Back to Journals » Patient Preference and Adherence » Volume 10
Medication risk communication with cancer patients in a Middle East cancer care setting
Authors Wilbur K, Al Okka M, Jumat E, Eissa N, Elbashir M, Sumaya Al Saadi Al-Yafei S
Received 3 November 2015
Accepted for publication 23 February 2016
Published 22 April 2016 Volume 2016:10 Pages 613—619
DOI https://doi.org/10.2147/PPA.S99718
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Kerry Wilbur,1 Maha Al-Okka,1 Ebaa Jumaat,1 Nesma Eissa,1 Merwa Elbashir,1 Sumaya M Al Saadi Al-Yafei2
1College of Pharmacy, Qatar University, 2Pharmacy Department, National Center for Cancer Care and Research, Doha, Qatar
Purpose: Cancer treatments are frequently associated with adverse effects, but there may be a cultural reluctance by care providers to be forthcoming with patients regarding these risks for fear of promoting nonadherence. Conversely, research in a number of countries indicates high levels of patient desire for this information. We sought to explore cancer patient experiences, satisfaction, and preferences for medication risk communication in a Middle East care setting.
Methods: We developed and administered a ten-item questionnaire (Arabic and English) to a convenience sample of consenting adult patients receiving treatment at the National Center for Cancer Care and Research in Qatar.
Results: One hundred and forty-three patients were interviewed. Most (88%) stated that the level of side effect information they received was sufficient, with physicians (86%) followed by pharmacists (39%) as the preferred sources. The majority (97%) agreed that knowing about possible side effects would help them recognize and manage the reaction, and 92% agreed that it would help them understand how to minimize or prevent the risks. Eighteen percent indicated that this information would make them not want to take treatment. Two-thirds (65%) had previously experienced intolerance to their cancer treatment regimen.
Conclusion: Most patients surveyed expressed preference for the details of possible side effects they may encounter in their treatment. However, one in five considered such information a factor for nonadherence, indicating the need for patient-specific approaches when communicating medication risks.
Keywords: risk communication, cancer treatment, Middle East
Introduction
Communication in cancer care encompasses a host of multifaceted subject matter. Perhaps unlike most other diseases, patients (and often families) must not only contend with the realities of the diagnosis and possible unfavorable prognosis but also digest information related to complex and often debilitating therapies.1,2 Appropriate counseling strategies by multidisciplinary team members are then integral to facilitating information exchange and addressing patient concerns to promote understanding and guide treatment decision making.
While health professionals may inherently recognize the value of good communication, the provision of adequate information to cancer patients has been confirmed in countless studies and includes reports of decreased anxiety and depression, promotion of treatment adherence and self-care, as well as enhanced patient satisfaction with overall management.3–7 Counseling by health care providers regarding the potential adverse effects associated with treatments and the advised management strategy is consistently ranked high in importance by cancer patients.8,9 In a systematic review summarizing 112 studies (conducted in 1980–2003), the most frequently expressed information needed by cancer patients was clinical teaching related to treatment.10 Emotional well-being among cancer survivors has been found to be inversely related to the number of unmet information needs related to side effects and symptoms.6–11 Patients reflecting at the conclusion of cancer treatment have opined that forthright provision of information related to medication intolerances would have decreased their fear associated with chemotherapy.12 However, the desired level of such detail is different across cultures, and very little of this work has been conducted among Arab cancer patients.13–15
The Middle East region is currently undergoing an expansion of specialized oncology treatment centers to address the rising incidence of cancer cases among their populations.16 A variety of different health professionals offer medication counseling (formally and informally) to oncology patients over the course of treatment and recovery. They may share responsibilities to educate cancer patients about medication risks; however, prior studies among oncology nurses and physicians in North America, Europe, and Asia have demonstrated that health professionals may underestimate the amount and nature of information needs of cancer patients.1,9,12,17–20 Reluctance to offer detailed information regarding treatment side effects may arise from fears of aversely influencing patient decision making or provoking nonadherence.21–25 This is especially true among Arab cultures where traditional beliefs and social norms can contribute to avoidance strategies in cancer screening and treatment behaviors, such as a desire to present no weakness or bodily symptoms to family members.26,27 Cancer patients elsewhere express a strong desire for treatment information, but it is unknown if this is consistent in a Middle East context. We sought to explore Qatar cancer patients’ experience and satisfaction with the communication of potential risks associated with their therapy and to elicit their preferences in this regard.
Methods
We conducted a cross-sectional survey to answer these research questions. To identify the development or use of an existing instrument to evaluate risk communication to cancer patients, a comprehensive English language literature review was conducted using pertinent electronic health databases (PubMed, EMBASE, International Pharmaceutical Abstracts [IPA], Cumulative Index to Nursing and Allied Health Literature [CINAHL]) from 1990 to September 2014 and Google and Google Scholar search engines using a combination of predetermined keywords: “medication safety”, “patient preferences/satisfaction”, “risk”, “side/adverse effects”, “education”, “information”, and “counseling”. Online resources of multinational organizations, such as the World Health Organization and various international societies in oncology and cancer care, were verified. Online resources were similarly searched using keywords in Arabic. Hand search of references of retrieved articles was also performed. Reviews or reports outlining cancer patients’ information needs and any research pertaining to health professional treatment risk communication in this regard were evaluated and adapted for development of our questionnaire as no suitable validated instrument could be identified.
Survey questions were structured according to four main domains: subject demographics, patient care experiences, satisfaction, and preferences for receiving information related to the potential intolerances and side effects of their treatment. The draft was then reviewed for face validity by a small working group comprising six pharmacists and a layperson familiar with cancer care. The working group also participated in a structured discriminant content validity process (Table 1).28 Modifications were made based on the feedback provided and consensus reached among all researchers and subject interviewers. Native Arabic speakers fluent in English translated the survey into Arabic (forward translation), and then the document was back translated into English by the first group (who were therefore familiar with English content) and a third native Arabic speaker fluent in English who was blinded to the original English version. Any discrepancies were then reviewed, discussed, and corrected. Reliability testing was conducted for the scale satisfaction and preference responses showing internal consistency of the items tested with Cronbach’s α value of 0.85 and 0.77, respectively.
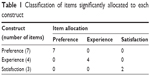  | Table 1 Classification of items significantly allocated to each construct |
A convenience sample of patients aged 16 and older who could communicate in English or Arabic was recruited from the country’s specialty oncology setting, the National Center for Cancer Care and Research (NCCCR). The authors met potential subjects attending follow-up appointments to explain the research, and once verbal consent was obtained, administered the survey. Ethical approval was obtained from institutional review boards of Qatar University and Hamad Medical Corporation. According to the Hamad Medical Corporation ethics board, written consent from the subjects was not necessary for this study.
Categorical data are presented as percentages of frequency or occurrence, and continuous data are presented as mean with standard deviation. For final analysis purposes, any 5-point Likert scale employed was reclassified for those who answered “strongly agree” and “agree” as having agreed and those who answered “strongly disagree” and “disagree” as having disagreed. Specific responses were further stratified according to demographic parameters of nationality, sex, level of education, and age through univariate and multiple regression analyses to examine differences in anticipated adherence behavior when offered treatment risk information (dependent variable). Statistical comparisons of frequencies utilized χ2 tests with α≤0.05 considered statistically significant. All data analyses were conducted using IBM SPSS® (IBM Corporation, Armonk, NY, USA) for Mac release 20.0.
Results
One hundred and forty-five consenting patients completed the questionnaire during an 8-week period, the majority of whom were female (102, 70.3%) and in the daycare setting (139, 95.8%) where the most frequently treated malignancies include leukemia and breast, colorectal, dermatologic, and thyroid cancers (Table 2). Thirty different countries of origin were represented. Most had attended at least high school or more (129, 85.7%) and have been living in Qatar for an average of 13 years. Few (14, 9.7%) were making their first visit to NCCCR for care with an average duration of treatment of 13 months. While all could identify the routes of administration of their therapy, few could name their medications.
The overwhelming majority (144, 99.3%) of patients interviewed reported receiving information related to the possible side effects of their treatment, and almost always (130, 89.6%) from more than one health professional. Patients most often recalled the source as physicians (141, 97.2%), the nurse(s) who administered the medication (88, 60.7%), inpatient (71, 49%) or outpatient (65, 44.8%) pharmacists, or other nurses (34, 23.4%; Figure 1). Half (75, 51.7%) were also provided written medication information. Most (127, 88%) felt that they had received sufficient information according to their own needs and expressed high levels of satisfaction with both the amount of risk information (137, 94.5%) and the manner in which it was communicated (137, 94.5%).
When the quantity of potential adverse events disclosed during an educational encounter was explored, stated preferences varied somewhat according to the region of origin (Table 3). Favored sources of safety information were physicians (142, 98.6%), pharmacists (56, 38.6%), nurses (31, 21.4%), the Internet (6, 4.1%), and family and friends (5, 3.4% each; Figure 1). Almost half identified more than one of these sources, but in 78 (53.7%) cases, only the physician was chosen.
When asked how receiving safety information might influence their behavior, 27 (18.9%) believed that knowing the potential side effects would make them unwilling to take the medication. Some regional differences among patients emerged (37.5% Gulf Coast Corporation vs 15.8% Middle East and North Africa, P=0.029, vs 12.1% Philippines, P=0.030; Figure 2). Further logistic regression analysis failed to identify any statistically significant relationship between any of the a priori identified variables (sex, age, or level of education) on anticipated nonadherence behavior when offered treatment risk information. Among all patients interviewed, 139 (97.2%) and 131 (91.6%), respectively, agreed that drug risk communication would help them minimize and manage any intolerance that could occur.
Ninety-three patients (64%) had previously experienced an adverse effect to their therapy, which included nausea, diarrhea, vomiting, hair loss, numbness, fever, or fatigue. They shared various strategies for management, the most popular being administration of another medication for its treatment or seeking consultation from the emergency department. When those never suffering from a side effect (n=86) were asked how they would approach the situation, the majority indicated that they would seek care from the emergency department (30, 34.8%).
Discussion
Our study found high prevalence of treatment risk counseling at this care site. According to these patients’ reports, practically all could remember receiving medication safety information coupled with highly expressed satisfaction regarding its content and delivery indicating good concordance between perceived information needs and the communication provided. These patients described preference for receiving all or most details of the potential adverse effects associated with their treatment, which is consistent with studies elsewhere, including the few regional findings available. When Saudi Arabian nationals with symptoms suspicious for malignancy who were referred for cancer diagnosis were surveyed, the majority (99%) wanted to know the benefits and adverse effects of therapy.14 Similarly, surveyed Jordanian cancer patients wanted to know everything about their treatments, but rated this somewhat less than knowledge desired regarding their disease status.15
Given the reported satisfaction found in our study sample, it may be opined that at this care setting, Qatar cancer patients received the type of safety information matching their needs, in this case, “all” or “most”. Understanding cancer patient information needs has been a longstanding pursuit among researchers and providers, and various frameworks have been proposed.29,30 Theories on health information needs postulate that a person’s perceived information need may be influenced by goals (eg, purpose of information), context (eg, personal circumstances or values), situation (eg, event or critical incident), and time (eg, in the continuum of care).31 For example, it has been previously described how specific information needs among individual cancer patients can change over time from diagnosis to recovery and remission.32,33 In our particular study population, such needs are likely heterogeneous given that the duration of care since cancer diagnosis ranged from first visit to 8 years and we did not seek out specific diagnostic or prognostic data. Additionally, while our patients reported high satisfaction with health care provider communication, this has been found to be an imperfect surrogate end point for actual desired illness behaviors, such as medication adherence, which we did not take further measures to assess.34
While the majority of patients in our study believed receiving medication safety counseling would facilitate the prevention and management of possible adverse events, we found that health professional concerns about communicating treatment risk and resultant nonadherence, especially among patients from the Gulf Coast Corporation region, are not unfounded. A fundamental responsibility of health care providers is to give timely and appropriate information to patients. Berry et al35 and Knapp et al36 have conducted extensive research related to the nature of and fashion in which side effect information is presented to patients and how these explanations might influence medication adherence. They have largely concluded that personalized information framing benefits positively with both verbal and numeric descriptors (reported as natural frequencies [one in 100] instead of relative terms [10%]) enhances patient understanding.
Physicians as the most preferred information provider is not unusual given a recognized regional patient deference to medical authority.15,37 However, this predilection is incongruent with the patients’ frequent actual care experiences of receiving safety information from nurses (second only to physicians and before pharmacists, but ranked following pharmacists in terms of favored resource). Current perceptions of allied health professionals’ roles and responsibilities, notably those of nurses and pharmacists, are evolving, but still largely trenchant in traditional scripts of service: drug administration and dispensing, respectively.38,39 Interestingly, in a prior study of nurses and pharmacists in this setting, they acknowledged the need for physician-led education at the time of diagnosis and obtaining treatment plan consent, but underscored the significance of their supporting patient counseling and risk communication roles given physicians’ restricted consultation times and opportunity for follow-up contact with patients.40
The low stated instances of web-based resources for cancer treatment and risk information are surprising given reports of information-seeking behavior among cancer patients elsewhere.41 It is possible that as just over half of our subjects had Arabic as the first language, unsuccessful efforts to find cancer-related materials in their native language online were not considered. Low reliance on family for information was similarly unanticipated. Within Middle Eastern Arab families, information, and sometimes decision making, is shared with extended family members.26,27 Interdependence among relatives is also prominent within South East Asian cultures.42 Again, this may be attributed in part to a high level of deference to the judgments of medical personnel (namely, physicians).
Different cultures assign different weights to disclosures regarding cancer diagnosis, prognosis, and treatment.13 The ethnic diversity within our study population highlights how health services and communication must be flexible in order to meet distinct patient needs. Attention to culturally competent cancer care is especially pertinent in developing countries in the Middle East and other regions where both patients and providers from multiple distinct backgrounds converge in care settings. We know that health professionals’ risk communication perspectives can be incompatible with patient information priorities and that these preferences cannot be simply distilled through a uniform cultural characteristic. Instruments have been developed to aid efforts to systematically assess level of individual patient education and information needs, but further exploration of their feasibility of how they would practically support clinician judgments will be of benefit.15,43
A number of limitations to our study merit discussion. First is our survey tool itself; our search at the study outset did not identify a previously validated questionnaire (English and Arabic) suitable for administration in our population, although we did take steps to confirm certain psychometric properties (face and content validity) of items we adopted from other studies and generated ourselves. Another important concern is that while our university researchers distinguished themselves from NCCCR caregivers, the hospital environment for data collection may have contributed to social desirability bias, yielding the high levels of patient satisfaction observed. Our sample population consisted of Arabs and Asians from many backgrounds and is felt to be representative of major ethnic groups residing in Qatar; however, it is also largely from a daycare setting and so we cannot generalize our findings to inpatient subjects who may be more ill or newly diagnosed. Most patients enrolled in our study were not at their first care visit and had been receiving treatment (on average) for a year. We were not observing actual medication counseling encounters and so our data relied on patient memory which could be subject to recall bias over time.
Conclusion
When receiving medication counseling, most surveyed oncology patients at Qatar’s national cancer center expressed preference for the details of possible side effects they may encounter in their treatment, although a proportion acknowledged such information as a potential factor for nonadherence. Physicians were the favored information source, but patients reported receiving risk information from other health care providers and were largely satisfied with the content and its communication.
Acknowledgments
This publication was made possible by the Undergraduate Research Experience Program award (UREP 14-001-3-001) from the Qatar National Research Fund (a member of Qatar Foundation). The statements made herein are solely the responsibility of the authors.
Author contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data, took part in either drafting the article or revising it critically for important intellectual content, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Belvedere O, Minisini A, Ramello M, Sobrero A, Grossi F. Information given to cancer patients on diagnosis, prognosis and treatment: the clinical oncologist’s perspective. Eur J Cancer. 2004;40(12):1850–1854. | ||
Read H, Ladds S, Rhodes B, Brown D, Portlock J. The impact of a supplementary medication review and counselling service within the oncology outpatient setting. Br J Cancer. 2007;96(5):744–751. | ||
Mallinger JB, Griggs JJ, Shields CG. Patient-centered care and breast cancer survivors’satisfaction with information. Patient Educ Couns. 2005;57(3):342–349. | ||
Haris KA. The informational needs of patients with cancer and their families. Cancer Pract. 1998;6(1):39–46. | ||
Husson O, Mols F, van de Poll-Franse LV. The relation between information provision and health-related quality of life, anxiety, and depression among cancer survivors: a systematic review. Otolaryngol Head Neck Surg. 2011;22:761–772. | ||
Kent EE, Arora NK, Rowland JH, Bellizzi KM, Forsythe LP, Hamilton AS. Health information needs and health-related quality of life in a diverse population of long-term cancer survivors. Patient Educ Couns. 2012;89:345–352. | ||
Roberts C, Benjamin H, Chen L, et al. Assessing communication between oncology professionals and their patients. J Cancer Educ. 2005;20:113–118. | ||
Koinberg I, Langius-Eklof A, Holmberg L, Fridlund B. The usefulness of a multidisciplinary educational programme after breast cancer surgery: a prospective and comparative study. Eur J Oncol Nurs. 2006;10(4):273–282. | ||
Piredda M, Rocci L, Gualandi R, Petitti T, Vincenzi B, De Marinis MG. Survey on learning needs and preferred sources of information to meet these needs in Italian oncology patients receiving chemotherapy. Eur J Oncol Nurs. 2008;12(2):120–126. | ||
Rutten LJF, Arora NK, Bakos AD, Aziz N, Rowland J. Information needs and sources of information among cancer patients: a systematic review of research (1980–2003). Patient Educ Couns. 2005;57:250–261. | ||
Keegan THM, Lichtensztajn DY, Kato I, et al; AYA HOPE Study Collaborative Group. Unmet adolescent and young adult cancer survivors information and service needs: a population-based cancer registry study. J Cancer Surviv. 2012;6(3):239–250. | ||
Guleser GN, Tasci S, Kaplan B. The experience of symptoms and information needs of cancer patients undergoing radiotherapy. J Cancer Educ. 2012;27(1):46–53. | ||
Dein S. Explanatory models of and attitudes towards cancer in different cultures. Lancet Oncol. 2004;5(2):119–124. | ||
Al Amri AM. Cancer patients’ desire for information: a study in a teaching hospital in Saudi Arabia. East Mediterr Health J. 2009;15(1):19–24. | ||
Al Qadire M. Jordanian cancer patients’ information needs and information-seeking behaviour: a descriptive study. Eur J Oncol Nurs. 2014;18(1):46–51. | ||
Brown R, Kerr K, Haoudi A, Darzi A. Tackling cancer burden in the middle east: Qatar as an example. Lancet Oncol. 2012;13(11):e501–e508. | ||
Zheng R, Johnson J, Qang Q. A need for cancer patient education from the perspective of Chinese patients and nurses: a comparison study. Support Care Cancer. 2014;22:2457–2464. | ||
Ancel G. Information needs of cancer patients: a comparison of nurses’ and patients’ perceptions. J Cancer Edu. 2012;27(4):631–640. | ||
The Italian Group for the Evaluation of Outcomes in Oncology. Awareness of disease among Italian cancer patients: is there a need for further improvement in patient information? Ann Oncol. 1999;10:1095–1100. | ||
Ruesch P, Schaffert R, Fischer S, et al. Information needs of early-stage prostate cancer patients: within- and between-group agreement of patients and health professionals. Support Care Cancer. 2014;22(4):999–1007. | ||
Uchitome Y, Yamawaki S. Truth-telling practice in cancer care in Japan. Ann N Y Acad Sci. 1997;809:7–16. | ||
Faria SL, Souhami L. Communication with the cancer patient: information and truth in Brazil. Ann N Y Acad Sci. 1997;809:163–171. | ||
Puts MT, Tapscott B, Fitch M, et al. A systematic review of factors influencing older adults’ decision to accept or decline cancer treatment. Cancer Treat Rev. 2015;41(2):197–215. | ||
Harder H, Ballinger R, Langridge C, Ring A, Fallowfield LJ. Adjuvant chemotherapy in elderly women with breast cancer: patients’ perspectives on information giving and decision making. Psychooncology. 2013;22(12):2729–2735. | ||
Wouters H, van Geffen EC, Baas-Thijssen MC, et al. Disentangling breast cancer patients’ perceptions and experiences with regard to endocrine therapy: nature and relevance for non-adherence. Breast. 2013;22(5):661–666. | ||
Cohen M. An integrated view of cultural perceptions of cancer among Arab people in Israel. Health Psychol Rev. 2014;8(4):490–508. | ||
Silbernann M, Hassan EA. Cultural perspectives in cancer care: impact of Islamic traditions and practices in Middle Eastern countries. J Pediatr Hematol Oncol. 2011;33(suppl 2):S81–S86. | ||
Johnston M, Dixon D, Hart J, Glidewell L, Schroder C, Pollard B. Discriminant content validity: a quantitative methodology for assessing content of theory-based measures, with illustrative applications. Br J Health Psychol. 2014;19(2):240–257. | ||
Coulter A, Entwistle V, Gilbert D. Sharing decision with patients: is information good enough? BMJ. 1999;318:318–322. | ||
Dervin B, Nilan M. Information needs and uses. Annu Rev Inf Sci Technol. 1986;21:3–33. | ||
Ormandy P. Defining information need in health-assimilating complex theories derived from information science. Health Expect. 2011;14(1):92–104. | ||
Matsuyama RK, Kuhn LA, Molisani A, Wilson-Genderson MC. Cancer patients’ information needs the first nine months after diagnosis. Patient Educ Couns. 2013;90(1):96–102. | ||
Tan AS, Nagler RH, Hornik RC, DeMichele A. Evolving information needs among colon, breast, and prostate cancer survivors: results from a longitudinal mixed-effects analysis. Cancer Epidemiol Biomarkers Prev. 2015;24(7):1071–1078. | ||
de Haes H, Bensing J. Endpoints in medical communication research, proposing a framework of functions and outcomes. Patient Educ Couns. 2009;24(7):287–294. | ||
Berry DC, Michas IC, de Rosis F. Evaluating explanations about drug prescriptions: effects of varying the nature of information about side effects and its relative position in explanations. Psychol Health. 1998;13(5):767–784. | ||
Knapp P, Gardner PH, McMillan B, Raynor DK, Woolf E. Evaluating a combined (frequency and percentage) risk expression to communicate information on medicine side effects to patients. Int J Pharm Pract. 2013;21(4):226–232. | ||
Kane T. A clinical encounter of east meets WEST: a case study of the productions of ‘American-Style’ doctors in a Non-American setting. Global Stud J. 2009;2(4):12–16. | ||
Wilbur K, Hammuda A, Benilles A. Physician perceptions of pharmacist roles in a primary care setting in Qatar. Global Health. 2012;8:12–15. | ||
Hassan J, Hassan A, King ML. Nursing image in Qatar: past, present, and future. Middle East J Nurs. 2012;6(4):26–28. | ||
Wilbur K, Babiker A, Al-Okka M, Jumaat E, Al-Yafei SM, Nashwan AJ. Risk communication with Arab patients with cancer: a qualitative study of nurses and pharmacists. BMJ Open. 2015;5(4):e006890. | ||
Ofran Y, Paltiel O, Pelleg D, Rowe JM, Yom-Tov E. Patterns of information-seeking for cancer on the internet: an analysis of real world data. PLoS One. 2012;7(9):e45921. | ||
Stanford University School of Medicine [webpage on the Internet]. McBride M Health and Healthcare of Filipino American Elders. Stanford University School of Medicine; 2015. Available from: http://web.stanford.edu/group/ethnoger/filipino.html. Accessed July 6, 2015. | ||
Arraras JI, Kuljanic-Vlasic K, Bjordal K, et al; Group EQoL. EORTC QLQ-INFO26: a questionnaire to assess information given to cancer patients a preliminary analysis in eight countries. Psychooncology. 2007;16(3):249–254. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




