Back to Journals » Patient Preference and Adherence » Volume 11
Medication adherence and persistence in type 2 diabetes mellitus: perspectives of patients, physicians and pharmacists on the Spanish health care system
Authors Labrador Barba E, Rodríguez de Miguel M, Hernández-Mijares A , Alonso-Moreno FJ, Orera Peña ML , Aceituno S, Faus Dader MJ
Received 17 September 2016
Accepted for publication 25 January 2017
Published 4 April 2017 Volume 2017:11 Pages 707—718
DOI https://doi.org/10.2147/PPA.S122556
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Elena Labrador Barba,1 Marta Rodríguez de Miguel,1 Antonio Hernández-Mijares,2,3 Francisco Javier Alonso-Moreno,4 Maria Luisa Orera Peña,1 Susana Aceituno,5 María José Faus Dader6
1Department of Medicine, Mylan, Madrid, 2Department of Endocrinology and Nutrition, Doctor Peset University Hospital, Valencia, 3Department of Medicine, University of Valencia, Valencia, 4Department for Primary Health Care, Centro de Salud Sillería, Toledo, 5Outcomes’10, Castellon, 6Department of Biochemistry and Molecular Biology, Faculty of Pharmacy, University of Granada, Granada, Spain
Objective: A good relationship between diabetes patients and their health care team is crucial to ensure patients’ medication adherence and self-management. To this end, we aimed to identify and compare the views of type 2 diabetes mellitus (T2DM) patients, physicians and pharmacists concerning the factors and strategies that may be associated with, or could improve, medication adherence and persistence.
Methods: An observational, cross-sectional study was conducted using an electronic self-administered questionnaire comprising 11 questions (5-point Likert scale) concerning factors and strategies related to medication adherence. The survey was designed for T2DM patients and Spanish National Health System professionals.
Results: A total of 963 T2DM patients, 998 physicians and 419 pharmacists participated in the study. Overall, a lower proportion of pharmacists considered the proposed factors associated with medication adherence important as compared to patients and physicians. It should be noted that a higher percentage of physicians in comparison to pharmacists perceived that “complexity of medication” (97% vs 76.6%, respectively) and “adverse events” (97.5% vs 72.2%, respectively) were important medication-related factors affecting adherence. In addition, both patients (80.8%) and physicians (80.8%) agreed on the importance of “cost and co-payment” for adherence, whereas only 48.6% of pharmacists considered this factor important. It is also noteworthy that nearly half of patients (43%) agreed that “to adjust medication to activities of daily living” was the best strategy to reduce therapeutic complexity, whereas physicians believed that “reducing the frequency of administration” (47.9%) followed by “reducing the number of tablets” (28.5%) was the most effective strategy to improve patients’ adherence.
Conclusion: Our results highlight the need for pharmacists to build a stronger relationship with physicians in order to improve patients monitoring and adherence rates. Additionally, these findings may help to incorporate greater patient-centeredness when developing management strategies, focusing on adjusting medication regimens to patients’ daily lives.
Keywords: type 2 diabetes mellitus, adherence, persistence, factors, strategies
Introduction
Diabetes is a highly common metabolic disease whose prevalence worldwide has increased in recent decades.1 In 2013, its prevalence was estimated at 8.3%, affecting 382 million people;2 notably, a further increase to 592 million is expected by 2035.3 The estimated prevalence of type 2 diabetes mellitus (T2DM) in Spain is 13.8%, with approximately 6% of the population being undiagnosed.4 Other chronic conditions are common among T2DM patients; most adults with diabetes have at least one comorbid chronic disease,5 and obesity, dyslipidemia and hypertension4,6–8 are the most prevalent.
Diabetes management is mainly aimed at keeping blood glucose levels stable and preventing or delaying development of other medical complications. T2DM patients typically require pharmacotherapy for hyperglycemia control, along with diet and exercise.9,10 In addition to this medication, these patients require pharmacologic therapy for the control of other chronic conditions. As a result, diabetic patients need complex medication regimens. In Spain, poorly controlled T2DM patients are highly prevalent (51.4%), and one of the most important factors associated with poor glycemic control is the complexity of the disease and therapy.11
Correct adherence to prescribed medication is crucial for the control of diabetes and related comorbidities.12 A significant barrier to achieving clinical outcomes, however, is poor medication adherence,13,14 which is associated with increased morbidity, mortality, health care expenditure and hospital admissions.15,16
Nonadherence to medication is a critical problem among patients with chronic diseases, and in this regard, adherence rates of 50% have been reported for long-term therapies.17 Like other chronic conditions, medication adherence in diabetes is considered suboptimal. A recent systematic review found that only a 22.2% of studies reported a good adherence (≥80%) among the diabetic population.18
Several studies have been conducted to understand nonadherence and to identify the determinants associated with it showing that medication adherence is influenced by numerous factors that may be related to patients, medication or environmental issues.19,20 Additionally, results have demonstrated that simplifying medication regimens and improving patient’s motivation and education could be effective strategies to improve adherence.21
Moreover, recent evidence indicates that T2DM patients’ involvement in the disease management may improve adherence to therapy.22 Thus, some studies reported that patients increased their engagement and motivation if they perceived their preferences are considered in the development of management strategies, and consequently, medication adherence and clinical outcomes may improve.23
Different models of health care should be considered in which the patient must play an active role along with health care professionals.24 In this sense, pharmacists contribute significantly to diabetes management by serving as a bridge between patients and physicians and by ensuring the continuing of care which is essential to improve adherence and achieve clinical outcomes.25 Therefore, a good interaction between patients and a health care team comprising physicians, nurses and pharmacists is critical to achieve disease understanding and thereby improve patients’ adherence and self-management.
Nevertheless, it has been recently proved that patients and physicians under the Spanish National Health System (NHS) have different views concerning diabetes medical management.26 In addition to this, there is enough evidence to suggest that patients and health care professionals may have different perceptions of adherence.27,28
Due to these reasons, in order to improve strategies for better adherence to medication, it is necessary to understand the perspective of both patients and health care professionals. To this end, a real-world survey was designed to obtain the views and opinions of patients, physicians and pharmacists and to identify the differences between these three groups related to the factors associated with medication adherence and persistence and the strategies which may improve them from the Spanish NHS perspective.
Research design and methods
The present study involved a cross-sectional, electronic self-administered survey on patients, physicians and pharmacists working in the Spanish Public NHS.
The study protocol was approved by the Clinical Research Ethics Committee of the Hospital Universitario Puerta del Hierro Majadahonda (Madrid, Spain) approval number Acta nº 308, dated March 9, 2015, and written informed consent was obtained from all participants before their inclusion in the study.
Participants
A sample size of 1,036 T2DM patients was calculated based on the general adult population in Spain (N=38,581,569)29 and recent data on the prevalence of T2DM patients (13.8%).4 In addition, the sample size for physicians (N=1,005) and pharmacists (N=875) was calculated according to the number of physicians (primary care [PC]: N=28,498, endocrinology: N=879 and internal medicine: N=3,357)30 and pharmacists (N=18,628)31 practicing in the Spanish NHS. Sample size was estimated by assuming the maximum variability criterion, with a confidence level of 95% and a precision of 4%. Recruitment was conducted from June 2015 to September 2015, until the desired sample size was achieved.
Patients
Adult T2DM patients with at least one comorbidity associated to diabetes such as obesity, hypertension and/or dyslipidemia and who were able to provide appropriate answers to the survey questions were eligible to participate in the study. Patient selection was conducted with support from the Spanish Diabetes Federation (FEDE: Federación de Diabéticos Españoles).
Members of other societies belonging to the FEDE from 17 autonomous communities were invited to participate.
Physicians
Physicians were eligible to participate if they have been practicing medicine in the Spanish Public NHS for at least 5 years post-training residency. In addition, they had to provide their informed consent.
Pharmacists
To be eligible for participation, the pharmacists had to be managers or employees of a pharmacy for at least 5 years. In addition, they had to provide their informed consent.
Study variables
Sociodemographic variables (age, gender, place of residence) were obtained for all participants.
Education level, employment status and clinical variables such as time since T2DM diagnosis, type and duration of medication and comorbidities (hypertension, dyslipidemia and obesity) and their treatment were recorded exclusively for T2DM patients.
Physicians also reported their medical specialty, area of health care and the estimated number of T2DM patients seen per month. Furthermore, pharmacists reported the pharmacy area and approximate number of T2DM patients attended per month.
A version of the Morisky Medication Adherence Scale (MMAS-4) validated for Spanish population was used to evaluate adherence.32
Survey design
An ad hoc electronic-based survey consisting of 11 questions was designed for patients, physicians and pharmacists based on the information obtained from a review of the literature. The survey was structured into two parts: 1) factors associated with adherence to and persistence with T2DM medication and 2) strategies to improve T2DM medication adherence and persistence. All questions were scored using a 5-point Likert scale (Table 1). The answers reflected T2DM patients’ self-perception in addition to the perception of physicians and pharmacists about their T2DM population. Patients were allowed to answer by phone in case of limited access to internet.
  | Table 1 Ad hoc self-administered survey used in the study |
Statistical analysis
A descriptive analysis using SPSS version 19.0 was applied. Categorical variables were described as absolute and relative frequencies, whereas central tendency and dispersion were reported for quantitative variables. The Chi-square test was applied to compare the scores distribution obtained for each question between the different groups. For all tests, statistical significance was set at P<0.05. In order to simplify the analysis, a 3-point Likert scale was used instead of a 5-point Likert scale, for which we merged some responses (Not at all important/Somewhat important) and (Important/Very important).
Results
Description of the participants
A total of 963 patients, 998 physicians and 419 pharmacists distributed across 17 Spanish autonomous communities participated in the study and were included in the analysis.
The clinical characteristics of T2DM patients and the sociodemographic characteristics of all participants (patients, physicians and pharmacists) are described in Table 2.
Patients’ mean age was 60.4 (standard deviation [SD]: 15.5) years, and approximately half of the study subjects were female (50.1%). Of the total participants, 22% (n=212) had college education, and 43.3% (n=417) were retired when the survey was conducted. The mean time since T2DM diagnosis was 11.3 (SD: 8.9) years. All patients were treated with prescribed medication for their diabetes. Mean time from medication start was 10.5 (8.2) years. Of the total, 88.5% (n=852) received oral medication, while 27.5% were receiving combined therapy (oral + injectable).
Of the total physicians, 68.8% (n=687) were male with a mean age of 52.8 (SD: 7.9) years. Overall, 80.9% (n=805) of participants were PC physicians and had been practicing medicine for a median of 26 (range 19–32) years. Participants reported seeing a median of 90 (range 50–150) T2DM patients per month.
Finally, pharmacists’ mean age was 43.9 (SD: 9.9) years, and only 28.4% (n=119) were male. Participants reported practicing pharmacy for a median of 17 (range 10–25) years, and 45.7% (n=192) indicated seeing more than 100 T2DM patients per month.
Adherence and persistence
Morisky–Green questionnaire results showed that more than half of T2DM patients who participated in the study (65.4%; 95% confidence interval [CI]: 62.4–68.4) reported taking their medication correctly. In line with this data, most physicians (86.3%; 95% CI: 84–88.3) and pharmacists (84.6%; 95% CI: 80.8–87.8) believed that more than half of patients adhered to their medication.
Questionnaire scores
Factors associated with adherence to and persistence with T2DM medication
Comparing patients’, physicians’ and pharmacists’ scores, statistically significant differences were found for all the questions evaluated (P<0.001).
Related to patients’ characteristics
The relative importance given to different factors related to patient’s characteristics which may influence T2DM medication adherence and persistence is shown in Table 3. Overall, both patients and physicians shared the view that patients’ characteristics are important factors for medication adherence. However, the proportion of pharmacists who deemed these features important was lower compared to the other groups. As an example, most patients (85.5%) and physicians (84.5%) answered that patient–clinician decision making was an important factor for adherence to medication, while only 47.3% of pharmacists considered this factor important. Interestingly, compared to other groups, a higher percentage of physicians (72.3%) perceived that patients’ environmental characteristics like “a family member or patient’s friend has the condition” were important compared with the patients themselves (55.4%) and pharmacists (53.1%).
  | Table 3 Importance given to patients’ characteristics |
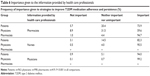
Related to medication and disease characteristics
Results showed that in general, physicians gave greater importance to medication and disease features compared to patients and pharmacists (Table 4). Among these results, it should be noted that a significantly higher percentage of physicians in comparison to pharmacists perceived that “complexity of medication administration” (97% vs 76.6%, respectively) and “adverse events” (97.5% vs 72.2%, respectively) were important medication-related factors affecting adherence. In addition, both patients (80.8%) and physicians (80.8%) agreed on the importance of “cost and co-payment” for adherence; nevertheless, only 48.6% of pharmacists considered this factor important. Similarly, most patients and physicians indicated that an “asymptomatic disease” (80.7% and 87%, respectively) and an “absence of disease complications” (80.6% and 80%, respectively) were important disease-related factors for adherence, while only 60% of pharmacists agreed with these statements.
  | Table 4 Importance given to medication and disease characteristics |
Related to health care professionals’ characteristics
Table 5 reports the relative importance placed by patients, physicians and pharmacists on different factors related to health care professionals’ characteristics. In this respect, it should be noted that a higher percentage of pharmacists perceived their characteristics were important compared to patients and physicians. As an example, 75.1% of pharmacists thought that “coordination between physicians and pharmacists” was important for medication adherence. Nonetheless, only 55% of physicians agreed with this statement. Similarly, the results showed that the majority of pharmacists indicated that their own motivation (91.5%), attitude (94.2%) and relationship with patients (85.3%) were important factors influencing adherence, whereas the proportion of physicians who deemed these factors important was significantly lower (57.3%, 62.3% and 52.9%, respectively).
Strategies to improve T2DM medication adherence and persistence
Statistically significant differences between patients’, physicians’ and pharmacists’ scores were found for all questions evaluating the importance given to strategies which may improve adherence and persistence (P<0.001).
Information provided by health care professionals
Consistent with results described, the majority of pharmacists (94.7%) believed that the information they provide to patients about medication is important. Conversely, a lower percentage of physicians (59.6%) perceived that this information contributes significantly to medication adherence and compliance. In addition, most physicians (99.2%) believed that the information they give to patients about medication along with nurses (95.5%) is important to improve patients’ adherence (Table 6).
However, when physicians’ and patients’ preferences regarding the information pathways were compared, physicians showed a higher predilection for oral (41.6% physicians vs 35.9% patients), written (36.2% physicians vs 30.4% patients) and group education (14.6% physicians vs 4% patients) to provide information to their patients, while patients showed a greater preference for communication over the phone (2.7% patients vs 0.3% physicians), email (10% patients vs 2.1% physicians) or home visits (8.8% patients vs 0.6% physicians) (P<0.001).
Complexity of the therapeutic regimen
Physicians believed that reducing the frequency of administration (47.9%) followed by reducing the number of tablets (28.5%) was the most effective strategy to improve patients’ adherence. However, a high percentage of patients (43%) thought that adjusting medication regimen to activities of daily living was the best strategy to improve their medication adherence, and only 15.5% of them considered a reduction in the frequency of medication administration as an effective strategy (Figure 1).
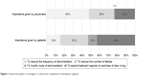  | Figure 1 Importance given to strategies to reduce the complexity of therapeutic regimen. |
Other techniques
Finally, the questionnaire showed that both pharmacists and physicians agreed on the effectiveness of pill dispensers (81.7% and 77.6%, respectively) and tablet counting (57.6% and 52.2%, respectively) in improving patients’ adherence. However, in the patients’ opinion, accomplishing medication schedules (66.9%) and reminders given over telephone, by mail or email (47.1%) were the most effective strategies to improve their medication adherence. Moreover, physicians were the group of participants who gave greatest importance to mobile applications (53.4%) for improving medication adherence in contrast with pharmacists (34.2%) or patients (45.3%). Surprisingly, “family and friends involvement in patient’s disease” was considered less important by patients (70.6%) compared to physicians (96.1%) and pharmacists (90.3%) (Table 7).
Discussion
The present study gathered opinions from patients, physicians and pharmacists about the factors and the strategies which may improve adherence to medication for the treatment of diabetes and other related chronic diseases. The views expressed by the three groups were consistent in various aspects; however, several differences were identified.
A high proportion of physicians and pharmacists considered that more than a half of patients adhere to their medication. In agreement with these considerations, almost two-third of T2DM patients reported good adherence. These results show that, in general, both physicians and pharmacists were able to estimate how well the patient is adhering to the medication. In addition, the rate of nonadherence reported in the study (34.6%) is similar to that reported in a previous study conducted in Spain.33
To achieve good medication adherence, the majority of patients considered it “important” to have knowledge about their disease and medication. Moreover, most subjects placed great importance on disease features such as chronicity, the presence of comorbidities or complications. These findings suggest that the majority of patients with T2DM diabetes interviewed understand the importance of taking medication and at the same time acknowledge the importance of being adequately informed about their disease, comorbidities and the benefits of medication.
The study showed that patients considered their relationship with physicians and their participation in the medication decision-making process very important for improving adherence. Supporting this idea, a recent observational study showed that insulin adherence was directly correlated with physician attention and engagement.34 This result emphasizes the need for integrating patients’ perspectives in the development of care planning and decision making, in order to increase their motivation and consequently their medication adherence.35
As previously reported36 and in accordance to our findings, patients’ and physicians’ opinions and perspectives concerning medication adherence differed to some extent. Thus, related to the strategies aimed at improving adherence, nearly half of patients agreed that to adjust their medication regimen to activities of daily living was the best strategy to reduce therapeutic complexity, in contrast to physicians who believed that reducing the frequency of administration followed by reducing the number of tablets was the most effective strategy to improve patients’ adherence.
The present findings are also consistent with previous studies, in which PC physicians and specialists emphasized the need to lower the number of daily diabetic medications to improve patients’ adherence, clinical outcomes and quality of life,37 whereas T2DM patients considered adjusting medication regimen to their daily lives more essential,22 stating that a more flexible dosing regimen that could be adapted to them would be an effective strategy to improve their adherence to antidiabetic therapy.
Our descriptive analysis is the first, to our knowledge, in which not only patients’ and physicians’ but also pharmacists’ perceptions in relation to medication adherence were elicited and compared. We believe that the present results provide a more comprehensive view of patients and health care professionals. In this sense, our results highlight that this group of professionals show significant differences in comparison with the other two groups of participants. Interestingly, we found many similarities between patients’ and physicians’ responses concerning adherence, while pharmacists’ view on patients’ adherence and their own role in patient care differed significantly from those reported by the other two groups. As an example, a lower percentage of pharmacists were of the opinion that specific disease and medication features were important for medication adherence compared to patients and physicians.
These results were unexpected as pharmacists perform closer patient monitoring than physicians and are aware of the occurrence of adverse events and patients’ comorbidities.38 In addition, our results show that a higher proportion of pharmacists believed that the role they play in managing patient adherence is important in comparison with patients and physicians. Previous studies have shown a more positive view of patients about pharmacists, in the sense, that patients believed that a multidisciplinary approach including pharmacists as the main actors together with physicians could improve diabetes management, especially in cases of clinical complexity, multi-morbidity and polymedication.39
This observational study has some inherent limitations in terms of its susceptibility to bias and confounding, restricting its ability to define causality.40 Another important aspect to consider is related to the lack of objective variables such as glycemic control and the absence of a direct measure of medication adherence. However, the method applied (MMAS-4) has been widely used and validated in Spanish patients with chronic diseases.
Additionally, sample size was calculated to be representative of each group of participants, and recruitment was performed in an independent and unbiased manner supported by important organizations (Spanish Diabetes Federation and the RedGDPs – Spanish Physician Association). However, participants might not represent the whole population. In addition, the possibility that some questions may have been misinterpreted cannot be ruled out.
The final limitation concerns the lack of validation of the questionnaire. Hence, the findings obtained in the present study should be interpreted with some caution.
Despite the limitations outlined, this study has several strengths such as the large number of participants included and the relevant information related to daily clinical practice in Spain.
Conclusion
The present study offers useful information about T2DM patients’, physicians’ and pharmacists’ views on medication adherence, providing useful insights into highly influential aspects in medical decision making within the NHS.
According to our results, health care professionals should acknowledge patients’ opinions and preferences in the development of medication management strategies, focusing on adjusting medication dosages and timing to patients’ daily lives in order to improve their adherence. Thus, our results suggest that the most effective way to manage poor adherence is to identify patients’ barriers to medication compliance and to implement strategies that are specific to overcome those barriers instead of the classical approach of simplifying a complex medication regimen. It is important to highlight that this strategy coincides with the one recommended by the most recent guidelines for diabetes care.41
Importantly, a major barrier to optimal adherence management has been previously identified as a fragmented and poorly coordinated health system.42 In this regard, our study acknowledges the need for pharmacists to build a stronger relationship with patients and physicians in order to work closely in designing, implementing and monitoring therapeutic plans to improve adherence rates, especially when treating diabetes patients with clinical complexity, multi-morbidity and polymedication.
Acknowledgments
The authors would like to thank all the physicians who participated in this study, the technical coordination of Outcomes’10 and Ana López Fernández (Mylan, Spain). This study was funded by Mylan. This study is part of the doctoral thesis of Elena Labrador within the Doctoral Program in Pharmacy, University of Granada, Granada, Spain.
Disclosure
The authors report no conflicts of interest in this work.
References
Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94(3):311–321. | ||
International Diabetes Federation. IDF Diabetes Atlas – 6th Edition. 2013. Available from: http://www.idf.org/diabetesatlas. Accessed July 1, 2016. | ||
Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014;103(2):137–149. | ||
Soriguer F, Goday A, Bosch-Comas A, et al. Prevalence of diabetes mellitus and impaired glucose regulation in Spain: the [email protected] Study. Diabetologia. 2012;55(1):88–93. | ||
Bae S, Rosenthal MB. Patients with multiple chronic conditions do not receive lower quality of preventive care. J Gen Intern Med. 2008;23(12):1933–1939. | ||
Suh DC, Choi IS, Plauschinat C, Kwon J, Baron M. Impact of comorbid conditions and race/ethnicity on glycemic control among the US population with type 2 diabetes, 1988–1994 to 1999–2004. J Diabetes Complications. 2010;24(6):382–391. | ||
Suh DC, Kim CM, Choi IS, Plauschinat CA, Barone JA. Trends in blood pressure control and treatment among type 2 diabetes with comorbid hypertension in the United States: 1988–2004. J Hypertens. 2009;27(9):1908–1916. | ||
Jellinger PS, Smith DA, Mehta AE, et al; AACE Task Force for Management of Dyslipidemia and Prevention of Atherosclerosis. American Association of Clinical Endocrinologists’ guidelines for management of dyslipidemia and prevention of atherosclerosis. Endocr Pract. 2012;18 (Suppl 1):1–78. | ||
King DE, Mainous AG, Carnemolla M, Everett CJ. Adherence to healthy lifestyle habits in US adults, 1988–2006. Am J Med. 2009;122(6):528–534. | ||
American Diabetes Association. Standards of medical care in diabetes–2013. Diabetes Care. 2013;36 (Suppl 1):S11–S66. | ||
Pérez A, Mediavilla JJ, Miñambres I, González-Segura D. Glycemic control in patients with type 2 diabetes mellitus in Spain. Rev Clin Esp. 2014;214(8):429–436. | ||
Bailey CJ, Kodack M. Patient adherence to medication requirements for therapy of type 2 diabetes. Int J Clin Pract. 2011;65(3):314–322. | ||
Ho PM, Rumsfeld JS, Masoudi FA, et al. Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med. 2006;166(17):1836–1841. | ||
Currie CJ, Peyrot M, Morgan CL, et al. The impact of treatment noncompliance on mortality in people with type 2 diabetes. Diabetes Care. 2012;35(6):1279–1284. | ||
Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43(6):521–530. | ||
Egede LE, Gebregziabher M, Dismuke CE, et al. Medication nonadherence in diabetes: longitudinal effects on costs and potential cost savings from improvement. Diabetes Care. 2012;35(12):2533–2539. | ||
World Health Organization. Adherence to long-term therapies. Evidence for action. 2003. Available from: http://www.who.int/chp/knowledge/publications/adherence_full_report.pdf. Accessed July 1, 2016. | ||
Krass I, Schieback P, Dhippayom T. Adherence to diabetes medication: a systematic review. Diabet Med. 2015;32(6):725–737. | ||
Spain CV, Wright JJ, Hahn RM, Wivel A, Martin AA. Self-reported barriers to adherence and persistence to treatment with injectable medications for type 2 diabetes. Clin Ther. 2016;38(7):1653–1664.e1. | ||
Saundankar V, Peng X, Fu H, et al. Predictors of change in adherence status from 1 year to the next among patients with type 2 diabetes mellitus on oral antidiabetes drugs. J Manag Care Spec Pharm. 2016;22(5):467–482. | ||
Tiktin M, Celik S, Berard L. Understanding adherence to medications in type 2 diabetes care and clinical trials to overcome barriers: a narrative review. Curr Med Res Opin. 2016;32(2):277–287. | ||
McSharry J, McGowan L, Farmer AJ, French DP. Perceptions and experiences of taking oral medications for the treatment of type 2 diabetes mellitus: a systematic review and meta-synthesis of qualitative studies. Diabet Med. 2016;33(10):1330–1338. | ||
Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycaemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2012;55(6):1577–1596. | ||
Hobbs JL. A dimensional analysis of patient-centered care. Nurs Res. 2009;58(1):52–62. | ||
Antoine SL, Pieper D, Mathes T, Eikermann M. Improving the adherence of type 2 diabetes mellitus patients with pharmacy care: a systematic review of randomized controlled trials. BMC Endocr Disord. 2014;14:53. | ||
Franch-Nadal J, Labrador Barba E, Gómez-García MC, Buil-Cosiales P, Millaruelo JM, Peña ML. Patient-reported outcomes in type 2 diabetes mellitus: patients’ and primary care physicians’ perspectives in the Spanish health care system. Patient Prefer Adherence. 2015;9:1413–1422. | ||
Zeller A, Taegtmeyer A, Martina B, Battegay E, Tschudi P. Physicians’ ability to predict patients’ adherence to antihypertensive medication in primary care. Hypertens Res. 2008;31(9):1765–1771. | ||
Kekäle M, Talvensaari K, Koskenvesa P, Porkka K, Airaksinen M. Chronic myeloid leukemia patients’ adherence to peroral tyrosine kinase inhibitors compared with adherence as estimated by their physicians. Patient Prefer Adherence. 2014;8:1619–1627. | ||
Instituto Nacional de Estadística (INE). Estimaciones de la población actual de España a 1 de enero de 2012 [Estimates of the current population of Spain as of January 1, 2012]. Available from: http://www.ine.es/jaxiT3/Tabla.htm?t=9663&L=0. Accessed July 1, 2016. Spanish. | ||
Ministerio de Sanidad, Política Social e Igualdad. 2011. Informe sobre oferta y necesidad de especialistas médicos en España (2010–2025) [Report on supply and need of medical specialists in Spain (2010–2025)]. 2011. Available from: http://www.msps.es/novedades/docs/OfYneceEspMedicos_ESP_2010_2025_03.pdf. Accessed July 1, 2016. Spanish. | ||
Consejo General de Colegios Oficiales de Farmacéuticos. Estadísticas de Colegiados y Farmacias Comunitarias [statistical data on collegiate and community pharmacies]. 2013. Available from: http://www.portalfarma.com/profesionales/infoestadistica/Paginas/default.aspx. Accessed July 1, 2016. Spanish. | ||
Val Jiménez A, Amorós Ballestero G, Martínez Visa P, Fernández Ferré ML, León Sanromà M. Estudio descriptivo del cumplimiento del tratamiento farmacológico antihipertensivo y validación del test de Morisky y Green [Descriptive study of patient compliance in pharmacologic antihypertensive treatment and validation of the Morisky and Green test]. Aten Primaria. 1992;10(5):767–770. Spanish [with English abstract]. | ||
López-Simarro F, Brotons C, Moral I, et al. Inercia y cumplimiento terapéutico en pacientes con diabetes mellitus tipo 2 en atención primaria [Inertia and treatment compliance in patients with type 2 diabetes in primary care]. Med Clin (Barc). 2012;138(9):377–384. Spanish [with English abstract]. | ||
Linetzky B, Jiang D, Funnell MM, Curtis BH, Polonsky WH. Exploring the role of the patient-physician relationship on insulin adherence and clinical outcomes in type 2 diabetes: insights from the MOSAIc study. J Diabetes. Epub 2016 Jul 1. | ||
Thomas J, Iyer NN, Collins WB. Associations between perceived chronic care quality, perceived patient centeredness, and illness representations among persons with diabetes. J Healthc Qual. 2014;36(5):50–59. | ||
Liguori Y, Murase K, Hamamura M. Differences between patient and physician opinions on adherence to medication for hypertension and diabetes mellitus. Curr Med Res Opin. 2016;32(9):1539–1545. | ||
Piercy J, Milligan G, Davies MJ, et al. The relationship between glucose-lowering medications, adherence, and outcomes in patients with type 2 diabetes. Value Health. 2015;18(7):A343. | ||
Pousinho S, Morgado M, Falcão A, Alves G. Pharmacist interventions in the management of type 2 diabetes mellitus: a systematic review of randomized controlled trials. J Manag Care Spec Pharm. 2016;22(5):493–515. | ||
McCann LM, Haughey SL, Parsons C, et al. A patient perspective of pharmacist prescribing: ‘crossing the specialisms-crossing the illnesses’. Health Expect. 2015;18(1):58–68. | ||
Yang W, Zilov A, Soewondo P, Bech OM, Sekkal F, Home PD. Observational studies: going beyond the boundaries of randomized controlled trials. Diabetes Res Clin Pract. 2010;88 (Suppl 1):S3–S9. | ||
ADA. Standards of medical care in diabetes-2016. Diabetes Care. 2016;39 (Suppl 1):S1–S112. | ||
Stellefson M, Dipnarine K, Stopka C. The chronic care model and diabetes management in US primary care settings: a systematic review. Prev Chronic Dis. 2013;10:E26. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.