Back to Journals » Clinical Ophthalmology » Volume 9
Micropulse diode laser trabeculoplasty in Nigerian patients
Authors Babalola OE
Received 11 February 2015
Accepted for publication 7 April 2015
Published 20 July 2015 Volume 2015:9 Pages 1347—1351
DOI https://doi.org/10.2147/OPTH.S82678
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Olufemi Emmanuel Babalola1,2
1Rachel Eye Center, Abuja, Nigeria; 2Department of Ophthalmology, College of Health Sciences, Bingham University, New Karu, Nigeria
Introduction: The term micropulse laser trabeculoplasty suggests that only a fraction of the laser power is applied to the trabeculum to effect pressure lowering. It has not yet been exclusively used in Negroes, and we wish to report on our experience in Nigerian patients.
Methods: The study design is a retrospective chart review of our patients at the Rachel Eye Center in Abuja. The 810 diode Optos FastPulse laser was used to apply 34 cycles of treatment to 30 eyes of 16 individuals. Patients were selected based on the failure of maximal medical therapy. One patient had two extra rounds of treatment, while two patients were treated in only one eye. The pressure change at 1 hour after the treatment was analyzed. Patients were followed up for a mean period of 160 days with continuous monitoring of pressure changes. Patients’ original therapy was not disturbed.
Results: Postlaser immediate drop in intraocular pressure (IOP) averaged 3.2 mmHg (CI 1.6–4.7, P<0.0001) representing 17.2% drop from baseline prelaser IOP. The drop in IOP was sustained over varying periods, from a few weeks to several months. There was a temporary spike in three instances. No serious side effects were noted.
Conclusion: Micropulse diode laser trabeculoplasty is a useful adjunct in the management of open-angle glaucoma in Nigerians. This corroborates the findings of other researchers in western populations.
Keywords: micropulse, diode laser, Nigeria, glaucoma
Introduction
Various forms of laser have been used to supplement pressure control in primary open-angle glaucoma (POAG) patients. Argon laser trabeculoplasty (ALT) was introduced by Wise and Witter.1 The residual scarification, however, meant that it could not be repeated. Another form of laser treatment used by people is the selective laser trabeculoplasty (SLT), which was more recently introduced by Latina and Tumbocon.2 The efficacy of SLT has been analyzed by Frezzotti et al3 and Sayin et al4 among others; SLT has the advantages that it does not leave a noticeable scar on the trabeculum and is repeatable. However, the equipment tends to be expensive and beyond the reach of many practices, especially in Africa. Also, it is not utilizable for most other laser applications such as posterior segment interventions. More recently, micropulse laser trabeculoplasty has been introduced, and its effects are compared with ALT.3 This can be in the form of either diode or argon.4
We report on our experience with micropulse diode laser trabeculoplasty (MDLT) in African eyes in Abuja, Nigeria.
Materials and methods
This was a retrospective chart review of patients treated with SLT between the years 2010 and 2013. The study was carried out at the Rachel Eye Center, Garki, Abuja. Ethical clearance was obtained from the medical ethics board of Rachel Eye Center. The objectives of the study were to review the efficacy and safety/tolerability of MDLT in Nigerian adults with POAG with failed maximal medical therapy and to compare our findings with the experience in other population. We also set out to analyze the effect of various criteria such as spot size, number of burns, total energy of laser applied, presence of peripheral anterior synechia (PAS), age, and sex on the outcome. The inclusion criteria were as follows: age >40 years, POAG with at least 50% gonioscopically open angles, and failure of maximal medical therapy. Exclusion criteria included failure to obtain consent, patients with poor access to the angle on gonioscopy, concomitant infection or inflammation, and infirmity sufficient to prevent adequate application of the laser. The procedure was explained to the patients, and the consent was obtained in writing. The instrument utilized for the laser treatment was Optos 810 nm FastPulse diode laser. The intraocular pressure (IOP) was measured by the Keeler intelliPuff Non Contact Tonometer. This instrument has been found to be comparable to the standard Goldmann applanation tonometry in a study we previously carried out in our clinic.5
The main indication for the treatment was an unsatisfactory response to medical management and/or a reluctance to undergo trabeculectomy. Three spot sizes of 75 μm, 125 μm, and 200 μm were utilized at various times for various patients. There was no uniformity in the literature as to the recommended spot size. Power setting of 1,000 mW and a 15% duty cycle over a duration of 200 ms was utilized for all cases. Burns were applied to the lower 180° half except where access was precluded by narrow approach or PAS.
With these settings, a train of 100 laser pulses with 300 μs ON time, each separated by 1,700 μs OFF time, is delivered with each 200 ms application at a repetition rate of 500 Hz. Thirty-four cycles of treatment were applied to 30 eyes of 16 individuals (mean age: 57 years [SD 8.08], five females and eleven males). One patient had two extra rounds of treatment, while two patients were treated in only one eye. IOP was measured by Keeler intelliPuff Non Contact Tonometer before and 1 hour after the laser treatment. IOP measurements were adjusted for corneal thickness. Patients were placed on diclofenac eye drops after the treatment. There was otherwise no interference with the patients’ ongoing glaucoma treatment. Thus, we were looking for the additional effect of the laser, if any.
The presence of PAS and other angle details were noted during the treatment. Subsequent measurements were carried out as patients came for follow-up treatment. It should be noted that all patients had routine computerized visual field test carried out before and after MDLT therapy. Data were extracted from the case notes and entered into Excel workbook. Analysis was carried out using the Stata version 9.0.
Results
A total of 34 cycles of treatment were analyzed. The mean age of the patients was 57 years, with a male/female ratio of 2:1. An average of 177 burns (95% CI 165–188) was applied per session. The average total power applied was 7.3 mJ (95% CI 6.4–8.3). Mean follow-up period was 160 days (95% CI 48–273). The maximum follow-up period was 800 days. Some patients dropped out of follow-up after a short period. Average prelaser IOP was 18.6 mmHg compared to 15.5 mmHg postlaser. Thus, postlaser immediate drop in IOP averaged 3.2 mmHg (CI 1.6–4.7, P<0.0001), representing 17.2% drop (Figure 1 [box and whisker plot] and Figure 2 [histogram]). The histogram shows the spread of change in IOP. Note that the IOP dropped by up to 60% in some instances. There were, however, three instances of a spike of 1 mmHg, 3 mmHg, and 4 mmHg. The spikes generally reversed without additional antihypertensive treatment to at least pretreatment levels by the following day.
  | Figure 1 Box and whisker plot showing change in IOP at 1 hour after MDLT. |
  | Figure 2 Histogram showing percentage change in IOP after MDLT. |
In Figure 3, we see that the drop in IOP was sustained over varying periods, from a few weeks to months. We also assessed the distribution of IOP within the study population over 3 years spanning before and after the treatment. Five time points were considered: at presentation, after maximal medical therapy, 1 hour after MDLT, at the lowest pressure recorded after laser, and at the highest pressure recorded after laser (Figure 4). The highest profile, as will be expected, was at presentation. This fell on the commencement of medical management. There was further drop immediately after laser application. It is likely that patients who are not on any treatment would have experienced a greater magnitude of drop in IOP with laser. However, all our patients were already on maximal medical therapy. Fluctuations between the lowest and highest measurements after laser may be associated with reduced compliance, with tachyphylaxis, or with reduction in the effect of the laser.
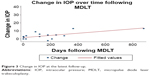  | Figure 3 Change in IOP at the latest follow-up. |
  | Figure 4 Distribution of IOP at various stages of follow-up within the study population. |
Factors that may affect outcome
We also assessed factors that may affect the outcome of lasers: spot size, total power delivered, total number of burns, presence or absence of PAS, and the sex and age of the patients. A spot size of 200 μm caused the lowest average drop (11 mmHg) compared to 125 μm (1.3 mmHg) and 75 μm (2.6 mmHg) (Figure 5). The total power delivered was positively correlated with the decrease in IOP (r=0.55), but there was a poor correlation with the total number of burns per se (Figures 6 and 7). The presence of PAS did not appear to affect the outcome (drop of 3.1 with PAS vs 3.6 without, P=0.607). Sex and age (Figure 8) were not significantly correlated with IOP change after treatment. There was a mean drop in IOP of 3.11 mmHg in females as compared to 3.17 in males (P=0.9709) during t-test.
  | Figure 5 The effect of spot size on the change in IOP. |
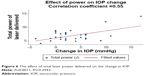  | Figure 6 The effect of total laser power delivered on the change in IOP. |
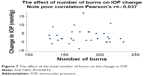  | Figure 7 The effect of the total number of burns on the change in IOP. |
  | Figure 8 The effect of age on the response to laser treatment. |
Discussion
MDLT was indicated in our patients following the failure of maximal medical therapy. In our practice, we define this as persistently high IOP or progression of visual field/retinal nerve fiber layer loss even with the application of a combination of three or four topical medications and/or with oral hypotensive medical treatment. The average drop in IOP of 17.2% is slightly lower than that obtained in a previous study by Ingvoldstad et al.6 They reported IOP reductions of 18.9% with ALT and 18.3% with MDLT.
Unlike in their study, we did not observe significant inflammatory response. In addition, PAS formation after treatment was not a noticeable problem. Fea et al7 also carried out MDLT in a cohort of 20 patients, following them up for about 12 months. The treatment was successful in 15 eyes (75%) at 12 months. The IOP was significantly lower throughout follow-up (P<0.01). At 12 months, the mean percentage of IOP reduction in the 15 respondent eyes was 22.1% and 12 eyes (60%) had IOP reduction higher than 20%. If the nonrespondent eyes are included, the average drop in IOP should probably approach our findings.
It is debatable whether Micropulse ALT is superior in the long term. The results published by doctors who use the IRIDEX laser suggest that Micropulse ALT may be better for sustained results. Gossage8 obtained a drop of 18% in IOP at 4 months.
There are ongoing clinical trials by Belyea9 comparing Micropulse ALT with SLT. It may also be useful to compare MDLT with micropulse ALT. The mechanism of action of MDLT is not clear at this time, but it has been speculated that this may be due to an increase in the expression of stromelysin by the trabecular juxtacanalicular cells.10
Limitation of the study
This is a retrospective review of case notes, and therefore, patients were not examined at specific time intervals.
Conclusion and general comments
Our findings suggest that MDLT does lower IOP in Nigerian patients with POAG. It appears to be a useful adjunct to conservative treatment. However, the effect may not be long lasting in all cases, and there is a subset of patients who appear not to respond to the therapy. It is, however, repeatable because thermal damage to the trabeculum is minimal.
The equipment we used in this study is generally much less expensive (Figure 9) than standard SLT and is applicable for other procedures, especially posterior segment laser interventions. This is an important consideration in developing countries. In our opinion, it is now difficult to justify destructive burns on the retina or the trabeculum, when indeed comparable effect can be achieved with subthreshold micropulse laser.
  | Figure 9 The FastPulse diode laser console-slit lamp setup. |
Acknowledgment
The abstract of this paper was presented at the 118th World Ophthalmology Congress held in Tokyo, Japan, as an E-poster presentation with interim findings. The poster’s abstract was published in e PosterAbstracts (http://www.myschedule.jp/woc2014/detail.php?session_unique_id=PO006&sess_id=2949&strong=1). The actual paper, however, has never been published.
Disclosure
The author reports no conflicts of interest in this work.
References
Wise JB, Witter SL. Argon laser therapy for open-angle glaucoma. Arch Ophthalmol. 1979;97:319–322. | ||
Latina MA, Tumbocon JA. Selective laser trabeculoplasty. A new treatment option for open angle glaucoma. Curr Opin Ophthalmol. 2002;13(2):94–96. | ||
Frezzotti P, Motolese I, Peruzzi S, et al. Selective Laser Trabeculoplasty: Hypotensive Efficacy, Anterior Chamber Inflammation and Postoperative Pain. Siena, Italy: Department of Surgery, Ophthalmology Unit, University of Siena; 2015. | ||
Sayin N, Alkin Z, Ozkaya A, et al. The efficacy of selective laser trabeculoplasty in medically uncontrolled glaucoma. ISRN Ophthalmol. 2013;2013:4. [Article ID 975281]. | ||
Babalola OE, Kehinde AV, Iloegbunam AC, Akinbinu T, Moghalu C, Onuoha I. A comparison of the Goldmann applanation and non-contact Keeler Pulsair (EasyEye) tonometers and the effect of central corneal thickness in indigenous African eyes. Ophthalmic Physiol Opt. 2009;29(2):182–188. | ||
Ingvoldstad DD, Krishna R, Willoughby L. Micropulse diode laser trabeculoplasty versus argon laser trabeculoplasty in the treatment of open angle glaucoma [abstract]. Invest Ophthal Vis Sci. 2005;46:123. | ||
Fea AM, Bosone A, Rolle T, Brogliatti B, Grignolo FM. Micropulse diode laser trabeculoplasty: a phase II clinical trial with 12 months follow up. Clin Ophthalmol. 2008;2(2):247–252. | ||
Gossage DD. 532 nm MicroPulse Laser Trabeculoplasty Successfully Lowers IOP as Primary Treatment. Iridex Clinical Case Reports Series. Available from: http://www.iridex.com/portals/0/physician-education/pdf/Gossage%20532%20MLT%202012.pdf. Accessed May 7, 2014. | ||
Belyea D. Micropulse Laser Trabeculoplasty Versus Selective Laser Trabeculoplasty for Treatment of Open Angle Glaucoma (MLT versus SLT). Available from: http://clinicaltrials.gov/ct2/show/NCT01956942. Accessed May, 2014. | ||
Parshley DE, Bradley JM, Fisk A, et al. Laser trabeculoplasty induces stromelysin expression by trabecular juxta-canalicular cells. Invest Ophthalmol Vis Sci. 1996;37:795–804. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
