Back to Journals » Journal of Pain Research » Volume 12
Medical record-based ascertainment of behaviors suggestive of opioid misuse, diversion, abuse, and/or addiction among individuals showing evidence of doctor/pharmacy shopping
Authors Esposito DB, Cepeda MS , Lyons JG, Yin R, Lanes S
Received 30 January 2019
Accepted for publication 24 May 2019
Published 24 July 2019 Volume 2019:12 Pages 2291—2303
DOI https://doi.org/10.2147/JPR.S203350
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Katherine Hanlon
Daina B Esposito,1 M Soledad Cepeda,2 Jennifer G Lyons,1 Ruihua Yin,1 Stephan Lanes1
On behalf of The Members of the Opioid Post-Marketing Consortium Observational Studies Working Group
1Department of Safety and Epidemiology, HealthCore, Inc, Wilmington, DE, USA; 2Department of Research and Development, Janssen, Titusville, NJ, USA
Objectives: Doctor/pharmacy shopping, the practice of seeking prescriptions from multiple healthcare sources without their coordination, may be a measure of prescription medicine abuse. This cross-sectional study examined the relationship between a claims-based doctor/pharmacy shopping definition and medical record documented behaviors suggestive of misuse, diversion, abuse and/or addiction.
Methods: Patients with ≥2 opioid dispensings starting in 2012 in a US administrative claims database were grouped into doctor/pharmacy shopping categories by number of providers and pharmacies used over 18 months: no shopping, minimal shopping, moderate shopping and severe shopping. Medical charts of opioid prescribers were reviewed to identify behaviors suggestive of misuse, diversion, abuse and/or addiction.
Results: Among 581,940 opioid users, 78% were classified as no shopping, 11% minimal shopping, 8% moderate shopping and 3% severe shopping. Almost 40% of severe shopping patients had no medical record documented behaviors (positive predictive value: 24.3%). Compared with no shopping, the odds ratio [OR] of ≥3 behaviors was 1.70 (95% confidence interval [CI] 0.50–5.78) for minimal shopping, 1.81 (95% CI 0.54–6.03) for moderate shopping, and 8.93 (95% CI 3.12–25.54) for severe shopping.
Conclusions: Claims-identified severe doctor/pharmacy shopping was strongly associated with behaviors suggestive of misuse, diversion, abuse and/or addiction, but the proportion of medical records documenting these was low.
Keywords: opioid, doctor/pharmacy shopping, abuse, misuse, addiction
Introduction
When applied to drugs with potential for abuse, the term “doctor/pharmacy shopping” refers to a patient’s practice of seeking prescriptions from multiple prescribers without their coordination or knowledge.1,2
Risk factors for doctor/pharmacy shopping include age (as the practice is less common in patients ≥65 years of age); concurrent use of benzodiazepines; and diagnoses of mood disorders, back pain, and abuse of non-opioid drugs.3–6 Malignancy-related pain is negatively correlated with shopping behavior.4 A previous study reported that almost 20% of patients exhibiting possible doctor/pharmacy shopping visited more than one state to obtain their prescriptions, whereas only 4% of patients with no shopping behavior did so.5 Patients in the doctor/pharmacy shopping category were more likely to pay fully in cash for prescription opioids than those in the no shopping category (44% vs 18%, respectively).6
Possible doctor/pharmacy shopping is associated with opioid misuse and abuse.7,8 When defined as overlapping prescriptions written by at least two prescribers and filled in at least three pharmacies, shopping behavior was ten times more likely to occur in patients with evidence of opioid abuse than in patients without such evidence (odds ratio [OR] 9.6; 95% confidence interval [CI], 7.9–11.8).4
The United States (US) Food and Drug Administration (FDA) has instituted post-marketing requirements (PMR) for extended-release and long-acting (ER/LA) opioid manufacturers that include refinement of measures for assessing opioid harm. One focus of the program is to improve the understanding of doctor/pharmacy shopping as a measure of misuse, abuse, addiction and diversion. In a recent study conducted as part of the PMR, having three or more prescribers and three or more dispensing pharmacies over an 18-month time period was shown to differentiate between courses of treatment with opioids and courses of treatment with diuretics.7 Diuretics were included in this study as a control/baseline group as they are not likely to be abused, therefore prescriptions obtained from multiple providers or dispensed via multiple pharmacies would not be indicative of abuse, misuse, addiction or diversion.7
The purpose of this study was to examine the relation between doctor/pharmacy shopping and behaviors suggestive of misuse, abuse and/or diversion described in medical records of opioid prescribers, and to determine whether the doctor/pharmacy shopping category may serve as a measure of these behaviors where opioid use disorders are not documented in administrative claims.
Materials and methods
The association between possible doctor/pharmacy shopping and behaviors suggestive of misuse, diversion, abuse, and/or addiction was examined using data from the HealthCore Integrated Research Database (HIRD), an insurance/health plan claims database that can be linked to medical records. While claims-based patterns of opioid dispensing do not capture patient intent or lack of coordination across care settings, the term “doctor/pharmacy shopping” will be used here to refer to the number of pharmacies and prescribers that the patient used to access opioids.
Data source
The HIRD is a large administrative healthcare database with longitudinal medical and pharmacy claims data from health plan members across the continental US. Member enrollment, medical care (professional and facility claims), outpatient prescription drug use, outpatient laboratory test result data, and healthcare utilization may be tracked for health plan members in the database dating back to January 2006. For the subset of patients who are fully-insured, meaning that risk for patient insurance costs is held by the health plan contributing data to the HIRD rather than by an employer group for which only administrative services are offered by the contributing health plan, the HIRD can be linked by patient identifiers to complementary data sources, including inpatient and outpatient medical records from healthcare providers. As of July 2014, the database contained approximately 36.1 million lives with medical and pharmacy eligibility, of which 8.5 million were currently active. Additional information concerning the HIRD is available in Table S1.
Population
Patients who met the following entrance criteria were eligible to be selected for medical record review.
Inclusion
- Patients 18 years or older on the date of the first immediate release (IR) or ER/LA opioid dispensing (ie, an opioid prescription of any dose or duration that was filled by the patient at a pharmacy) that occurred in 2012.
- Patients with at least two dispensed opioids (IR or ER/LA) within 18 months, with at least one dispensing occurring in 2012.
- Continuous, fully-insured enrollment with medical and pharmacy eligibility for at least six months prior to the first IR or ER/LA opioid dispensing.
- Continuous enrollment for 18 months following the first opioid dispensing in 2012, unless truncated by a claims-identified death.
Exclusion
- Patients who could not be classified into one of the four doctor/pharmacy shopping categories (described below).
- Patients for whom no medical records could be accessed.
- Patients with a known history of abuse were identified through the administrative claims data, because it is not permissible to access their medical records due to rules restricting the identification of these patients. While excluded from medical record review, these individuals were included as having an outcome of interest in sensitivity analyses so that individuals with either medical record-based or claims-based indications of problem use are captured as a composite. Codes used to define this exclusion are presented in Table S2.
For patients included in the study population, we defined the first recorded dispensing of an IR or ER/LA opioid in 2012 as the index date. The baseline period included all data from at least six months prior to the index date. The follow-up period during which we assessed possible doctor/pharmacy shopping behavior included the first 18 months following the index date (or all available months until date of death for patients who died).
Possible doctor/pharmacy shopping
Patients were assigned to one of four categories of possible doctor/pharmacy shopping using a published definition based on the total number of prescribers (ie, healthcare providers with a prescriber listed on an opioid dispensing) and pharmacies where patients obtained opioids over an 18-month period.7
- 1 or 2 prescribers AND 1 or 2 pharmacies OR
- 1 prescriber and >2 pharmacies OR
- >2 prescribers and 1 pharmacy
- 2 prescribers AND >2 pharmacies OR
- 3 or 4 prescribers AND 2 pharmacies
- 3 or 4 prescribers AND >2 pharmacies OR
- >4 prescribers AND 2 pharmacies
- >4 prescribers AND >2 pharmacies
Medical record abstraction
A random sample of patients meeting all entrance criteria was selected based on possible doctor/pharmacy shopping category, and medical records were requested from all providers who prescribed an opioid that was subsequently dispensed for each selected patient. Patients with at least one medical record obtained and abstracted were included in the main analyses.
Study size
Target sample sizes within each doctor/pharmacy shopping category (ie, 115 with no shopping, 139 with minimal shopping, 147 with moderate shopping, and 189 with severe shopping) were selected based on prior expectations about the prevalence of misuse, abuse, addiction and diversion in higher and lower risk patients.9–11 This sample size was sufficient to detect a trend in prevalence of misuse, diversion, abuse and/or addiction across categories of increasing shopping intensity using a Cochran-Armitage trend test even if the prevalence was only one fifth as common as expected.
Behaviors suggestive of misuse or abuse
A pre-specified list of behaviors suggestive of misuse or abuse was created through abstraction of all available medical records from an opioid prescriber during the 18-month follow-up period. These items were selected on the basis of literature review,9–27 consultation with clinical experts, and discussion with the FDA. Categories included laboratory findings; observed clinical consequences of opioid abuse; unusual healthcare utilization; inappropriate dose, source or route of administration; explicit reference to misuse, diversion, abuse and/or addiction; and risk factors. Full details concerning how each behavior was defined are shown in Table S3.
Patient characteristics
We assessed patient characteristics separately during the baseline and follow-up periods. The following covariates were ascertained using administrative data in the HIRD: age in years, gender, geographic region of residence, type of opioids used (IR, ER/LA or a combination), count of opioid dispensings, duration of opioid use (days), psychiatric comorbidities (alcoholism, anxiety disorder, bipolar disorder, history of suicide attempt, post-traumatic stress disorder, sleep disorder, and somatoform disorder), pain diagnoses (abdominal pain, amputation, arthritis, arthropathies, osteoarthritis and musculoskeletal pain, back pain, chronic pain, fibromyalgia, headache, malignancy, multiple sclerosis, neuropathic pain, peripheral vascular disease with claudication, ischemic extremity pain and/or skin ulcers, and stroke), use of other medications with abuse potential, types of healthcare facilities where the patient sought care, and number of office visits.
Analysis
We described demographic characteristics, clinical characteristics, healthcare utilization, and medication use as captured in the HIRD administrative claims data during the follow-up period. Characteristics were assessed for individuals who were included in the medical record review, individuals who were eligible for but not included in medical record review, and for those who were ineligible (Table S4).
For those individuals for whom at least one medical record was obtained, we identified the number and percentage of patients in each possible doctor/pharmacy shopping category with no behaviors, each specific behavior, at least one and as many as 34 (ie, all) of the defined behaviors suggestive of misuse, diversion, abuse, and/or addiction in the medical record. Because medical records of opioid prescribers captured few instances of many behaviors suggestive of abuse, misuse, addiction and diversion across all categories of doctor/pharmacy shopping, analysis of individual behaviors was not conducted. For patients with at least one, at least two, and at least three behaviors documented in medical records of healthcare providers prescribing opioids, the association with possible doctor/pharmacy shopping category status was examined by computing ORs and their 95% CIs comparing possible doctor/pharmacy shopping categories to the no shopping category. We then assessed performance characteristics for severe doctor/pharmacy shopping as indicative of at least three behaviors suggestive of medical record-based abuse, misuse, addiction and/or diversion. These included (1) positive predictive value (PPV) calculated as the true positives divided by the sum of true and false positives, (2) negative predictive value (NPV), calculated as true negatives divided by the sum of true negatives and false negatives, (3) sensitivity, calculated as the true positives divided by the sum of true positives and false negatives, and (4) specificity, calculated as the true negatives divided by the sum of true and false negatives with their respective 95% CIs.
In addition, two sensitivity analyses were pre-specified. In the first sensitivity analysis, we computed ORs and 95% CIs for claims-identified addiction/substance abuse treatment comparing each possible doctor/pharmacy shopping category versus no shopping. This was performed separately for patients with and without at least 18 months of continuous health plan eligibility following the index date to assess the impact of follow-up time on the associations of interest. In the second sensitivity analysis, we computed ORs and 95% CIs for health plan discontinuation comparing each possible doctor/pharmacy shopping category versus no shopping.
Analyses were conducted using SAS Enterprise Guide version 7.12 (SAS Institute Inc., SAS Enterprise Guide version 7.12, Cary, NC, USA). Due to privacy concerns, patient counts of less than or equal to 10 were not reported. A waiver of the Health Insurance Portability and Accountability Act of 1996 (HIPAA) authorization was granted by the New England Institutional Review Board prior to conduct of the study who subsequently approved this study.
Results
Of 8,689,706 individuals enrolled in the HIRD in 2012, 1,066,250 (12%) had an opioid dispensed that year. Of these patients, 581,940 (55%) had a second opioid dispensed within 18 months after the first pharmacy fill. After applying study entrance criteria, 243,554 (78%) individuals were classified as no shopping, 35,073 (11%) minimal shopping, 23,543 (8%) moderate shopping, and 10,302 (3%) severe shopping. A patient list containing a random sample of 750 individuals from each category was drawn, and medical records were requested (Figure 1). The number of medical records that we requested was based on the number of opioid prescribers observed in the administrative data, noting that medical records of healthcare providers who did not prescribe opioids were not included in the analysis. Many patients received opioids from multiple prescribers, therefore, we requested an average of 2.0 records per patient for each of the 115 individuals with no shopping, 2.7 records per patient for each of the 139 individuals with minimal shopping, 3.7 records per patient for each of the 147 individuals with moderate shopping, and 5.7 records per patient for each of the 189 individuals with severe shopping (Table 1).
 |
Table 1 Demographic and clinical characteristics by doctor/pharmacy shopping category |
 |
Figure 1 Formation of the study population. |
Patient characteristics
Among patients included in medical record review across possible doctor/pharmacy shopping categories, those with higher levels of possible shopping behavior were younger compared to those in the no shopping category (median age 47 years versus 55 years), and more were female (62% versus 54%). Those with higher levels of possible doctor/pharmacy shopping behavior had a higher occurrence of general pain complaints such as back pain during follow-up (72% versus 55%), headache (42% versus 16%), and abdominal pain (47% versus 30%, Table 1) than did those with no shopping (mean number of pain diagnoses 2.7 versus 2.2, data not shown). Prevalence of psychiatric comorbidity and use of non-opioid medications of abuse potential such as benzodiazepines were also higher in those with higher levels of possible shopping behavior (ie, mean number of psychiatric diagnoses were 1.3 versus 0.7; data not shown).
Individuals with higher levels of possible shopping behavior had a higher total number of opioid dispensings (mean 17.3 for severe shopping versus 6.9 for no shopping), and a higher proportion of those with more shopping behavior had a history of opioid use prior to the first dispensing (82% versus 70%). The proportion of patients using both IR and ER/LA opioids during follow-up was higher among those with more possible shopping behavior (61 patients for severe shopping category versus ≤10 patients for no shopping category). Very few patients used ER/LA opioids exclusively (Table 1).
Comparing individuals for whom charts were requested but unavailable to those who were included in medical record review, those with unavailable records were slightly younger, but were similar with respect to healthcare utilization, psychiatric comorbidities, pain conditions, medication use, and history of opioid use. Overall, patients with medical records reviewed were very similar to the sampling frame of eligible opioid users from which they were drawn (Table S2). For included patients, a lower proportion of the total medical records requested were obtained for those with severe shopping (69%) than for those with no shopping (79%, Table 1).
Behaviors documented in medical records of healthcare providers prescribing opioids
Overall, individual patients had between zero and eight of the 34 behaviors suggestive of abuse, misuse, addiction, and diversion documented in the medical records of opioid prescribers that were reviewed. No behaviors were identified in any record reviewed for 64% of individuals with no shopping, 58% with minimal shopping, 56% with moderate shopping, and 39% with severe shopping. Conversely, at least one behavior was identified in any record reviewed for 36% of individuals with no shopping, 42% with minimal shopping, 44% with moderate shopping, and 61% with severe shopping. There was a gradient in which more behaviors were observed in higher possible shopping categories (Table 2).
 |
Table 2 Behaviors suggestive of misuse, diversion, abuse and/or addiction identified through medical record review |
Across all shopping categories, the most frequently documented behavior in prescribers’ medical record was report of multiple causes of pain (22%) followed by resisted therapy changes (12%). Several behaviors, including resisted therapy changes, emergency room visits to obtain opioids, unauthorized dose escalation, and alcohol abuse were substantially more common in patients in the severe shopping versus no shopping category (Table 2). There were similarities in the proportion of patients exhibiting severe and no shopping behavior who cancelled pain clinic visits, saved or hoarded medication, or used opioids for a non-pain purpose.
Compared with no shopping, the OR of having at least one behavior documented in medical records of opioid prescribers was 1.28 (95% CI 0.77–2.13) for minimal shopping, 1.38 (95% CI 0.84–2.27) for moderate shopping, and 2.76 (95% CI 1.71–4.46) for severe shopping. Larger differences were observed for documentation of at least two behaviors (1.51, 95% CI 0.74–3.07 for minimal shopping, 1.55, 95% CI 0.77–3.13 for moderate shopping, and 4.15, 95% CI 2.20–7.81 for severe shopping) and at least three behaviors (1.70, 95% CI 0.50–5.78 for minimal shopping, 1.81, 95% CI 0.54–6.03 for moderate shopping, and 8.93, 95% CI 3.12–25.54 for severe shopping; Figure 2).
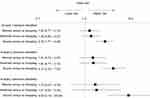 |
Figure 2 Patients with severe shopping behavior were more likely to have behaviors suggestive of misuse, diversion, abuse and/or addiction than patients with less intense shopping. |
When assessing performance characteristics of severe shopping as a surrogate marker for having at least three behaviors, we observed a PPV of 24.34% (95% CI 20.62% – 28.49%), NPV of 94.76% (95% CI 92.67–96.28), sensitivity of 68.66% (95% 56.16% - 79.44%) and specificity of 72.66% (95% CI 68.62–76.44%), noting that under ascertainment of true opioid use disorders is expected.
Sensitivity analyses
Although legal and health plan rules related to access of personally-identifying information for individuals with known substance abuse disorders required that we exclude these individuals from the medical record review component of the analysis, we observed that the proportion of subjects with claims for known substance use disorders increased across the specified doctor/pharmacy shopping categories (2% with no shopping behaviors, 5% with minimal shopping behaviors, 12% with moderate shopping behaviors, and 16% with severe shopping behaviors (data not shown)).
Among patients who met all other study entrance criteria (including follow-up health plan eligibility of 18 months), the OR comparing claims-identified addiction was 2.15 (95% CI 1.98–2.34) for minimal versus no shopping, 3.44 (95% CI 3.17–3.73) for moderate versus no shopping, and 7.15 (95% CI 6.54–7.81) for severe versus no shopping. In exploring whether patients in higher shopping categories were more likely to leave their health plan prior to 18 months after the start of follow-up, a trend was observed, with ORs of health plan discontinuation at 1.27 (95% CI 1.25–1.29) for minimal versus no shopping, 1.37 (95% CI 1.34–1.40) for moderate versus no shopping, and 1.50 (95% CI 1.46–1.55) for severe versus no shopping (Figure 3).
Conclusions
In this cross-sectional study of patients without known aberrant opioid use with at least two dispensings of opioids and medical record data available, being in the severe shopping category was strongly associated with having documentation of behaviors suggestive of misuse, abuse, addiction, and/or diversion in the medical records of opioid prescribers. The association was stronger when claims-based codes for aberrant opioid use were also included in the outcome. Despite an elevated proportion of severe shoppers with medical record-based evidence of abuse, misuse, addiction and/or diversion compared with non-shoppers, this claims-based doctor/pharmacy shopping definition did not discriminate well between individual patients who did and did not have these behaviors. While severe doctor/pharmacy shopping was a strong risk factor, it’s PPV as a surrogate outcome for abuse, misuse, addiction and/or diversion was low noting probable under-ascertainment of aberrant opioid use in the records of opioid prescribers who may not have observed or chosen to record these behaviors.
These results support previous research of the associations between doctor/pharmacy shopping and behaviors suggestive of misuse, diversion, abuse, and/or addiction and expands on prior knowledge by using medical record review rather than administrative claims to identify the study outcome.7,8
Overall, the proportion of opioid prescribers’ medical records containing documentation of behaviors suggestive of abuse, misuse, addiction and diversion was low. However, there was a trend of increasing prevalence of behaviors across increasing shopping categories. Patients with evidence of severe shopping in the claims were more likely than those with no shopping to have evidence of at least one behavior in the medical record. Nonetheless, almost 40% of those with severe shopping had no behaviors observed, and 36% of patients with no shopping had at least one behavior observed.
This discrepancy between shopping and medical record documentation likely arises both from real and artifactual sources. On one hand, individuals with problematic use may come to know of particular pharmacists and/or prescribers who are less rigorous in their screening, and preferentially seek out these providers. The result is that we expect both true aberrant use among non-shoppers (as individuals receiving opioids from a less cautious provider have no need to shop) and reduced documentation of behaviors suggestive of abuse, misuse, addiction and diversion for all groups. Given that the rate of problem use is likely highest and most under ascertained for individuals with higher levels of shopping, both situations result in the expectation of bias towards the null in our observed associations.
With this in mind, it is important to differentiate between a marker of risk and a surrogate measure. In this study, low PPV (24.34%) and specificity (72.66%) measures suggest that use of this claims-based definition of doctor/pharmacy shopping as a measure of abuse, misuse, addiction and/or diversion may misclassify a large proportion of individuals. As such, while the association between doctor/pharmacy shopping is clear and present, results of our study do not support consideration of the claims-based and medical record-based measures as interchangeable.
Gradients of increasing healthcare and medication utilization, psychiatric comorbidity, and behaviors that may be correlated with misuse, abuse, addiction, and diversion of opioids were present and consistent across the possible doctor/pharmacy shopping categories. Also, patients receiving opioids from a larger number of prescribers and pharmacies had more risk factors associated with abuse and opioid overdose (ie, psychiatric comorbidity, and concomitant benzodiazepine use) identified in claims data. It should be noted that doctor/pharmacy shopping, patient characteristics, and behaviors suggestive of misuse, abuse, addiction and diversion were all measured during the same 18-month window.
Several considerations should be taken into account in review of study findings. Using counts of prescriber and pharmacy claims to ascertain possible doctor/pharmacy shopping status does not capture a patient’s intentions, nor do counts capture whether or not healthcare providers are aware of other prescribers. Further, counts of claims cannot inform whether providers coordinated across settings or visits due to specific circumstances. Despite the negative connotation of the term “doctor/pharmacy shopping,” a patient may have legitimate reasons for obtaining opioid medication from more than one prescriber, especially in the context of a complicated medical history that involves care by multiple specialists. In addition, patients may relocate, travel, or simply access pharmacies that are more convenient to their healthcare provider location, home, or work at different times without any intent to “pharmacy shop.”
The behaviors identified in this study are not an exhaustive list of possible correlates of and risk factors for substance use disorders. Although each behavior was selected based on literature review or expert recommendation, not all of the behaviors directly indicate abuse, misuse, addiction or diversion.
Medical records are not likely to fully capture all of the behaviors that were considered. Physicians may hesitate to record potentially stigmatizing information in the medical record, which may be exacerbated by fears of legal action in the event that a patient uses opioids in an aberrant way leading to harm. This is problematic for both research and patient care given the importance of assessing and documenting these behaviors in evidence-based pain care.28 Further, we queried medical records from opioid prescribers only. This may result in systematic underestimation of the proportion of individuals with behaviors suggestive of abuse, misuse, addiction or diversion if healthcare providers recognizing potential problems never prescribed opioids and were therefore missing from the sample of providers included in our medical record review. Assuming that these missed behaviors would be more common among moderate and severe doctor/pharmacy shopping patients, this would create the expectation of bias towards the null.
Further, we expect that exclusion of patients with known substance use disorders from medical record review artificially reduced the observed prevalence of behaviors suggestive of abuse, misuse, addiction or diversion. Although sensitivity analyses showed a very similar relation between doctor/pharmacy shopping and claims-based versus medical-record based outcomes, any assessment of behavior prevalence must take this into consideration. It is expected that the inaccessible records of patients diagnosed with substance use disorders would have contained a higher number of instances of the behaviors. This is both because they are likely more common in these individuals and because healthcare providers seeing patients with more apparent problematic use may be more inclined to notice and document potential warning signs. The same behaviors may have been present but less often documented for other patients where the clinician had a lower awareness of and/or concern about disordered use. Further, it is not entirely clear whether individuals with outcomes identified in the claims had opioid use disorders specifically, and if so whether their disorders were more severe.
Not all medical records that were requested could be obtained as some facilities were unwilling or unable to provide them. A higher number of records were missing for the higher levels of possible shopping for which more records per patient were requested. Although we originally suspected that healthcare providers may differentially refuse to provide records for patients with aberrant drug behavior, this was not observed in refusal responses. The proportion of records that were denied by the treating clinician versus unavailable for administrative reasons (ie, lost, archived, or facility did not have a record of the patient in question) was similar across doctor/pharmacy shopping categories.
The categorization of shopping behavior ignores cash payments. Therefore, the results of this analysis are only representative of health plans that have submitted claims. Findings from a related study indicate that the use of cash to purchase opioids increases across shopping behavior categories and is highest among patients with severe shopping.7
In terms of generalizability, the majority of patients in this study are members of employer-sponsored managed care programs. Thus, the results and findings may not be generalizable to individuals receiving Medicaid or Social Security Disability Insurance. In addition, individuals reporting white race and higher income are typically over-represented in the HIRD population, which may limit generalizability to the other populations of opioid users. Finally, we excluded patients who were not enrolled in a health plan contributing data to the HIRD for the full 18-month period during which doctor/pharmacy shopping was assessed, unless the reason for incomplete follow-up was due to death. A sensitivity analysis showed that this exclusion resulted in a greater proportion of patients in higher intensity shopping categories being excluded compared with low intensity shopping categories. If individuals with substance use disorders have less stable health coverage (due to loss of employment, etc), it is possible that this criterion reduced the observed association between doctor/pharmacy shopping intensity and misuse, abuse, addiction and diversion.
Finally, the time period assessed preceded wide recognition of the opioid crisis in the US.29 In the intervening years, initiatives such as Prescription Drug Monitoring Programs have been implemented in most states, allowing prescribing clinicians to determine whether their patients have accessed other opioid sources and leading to changes in prescribing behavior.30–32 Insurers have also implemented additional authorization requirements aimed at reducing access to opioids without proper medical coordination.33 As such, it is reasonable to expect that observed patterns of doctor and pharmacy shopping may change over time.
Despite these limitations, this study adds a new perspective on doctor/pharmacy shopping for opioid analgesics as a strong risk factor for abuse, misuse, addiction and diversion. Assessing aberrant drug behavior via medical records allows capture of this outcome from a clinician viewpoint, and the medical record contains more nuance than administrative claims alone. However, our findings of a strong association are consistent between medical record review and assessment of claims. Further research is needed to explore whether different ways of assessing opioid misuse, abuse, addiction and diversion, such as direct patient perspectives, confirm the correlation between doctor/pharmacy shopping and aberrant use.
Acknowledgments
This project was conducted as part of a Food and Drug Administration (FDA)-required postmarketing study for extended-release and long-acting opioid analgesics and was funded by the Opioid Postmarketing Consortium (OPC) consisting of the following companies: Allergan; Assertio Therapeutics, Inc.; BioDelivery Sciences, Inc.; Collegium Pharmaceutical, Inc.; Daiichi Sankyo, Inc.; Egalet Corporation; Endo Pharmaceuticals, Inc.; Hikma Pharmaceuticals USA Inc.; Janssen Pharmaceuticals, Inc.; Mallinckrodt Inc.; Pernix Therapeutics Holdings, Inc.; Pfizer, Inc.; and Purdue Pharma, LP. The study was designed in collaboration between HealthCore, Inc. and the OPC and was implemented by HealthCore, Inc.
Disclosure
RY and SL are employees of HealthCore, Inc., and at the time of the study DBE and JGL were employees of HealthCore Inc., which received funding from the OPC to conduct the study. MSC is an employee of Janssen Research and Development. DBE reports employment by companies engaged in industry sponsored research: HealthCore, Inc and Ciconia Inc, outside the submitted work. MSC has nothing to report from Janssen Research and Development during the conduct of the study. SL reports employment with Campbell Alliance Ltd., during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. Katz N, Panas L, Kim M, et al. Usefulness of prescription monitoring programs for surveillance–analysis of Schedule II opioid prescription data in Massachusetts, 1996-2006. Pharmacoepidemiol Drug Saf. 2010;19(2):115–123. doi:10.1002/pds.1878
2. Peirce GL, Smith MJ, Abate MA, Halverson J. Doctor and pharmacy shopping for controlled substances. Med Care. 2012;50(6):494–500. doi:10.1097/MLR.0b013e31824ebd81
3. Cepeda MS, Fife D, Chow W, Mastrogiovanni G, Henderson SC. Assessing opioid shopping behaviour: a large cohort study from a medication dispensing database in the US. Drug Saf. 2012;35(4):325–334. doi:10.2165/11596600-000000000-00000
4. Cepeda MS, Fife D, Kihm MA, Mastrogiovanni G, Yuan Y. Comparison of the risks of shopping behavior and opioid abuse between tapentadol and oxycodone and association of shopping behavior and opioid abuse. Clin J Pain. 2014;30(12):1051–1056. doi:10.1097/AJP.0000000000000067
5. Cepeda MS, Fife D, Yuan Y, Mastrogiovanni G. Distance traveled and frequency of interstate opioid dispensing in opioid shoppers and nonshoppers. J Pain. 2013;14(10):1158–1161. doi:10.1016/j.jpain.2013.04.014
6. Cepeda MS, Fife D, Chow W, Mastrogiovanni G, Henderson SC. Opioid shopping behavior: how often, how soon, which drugs, and what payment method. J Clin Pharmacol. 2013;53(1):112–117. doi:10.1177/0091270012436561
7. Walker AM, Weatherby LB, Cepeda MS, Bradford D, Yuan Y. Possible opioid shopping and its correlates. Clin J Pain. 2017;33(11):976–982. doi:10.1097/AJP.0000000000000483
8. Sullivan MD, Edlund MJ, Fan MY, Devries A, Brennan Braden J, Martin BC. Risks for possible and probable opioid misuse among recipients of chronic opioid therapy in commercial and medicaid insurance plans: the TROUP study. Pain. 2010;150(2):332–339. doi:10.1016/j.pain.2010.05.020
9. Michna E, Ross EL, Hynes WL, et al. Predicting aberrant drug behavior in patients treated for chronic pain: importance of abuse history. J Pain Symptom Manage. 2004;28(3):250–258. doi:10.1016/j.jpainsymman.2004.04.007
10. Webster LR, Webster RM. Predicting aberrant behaviors in opioid-treated patients: preliminary validation of the opioid risk tool. Pain Med. 2005;6(6):432–442. doi:10.1111/j.1526-4637.2005.00072.x
11. Fleming MF, Balousek SL, Klessig CL, Mundt MP, Brown DD. Substance use disorders in a primary care sample receiving daily opioid therapy. J Pain. 2007;8(7):573–582. doi:10.1016/j.jpain.2007.02.432
12. Passik SD, Kirsh KL. The need to identify predictors of aberrant drug-related behavior and addiction in patients being treated with opioids for pain. Pain Med. 2003;4(2):186–189. doi:10.1046/j.1526-4637.2003.03018.x
13. Gupta A, Patton C, Diskina D, Cheatle M. Retrospective review of physician opioid prescribing practices in patients with aberrant behaviors. Pain Physician. 2011;14(4):383–389.
14. Jamison RN, Butler SF, Budman SH, Edwards RR, Wasan AD. Gender differences in risk factors for aberrant prescription opioid use. J Pain. 2010;11(4):312–320. doi:10.1016/j.jpain.2009.07.016
15. Cheatle MD, O’Brien CP, Mathai K, Hansen M, Grasso M, Yi P. Aberrant behaviors in a primary care-based cohort of patients with chronic pain identified as misusing prescription opioids. J Opioid Manag. 2013;9(5):315–324. doi:10.5055/jom.2013.0174
16. Compton P, Darakjian J, Miotto K. Screening for addiction in patients with chronic pain and “problematic” substance use: evaluation of a pilot assessment tool. J Pain Symptom Manage. 1998;16(6):355–363.
17. Lopato J, Mody S, Pesa J, Durkin M, Chang CL, O’Sullivan AK Empirical assessment of quality measures for opioid utilization.
18. Chabal C, Erjavec MK, Jacobson L, Mariano A, Chaney E. Prescription opiate abuse in chronic pain patients: clinical criteria, incidence, and predictors. Clin J Pain. 1997;13(2):150–155.
19. Butler SF, Budman SH, Fernandez KC, et al. Development and validation of the current opioid misuse measure. Pain. 2007;130(1–2):144–156. doi:10.1016/j.pain.2007.01.014
20. Martell BA, O’Connor PG, Kerns RD, et al. Systematic review: opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction. Ann Intern Med. 2007;146(2):116–127. doi:10.7326/0003-4819-146-2-200701160-00006
21. Turk DC, Swanson KS, Gatchel RJ. Predicting opioid misuse by chronic pain patients: a systematic review and literature synthesis. Clin J Pain. 2008;24(6):497–508. doi:10.1097/AJP.0b013e31816b1070
22. Witkin LR, Diskina D, Fernandes S, Farrar JT, Ashburn MA. Usefulness of the opioid risk tool to predict aberrant drug-related behavior in patients receiving opioids for the treatment of chronic pain. J Opioid Manag. 2013;9(3):177–187. doi:10.5055/jom.2013.0159
23. Larson MJ, Paasche-Orlow M, Cheng DM, Lloyd-Travaglini C, Saitz R, Samet JH. Persistent pain is associated with substance use after detoxification: a prospective cohort analysis. Addiction. 2007;102(5):752–760. doi:10.1111/j.1360-0443.2007.01759.x
24. Liebschutz JM, Saitz R, Weiss RD, et al. Clinical factors associated with prescription drug use disorder in urban primary care patients with chronic pain. J Pain. 2010;11(11):1047–1055. doi:10.1016/j.jpain.2009.10.012
25. Potter JS, Shiffman SJ, Weiss RD. Chronic pain severity in opioid-dependent patients. Am J Drug Alcohol Abuse. 2008;34(1):101–107. doi:10.1080/00952990701523706
26. Wasan AD, Butler SF, Budman SH, et al. Does report of craving opioid medication predict aberrant drug behavior among chronic pain patients? Clin J Pain. 2009;25(3):193–198. doi:10.1097/AJP.0b013e318193a6c4
27. Wasan AD, Ross EL, Michna E, et al. Craving of prescription opioids in patients with chronic pain: a longitudinal outcomes trial. J Pain. 2012;13(2):146–154. doi:10.1016/j.jpain.2011.10.010
28. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain - United States, 2016. MMWR Recomm Rep. 2016;65(1):1–49. doi:10.15585/mmwr.rr6501e1
29. Soelberg CD, Brown RE
30. Bao Y, Pan Y, Taylor A, et al. Prescription drug monitoring programs are associated with sustained reductions in opioid prescribing by physicians. Health Aff (Millwood). 2016;35(6):1045–1051. doi:10.1377/hlthaff.2015.1673
31. Haffajee RL, Jena AB, Weiner SG. Mandatory use of prescription drug monitoring programs. JAMA. 2015;313(9):891–892. doi:10.1001/jama.2014.18514
32. Excellence PMPCO, America USO. Briefing on PDMP Effectiveness; 2013. Accessed July 06, 2018.
33. Anthem blue cross launches program to tackle Inappropriate opioid use [press release]. 2016. Available from: https://www.anthem.com/press/connecticut/anthem-blue-cross-and-blue-shield-launches-program-to-tackle-inappropriate-opioid-and-rx-drug-use-improve-drug-safety-health-care-quality/. Accessed July 06, 2018.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

