Back to Journals » Therapeutics and Clinical Risk Management » Volume 10
Meta-analysis of oral contraceptives and rheumatoid arthritis risk in women
Authors Qi S, Xin R, Guo W, Liu Y
Received 9 July 2014
Accepted for publication 5 August 2014
Published 4 November 2014 Volume 2014:10 Pages 915—923
DOI https://doi.org/10.2147/TCRM.S70867
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Shuang Qi,1 Rui Xin,2 Weina Guo,3 Yan Liu4
1Department of Anesthesiology, China–Japan Union Hospital, 2Department of Radiology, 2nd Hospital affiliated to Jilin University, 3Intensive Care Unit, 2nd Hospital affiliated to Jilin University, 4Department of Hand Surgery, China–Japan Union Hospital, Jilin University, Changchun, Jilin, People’s Republic of China
Background and objectives: Epidemiological investigations of the relationship between oral contraceptives and rheumatoid arthritis (RA) risk have reported controversial results. Therefore, a meta-analysis of case-control or cohort studies was performed to evaluate the role of oral contraceptives in relation to risk of developing RA.
Methods: Eligible studies were identified from databases PubMed and EMBASE by searching and reviewing references. Random effect models were utilized to summarize the relative risk (RR) estimates with 95% confidence intervals (CIs).
Results: A total of 12 case-control studies and five cohort studies were eligible for our analysis. No statistically significant association was observed between oral contraceptives and RA risk (RR=0.88, 95% CI=0.75–1.03). In the subgroup of geographic area, a decreased risk of borderline significance was observed for oral contraceptive users in European studies (RR=0.79, 95% CI=0.62–1.01), but this association did not emerge in the North American studies group (RR=0.99, 95% CI=0.81–1.21). No evidence for publication bias was detected (P for Egger’s test =0.231).
Conclusion: Our results of meta-analysis do not support the hypothesis of a protective effect of oral contraceptives on the risk for RA in women.
Keywords: rheumatoid arthritis, oral contraceptive, hormone, meta-analysis
Introduction
Rheumatoid arthritis (RA) is a common chronic systemic inflammatory autoimmune disorder of the synovial tissues and joints, which affects approximately 1% of the adult population all over the world.1–3 Although the etiology of RA remains elusive, an increasing body of evidence suggests that sex hormones may play a role in RA pathogenesis. RA occurs approximately twice to thrice as often in women as in men.4 In addition, RA symptoms tend to diminish during pregnancy and aggravate postpartum.5,6 Owing to this background, recent epidemiological studies evaluated the risk of RA in users of oral contraceptives (OCs) versus nonusers.4,7–42 However, a conflicting picture on this issue was presented in these studies. Given that the vast majority of studies were of small sample size and characterized by low statistical power, these findings may be detected by chance. Therefore, we performed a meta-analysis of case-control and cohort studies to summarize the evidence and provide an accurate estimation of association between OCs use and RA risk.
Material and methods
Search strategy
Studies assessing the relationship between RA risk and OCs were identified in PubMed and EMBASE databases using the following search terms: (“oral contraceptives” OR “exogenous hormones” OR “hormone”) AND (“rheumatoid arthritis” OR “RA”) AND (“risk” OR “risk factor”). The latest date for this search was June 13, 2014. The bibliographies of relevant articles were checked by a manual search for additional publications of interest.
Inclusion criteria
We adopted the following inclusion criteria: (1) the report described a case-control or cohort study; (2) the report provided the relative risk (RR) or odds ratio with corresponding 95% confidence interval (CI), or sufficient information to calculate them (ie, the distribution of exposure); (3) when multiple reports involved the same study population, only the most informative one was identified for this analysis. We excluded the conference abstracts, case series, letter to editors, reviews, meta-analysis, and cross-sectional studies and we also excluded those studies that involved family cases in their subjects.
Data collection
We extracted information on the first author, sites where the study was performed, age of study population, number of subjects (cases, controls, or cohort size), study design, years of case diagnosis or cohort enrollment, length of follow-up for cohort studies, the method of OCs exposure assessment, the adjusted RR estimates with corresponding 95% CIs from multivariable model, match factors, and covariates adjusted for in the analysis.
Statistical analysis
Analyses were conducted using STATA version 12 (STATA Corporation, College Station, TX, USA). The measure of interest was the RR. ORs were directly considered as RRs, because the prevalence of RA was rare.43 A random-effect model with the method of DerSimonian and Laird, which incorporates the heterogeneity across studies, was employed to calculate the pooled RR.44 We evaluated the heterogeneity using the Cochran’s Q and I2 statistics.45,46 Significant heterogeneity was found as P-value for heterogeneity <0.10 or I2>50%. Stratified analyses were performed according to study design (case-control vs nested case-control vs cohort studies), source of control (population-based vs hospital-based case-control studies), and geographic area (European vs North American studies). Also, a sensitivity analysis was performed to investigate the influence of potential confounding (ie, age, smoking, parity/pregnancy, age at menarche, body mass index (BMI), social class, and marital status) on RA risk. We conducted a sensitivity analysis to assess the impact of individual studies on the overall results by excluding one study at a time. Potential publication bias was evaluated using Begg’s funnel plots and quantified by the Egger’s test (a P-value of <0.05 was considered statistically significant).47,48
The unit of the meta-analysis was a single comparison of OCs users versus nonusers. When a study presented separate RRs for different duration of OCs use versus nonuse, the overall risk estimate for OCs use versus nonuse was calculated from these separate RRs with the method proposed by Hamling et al.49 This method is utilized to combine estimates using the same reference category. Also, the association between estimates is taken into account. In the analyses on duration of OCs use, we define short-term use as <5 years, and long-term use ≥5 years. Among the included studies, two studies that reported long-term use as ≥4 years were also included in this meta-analysis. Then, we performed an analysis that excluded those two studies to investigate the robustness of the results of long-term OCs use.
Results
Search results and study characteristics
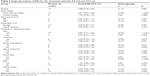
Based on our search terms, a total of 1,116 publications were identified in PubMed and EMBASE databases. Figure 1 shows the flowchart of literature inclusion and exclusion. We identified 47 publications for full-text evaluation, of which 30 publications were further excluded because they did not fulfill the inclusion criteria (ie, conference abstracts,34–42 meta-analyses/reviews,50–58 letters to editor/comments,59 cross-sectional studies,29,30 providing insufficient data,28 involving the same study population or overlapped data,8,31–33 involving family cases,13,17 reporting the relationship between noncontraceptive hormones and RA among perimenopausal and postmenopausal women,11 and using OCs users with less than one patient as reference9). Therefore, our meta-analysis was based on 17 publications, including 12 case-control and five cohort studies published between 1982 and 2010.4,7,10,12,14–14,18–27 All studies were published in English. The other characteristics of included studies are listed in Table 1.
  | Figure 1 The flowchart of literature selection. |
Overall association of OCs use and RA risk
Figure 2 presents the study-specific and pooled RRs and 95% CIs of RA for OCs users versus nonusers. The summary estimates were 1.02 (95% CI=0.90–1.15, I2=0.0%, P for heterogeneity =0.688), 0.81 (95% CI=0.63–1.05, I2=66.4%, P for heterogeneity <0.001), and 0.88 (95% CI=0.75–1.03, I2=61.1%, P for heterogeneity =0.001) for cohort studies, case-control studies, and all studies, respectively. In further analysis, according to the type of controls for the case-control studies, similar trends with the overall result were observed in population-based case-control studies (RR=0.87, 95% CI=0.65–1.17, I2=47.1%, P for heterogeneity =0.093) and hospital-based case-control studies (RR=0.78, 95% CI=0.51–1.18, I2=77.3%, P for heterogeneity =0.001). Considering subgroups of geographic area, the combined estimate was 0.79 (95% CI=0.62–1.01, I2=67.6%, P for heterogeneity =0.001) in European studies and the corresponding estimate was 0.99 (95% CI=0.81–1.21, I2=37.7%, P for heterogeneity =0.155) in North American studies. Considering subgroups of matching or adjusted factors, the correlation of OCs use related with RA risk was not significantly modified by age, smoking, parity/pregnancy, age at menarche, BMI, social class, or marital status (Table 2). In the analyses on duration of OCs use, the pooled RRs were 0.84 (95% CI=0.56–1.27, I2=80.0%, P for heterogeneity <0.001) for short-term use and 0.84 (95% CI=0.64–1.10, I2=52.8%, P for heterogeneity =0.048) for long-term use.
  | Figure 2 Forest plots of RA risk and OCs use. |
Sensitivity analysis and publication bias
In the sensitivity analysis, we removed one study at a time to assess robustness of the overall results. The results of the sensitivity analysis are shown in Table 3. The Begg’s funnel plot does not show any asymmetry (Figure 3). Also, no publication bias was ascertained by Egger’s test (P for Egger’s test =0.231).
  | Table 3 Results of sensitivity analysis for RA risk with OCs use |
  | Figure 3 Begg’s funnel plot (with pseudo 95% confidence limits) analysis to detect publication bias. |
Discussion
Female hormones have long been considered to play a role in human disease. Many epidemiologic studies that evaluated the relationship between OCs use and RA have yielded conflicting results, with inverse and positive correlations reported. To clarify this issue, five system reviews or meta-analyses have been published between 1989 and 1996.52–55,57 However, the results from previous meta-analysis remain controversial. Romieu et al in their meta-analysis of nine case-control studies found no significant association between OCs use and RA risk (RR=0.79, 95% CI=0.58–1.08).54 Spector and Hochberg reported that OCs use was associated with a decreased risk of RA (RR=0.73, 95% CI=0.61–0.85).55 In 1996, Pladevall-Vila et al summarized the evidence of seven case-control and three cohort studies published before 1993.57 The combined results showed that OCs use cannot decrease the risk of RA (RR=0.95, 95% CI=0.81–1.21).57 Since 1993, more than ten original studies have proven or denied those findings.17–34 Therefore, an updated meta-analysis was undertaken. Specifically, in our study, we (1) included the studies published to date, (2) excluded the overlapped data, (3) analyzed the variables (ie, study design, source of control, geographic area, and matching or adjustment factors) across studies, (4) investigated how the RA risk changed with the dose effect of duration of OCs use, and (5) conducted sensitivity analyses and publication bias.
Our current meta-analysis of 12 case-control and five cohort studies suggested that use of OCs was not significantly associated with RA risk. The association was not significantly affected by study design, source of control, or matching/adjustment factors. However, subgroup meta-analyses of geographic area based on limited numbers of studies indicated that compared with nonusers, a decreased risk of borderline significance was observed for OCs users in European studies, but this association did not emerge in the North American studies group.
Another problematic OCs variable (ie, current use) has been evaluated by three case-control and two cohort studies.7,15,21,24,26 All studies showed that there was a nonsignificant increase or decrease in RA risk emerged except in one hospital-based case-control study with 228 cases and 302 controls.7 Vandenbroucke et al found a 55% reduction in RA risk among current users. However, the number of current users was small, and we cannot exclude the possibility that the finding, of a significant decreased risk for RA among current users, is a chance finding and should be interpreted with caution. Given that “current use” measures different time points with respect to the date of diagnosis (or date of interview for controls) in case-control versus prospective cohort studies, risk estimates of this variable cannot be pooled across study designs.
Heterogeneity is often a concern in a meta-analysis. In our meta-analysis, evidence of substantial heterogeneity across studies of the associations of OCs use with RA risk was observed. This finding was consistent with a previous meta-analysis published in 1996, which showed that the source of controls was the most important characteristic in accounting for the strong heterogeneity.57 In our subgroup analyses by study design and source of controls, no significant heterogeneity was detected in cohort (I2=0.0%) or population-based case-control studies (I2=47.1%), but substantial heterogeneity was observed in hospital-based case-control studies (I2=77.3%). In hospital-based case-control studies, the choice of control populations differed markedly. The controls were women with a diagnosis of soft tissue rheumatism (bursitis, tenosynovitis, shoulder-hand syndrome, carpal tunnel syndrome, low back pain, etc) or osteoarthritis (localized to knee, hip, or vertebrae) recruited from outpatient clinics of university hospitals or private clinics. Moreover, the included studies were conducted in different countries, where people may share little in terms of genetic background, lifestyles, and RA incidence. Thus, the characteristics of subjects and study design likely contributed to the observed heterogeneity.
To evaluate the effect of exposure duration, short-term use of OCs was defined as duration of <5 years, and long-term use as duration of ≥5 years. We found that no significant reduction in RA risk was associated with short-term or long-term use. Moreover, the relationship between dose of OCs use and RA risk has been addressed in a hospital-based case-control study with 135 cases and 378 controls.14 Hazes et al defined the use of low-dose OCs as dose of <0.05 mg estrogen and high dose as dose of ≥0.05 mg estrogen, and found that the dose did not moderate the RR estimates. Evaluation of dose effect lends support for a causality of an association between exposure and disease, therefore, further investigation of OCs use with RA risk is needed with particular attention to duration and dose of OCs use.
Potential limitations of the present meta-analysis need to be addressed. First, because our analysis was mainly based on retrospective case-control studies, the observed null association may be masked by the recall and select biases originating from primary studies. Moreover, unmeasured or residual confounding is always a subject of major concern in observational studies. Although the results of subgroup analyses showed that the relationship between OCs use and RA risk was not influenced by the confounders such as age, smoking, parity/pregnancy, age at menarche, BMI, social class, or marital status, the likelihood that our finding resulted from other unmeasured confounders cannot be excluded. Second, we were unable to evaluate the components of OCs with RA risk. During the 1980s, OCs markedly differed from the ones used later on, eg, low estrogen, triphasic.60 Therefore, the formulation of OCs with RA risk remains open to discussion. Third, the RA case identification was based on different diagnosis criteria. Both 1958 American College of Rheumatology (ACR) and 1987 ACR criteria for RA were adopted in included studies. Thus, misclassification of subjects was possible and the relationship between OCs use and RA risk may be underestimated or overestimated. Furthermore, nowadays, RA classification criteria are updated by 2010 ACR classification criteria. Further evaluation of the relationship between OCs use and RA risk should adopt the new ACR classification criteria. Finally, publication bias could be a problem because studies with null effects are less likely to be published than those providing statistically significant results. Although no evidence of publication bias was detected by Egger’s test and Begg’s funnel plots in our meta-analysis, the estimation may not be accurate enough as the number of the included studies is relatively small.
In summary, findings of the present meta-analysis of 17 observational studies indicate that OC use cannot reduce the risk of RA. Yet, many questions still need to be addressed. Further large-scale prospective studies with emphasis on strict case definition based on the 2010 ACR classification criteria, formulation of OCs, duration of OCs use, dose of OCs use, and confounders are warranted to validate our findings.
Disclosure
The authors report no conflicts of interest in this work.
References
McInnes IB, Schett G. The pathogenesis of rheumatoid arthritis. N Engl J Med. 2011;365(23):2205–2219. | ||
Gibofsky A. Overview of epidemiology, pathophysiology, and diagnosis of rheumatoid arthritis. Am J Manag Care. 2012;18(13 suppl): S295–S302. | ||
Klareskog L, Catrina AI, Paget S. Rheumatoid arthritis. Lancet. 2009; 373(9664):659–672. | ||
Merlino LA, Cerhan JR, Criswell LA, Mikuls TR, Saag KG. Estrogen and other female reproductive risk factors are not strongly associated with the development of rheumatoid arthritis in elderly women. Semin Arthritis Rheum. 2003;33(2):72–82. | ||
Hazes JM. Pregnancy and its effect on the risk of developing rheumatoid arthritis. Ann Rheum Dis. 1991;50(2):71–72. | ||
Silman A, Kay A, Brennan P. Timing of pregnancy in relation to the onset of rheumatoid arthritis. Arthritis Rheum. 1992;35(2):152–155. | ||
Vandenbroucke JP, Valkenburg HA, Boersma JW, et al. Oral contraceptives and rheumatoid arthritis: further evidence for a preventive effect. Lancet. 1982;2(8303):839–842. | ||
Linos A, Worthington JW, O’Fallon WM, Kurland LT. Case-control study of rheumatoid arthritis and prior use of oral contraceptives. Lancet. 1983;1(8337):1299–1300. | ||
Allebeck P, Ahlbom A, Ljungström K, Allander E. Do oral contraceptives reduce the incidence of rheumatoid arthritis? A pilot study using the Stockholm County medical information system. Scand J Rheumatol. 1984;13(2):140–146. | ||
del Junco DJ, Annegers JF, Luthra HS, Coulam CB, Kurland LT. Do oral contraceptives prevent rheumatoid arthritis? JAMA. 1985;254(14): 1938–1941. | ||
Vandenbroucke JP, Witteman JC, Valkenburg HA, et al. Noncontraceptive hormones and rheumatoid arthritis in perimenopausal and postmenopausal women. JAMA. 1986;255(10):1299–1303. | ||
Darwish MJ, Armenian HK. A case-control study of rheumatoid arthritis in Lebanon. Int J Epidemiol. 1987;16(3):420–424. | ||
Hazes JM, Silman AJ, Brand R, Spector TD, Walker DJ, Vandenbroucke JP. Influence of oral contraception on the occurrence of rheumatoid arthritis in female sibs. Scand J Rheumatol. 1990; 19(4):306–310. | ||
Hazes JM, Dijkmans BC, Vandenbroucke JP, de Vries RR, Cats A. Reduction of the risk of rheumatoid arthritis among women who take oral contraceptives. Arthritis Rheum. 1990;33(2):173–179. | ||
Moskowitz MA, Jick SS, Burnside S, et al. The relationship of oral contraceptive use to rheumatoid arthritis. Epidemiology. 1990;1(2): 153–156. | ||
Spector TD, Roman E, Silman AJ. The pill, parity, and rheumatoid arthritis. Arthritis Rheum. 1990;33(6):782–789. | ||
Brennan P, Silman AJ. An investigation of gene–environment interaction in the etiology of rheumatoid arthritis. Am J Epidemiol. 1994;140(5):453–460. | ||
Jorgensen C, Picot MC, Bologna C, Sany J. Oral contraception, parity, breast feeding, and severity of rheumatoid arthritis. Ann Rheum Dis. 1996;55(2):94–98. | ||
Doran MF, Crowson CS, O’Fallon WM, Gabriel SE. The effect of oral contraceptives and estrogen replacement therapy on the risk of rheumatoid arthritis: a population based study. J Rheumatol. 2004;31(2): 207–213. | ||
Pedersen M, Jacobsen S, Klarlund M, et al. Environmental risk factors differ between rheumatoid arthritis with and without auto-antibodies against cyclic citrullinated peptides. Arthritis Res Ther. 2006;8(4):R133. | ||
Brennan P, Bankhead C, Silman A, Symmons D. Oral contraceptives and rheumatoid arthritis: results from a primary care-based incident case-control study. Semin Arthritis Rheum. 1997;26(6):817–823. | ||
Pikwer M, Bergström U, Nilsson JA, Jacobsson L, Berglund G, Turesson C. Breast feeding, but not use of oral contraceptives, is associated with a reduced risk of rheumatoid arthritis. Ann Rheum Dis. 2009; 68(4):526–530. | ||
Berglin E, Kokkonen H, Einarsdottir E, Agren A, Rantapää Dahlqvist S. Influence of female hormonal factors, in relation to autoantibodies and genetic markers, on the development of rheumatoid arthritis in northern Sweden: a case-control study. Scand J Rheumatol. 2010;39(6): 454–460. | ||
Vessey MP, Villard-Mackintosh L, Yeates D. Oral contraceptives, cigarette smoking and other factors in relation to arthritis. Contraception. 1987;35(5):457–464. | ||
Hannaford PC, Kay CR, Hirsch S. Oral contraceptives and rheumatoid arthritis: new data from the Royal College of General Practitioners’ oral contraception study. Ann Rheum Dis. 1990;49(10):744–746. | ||
Hernandez-Avila M, Liang MH, Willett WC, et al. Exogenous sex hormones and the risk of rheumatoid arthritis. Arthritis Rheum. 1990; 33(7):947–953. | ||
Karlson EW, Mandl LA, Hankinson SE, Grodstein F. Do breast-feeding and other reproductive factors influence future risk of rheumatoid arthritis? Results from the Nurses’ Health Study. Arthritis Rheum. 2004;50(11):3458–3467. | ||
Rodríguez LA, Tolosa LB, Ruigómez A, Johansson S, Wallander MA. Rheumatoid arthritis in UK primary care: incidence and prior morbidity. Scand J Rheumatol. 2009;38(3):173–177. | ||
Beydoun HA, el-Amin R, McNeal M, Perry C, Archer DF. Reproductive history and postmenopausal rheumatoid arthritis among women 60 years or older: Third National Health and Nutrition Examination Survey. Menopause. 2013;20(9):930–935. | ||
Adab P, Jiang CQ, Rankin E, et al. Breastfeeding practice, oral contraceptive use and risk of rheumatoid arthritis among Chinese women: the Guangzhou Biobank Cohort Study. Rheumatology (Oxford). 2014; 53(5):860–866. | ||
Wingrave SJ. Reduction in incidence of rheumatoid arthritis associated with oral contraceptives. Royal College of General Practitioners’ Oral Contraception Study. Lancet. 1978;1(8064):569–571. | ||
van Zeben D, Hazes JM, Vandenbroucke JP, Dijkmans BA, Cats A. Diminished incidence of severe rheumatoid arthritis associated with oral contraceptive use. Arthritis Rheum. 1990;33(10):1462–1465. | ||
Pedersen M, Jacobsen S, Garred P, et al. Strong combined gene-environment effects in anti-cyclic citrullinated peptide-positive rheumatoid arthritis: a nationwide case-control study in Denmark. Arthritis Rheum. 2007;56(5):1446–1453. | ||
Hernandez-Avila M, Liang MH, Willett WC, et al. Oral contraceptives, replacement oestrogens and the risk of rheumatoid arthritis. Br J Rheumatol. 1989;28(suppl 1):31. | ||
Spector TD, Roman E, Silman AJ. A UK case-control study on the effect of parity and the oral contraceptive pill on the development of rheumatoid arthritis. Br J Rheumatol. 1989;28(suppl 1):32. | ||
Del Junco DJ, Annegers JF, Coulam CB, Luthra HS. The relationship between rheumatoid arthritis and reproductive function. Br J Rheumatol. 1989;28(suppl 1):33. | ||
Hazes JM, Dijkmans BA, Vandenbroucke JP, De Vries RR, Cats A. Oral contraceptives and rheumatoid arthritis; further evidence for a protective effect independent of duration of pill use. Br J Rheumatol. 1989;28(suppl 1):34. | ||
Hazes JM, Silman AJ, Brand R, Spector TD, Walker DJ, Vandenbroucke JP. A case-control study of oral contraceptive use in women with rheumatoid arthritis and their unaffected sisters. Br J Rheumatol. 1989;28(suppl 1):35. | ||
Hannaford PC, Kay CR. Oral contraceptives and rheumatoid arthritis: new data from the Royal College of General Practitioners’ Oral Contraception Study. Br J Rheumatol. 1989;28(suppl 1):36. | ||
Linos A, Kaklamanis E, Kontomerkos A, Vagiopoulos G, Tjonou A, Kaklamanis P. Rheumatoid arthritis and oral contraceptives in the Greek female population: a case-control study. Br J Rheumatol. 1989; 28(suppl 1):37. | ||
Allebeck P, Adami HO, Klareskog L, Persson I. Non-contraceptive hormones and rheumatoid arthritis: possibilities of using a Swedish population-based cohort. Br J Rheumatol. 1989;28(suppl 1):38–40. | ||
Koepsell T, Dugowson C, Voigt L, et al. Preliminary findings from a case-control study of the risk of rheumatoid arthritis in relation to oral contraceptive use. Br J Rheumatol. 1989;28(suppl 1):41. | ||
Greenland S. Quantitative methods in the review of epidemiologic literature. Epidemiol Rev. 1987;9:1–30. | ||
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. | ||
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. | ||
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. | ||
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–1101. | ||
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. | ||
Hamling J, Lee P, Weitkunat R, Ambühl M. Facilitating meta-analyses by deriving relative effect and precision estimates for alternative comparisons from a set of estimates presented by exposure level or disease category. Stat Med. 2008;27(7):954–970. | ||
Vandenbroucke JP. Oral contraceptives and the risk of rheumatoid arthritis: the great transatlantic divide? Scand J Rheumatol Suppl. 1989; 79:31–32. | ||
Vandenbroucke JP, Hazes JM, Dijkmans BA, Cats A. Oral contraceptives and the risk of rheumatoid arthritis: the great transatlantic divide? Br J Rheumatol. 1989;28(suppl 1):1–3. | ||
Esdaile JM. Exogenous female hormones and rheumatoid arthritis: a methodological view of the contradictions in the literature. Br J Rheumatol. 1989;28(suppl 1):4–10. | ||
Spector TD, Hochberg MC. The protective effect of the oral contraceptive pill on rheumatoid arthritis: an overview of the analytical epidemiological studies using meta-analysis. Br J Rheumatol. 1989;28(suppl 1):11–12. | ||
Romieu I, Hernandez-Avila M, Liang MH. Oral contraceptives and the risk of rheumatoid arthritis: a meta-analysis of a conflicting literature. Br J Rheumatol. 1989;28(suppl 1):13–17. | ||
Spector TD, Hochberg MC. The protective effect of the oral contraceptive pill on rheumatoid arthritis: an overview of the analytic epidemiological studies using meta-analysis. J Clin Epidemiol. 1990;43(11): 1221–1230. | ||
Liang MH, Karlson EW. Female hormone therapy and the risk of developing or exacerbating systemic lupus erythematosus or rheumatoid arthritis. Proc Assoc Am Physicians. 1996;108(1):25–28. | ||
Pladevall-Vila M, Delclos GL, Varas C, Guyer H, Brugués-Tarradellas J, Anglada-Arisa A. Controversy of oral contraceptives and risk of rheumatoid arthritis: meta-analysis of conflicting studies and review of conflicting meta-analyses with special emphasis on analysis of heterogeneity. Am J Epidemiol. 1996;144(1):1–14. | ||
Masi AT, Aldag JC, Chatterton RT. Sex hormones and risks of rheumatoid arthritis and developmental or environmental influences. Ann N Y Acad Sci. 2006;1069:223–235. | ||
Vandenbroucke JP. Oral contraceptives and rheumatoid arthritis. Lancet. 1983;322(8343):228–229. | ||
Gandini S, Iodice S, Koomen E, Di Pietro A, Sera F, Caini S. Hormonal and reproductive factors in relation to melanoma in women: current review and meta-analysis. Eur J Cancer. 2011;47(17):2607–2617. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.