in their genital tract. It has been suggested that the initial step in the formation of TOA is damage and necrosis of fallopian tube epithelium by a pathogen usually an anaerobic bacterium, thereby establishing a favorable environment for anaerobic invasion and growth. The destruction of the fallopian tube results in the production of purulent exudates.7,11 After a while, the ovary becomes involved in the inflammation. The abscess may also engage neighboring structures, such as bowel, bladder, and the contralateral fallopian tube and ovary. If the inflammation is not stopped, tissue planes are lost and the identification of pelvic structures and organs becomes difficult. At this stage, rupture of the abscess may occur, causing life-threatening peritonitis.7 Other complications may include small bowel obstruction15,16 and bowel perforation especially involving the sigmoid colon.17
In our study, seven patients had recent removal of IUD, four patients had a recent hysteroscopy dilatation and curettage, two patients had a recent vaginal delivery, one patient had a recent pipelle biopsy, and one patient had a recent oocyte retrieval for IVF. Surgical procedures of the female genital tract, abdominal, or vaginal, place the patient at increased risk for PID, with ~15% of pelvic infections occurring after procedures that break the cervical mucus barrier.18,19 Such infections have been reported after dilatation and curettage,18,19 oocytes vaginal retrieval for IVF,19,20 Essure insertions even few years later with Essure acting either as a nidus or as a conduit for infection,21 and pipelle sampling.19
TOA can also be secondary to an infection by contiguity originating in the small bowel secondary to Crohn’s disease,22 or in the appendix with acute appendicitis, subsequent perforation, and periappendiceal abscess formation that would later involve the adjacent right ovary and tube.23 The infection could also originate in the large bowel with diverticulitis and abscess formation involving especially the left ovary being very close to the sigmoid colon where most diverticulae occur.5,24 Occasionally, the infection could involve the upper gastrointestinal tract with one case of TOA in the literature due to a perforated peptic ulcer.25
The infection could also be due to hematogenous spread such as Mycobacterium tuberculosis; we had two cases in our study. There are reported cases in the literature of TOA due to Pasteurella mutocida secondary to bacteremia from cat scratch disease.26 We also had one case with the same bacterium.
Complications of abdominal and pelvic malignancy can also lead to a TOA.26 In our study, one patient had a TOA with lymphoma and another patient had a TOA with a serous ovarian carcinoma.
The mean age of patients presenting with TOA was 37.8 years with ~43% in the age group of 40–49 years and 6.9% in the age group of >50 years, which is similar to that found in the study of Halperin et al conducted in Israel. It seems that our study likewise indicates a change in the epidemiology of TOA.27 In Halperin et al’s27 study, the older group of patients had a more aggressive disease likely explained by more aggressive microorganisms and/or by the delay in diagnosis and treatment of PID. In our study, patients older than 40 years had longer hospital stay compared to patients younger than 30 years. And patients who were sexually active, usually younger, had shorter hospital stay, which again may be similar to the findings by Halperin et al, although our studies’ aims and analyses were different. Demitras et al28 also found a mean age for patients with TOA of 41.4 years.
In our study, 90 patients had negative cultures and 80 patients had positive cultures with a mixture or a dominant pathogens (Table 3). Twenty-two patients had BV. Two patients had tuberculosis. Two patients had Streptococcus pneumoniae TOA, which is unusual but has also been reported by Seshadri et al.29 Actinomyces species that are usually associated with long-term IUD use7 were present in six of our patients, of whom four of them were associated with prolonged IUD use. Two principles are essential for the understanding of the pathogenesis of female genital tract infections. The first one is that except for a few microorganisms, such as group A β-hemolytic Streptoccocus, Chlamydia trachomatis, and Neisseria gonorrhea, the pathogens causing genital tract infections arise from the microflora of the vagina and cervix. The second principle is that pelvic infections are usually of polymicrobic etiology.7 The microbial content of TOA is usually a mixture of anaerobic, aerobic, and facultative microorganisms. Anaerobic bacteria are isolated in >50%. Some microorganisms frequently cultured include Escherichia coli (37%), Bacteroides fragilis (22%), various Bacteroides species (26%), peptostreptococci (18%), and peptococci (11%).7
Patients typically present with lower abdominal pain 98% (97.7% in our study), with or without fever and chills 50% (48% had fever in our study), with a history of previous PID/STD ~50% (37% in our study), and with abnormal vaginal discharge 28% (33% in our study).7 Abdominal examination commonly elicits lower abdominal tenderness with or without guarding (96% in our study). Vaginal examination often demonstrates mucopurulent cervicovaginal discharge, cervical motion tenderness (32% in our study), and adnexal tenderness (48% in our study) with sometimes the suspicion of an adnexal mass, which is difficult to ascertain when usually the pain precludes an adequate bimanual examination.7
In our study, the mean WBC count was 16.1 and the mean neutrophil count was 13.4. The mean CRP taken for 144 patients was 152.6 (Table 2). Laboratory tests in patients with TOA usually show an elevated WBC count and neutrophil count with also elevated inflammatory markers, including erythrocyte sedimentation rate, CRP, and pentraxin 3 (PTX3), which is a novel acute inflammatory protein secreted by macrophages, dendritic cells, monocytes, smooth muscle cells, fibroblasts, and epithelial cells.8 Demirtas et al28 have indicated in their study that CRP values were observed to have a statistical significance in the diagnosis of an abscess, whereas the leukocyte count did not. CRP had a diagnostic value of 73% with a specificity of 83% and a sensitivity of 79% based on a cutoff value of 11.5 mg/L on the other hand, and because of the low diagnostic value of the leukocyte count, a cutoff value could not be specified.28 Güngördük et al3 found that at a cutoff of ≥21 mg/L CRP had a diagnostic value of 80.4% with a specificity of 82.3% and a sensitivity of 65.8%. Erythrocyte sedimentation rate was requested only for a few patients in our study, and most of our patients had CRP instead. PTX3 is a test that is not yet available in New Zealand, but it appears from Chang et al study that this test has higher sensitivity (84.38%) and lower false negative rates (15.63%) when compared to CRP for the diagnosis of severe PID and TOA.8 Patients with TOA usually have higher plasma levels of PTX3 when compared to patients with PID without TOA. There are other markers of inflammation mentioned in the literature, such as osteopontin, neutrophil gelatinase-associated lipocalin, and YKL-40, whose levels also correlate with the severity of PID and TOA, and these are beyond the scope of this study.28,30 The high level of CRP was associated with longer duration of hospitalization and disease severity.28 This was also echoed in our study; patients with a higher CRP were more likely to have longer hospital stay. Every unit rise in the CRP count increased hospital stay by ~0.2% (Table 9, Model 6). Nonetheless, it was also demonstrated in our study that every unit increase in the CRP increases the chance of resolution of TOA by ~10%, this was not very well understood but may likely to be due to the fact that patients who had raised CRP were more likely to have surgery, although this was barely statistically significant with a P-value of 0.037. Again those patients with higher CRP count and those with larger size TOA were more likely to require a longer antibiotics treatment with the P-values of 0.0096 and 0.009, respectively (Table 9). Every unit increase in the CRP count was noted to be associated with ~2% reduction in the repeat surgical or radiological drainage of TOA. Vaginal wet smears have been evaluated in the literature to have a high sensitivity for PID/TOA (87%–91%) if three or more WBC were seen per high-power field with a negative predictive value of 94.5% if none is seen;1 this was not evaluated in our study.
Most of our patients (84%) had an USS pelvis, which in most cases was a combination of transabdominal and transvaginal scanning with the use of Doppler studies: 57 patients had a CT scan and seven patients had an MRI scan. Pelvic USS is the initial modality of choice for assessing patients with suspected PID/TOA with a diagnostic sensitivity of 56%–93% and a specificity of 86%–98%.12,31–36 MRI has a diagnostic sensitivity of 100% and a specificity of 90%, which is superior to that of USS.31,34 CT scan is generally not indicated for differential diagnosis of pelvic masses because of poor soft tissue discrimination except for fatty tissue and calcification and the disadvantages of irradiation. In our study, most CT scan would have been requested by the general surgical team or by the gynecology team when complications of TOA, for example, TOA rupture was suspected.
Ultrasonography is most useful for differentiating TOA from other stages of PID. In PID, the most common sonographic findings include thickened, heterogeneous endometrium, an enlarged uterus with fluid in the cavity and fluid-filled fallopian tubes.32 The next step is a tubo-ovarian complex, which is a pelvic inflammatory mass without any collection of pus within a cavity, in which edematous, adherent, infected ovaries, and tubes can still be visualized but cannot be separated by an endovaginal probe. In TOA, there is a loss of normal boundaries between the fallopian tube and ovary due to pus-filled, edematous-inflamed tissue. A variety of sonographic appearances result, as described by Timor-Tritsch et al, as presented in the paper by Adhikari et al.32 The typical sonographic appearance of a TOA is a complex adnexal mass of varying echogenicity with debris, septations, and irregular margins. The other sonographic markers of TOA are pyosalpinx and loculated or speckled, echogenic fluid in the cul-de-sac.32,33,36 Thickening of uterosacral ligament is visible when inflammation extends posteriorly, internal gas bubbles, strong indicators of TOA, are rarely seen, and the rectosigmoid and the ureter are the most common organs that can be involved with TOA.36 The MRI appearance of TOA is described as a thick-walled adnexal mass with low signal intensity contents on T2-weighted images. However, this appearance is variable; there are cases of TOA demonstrating intense or increased signal intensity on T1-weighted images, and some have heterogeneous signal intensity on T2-weighted images.35 In our study, we aimed to include patients with a radiologically/ultrasonographically proven TOA, but in fact there is no such entity of a radiologically proven TOA; the diagnosis of TOA is more complex than that and should be based on history and physical examination and aided by laboratory findings and medical imaging.33,35 The ultrasonographic findings of TOA are not specific and could resemble and mimic or be mistaken for other cystic ovarian masses, including an endometrioma, hemorrhagic cyst, sebaceous dermoid, or some malignant ovarian neoplasms.35,37 Even with MRI and positron emission tomography scans, a TOA can be misdiagnosed as a pelvic malignancy. Rakheja et al35 reported on a case of 20 years old woman with an intensely F-FDG avid bilateral TOA mistakenly diagnosed as ovarian malignancy. This patient subsequently had an unnecessary BSO.
In our study, the diagnosis of TOA was confirmed by surgery, mainly laparoscopy, for ~18% of patients, laparoscopy being the gold standard for the diagnosis of TOA.32,33
In our study, conservative medical treatment including the two cases that had radiological drainage was successful in ~77%, which is in line with the majority of studies demonstrating a success rate of ≥70%.1 Moreover, it appears that in our institution, there was no differentiation in management for patients with unruptured TOA versus ruptured TOA. If a patient was well enough, medical treatment would be instituted first and surgery would be decided depending on worsening clinical signs and symptoms. Most TOAs respond well to broad spectrum IV antibiotics followed by oral antibiotics over a prolonged period of time. Triple antibiotic therapy, like the regimen used by us, seems to be the treatment of choice with a success rate varying between 16% and 95%.1,7
Historically, surgical management ranging from posterior colpotomy, transabdominal surgical drainage, and unilateral salpingo-oophorectomy to TAH and BSO in combination with antibiotics was performed in women with TOA. Although this approach offered high cure rates, it resulted in hormone deficiency and left women of child-bearing age without reproductive potential. In addition, due to the presence of friable inflammatory tissues and adhesions, surgery in this group of patients is often technically difficult and is associated with complications. Thus, Kaplan et al, as presented in the paper by Granberg et al reported that bowel injury occurred in 8.4% of the patients who underwent laparotomy.7 In our study, we had two bowel injuries with our 20 laparotomies, which is ~10% of our patients. Midline laparotomy is preferred over Pfannesteil incisions as the former allow surgeons to extend the incision cephalad to get better exposure, and retroperitoneal dissection may also be used as demonstrated by Sharma et al to avoid bowel injury.38
Posterior colpotomy is limited in that it is restricted to patients who meet the criterion of a fluctuant mass in the midline that dissects the rectovaginal septum. Additionally, it must be adherent to the parietal peritoneum. And given the complications rates and the limited patient selection, this approach should not be used in the management of TOA.5 None of our patients underwent this procedure.
Today the aim of surgical management is to be as minimally invasive and as conservative as possible. This means that when surgery is undertaken, lysis of adhesions, drainage of the abscess, excision of infected and necrotic tissues, and irrigation of the peritoneal cavity are usually conducted.7 In our study, this principle was generally followed, with procedures performed being drainage and lavage alone for 20 patients, excision for 12 patients, appendicectomy for five patients with TAH, and BSO performed on five patients (Table 4).
In our study, among the 23 patients managed by operative laparoscopy, there was only one complication, which was a pulmonary embolus, that again confirms, in line with the other studies, the safety of this type of procedure. In many centers, laparoscopy has been the gold standard for the diagnosis and treatment of TOA for many years.5,7,40–42 Yang et al42 recommend the use of Hasson open entry technique to minimize inadvertent injury to visceral organs. Henry-Suchet39 carried out laparoscopic adhesiolysis and drainage of abscess in combination with antibiotics in 50 women. In 45 patients (90%), the approach was successful, while 5% required further surgery. Similar to the study of Henry-Suchet,7,39 Reich et al, as presented in the paper by Buchweitz et al reported no complications following laparoscopic and organ-preserving management of TOA in 25 patients.41 In some studies, no drain is necessary after laparoscopic drainage.38 Buchweitz et al41 compared the intraoperative and postoperative safety and prospects of fertility in women who had laparoscopic incision of the abscess cavity and lavage only to women who had laparoscopic salpingectomy or salpingo-oophorectomy. They found that a significantly higher incidence of complications occurred when ablative treatment was performed when compared with organ-preserving surgery.41 Some of the complications noted with the ablative group were intestinal perforation, bowel serosal injury, greater omentum injury, lacerations of blood vessels collaterals of the internal iliac artery, bowel obstruction, deep venous thrombosis, and readmission with lower abdominal pain. There were more live term pregnancies in the drainage group compared to the ablation group with no ectopic pregnancies reported.7 In 1995, Raiga et al, as presented in the paper by Yang et al evaluated the effects on fertility with the use of laparoscopy in the treatment of TOA.42 All patients were treated with lysis of adhesions, drainage of purulent material, and irrigation with saline, and some patients needed further laparoscopic drainage with linear salpingotomies and/or fimbrioplasty to facilitate drainage of abscess. All patients had complete response, and 12% of patients needed further surgery at a later stage with up to 9 years of follow-up. The spontaneous pregnancy rate was 63%, and there was a tendency toward reduced adhesions on the second-look laparoscopies, which is likely attributed to the nearby healthy tissue having decreased exposure to necrotic and inflamed material. Hence, Rosen et al in 2009 recommended considering early/immediate laparoscopy to allow for accurate diagnosis and effective treatment under magnification, with minimal complications, with possibly faster response rates, with shorter hospitalization times, and with decreased infertility.5 Mitchell added that if active surgical management is not performed, there is a risk of rupture of TOA and life-threatening peritonitis, with medical management alone, which is ~3%–4%.5 Our study was not designed to look in particular at patients who had laparoscopy but combined also those who had laparotomy. Overall, 93.2% of our patients who had surgical management reported complete resolution, which is again in line with 90%–100% of initial response rate with the use of immediate laparoscopy reported by Mitchell et al. Patients who had surgical management in our study had longer hospital stay with shorter duration of antibiotics compared to the medical management group. We did not look at patients’ fertility post-TOA. However, we do share the opinion of Mitchell et al that we should resort more frequently to laparoscopy to manage patients with suspected TOA, and this study has demonstrated clearly that there are benefits to patients from this attitude. It is of note that most of our laparoscopies in this study were performed by the surgical team in their quest to rule out a perforated/inflamed appendix, and it appears that those patients may be considered lucky to have their TOA dealt with actively, with benefits in complete resolution, less days on antibiotics, possibly less scarring and adhesions, and fertility preservation for those who were still young and contemplating pregnancies.
Image-guided drainage in combination with antibiotics is the third modality of management of TOA. In our study, only two patients had primary transabdominal drainage of TOA: one patient was CT guided and one patient was USS guided and one patient had complete resolution and one patient did not. Three patients had secondary drainage, with all having no resolution after 6 months of index admission. During the past 2–3 decades, several studies have described image-guided drainage of pelvic abscesses with concomitant IV antibiotics to be an efficacious mode of treatment. Various approaches for abscess drainage have been reported, including transabdominal, transgluteal, transvaginal, and transrectal with the use of either computer tomographic guidance or ultrasonographic guidance. In a Norwegian study,43 published in 2005, by Gjelland et al involving 302 women with TOA, it was demonstrated that transvaginal needle aspiration of abscess content together with IV antibiotics was successful in 282 (93.4%) of the patients. In 20 women (6.6%), a laparoscopy or laparotomy was required. One hundred ninety-seven (65.2%) women had only one needle aspiration, 80 (26.5%) women needed two aspirations, and 15 (5%) women needed three aspirations, while at least ten (3.2%) women needed four aspirations. The success of the procedure was not affected by the size of the abscess or by its multilocularity. No procedure-related complications such as bowel injury were recorded.43
In another study by Goharkhay et al,4 the outcome of the treatment of TOA by image-guided drainage and IV antibiotics versus antibiotics alone, of the total of 58 patients, 50 patients were initially treated with IV antibiotics and eight patients had initial ultrasound-guided drainage and irrigation of abscess cavity with clindamycin. Complete response was noted in 29 (58%) patients treated with IV antibiotics alone. Failure to respond to IV antibiotics was related to the size of the abscess. All eight (100%) women who had primary drainage responded to treatment. Of the 21 women who failed medical treatment, two women underwent surgery and 19 women underwent salvage drainage with ultrasound guidance for eleven patients and CT guidance for eight patients. Eighteen of the 19 salvage drainage resulted in complete recovery. Patients with primary drainage group had shorter hospital stay and showed more rapid resolution of fever than women who had antibiotics only.4,13 Harisinghani et al44 in their study published in 2003 showed that the computer tomographic percutaneous transgluteal approach for drainage of deep pelvic abscesses with catheter placement was a safe and effective alternative to surgery for deep pelvic abscesses. One hundred thirty-four of 140 (96%) patients in their series had complete resolution of the abscess without subsequent surgery.44 It seems that this modality of management of TOA is underused in our institution, and we recommend that image-guided drainage be used more frequently to improve the outcome of patients as clearly demonstrated in the aforementioned studies.
Is TOA size associated with the duration of hospitalization and complications? In our study, the size of the TOA was a significant factor, and with every increase of 1 cm in the overall size of the TOA, there was a 23% reduction in the resolution of TOA. Patients with larger TOA size were more likely to be readmitted to hospital within 6 months of index admission (OR: 1.2 [1.04–1.39] and P-value 0.02). The size of the TOA was also an important factor influencing hospital stay; in fact, with every 1 cm increase in the size of TOA, there was ~6% increase in the duration of hospitalization. In other words, with every 2 cm increase in the size of the TOA, the duration of hospitalization was increased by 1 day (Table 9, Model 9), which is similar to that of Dewitt et al45 who demonstrated that with every 1 cm increase in the size of the abscess, there was an increase of hospitalization by 0.4 days. Again patient with larger TOA was more likely to require longer antibiotics treatment with the P-value of 0.009. Several authors have investigated the impact of TOA size on the outcome of antimicrobial therapy, the need for surgery, and the rate of surgery-associated complications. Reed et al, as presented in the paper by Goharkhay et al found surgery to be necessary in 60% of patients with a TOA size of >10 cm compared to 20% of those with a TOA size of <5 cm.3 Doganay et al46 reported that laparotomy was performed in 72% of patients with TOA diameter of >10 cm and in 26% of patients with an abscess diameter of <5 cm. Dewitt et al45 showed that abscesses of >8 cm required drainage or surgery more often than abscesses of smaller sizes and TOAs of >8 cm in size were associated with longer duration of hospitalization. Güngördük et al3 found that a TOA size of >7 cm was associated with adverse outcomes, including failed response to antibiotic therapy, longer duration of hospitalization, and higher risk of surgical complications. A TOA size of 6.5 cm predicted the need for surgery with a sensitivity of 77.6% and a specificity of 65.0%.3
In our study, 15 patients had endometriosis complicated by TOA who required surgery, ten patients had complete resolution within 6 months, and five patients needed surgery at a later stage, one patient needing bowel resection and permanent colostomy, and one ureter reimplantation, and another one bowel resection with reanastomosis. One patient had a very long and protracted course over almost 2 years. Of the 16 index readmissions after 6 months, nine index readmissions were for patients with endometriosis. Those patients with this combined pathology posed also a diagnostic dilemma with the endometrioma looking like TOA on USS and with pathological findings of Endometrioma without TOA in certain cases which may indicate either resolution of the infection prior to surgery or absence of TOA in the first place. The development of TOA in the context of pelvic endometriosis has been described by several authors,9,42,47–50 and may be due to increased susceptibility to infection particularly in the altered immune environment seen with endometrial glands and stroma although there are no epidemiologic data to support this theory.49 An endometrioma may become a nidus for infection especially with assisted reproductive technology; mainly Oocyte retrieval with inadvertent puncture of an endometrioma. Elizur et al49 found that women with endometriosis had more severe pelvic infection PID/TOA which was more refractory to conservative antibiotic treatment, often requiring surgical intervention. Elizur et al49 have also added that endometriosis is a risk factor for the development of severe PID/TOA, particularly after IVF treatment. Romero et al recommended vaginal douching with Povidone iodine followed by saline irrigation and adherence to strict aseptic technique to decrease the rate of infection for patients with endometriosis/endometrioma undergoing IVF treatment.50 Our study was not organized to look at this group of patients in particular. Nonetheless; with our limited analysis of those above cases, we do share the opinion of Elizur et al,49 about the severity and complexity of patients with TOA and endometriosis.
Conclusion
Our study showed that TOA is a complication of PID that affects the older gynecological patient and may have a pathophysiology that is different from that of PID with less involvement of the known STDs caused typically by chlamydia and gonorrhea. The diagnosis of TOA is complex and relies on history, physical examination, and laboratory tests including full blood count and CRP, which is aided by ultrasonography, CT scan and MRI and may also be ascertained by laparoscopy or laparotomy. CRP and the size of the TOA were the important prognostic factors to consider for the duration of hospitalization and the need for surgical and/or radiological drainage. Medical management alone was successful in 77% of patients, while medical and surgical drainage was superior with 93% success rate although the duration of hospitalization was longer for those who had surgery and the duration of antibiotic treatment was longer for the medical treatment group. Laparoscopic surgical drainage is safe and effective for the initial management of TOA. Radiological drainage was underused and could be resorted to more frequently to improve clinical outcome. TOA with endometriosis poses a diagnostic and therapeutic dilemma with a protracted and complicated course usually requiring definitive extirpative surgery. The major limitation of our study was the fact that it was a retrospective study and that at times proper follow-up was not arranged for all patients. Future prospective randomized studies may be able to better elucidate some of the issues raised in this study regarding, for example, the duration of hospitalization and the cost effectiveness of medical versus surgical management.
Acknowledgments
This study was supported by the Department of Obstetrics, Gynaecology, and Women’s Health, Middlemore Hospital, County Manukau District Health Board, Otahuhu, Auckland, New Zealand. The supervisor for this study was Lynsey Hayward, obstetrics and gynecology consultant at Middlemore Hospital. The study protocol was arranged with the assistance of Alain C Vandal, senior biostatistician at Center for Clinical Research and Effective Practice. Data analysis was performed by Christin Coomarasamy, data analyst, under the supervision of Vandal.
Disclosure
The author now works as an O&G Consultant at Waitemata District Health Board (WDHB); Waitakere Hospital, Auckland, New Zealand. The author reports no other conflicts of interest in this work.
References
Lareau SM, Beigi RH. Pelvic inflammatory disease and tubo-ovarian abscess. Infect Dis Clin North Am. 2008;22(4):693–708. | ||
Kuo CF, Tsai SY, Liu TC, Lin CC, Liu CP, Lee CM. Clinical characteristics and treatment outcomes of patients with tubo-obarian abscess at a tertiary care hospital in northern Taiwan. J Microbiol Immunol Infect. 2012;45(1):58–64. | ||
Güngördük K, Guzel E, Asicioğlu O, et al. Experience of tubo-ovarian abscess in western Turkey. Int J Gynaecol Obstet. 2014;124(1):45–50. | ||
Goharkhay N, Verma U, Maggiorotto F. Comparison of CT- or ultrasound-guided drainage with concomitant intravenous antibiotics vs. intravenous antibiotics alone in the management of tubo-ovarian abscesses. Ultrasound Obstet Gynecol. 2007;29(1):65–69. | ||
Rosen M, Breitkopf D, Waud K. Tubo-ovarian abscess management options for women who desire fertility. Obstet Gynecol Surv. 2009;64(10):681–689. | ||
Dulin JD, Akers MC. Pelvic inflammatory disease and sepsis. Crit Care Nurs Clin North Am. 2003;15(1):63–70. | ||
Granberg S, Gjelland K, Ekerhovd E. The management of pelvic abscess. Best Pract Res Clin Obstet Gynaecol. 2009;23(5):667–678. | ||
Chang CC, Wang PH, Su PH, et al. Significant elevation of plasma pentraxin 3 in patients with pelvic inflammatory disease. Clin Chem Lab Med. 2011;49(10):1655–1660. | ||
Kavoussi SK, Pearlman MD, Burke WM, Lebovic DI. Case report: endometrioma complicated by tubo-ovarian abscess in a woman with bacterial vaginosis. Infect Dis Obstet Gynecol. 2006;2006:84140. | ||
Crossman SH. The challenge of pelvic inflammatory disease. Am Fam Physician. 2006;73(5):859–864. | ||
Dogan E, Altunyurt S, Altindag T, Onvural A. Case report: tubo-ovarian abscess mimicking ovarian tumor in a sexually inactive girl. J Pediatr Adolesc Gynecol. 2004;17(5):351–352. | ||
Zeger W, Holt K. Gynecologic infections. Emerg Med Clin North Am. 2003;21(3):631–648. | ||
Charonis G, Larsson PG. Prolonged use of intrauterine contraceptive device as a risk factor for tubo-ovarian abscess. Acta Obstet Gynecol Scand. 2009;88(6):680–684. | ||
Bandyopadhyay S, Sinha S, Wui Chien PF, Fleming D. Diagnostic dilemma posed by severe pelvic actinomycosis associated with prolonged use of copper intrauterine device. Clin Pract. 2011;1(4):e112. | ||
Harel Z, Tracy TFJ, Bussey JG. Communication in brief: small bowel obstruction in an adolescent with pelvic inflammatory disease due to Chlamydia trachomatis. J Pediatr Adolesc Gynecol. 2003;16(3):125–128. | ||
Pines G, Klein Y, Ben-Arie A, Machlenkin S, Kashtan H. Small bowel obstruction due to tubo-ovarian abscess. Isr Med Assoc J. 2008;10(6):481–482. | ||
Prakash RK, Shah N, Ferguson DR. Image of the month. A tubo-ovarian abscess that perforates the sigmoid colon. Clin Gastroenterol Hepatol. 2010;8(6):A26. | ||
Weledji EP, Elong F. Small bowel obstruction and perforation attributed to tubo-ovarian abscess following ‘D’ and ‘C’. World J Emerg Surg. 2013;8(1):41. | ||
Terao M, Koga K, Fujimoto A, et al. Factors that predict poor clinical course among patients hospitalized with pelvic inflammatory disease. J Obstet Gynaecol Res. 2014;40(2):495–500. | ||
Hoecke FV, Beuckelaers E, Lissens P, Boudewijns M. Actinomyces urogenitalis bacteremia and tubo-ovarian abscess after in vitro fertilization (IVF) procedure. J Clin Microbiol. 2013;51(12): 4252–4254. | ||
Solt I, Loffe Y, Elmore RG, Solnik J. Group A streptococcal peritonitis and ruptured tubo-ovarian abscess three years after essure(R) insertion: a case report. J Womens Health (Larchmt). 2011;20(5):781–783. | ||
Hartmann KA, Lerand SJ, Jay MS. Tubo-ovarian abscess in virginal adolescents: exposure of the underlying etiology. J Pediatr Adolesc Gynecol. 2009;22(3):e13–e16. | ||
Vyas RC, Sides C, Klein DJ, Reddy SY, Santos MC. The ectopic appendicolith from perforated appendicitis as a cause of tubo-ovarian abscess. Pediatr Radiol. 2008;38(9):1006–1008. | ||
Metz Y, Nagler J. Diverticulitis presenting as a tubo-ovarian abscess with subsequent colon perforation. World J Gastrointest Surg. 2011;3(5):70–72. | ||
Su HY, Liu JY, Chen CH. Pelvic inflammatory disease with perforated peptic ulcer mimicking tubo-ovarian abscess. Int J Gynaecol Obstet. 2005;88(3):329–330. | ||
Gensheimer WG, Reddy SY, Mulconry M, Greves C. Case report: Abiotrophia/Granulicatella tubo-ovarian abscess in an adolescent virginal female. J Pediatr Adolesc Gynecol. 2010;23(1):e9–e12. | ||
Halperin R, Levinson O, Yaron M, Bukovsky I, Schneider D. Tubo-ovarian abscess in older women: is the woman’s age a risk factor for failed resonse to conservative treatment? Gynecol Obstet Invest. 2003;55(4):211–215. | ||
Demitras O, Akman L, Demitras GS, Hursitoglu BS, Yilmaz H. The role of serum inflammatory markers for predicting the tubo-ovarian abscess in acute pelvic inflammatory disease: a single-center 5-year experience. Arch Gynecol Obstet. 2013;287(3):519–523. | ||
Seshadri S, Kirwan J, Neal T. Perimenopausal pneumococcal tubo-ovarian abscess-case report and review. Infect Dis Obstet Gynecol. 2004;12(1):27–30. | ||
Tee YT, Wang PH, Yang SF, et al. Correlation of plasma osteopontin and neutrophil gelatinase-associated lipocalin levels with the severity and clinical outcome of pelvic inflammatory disease. Taiwan J Obstet Gynecol. 2014;53(2):158–161. | ||
Lee DC, Swaminathan AK. Sensitivity of ultrasound for the diagnosis of tubo-ovarian abscess: a case report and literature review. J Emerg Med. 2011;40(2):170–175. | ||
Adhikari S, Blaivas M, Lyon M. Ultrasound in emergency medicine: role of bedside transvaginal ultrasonography in the diagnosis of tubo-ovarian abscess in the emergency department. J Emerg Med. 2008;34(4):429–433. | ||
Thomassin-Naggara I, Dubernard G, Lafont C, Chopier J, Darai E, Bazot M. Imagerie de l’infection pelvienne [Imagery of pelvic infection]. J Radiol. 2008;89:134–141. French. | ||
Varras M, Polyzos D, Perouli E, Noti P, Pantazis I, Akrivis Ch. Tubo-ovarian abscesses: spectrum of sonographic findings with surgical and pathological correlations. Clin Exp Obstet Gynecol. 2003;30(2–3):117–121. | ||
Rakheja R, Makis W, Hickeson M. Bilateral tubo-ovarian abscess mimics ovarian cancer on MRI and 18F-FDG PET/CT. Nucl Med Mol Imaging. 2011;45(3):223–228. | ||
Velcani A, Conklin P, Specht N. Sonographic features of tubo-ovarian abscess mimicking an endometrioma and review of cystic adnexal masses. J Radiol Case Rep. 2010;4(2):9–17. | ||
Kim SH, Kim SH, Yang DM, Kim KA. Unusual causes of tubo-ovarian abscess: CT and MR imaging findings. Radiographics. 2004;24(6):1575–1589. | ||
Sharma N, Ganesh D, Srinivasan J, Jayakumar S, Mathew R. Retroperitoneal approach for dissection of inflamed pelvic viscera in acute pelvic inflammatory disease-case report. J Clin Diagn Res. 2014;8(5):OD03–OD05. | ||
Henry-Suchet J. Laparoscopic treatment of tubo-ovarian abscess: thirty years’ experience. J Am Assoc Gynecol Laparosc. 2002;9(3):235–237. | ||
Molander P, Cacciatore B, Sjöberg J, Paavonem J. Laparoscopic management of suspected acute pelvic inflammatory disease. J Am Assoc Gynecol Laparosc. 2000;7(1):107–110. | ||
Buchweitz O, Malik E, Kressin P, Meyhoefer-Malik A, Diedrich K. Laparoscopic management of tubo-ovarian abscesses. Surg Endosc. 2000;14(10):948–950. | ||
Yang CC, Chen P, Tseng JY, Wang PH. Advantages of open laparoscopic surgery over exploratory laparotomy in patients with tubo-ovarian abscess. J Am Assoc Gynecol Laparosc. 2002;9(3):327–332. | ||
Gjelland K, Ekerhovd E, Granberg S. Transvaginal ultrasound-guided aspiration for treatment of tubo-ovarian abscess: a study of 302 cases. Am J Obstet Gynecol. 2005;193(4):1323–1330. | ||
Harisinghani MG, Gervais DA, Maher MM, et al. Transgluteal approach for percutaneous drainage of deep pelvic abscesses: 154 cases. Radiology. 2003;228(3):701–705. | ||
Dewitt J, Reining A, Allsworth JE, Peipert JF. Tuboovarian abscesses: is size associated with duration of hospitalization & complications? Obstet Gynecol Int. 2010;2010:847041. | ||
Doganay M, Iskender C, Kilic S, et al. Treatment approaches in tubo-ovarian abscesses according to scoring system. Bratisl Lek Listy. 2011;112(4):200–203. | ||
Kakizawa H, Toyota N, Hieda M, et al. Gynecologic abscess: CT-guided percutaneous drainage. Hiroshima J Med Sci. 2006;55(3):97–100. | ||
Mokdad C, Rozsnayi F, Delaunay F, et al. Prise en charge chirurgicale des abcès tubo-ovariens complicant une endométriose profonde. [Surgical treatment of tubo-ovarian abscess occurring in deep endometriosis]. Gynecol Obstet Fertil. 2010;38(7–8):490–495. French. | ||
Elizur SE, Lebovitz O, Weintraub AY, et al. Pelvic inflammatory disease in women with endometriosis is more severe than those without. Aust N Z J Obstet Gynaecol. 2014;54(2):162–165. | ||
Romero B, Aibar L, Martínez Navarro L, Fontes J, Calderón MA, Mozas J. Pelvic abscess after oocyte retrieval in women with endometriosis: a case series. Iran J Reprod Med. 2013;11(8):677–680. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.