Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 12
Metabolic syndrome is associated with peripheral endothelial dysfunction amongst men
Authors Taher R, Sara JD, Heidari B, Toya T , Lerman LO , Lerman A
Received 9 February 2019
Accepted for publication 11 April 2019
Published 5 July 2019 Volume 2019:12 Pages 1035—1045
DOI https://doi.org/10.2147/DMSO.S204666
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Juei-Tang Cheng
Riad Taher,1 Jaskanwal D Sara,1 Behnam Heidari,1 Takumi Toya,1 Lilach O Lerman,2 Amir Lerman1
1Division of Cardiovascular Diseases, Mayo Clinic College of Medicine and Science, Rochester, MN, USA; 2Division of Nephrology and Hypertension, Department of Medicine, Mayo Clinic College of Medicine and Science, Rochester, MN, USA
Purpose: Metabolic syndrome (MetS) and peripheral endothelial dysfunction (PED) are both independently associated with an increased risk of cardiovascular disease (CVD). PED provides prognostic information beyond that provided by conventional risk factors. However, the association between MetS and PED remains uncertain. We evaluated the association between MetS and PED.
Patients and methods: We performed a retrospective analysis of patients who were referred to Mayo Clinic between 2006 and 2014 for evaluation of chest pain and/or an assessment of CVD risk that included an assessment of PED measured with reactive hyperemia peripheral arterial tonometry. MetS was defined as the presence of at least 3 of the following: body mass index≥25 kg/m,2 impaired fasting glucose or diabetes, high blood pressure or hypertension, hypertriglyceridemia, or low high-density lipoprotein cholesterol.
Results: Six hundred seventy-eight patients were included (mean age 51.9±13.5 years, 418 (61.6%) women), of which 293 (43.2%) had PED, and 249 (36.7%) had MetS. In multivariable analyses adjusted for age, sex, CVD, smoking status, and elevated low-density lipoprotein, MetS was significantly associated with PED (Odds Ratio (OR) 2.06; P=0.0090). Of the individual MetS components, only being overweight and MetS range high-density lipoprotein had a similar association. After stratifying by sex, the association between MetS and PED persisted only in men (OR 3.16, P=0.0094).
Conclusions: MetS is associated with PED in men undergoing an assessment of chest pain and/or CVD risk. Identifying PED in individuals with MetS could provide an abridged assessment of risk, potentially allowing for earlier and more intensive management of risk factors.
Keywords: metabolic syndrome, peripheral endothelial dysfunction, reactive hyperemia peripheral arterial tonometry, cardiovascular disease
Introduction
Metabolic syndrome (MetS) is common, with an estimated prevalence of 34.5% amongst the adult population of the United States1 and is associated with increased cardiovascular disease (CVD) and mortality.2
Endothelial dysfunction precedes atherosclerosis and is independently associated with adverse CVD events.3 Endothelial dysfunction can be measured peripherally and non-invasively by assessing the reactive hyperemia response.4 Observational data demonstrate that individuals with minimal traditional cardiovascular risk factors who have peripheral endothelial dysfunction (PED) have a higher incidence of cardiovascular events including mortality at follow-up compared to those without PED.3,5 Thus, PED provides prognostic information above and beyond that provided by conventional CVD risk factors.
While MetS predicts an increased risk for CVD, it is not clear whether it adds additional important information to existing cardiovascular risk stratification models.6 Thus, whether evaluating for MetS contributes to patient risk estimation remains uncertain. In addition, the mechanism by which MetS mediates the increased incidence of cardiovascular events is not fully determined. The significant association between MetS and PED had been described in previous studies;7,8 however, other studies had demonstrated only partial9 or weak10 association between MetS and peripheral vascular health.
In the current study, we evaluate the association between MetS and PED, as an index of endothelial function and vascular health as a potential mediator for cardiovascular risk in these individuals.
Patients and methods
In this retrospective cross-sectional study, 722 patients were referred by their primary physicians to Mayo Clinic between 2006 and 2014 for assessment of chest pain and/or assessment of cardiovascular risk and underwent PED testing using EndoPAT. The decision to undertake EndoPAT testing was at the clinical discretion of the evaluating physician. Only the first test for each patient was included in the final data analysis and thus 44 tests were excluded. EndoPAT (Itamar Medical Ltd., Caesarea, Israel) which is Food and Drug Administration approved noninvasive device, assesses PED by measuring Reactive Hyperemia Peripheral Arterial Tonometry (RH-PAT).4 The reactive hyperemia protocol consists of a 16-min reactive hyperemia test, in the following sequence: a 5-min baseline measurement, after which a blood pressure cuff on the test arm is inflated to 60 mmHg above baseline systolic blood pressure, or at least 200 mmHg for 5 min, after which the cuff is deflated, and the post-deflation PAT tracing is recorded for an additional 6 mins. The ratio of the PAT signal after cuff release compared to baseline is calculated through a computer algorithm automatically normalizing for baseline signal and indexed to the contralateral arm. Previous studies have demonstrated that a 1-min RH-PAT index of less than 2.0 correlates best with abnormal PED, with a specificity of over 96%.11
Patients’ consent
The study was approved by Mayo Clinic International Review Board with compliance with the Declaration of Helsinki, and all patients provided written informed consent to participate in the protocol and have their clinical information and data used for this and other research studies.
Patients’ information
Data were collected on the following parameters: demographic factors (race, sex, and age), traditional cardiovascular risk factors (hypertension; diabetes mellitus; dyslipidemia, defined according to The American Association of Clinical Endocrinologists’ (AACE) 2017;12 smoking status and obesity defined as body mass index (BMI) ≥30 kg/m2)13 and presence of obstructive CVD, which was defined as a history of percutaneous coronary intervention, history of coronary artery bypass graft surgery, coronary artery stenosis of ≥50% of at least one coronary artery on coronary angiogram or coronary computed tomography angiography, history of ischemic stroke or transient ischemic attack assumed not to be secondary to atrial fibrillation, carotid artery stenosis ≥50%, or a clinical diagnosis of peripheral artery disease. Data on laboratory information were also collected including fasting plasma glucose (FPG), hemoglobin A1C, lipid profile, and creatinine with which estimated glomerular filtration rate (eGFR) was calculated using MDRD equation.14
The definition of MetS in the current study was based largely upon the Adult Treatment Panel III (ATP III) criteria, the most widely used definition in clinical practice,15 which defines the MetS as the presence of any three of the following: (1) waist circumference in men≥102 cm and in women≥88 cm (2) Serum triglycerides≥150 mg/dL or drug treatment for elevated triglycerides (3) Serum high-density lipoprotein (HDL) cholesterol<40 mg/dL in men or <50 mg/dL in women or drug treatment for low HDL cholesterol (4) Blood pressure 130/85 mmHg or drug treatment for elevated blood pressure (5) FPG≥100 mg/dL or drug treatment for elevated blood glucose. The AACE 200316 definition of MetS enables using overweight defined as BMI≥25 kg/m213 as marker of adiposity. The relationship between the variable definitions of MetS and incident CVD and mortality appears to be similar.17 Other study18 that evaluated the ability of different definitions of MetS to predict cardiovascular risk among individuals found AACE 2003 criteria less sensitive but more specific than ATP III criteria.
Identification of MetS in the current study was based on the ATP III criteria with substitution of waist circumference for BMI≥25 kg/m2 (adopted as criterion of MetS by AACE 2003) considering lack of data on waist circumference in the patient sample.
Statistical analysis
Baseline characteristics of the study population were presented as mean±standard deviation (SD) for normally distributed continuous variables, and number plus percent for categorical variables. Study participants were divided into those with normal and those with abnormal endothelial function. To compare variable between the two study groups we did two sample t-test for normally distributed continuous variables, Mann–Whitney U test for non-normally distributed variables, and χ2 test for categorical variables. EndoPAT indexes and frequency of an abnormal RH-PAT index were compared between subjects with and without MetS. Logistic regression model was done to estimate the associations between RH-PAT index and MetS. Multivariable analyses assessing the association between MetS, as well as its individual components, and abnormal RH-PAT index were performed and adjusted for traditional cardiovascular risk factors which are not included in the definition of MetS, which include age, sex, CVD, smoking status and elevated low-density lipoprotein (LDL). Two-sided P-values less than 0.05 were accepted as significant. All statistical analyses were performed using JMP 9 software (SAS Institute, Inc., Cary, NC, USA).
Results
Six hundred seventy-eight subjects were included in our study, of which 418 (61.7%) were women and 613 (90.4%) were Caucasian. The mean age was 51.9±13.5 years. Two hundred forty-nine subjects (36.7%) had MetS and 293 (43.2%) had an abnormal RH-PAT index. Patients’ baseline characteristics are summarized in Table 1. Compared to those with a normal RH-PAT, patients with an abnormal RH-PAT index had a significantly higher frequency of obstructive CVD, dyslipidemia, overweight, type 2 diabetes, high FPG, low HDL, and high triglycerides. In addition, patients with an abnormal RH-PAT index had a significantly higher frequency of MetS. Compared to women, men had a significantly higher frequency of MetS, abnormal RH-PAT index, obstructive CVD, obesity, past or current smokers, high FPG and dyslipidemia (Table 2).
 |
Table 1 Patients’ characteristics |
 |
Table 2 Patients’ characteristics stratified by sex |
There was a statistically significant correlation between the incremental sum of MetS components and RH-PAT index. Each additional MetS component reduced the RH-PAT index by 0.08 (r2=0.03, P<0.0001). After stratifying by sex, each additional MetS component reduced the RH-PAT index by 0.07 (r2=0.02, P=0.0069) and 0.10 (r2=0.04, P=0.0014) in women and men, respectively (not shown in the tables).
Mean RH-PAT index among patients with MetS was lower compared to patients without MetS in all individuals and after stratifying by sex to men and women (Table 3).
 |
Table 3 Mean RH-PAT index in MetS with stratification by sex |
In a univariable analysis, MetS was significantly associated with an abnormal RH-PAT index with an Odds Ratio (OR) of 2.32 (P<0.0001), as well as after stratifying individually for age, sex, CVD, smoking status, dyslipidemia, and obesity (Table 4).
 |
Table 4 The association between MetS and abnormal RH-PAT index |
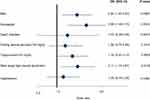
In multivariable analyses (Figure 1) adjusting for factors not included in the definition of MetS, namely, age, sex, presence of obstructive CVD, smoking status, and elevated LDL (LDL≥130 mg/dL or treatment by lipid-lowering therapy), MetS was significantly associated with an abnormal RH-PAT index (OR 2.06; P=0.0090). Of the MetS components, overweight and MetS range HDL had a similar association. After stratifying by sex (Figure 2), MetS was associated with an abnormal RH-PAT index only among men (OR 3.16, P=0.0094). Of the MetS components, overweight only had a similar association amongst men, while MetS range HDL only had a similar association amongst women.
Table 5 shows the modification effect of statin treatment on the association between MetS, as well as its components, and abnormal RH-PAT index. The interaction was significant only among women with MetS.
 |
Table 5 The modification effect of statin treatment on the association between MetS, as well as MetS components, and abnormal RH-PAT |
Discussion
The current study demonstrates a significant association between PED and MetS; however, after stratification by sex, this association remains significant only in men. Thus, our findings support the potential role of pre-clinical assessment for impaired endothelial function in individuals with MetS as a marker of increased risk for CVD. This would give rise to an objective, noninvasive assessment of vascular health by providing an integrated index of CVD risk that is more easily obtained and may provide more prognostic information than that provided by classifying individuals as having MetS.
The findings of our study additionally highlight the following points:
MetS and sex
Bi et al19 found that the association between android fat, insulin resistance, and MetS exists only in men. Furthermore, a recent study20 in overweight or obese but otherwise healthy subjects found that men had a more detrimental cardiometabolic risk profile compared to women despite similar age and BMI. The current study extends these findings by demonstrating a significant relationship between MetS and PED as a marker of early atherosclerosis, amongst men but not women after adjusting for CVD and conventional CVD risk factors which are not included in the MetS definition.
Bjorntorp et al21 showed that the risk of coronary heart disease rises among women whose waist-to-hip ratio is higher than 0.5. CVD had been linked to upper body obesity that is independent to the degree of overall obesity in another study .22 Waist circumference is a measurement of abdominal obesity and provides risk information that is not accounted for by BMI,23,24 although BMI is more convenient to measure in clinical practice and is also known to correlate with CVD risk.25 In the current study, given a lack of data on waist circumference, we used BMI as an alternative indicator of adiposity. We showed, in multivariable analysis, that overweight is associated with abnormal PED in all individuals and men only, which may in part explain the discordance between sexes in the association between MetS and PED. In turn, these findings underscore the potential importance of using waist circumference as a more appropriate indicator of adiposity and marker of risk in women.
MetS and its components
Among individual MetS components, only overweight and MetS range HDL have significant association with PED in multivariable analyses. After stratifying by sex, that association was demonstrated between PED and MetS range HDL only in women, and overweight only in men. In fact, the data regarding the relationship between MetS components and vascular risk are variable in the literature. In a prospective study of a population of patients with angiographically significant coronary artery disease,26 from the individual components of metabolic syndrome (defined per the ATP III criteria), only the low HDL independently predicted vascular events. Further, in a prospective, multicenter, international study,9 early atherosclerosis was evaluated in a variety of ways including the carotid-femoral pulse wave velocity (CF-PWV) and cardio-ankle vascular index (CAVI). The authors found higher CF-PWV only to be associated with the presence of MetS and found no association between CAVI and MetS. CAVI was associated with high glucose and blood pressure while CF-PWV was associated with all five MetS components individually. In another study,27 the larger the number of the MetS components, the greater the increase in PWV. The current study is in accord with the findings of these studies by demonstrating reduction of RH-PAT index by each additional individual MetS component and by demonstrating the role of overweight in men, as discussed before, and low HDL in women which are independently associated with PED as an early marker of atherosclerosis in a relatively young group of patients presenting for evaluation of chest pain and/or evaluation of CVD risk. Conversely, Sattar et al10 did show that MetS and its components had a weak or no association with vascular risk in elderly patients. However, the study was based on two patient populations aged 60–79 and 70–82 which is significantly older than the age in the current study.
Weisrock et al28 found good reliability of PAT in different groups but not in subjects with hypertension, possibly due to variations in heart rate. That could explain the absence of significant association between PED and hypertension in our study. We did not find a significant association between type2 diabetes and PED which could be due to small number of diabetic patients (53, 7.8%) and relatively good diabetes control (mean Hba1c 7.07±1.12% in the diabetic patients). Further studies are needed.
MetS and statin treatment
The current study shows that statin treatment may ameliorate the association between PED and MetS among women. Statins were shown to improve PED evaluated by flow-mediated dilation in subjects with hyperlipidemia and MetS and/or diabetes.29 In another study,30 obese men with MetS, but without CVD, had reduced levels of endothelial progenitor cells which improved after treatment with statins. Thus, the current study supports the early treatment of seemingly low-risk individuals with MetS to modify PED with a view to reduce CVD risk. However, our study only showed a beneficial effect of statin treatment in women. Compared to women, men in our study had a higher frequency of obstructive CVD and CVD risk factors. Thus, the lack of interaction of statin treatment with the association between MetS and PED in men could be due to the greater burden of CVD in men compared to women. These results raise the question whether patients with MetS, even relatively low-risk patients, could gain benefit from early initiation of statin therapy as primary prevention for CVD regardless of LDL level. This requires further studying.
Strength and limitations of the study
The current study has several strengths including a large number of patients allowing adjustment for several potentially confounding variables. Limitations of the current study include: (1) some of the patients in the non-known CVD could still have occult disease that may be obstructive or non-obstructive in spite of guideline-based investigation, (2) we used BMI≥25 kg/m2 as a surrogate indicator of adiposity as opposed to waist circumference due to lack of data, (3) there is still no clear protocol for which patients should undergo PED testing for evaluation of cardiovascular risk, indeed the decision to perform testing was based on each physician’s individual clinical judgment in evaluating chest pain and/or cardiovascular risk, and (4) this was a retrospective cross-sectional analysis which makes deriving causal associations challenging.
Conclusions
The current study demonstrates that MetS is associated with PED in men even after adjusting for confounding variables, including baseline CVD status. PED may therefore act as a mediator of CVD risk in patients with MetS. Identifying PED using EndoPAT in individuals with MetS, including low-risk subjects could provide an abridged assessment of risk, potentially allowing for earlier and more intensive management of CVD risk factors.
Abbreviation list
MetS, metabolic syndrome; CVD, cardiovascular disease; PED, peripheral endothelial dysfunction; RH-PAT, Reactive Hyperemia Peripheral Arterial Tonometry; LDL, low-density lipoprotein; HDL, high-density lipoprotein; BMI, body mass index; FPG, fasting plasma glucose; ATP III, Adult Treatment Panel III; AACE, American Association of Clinical Endocrinologists’; OR, odds ratio; CI, confidence interval; Fig., figure; CF-PWV, carotid-femoral pulse wave velocity; CAVI, cardio-ankle vascular index; PROSPER, Pravastatin in elderly individuals at risk of vascular disease; SD, standard deviation; DLP, dyslipidemia; SBP, systolic blood pressure; DBP, diastolic blood pressure.
Data sharing statement
By direct contact with the corresponding author.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
Dr Amir Lerman reports personal fees from Itamar Medical and Philips Volcano, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. Ford ES. Prevalence of the metabolic syndrome defined by the International Diabetes Federation among adults in the U.S. Diabetes Care. 2005;28(11):2745–2749.
2. Gami AS, Witt BJ, Howard DE, et al. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta-analysis of longitudinal studies. J Am Coll Cardiol. 2007;49(4):403–414. doi:10.1016/j.jacc.2006.09.032
3. Bonetti PO, Lerman LO, Lerman A. Endothelial dysfunction: a marker of atherosclerotic risk. Arterioscler Thromb Vasc Biol. 2003;23(2):168–175.
4. Martin EA, Prasad A, Rihal CS, Lerman LO, Lerman A. Endothelial function and vascular response to mental stress are impaired in patients with apical ballooning syndrome. J Am Coll Cardiol. 2010;56(22):1840–1846. doi:10.1016/j.jacc.2010.03.107
5. Matsuzawa Y, Kwon TG, Lennon RJ, Lerman LO, Lerman A. Prognostic value of flow-mediated vasodilation in brachial artery and fingertip artery for cardiovascular events: a systematic review and meta-analysis. J Am Heart Assoc. 2015;4(11):e002270. doi:10.1161/JAHA.115.002270
6. Scuteri A, Laurent S, Cucca F, et al., Metabolic Syndrome and Arteries Research (MARE) Consortium. Metabolic syndrome across Europe: different clusters of risk factors. Eur J Prev Cardiol. 2015;22(4):486–491. doi:10.1177/2047487314525529
7. Matsuzawa Y, Sugiyama S, Sugamura K, et al. Successful diet and exercise therapy as evaluated on self-assessment score significantly improves endothelial function in metabolic syndrome patients. Circ J. 2013;77(11):2807–2815.
8. Lteif AA, Han K, Mather KJ. Obesity, insulin resistance, and the metabolic syndrome: determinants of endothelial dysfunction in whites and blacks. Circulation. 2005;112(1):32–38. doi:10.1161/CIRCULATIONAHA.104.520130
9. Topouchian J, Labat C, Gautier S, et al. Effects of metabolic syndrome on arterial function in different age groups: the Advanced Approach to Arterial Stiffness study. J Hypertens. 2018;36(4):824–833. doi:10.1097/HJH.0000000000001631
10. Sattar N, McConnachie A, Shaper AG, et al. Can metabolic syndrome usefully predict cardiovascular disease and diabetes? Outcome data from two prospective studies. Lancet. 2008;371(9628):1927–1935. doi:10.1016/S0140-6736(08)60602-9
11. Lerman A, Zeiher AM. Endothelial function: cardiac events. Circulation. 2005;111(3):363–368. doi:10.1161/01.CIR.0000153339.27064.14
12. Jellinger PS, Handelsman Y, Rosenblit PD, et al. American Association of Clinical Endocrinologists and American College of Endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease. Endocr Pract. 2017;23(suppl 2):1–87. doi:10.4158/EP171764.APPGL
13. No authors listed – National Institutes of Health, National Heart, Lung, and Blood Institute. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults-the evidence report. Obes Res. 1998;6(Suppl2):51S–209S.
14. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130(6):461–470.
15. Alberti KG, Eckel RH, Grundy SM, et al., International Diabetes Federation Task Force on Epidemiology and Prevention, Hational Heart, Lung, and Blood Institute, American Heart Association, World Heart Federation, International Atherosclerosis Society, International Association for the Study of Obesity. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–1645. doi:10.1161/CIRCULATIONAHA.109.192644
16. Meigs J. Metabolic syndrome and risk for type 2 diabetes. Expert Rev Endocrin Metab. 2006;1(1):57–66. doi:10.1586/17446651.1.1.57
17. Lawlor DA, Smith GD, Ebrahim S. Does the new International Diabetes Federation definition of the metabolic syndrome predict CHD any more strongly than older definitions? Findings from the British Women’s Heart and Health Study. Diabetologia. 2006;49(1):41–48. doi:10.1007/s00125-005-0040-3
18. Strazzullo P, Barbato A, Siani A, et al. Diagnostic criteria for metabolic syndrome: a comparative analysis in an unselected sample of adult male population. Metabolism. 2008;57(3):355–361. doi:10.1016/j.metabol.2007.10.010
19. Bi X, Loo YT, Henry CJ. Android fat as a determinant of metabolic syndrome: sex differences. Nutrition. 2018;57:127–132. doi:10.1016/j.nut.2018.05.016
20. Schorr M, Dichtel LE, Gerweck AV, et al. Sex differences in body composition and association with cardiometabolic risk. Biol Sex Differ. 2018;9(1):28. doi:10.1186/s13293-018-0189-3
21. Bjorntorp P. Regional patterns of fat distribution. Ann Intern Med. 1985;103(6(pt2)):994–995.
22. Rich-Edwards JW, Manson JE, Hennekens CH, Buring JE. The primary prevention of coronary heart disease in women. N Engl J Med. 1995;332(26):1758–1766. doi:10.1056/NEJM199506293322607
23. Koster A, Leitzmann MF, Schatzkin A, et al. Waist circumference and mortality. Am J Epidemiol. 2008;167(12):1465–1475. doi:10.1093/aje/kwn079
24. Jacobs EJ, Newton CC, Wang Y, et al. Waist circumference and all-cause mortality in a large US cohort. Arch Intern Med. 2010;170(15):1293–1301. doi:10.1001/archinternmed.2010.201
25. Prospective Studies Collaboration, Whitlock G, Lewington S, Sherliker P, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–1096. doi:10.1016/S0140-6736(09)60318-4
26. Saely CH, Koch L, Schmid F, et al. Adult treatment panel III 2001 but not International Diabetes Federation 2005 criteria of the metabolic syndrome predict clinical cardiovascular events in subjects who underwent coronary angiography. Diabetes Care. 2006;29(4):901–907.
27. Wrp L-V, Rodrigues S, Cepeda FX, et al. Arterial stiffness and its association with clustering of metabolic syndrome risk factors. Diabetol Metab Syndr. 2017;9:87. eCollection 2017. doi:10.1186/s13098-017-0286-1
28. Weisrock F, Fritschka M, Beckmann S, et al. Reliability of peripheral arterial tonometry in patients with heart failure, diabetic nephropathy and arterial hypertension. Vasc Med. 2017;22(4):292–300. doi:10.1177/1358863X17706752
29. Murrow JR, Sher S, Ali S, et al. The differential effect of statins on oxidative stress and endothelial function: atorvastatin versus pravastatin. J Clin Lipidol. 2012;6(1):42–49. doi:10.1016/j.jacl.2011.08.006
30. Westerweel PE, Visseren FL, Hajer GR, et al. Endothelial progenitor cell levels in obese men with the metabolic syndrome and the effect of simvastatin monotherapy vs. simvastatin/ezetimibe combination therapy. Eur Heart J. 2008;29(22):2808–2817. doi:10.1093/eurheartj/ehn431
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.