Back to Journals » Integrated Pharmacy Research and Practice » Volume 10
Medical Devices-Related Counseling Practices Among Community Pharmacists: A Nationwide Cross-Sectional Study from Saudi Arabia
Authors Fathelrahman AI
Received 7 March 2021
Accepted for publication 27 August 2021
Published 10 September 2021 Volume 2021:10 Pages 113—125
DOI https://doi.org/10.2147/IPRP.S310027
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Mudassar Iqbal Arain
Ahmed Ibrahim Fathelrahman
Department of Clinical Pharmacy, College of Pharmacy, Taif University, Taif, Saudi Arabia
Correspondence: Ahmed Ibrahim Fathelrahman
Department of Clinical Pharmacy, College of Pharmacy, Taif University, P.O. Box 888, Taif, 21974, Saudi Arabia
Tel +966 537298070
Email [email protected]
Objective: The current study was conducted to assess medical devices-related counseling practices among community pharmacists in Saudi Arabia.
Methodology: This was a cross-sectional study conducted among community pharmacists from Saudi Arabia using a convenience sampling technique. An online questionnaire based on Google forms was used to collect data. Descriptive and inferential analyses were conducted using SPSS statistics 22. Student t-test, one way ANOVA, and Pearson correlation statistics were used where applicable. Results with a p-value of < 0.05 were considered statistically significant.
Results: One thousand and six community pharmacists responded to the survey. Males’ rating of their ability to operate medical devices was significantly higher than females (overall average score of 3.8 versus 3.5, p=0.033). As years of experience increased there were slight but significant increases in the overall scores on ability to operate medical devices (p=0.002) and confidence to counsel patients about the devices (p=0.032). Those who got a board certification used devices for self-treatment significantly more than their counterparts (on average 6.9 devices versus 5.2, p=0.003). Those who received clinical training reported higher rates of ability to use/operate devices (p=0.011), confidence to counsel patients on devices (p=0.001), and counseling practice (p=0.044) than those who did not receive clinical training.
Conclusion: The present study revealed good to very good self-reported medical devices-related counseling practices. There is a need for more future rigorous research to evaluate pharmacists’ actual practice in this area. Pharmacy educators and CPD programs should pay attention to updating pharmacists’ knowledge and skills and improve their contribution to medical devices supportive services.
Keywords: community pharmacists, correlations, counseling practices, medical devices, Saudi Arabia
Introduction
Patients counseling represents a core part of classic and modern pharmacists’ roles.1–5 It has been documented and assessed worldwide and has been applied on both general pharmaceutical care and health6–9 and for caring about specific patients’ conditions and needs.10–13 However, the literature on community pharmacy services and pharmacists’ counseling practices in Saudi Arabia revealed conflicting findings. A substantial proportion of such literature showed poor patterns of practice, whereas some studies indicated clear positive and satisfactory findings. For example, Alanazi et al14 conducted a review on the literature documenting pharmaceutical care in community pharmacies in Saudi Arabia and reported that dispensing of medicines is the only service provided by community pharmacists with very limited scope of other pharmaceutical care services. Alfadl et al15 conducted a study on medication counseling practice at community pharmacies in Qassim region at the central region of Saudi Arabia and reported that only one fifth of the counseling content assessed in the study was found satisfactory and that the quality of medication counseling services provided to patients was poor. A systematic review on the studies addressing community pharmacists’ patient-centered care services in Saudi Arabia indicated great shortages in providing high quality services.16 A cross-sectional study conducted in Riyadh, Saudi Arabia evaluating counseling practices in community pharmacies showed shortcomings in proper dispensing practices and medication counseling at community pharmacies.17
However, most previous studies were not directly addressing the counseling practices of a particular pharmaceutical care service. It is possible that such studies overlooked some of the available best practices because researchers focused on assessing counseling or medications centered care in general. There might be room for identifying positive findings when assessing a particular service like diabetic care, smoking cessation assistance, and supporting customers regarding their cosmetic products and medical devices. In this regard, there were reports documenting the presence of positive practices. For example, Gillani et al18 assessed community pharmacist perceptions of healthcare services in Saudi Arabia. Among findings, one third of the respondents claimed they provided clinical services to the community. The study revealed that confidence to practice can be predicted by knowledge to practice, value of practice, and need for practice.18 A sample of community pharmacists from Riyadh have been surveyed. They perceived counseling patients on OTC, prescription drugs, and other health-related problems as a top priority compared to other activities like dispensing, stocking, and purchasing.19 According to a study conducted by Alshahrani,20 community pharmacists in Saudi Arabia showed extensive knowledge, were prepared to play a supportive role, and displayed positive attitudes towards the fight against coronavirus disease of 2019 (COVID-19). Regarding counseling, most community pharmacists considered that counseling customers on COVID-19 is an important activity. A survey of community pharmacists from the western region of Saudi Arabia indicated good responses among pharmacists regarding their professional role in dispensing beauty products and their counseling practice in this area.21
To our knowledge, there has been no study conducted in Saudi Arabia addressing pharmacists counseling practice regarding medical devices. However, we conducted a study among a small sample of pharmacy students from Saudi Arabia to explore their preparedness to counsel patients about medical devices.22 Pharmacy students showed moderate knowledge and reported high-to-moderate perceived preparedness to counsel patients about medical devices. Students’ perceived ability to use medical devices and perceived ability to counsel were highly correlated.22 Blood glucose monitor, blood pressure monitor, insulin pen, and metered dose inhaler (MDI) were rated highest compared to other devices regarding both use and counseling abilities.22 In the same context we conducted a pilot study among Sudanese pharmacists to assess their readiness to counsel patients about medical devices.23 Devices commonly available in the market were perceived to be better used by pharmacists. Five devices, namely thermometers, weighing scales, syringes, blood glucose monitors, and blood pressure monitors, were the most-used personally by pharmacists and the pharmacists reported highest confidence to use them properly and highest confidence to counsel patients about them. The study generates a hypothesis that the ability to counsel patients about medical devices is likely a reflection of pharmacists’ exposure to such devices, and is likely related to their ability to use such devices.23
Hence, the present study was conducted to assess medical devices-related counseling practices among community pharmacists in Saudi Arabia using a large nationwide sample.
Methodology
Study Design and Participants
A cross-sectional survey-based study was conducted between August to November 2020 involving community pharmacists from different regions of Saudi Arabia. Convenience sampling was employed as a sampling technique.
Study Setting
The study setting included community pharmacies from different regions of Saudi Arabia. All pharmacies have a licence from the health authority to provide services to all patients and customers from the broad community population were eligible for inclusion. This includes chain and individual pharmacies and pharmacies affiliated to hospitals and health centers but open outside the institution to provide services to the whole community. In Saudi Arabia, community pharmacies’ basic scope of services normally includes dispensing prescribed and over-the-counter medications as well as cosmetic and household products and medical devices. Pharmacists are allowed to provide counseling to the patients and customers as a core part of their services. In-patient and out-patient hospital pharmacies and pharmacies located inside health centers to service only patients attending the institutions were not included.
Ethical Considerations
Taif university research ethics committee approved the study (reference number 41–00193). A brief description of the study and its importance and goals was displayed at the beginning of the survey with a question asking pharmacists to choose “yes” if they were voluntarily willing to participate. Respondents were informed that participation was optional, and that data would be anonymously analyzed and presented. All agreed to participate in the survey. The data was downloaded anonymously from Google Forms in the form of an Excel sheet. Nothing can be used to uncover the identity of the participants.
Data Collection
Respondents completed an online survey using Google forms. The link to the survey was shared with key persons in community pharmacy groups and by distribution among pharmacists using social media like WhatsApp and Facebook groups. To encourage the participation of community pharmacists, reminders were sent frequently.
Sample Size
According to most recently available statistics reported by AlRuthia et al in 2018,24 the number of community pharmacists working in different regions of Saudi Arabia was 8,419. By convention, surveying a sample of 10% of a population would be representative. In the light of such information, the researcher assumed that surveying 850 pharmacists would be representative of the community pharmacists in the whole country (ie, 10%).
The Survey
The original questionnaire included 10 items developed specifically for the purpose of this study based on general reading of literature. The present analysis included only seven, as follows: 1) types of medical devices respondents encountered during practice (12 therapeutic categories); 2) medical devices used personally by the respondents for self-treatment (20 medical devices/responses; no or yes); 3) medical devices representing patients’ common inquiry (20 medical devices/each rated on a 5-point Likert scale, with possible scores ranging from 1–5); 4) self-rating of ability to use or operate medical devices (20 medical devices/each rated on a 5-point Likert scale, with possible scores ranging from 1–5); 5) self-rating of confidence to counsel patients about medical devices (20 medical devices/each rated on a 5-point Likert scale, with possible scores ranging from 1–5); 6) reported counseling practice (20 medical devices/each rated on a 5-point Likert scale, with possible scores ranging from 1–5); and 7) medical devices being supplied to patients (20 medical devices/each rated on 5-point Likert scale, with possible scores ranging from 1–5).
Validation of Questionnaire
Five academic staff from different origins, countries, and academic institutions who had excellent experiences in pharmacy practice and healthcare services in addition to a practicing clinician validated the questionnaire items for face and content. Their feedback has been used to edit the questionnaire regarding phrasing and contents until they were satisfied. Furthermore, the questionnaire has been piloted on smaller sample of pharmacists from Sudan and the data has been published elsewhere.23 Questions measuring ability to use medical devices (20 items, Cronbach’s alpha=0.887), confidence to counsel patients about medical devices (20 items, Cronbach’s alpha=0.921), medical devices representing patients’ common inquiry (20 items, Cronbach’s alpha=0.912), reported counseling practice (20 items, Cronbach’s alpha=0.937), and supplying devices to the patients (20 items, Cronbach’s alpha=0.938) showed high reliability. Slight edits in some wordings were made in the version used in the current study, such as using the description Metered Dose Inhalers (MDIs) instead of inhalers and adding the description “diskus” with “accuhalers”. The questionnaire is provided as Supplementary material.
Statistical Analysis and Data Presentation
Descriptive and inferential analyses were conducted using IBM SPSS version 22.25 For all variables with 5-point Likert scale responses, scores on average ratings were computed for every device (minimum score=0, maximum score=5). This included scores on the following: 1) the device representing patients’ common inquiry, 2) pharmacists’ ratings on their ability to use the device, 3) pharmacists’ ratings on their confidence to counsel patients about the device, 4) pharmacists’ ratings on counseling practice regarding the device, and 5) pharmacists’ ratings of supplying patients with the device. A final average score was computed for each of the previous five items representing the counseling-related practices on all 20 medical devices (ie, five variables on overall counseling practices scores). For the purpose of this study, self-reported practice of pharmacists was considered excellent when the average score is ≥4, very good when the average score is ≥3.5–<4, good when the average score is ≥3–<3.5, average when the average score is ≥2–<3, poor when the average score is <2–≥1.5, and very poor when the average score is <1.5. A variable was computed from the 20 questions on medical devices use for self-treatment by calculating the sum of the yes responses (theoretically, maximum possible score should be 20 but actually no respondent selected yes for all devices).
Comparisons regarding computed scores between dichotomous demographic and background variables were conducted using Student’s t-test. One-way analysis of variance (ANOVA) was used to test differences between demographic and background groups having multicategory responses. Correlational analyses were performed using Pearson correlation. In all analyses, results with a p-value of <0.05 were considered statistically significant.
Results
Demographic Characteristics
One thousand and six community pharmacists responded to the online survey. The highest category of participants was those aged 25–34 years old (73.6%) (Table 1). Males represented the majority (97.1%). The majority were non-Saudi (92.8%), located in cities (92.5%), and were bachelor’s degree holders (84.4%). Slightly more than one fifth of the respondents received clinical training (23.4%%) or got a board certification (22%). By geographical region, most respondents were from Makkah region (n=388, 38.6%), which included three populous provinces: Makkah, Taif, and Jeddah (Figure 1). This was followed by Riyadh region that included the capital city and other provinces (n=228, 22.7%). The third highest category of respondents were from Asir (n=106, 10.5%) followed by Al Madinah region (n=77, 7.7%) as the fourth highest category of respondents. Few of the respondents were from the other regions of Saudi Arabia.
 |
Table 1 Demographic and Background Information of Respondents (N=1,006) |
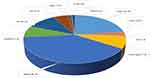 |
Figure 1 Distribution of community pharmacists by region (N=1,006). |
Awareness About Medical Devices
Awareness about medical devices arises from being exposed to the devices during practice or early training (Figure 2) or because of personal use of a device for self-treatment (Figure 3). From Figure 2, the types of medical devices (by therapeutic categories) the respondents encountered were mostly pulmonary (89.6%) followed by cardiology (71.2%). Figure 3 shows medical devices used by respondents for self-treatment. Thermometers (57.3%), weighing scales (54.2%), first aid equipment (46.2%), blood pressure monitors (39.6%), and blood glucose monitors (34.3%) were the devices most used personally by pharmacists. Implanted devices (12.9%) were the least used devices.
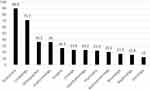 |
Figure 2 Types of medical devices (by therapeutic categories) that pharmacists (N=1,006) come across during practice (y-axis represents percentage). |
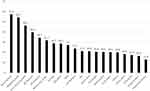 |
Figure 3 Medical devices used by pharmacists (N=1,006) for self-treatment (y-axis represents percentage). |
Medical Devices Represent Patients’ Common Inquiry
The top five devices which represented patients’ common inquiry (Table 2, the first four devices got a rating score ≥4) were blood glucose monitors (score=4.28), blood pressure monitors (4.23), thermometers (4.14), weighing scales (4.04), and metered dose inhalers (MDIs, 3.97). Implanted devices (2.68), stethoscope (2.67), and testing kits (2.66) represented devices with the least patients’ inquiry. The overall average score of this counseling-related practice (ie, being a patient’s common inquiry) on the five-point Likert scale was acceptable (score=3.46).
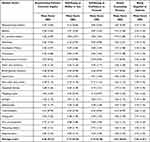 |
Table 2 Medical Devices Counseling-Related Practices Concerning the 20 Devices Covered by the Study |
Pharmacists’ Self-Rating of Ability to Use/Operate Medical Devices
The top seven devices rated highest (all got a rating score ≥4) by pharmacists in terms of ability to be used (Table 2) were blood glucose monitors (score=4.35), blood pressure monitors (4.33), thermometers (4.29), weighing scales (4.22), nebulizers (4.16), metered dose inhalers (MDIs, 4.13), and insulin pens (4.07). Implanted devices (2.64), respirometers (2.92), and testing kits (2.98) represented the devices that pharmacists were least able to use/operate. The overall average score of this counseling-related practice (ie, ability to use/operate medical devices) on the five-point Likert scale was excellent (score=3.77).
Pharmacists’ Self-Rating of Confidence to Counsel Patients About Medical Devices
The top seven devices rated highest (all got a rating score ≥4) by pharmacists in terms of confidence to counsel about (Table 2) were blood glucose monitors (score=4.26), blood pressure monitors (4.24), thermometers (4.22), weighing scales (4.15), nebulizers (4.05), insulin pens (4.01), and metered dose inhalers (MDIs, 4.00). Implanted devices (score=2.75), respirometers (3.03), and testing kits (3.09) represented the devices that pharmacists were least confidence to counsel about. The overall average score of this counseling-related practice (ie, confidence to counsel patients about medical devices) on the five-point Likert scale was excellent (score=3.75).
Reported Counseling Practice Related to Medical Devices
The top five devices rated highest by pharmacists in terms of counseling practice (Table 2, the first four devices got a rating score ≥4) were blood glucose monitors (score=4.17), blood pressure monitors (4.15), thermometers (4.10), weighing scales (4.02), and nebulizers (3.92). Implanted devices (score=2.79), respirometers (3.00), testing kits (3.06), and stethoscope (3.07) represented the devices which got the least counseling. The overall average score of this counseling-related practice (ie, reported counseling about medical devices) on the five-point Likert scale was excellent (score=3.63).
Pharmacists’ Supply of Medical Devices
The top five devices rated highest in terms of being supplied by pharmacists to the patients (Table 2, none got a rating score ≥4) were blood glucose monitors (score=3.68), blood pressure monitors (3.66), thermometers (3.65), weighing scales (3.62), and nebulizers (3.35). Implanted devices (score=2.59), respirometers (2.73), stethoscope (2.76), and testing kits (2.77) represented the devices least supplied to patients. The overall average score of this counseling-related practice (ie, supplying patients with medical devices) on the five-point Likert scale was acceptable (score=3.20).
Comparisons Between Groups
Comparisons by demographic categories were conducted concerning the mean scores (on the five-point Likert scale) for each one of the five counseling-related practices (ie, “devices representing patients’ common inquiry”, “pharmacists’ self-rating of ability to use/operate the devices”, “pharmacists’ self-rating of confidence to counsel about the devices”, “reported counseling practice”, and “devices being supplied to patients”), besides the variable “being used personally by pharmacists for self-treatment”.
Table 3 shows variability in the medical devices counseling-related practices by gender and years of experience. Males’ rating of their ability to operate medical devices was significantly higher than females (overall average score of 3.8 versus 3.5, Student’s t-test p-value=0.033). As years of experience increased there were slight but significant increases in the overall scores on ability to operate medical devices and confidence to counsel patients about the devices (ANOVA p-values=0.002 and 0.032, respectively). Table 4 shows variability in the medical devices counseling-related practices by highest qualification, board certification, and clinical training. Those who got a board certification used devices for self-treatment significantly more than their counterparts (on average 6.9 devices versus 5.2, Student’s t-test p-value=0.003). Those who received clinical training reported higher rates of ability to use/operate devices, confidence to counsel patients on devices and reported counseling practice than those who did not receive clinical training (Student’s t-test p-values=0.011, 0.001, and 0.044, respectively). By age group there were no significant differences in the overall scores of all counseling-related practices.
 |
Table 3 Variability in the Medical Devices Counseling-Related Practices by Gender and Years of Experience |
 |
Table 4 Variability in the Medical Devices Counseling-Related Practices by Highest Qualification, Board Certification, and Clinical Training |
Correlational Analyses
Table 5 shows the correlations between medical devices counseling-related practices. “Reported ability to use medical devices”, “confidence to counsel patients about medical devices”, and “reported counseling about medical devices” were all highly and significantly correlated with each other. “Supplying patients with medical devices” correlated slightly but significantly with “using devices personally for self-treatment” and moderately and significantly with all other counseling practices. “Devices representing patients’ common inquiry” correlated moderately and significantly with all counseling practices, except “using devices personally for self-treatment”, where the correlation was low.
 |
Table 5 Correlations Between Medical Devices Counseling-Related Practices |
Discussion
The influence of community pharmacists as health and pharmaceutical care providers is great on their societies worldwide due to their high accessibility and availability.26–31 Serving community needs concerning medical devices is an essential emerging role expected to be fulfilled efficiently by community pharmacists everywhere.32,33 This is specifically important due to the increasing concerns about bioethical and healthcare concepts like autonomy, patients’ rights, and self-care, which give patients and consumers more rights and roles in making decisions and caring for their own health.34–38 In some countries, patients and customers go to community pharmacies and request a variety of pharmaceutical products, cosmetics, and medical devices without prescriptions.39–44 Saudi Arabia is not different in this regard.45 This requires a control from community pharmacists to reduce harms associated with misuse and irrational use and to ensure achievement of intended outcomes. This in turns necessitates pharmacists’ preparedness with required knowledge and skills and their willingness to counsel patients about such products.
The present study revealed good to very good medical devices-related counseling practices, as the average scores of most devices-related counseling practices assessed were above 3.5. The study covered five medical devices-related counseling practices. There were high-to-weak, but always significant correlations between such practices. The reported ability to use medical devices, confidence to counsel about devices, and reported counseling were all highly and significantly correlated with each other. For all counseling practices, the four top rated devices were the same, which were blood glucose monitors, blood pressure monitors, thermometers, and weighing scales. Among other top-rated devices in certain counseling practices were nebulizers, metered dose inhalers, and insulin pens. The consistent pattern of highly scored devices across different counseling practices (ie, reported use for self-treatment, ability to use, confidence to counsel, counselling, and supplying devices) and the high correlations between such counseling practices indicates the coherence and consistency of the findings of this study.
Improving counseling practice of community pharmacists requires the presence of enabling factors and removal of obstacles and barriers encountered during practice, as had been established from previous research. The lack of knowledge and time, absence of pharmacy information database, deficiency of continued professional development training, and professional and cultural issues were barriers to providing counseling in Saudi Arabia.16 Nationalization of practice and the presence of incentives and rewards for providing patient-centered care have been identified as motivators of positive practice change in community pharmacy in Saudi Arabia.46 The authors highlighted the importance of effective collaboration between community pharmacy owners or chief operating officers, professional pharmacy organizations, and pharmacy colleges for the successful implementation of the change process in community pharmacy practice in the KSA.46
The presence of a small proportion of female pharmacists in this sample reflects the actual pattern of practice in Saudi Arabia. AlRuthia et al24 documented the status of the licensed pharmacy workforce in Saudi Arabia and reported that females represented only 14.84% of pharmacists working in different settings of practice. Most of those were working in hospitals and academia. Almaghaslah et al47 also documented the pharmacy workforce in Saudi Arabia and reported that community pharmacists represent 74.5% of total pharmacists in the private sector and females account for 0.3% only.
The strengths of the present study were the large sample size and the relative representation of different geographical regions of Saudi Arabia, making it a nationwide survey. A limitation of the study was the absence of a sampling frame (a list of all pharmacists in Saudi Arabia with their emails or contact information) which prevented researchers from taking a probability sample which in turns prevented the stratification of the sample by geographical region. Thus, a convenient sampling technique was used as the only feasible sampling technique for this huge number of participants. Another limitation of the study was its relay on self-reporting of practice rather than assessing actual practice. This might be associated with the possibility of some reporting bias which cannot be totally ruled out. However, nothing throws doubt on the validity of findings of this study given that most pieces of findings were consistent. As baseline data, the findings of this study would represent an excellent starting point and a base for future more rigorous study designs in this overlooked area of practice. Another limitation was the nature of the online survey. Surveying this huge number of participants was difficult to achieve face-to-face. In addition, the time of data collection was during the mid-time of the COVID-19 outbreak in Saudi Arabia, which was associated with complete lockdown. Hence, it was impossible to survey pharmacists face-to-face. However, an advantage of the online survey which has been gained in this study is the possibility of surveying a large sample of respondents. The participation of pharmacists from different regions of Saudi Arabia made the study representative of pharmacists working all over the Kingdom.
Conclusion
The present study revealed good-to-very good self-reported medical devices-related counseling practices. There is a need for more rigorous future research to evaluate pharmacists' actual practice in this area. Pharmacy educators and CPD programs should pay attention to updating pharmacists’ knowledge and skills and improve their contribution to medical devices supportive services.
Acknowledgment
The author would like to acknowledge the assistance of the following academics, practitioners, and researchers in the validation of the questionnaire for the face and content: Professor Ab Fatah Ab Rahman (Professor of Clinical Pharmacy, Faculty of Medicine & Health Sciences, Universiti Sultan Zainal Abidin, Malaysia); Professor Mohamed Izham Mohamed Ibrahim (Professor of Social & Administrative Pharmacy, College of Pharmacy, Qatar University); Dr Ahmed Awaisu (College of Pharmacy, Qatar University); Dr Ali Alshahrani (College of Pharmacy, Taif University, Saudi Arabia); Dr Mona Alshiekh (College of Pharmacy, Taif University, Saudi Arabia); and Dr Fathelrahman Ibrahim Fathelrahman, MD, Ophthalmology.
Disclosure
The author reports no conflicts of interest in this work.
References
1. Wiedenmayer K, Summers RS, Mackie CA, et al. Developing Pharmacy Practice: A Focus on Patient Care: Handbook. World Health Organization; 2006.
2. Lin YY. Evolution of Pharm D education and patient service in the USA. J Exp Clin Med. 2012;4(4):227–230. doi:10.1016/j.jecm.2012.06.012
3. Roche C, Kelliher F. Exploring the patient consent process in community pharmacy practice. J Bus Ethics. 2009;86(1):91–99. doi:10.1007/s10551-008-9836-7
4. Gernant SA, Bacci JL, Upton C, et al. Three opportunities for standardization: a literature review of the variation among pharmacists’ patient care services terminology. Res Soc Admin Pharm. 2020;16(6):766–775. doi:10.1016/j.sapharm.2019.08.034
5. van Mil JF, Schulz M, Tromp TF. Pharmaceutical care, European developments in concepts, implementation, teaching, and research: a review. Pharm World Sci. 2004;26(6):303–311. doi:10.1007/s11096-004-2849-0
6. Fang Y, Yang S, Zhou S, Jiang M, Liu J. Community pharmacy practice in China: past, present and future. Int J Clin Pharm. 2013;35(4):520–528. doi:10.1007/s11096-013-9789-5
7. Pitkä K, Löfhjelm U, Passi S, Airaksinen M. Integrating internships with professional study in pharmacy education in Finland. Am J Pharm Educ. 2014;78(9):173. doi:10.5688/ajpe789173
8. Arimbawa PE, Adi IP. Patient perceptions on the role of a pharmacist and the understanding of the rational use of medicines (RUM). Sustain Sci Manag. 2019;14(6):137–144.
9. Basak SC, van Mil JF, Sathyanarayana D. The changing roles of pharmacists in community pharmacies: perception of reality in India. Pharm World Sci. 2009;31(6):612–618. doi:10.1007/s11096-009-9307-y
10. Tiralongo E, Braun LA, Wilkinson JM, et al. Exploring the integration of complementary medicines into Australian pharmacy practice with a focus on different practice settings and background knowledge. J Complement Integr Med. 2010;7(1). doi:10.2202/1553-3840.1411.
11. Omboni S, Caserini M. Effectiveness of pharmacist’s intervention in the management of cardiovascular diseases. Open Heart. 2018;5(1):e000687. doi:10.1136/openhrt-2017-000687
12. Shawahna R. Development of key performance indicators to capture in measuring the impact of pharmacists in caring for patients with epilepsy in primary healthcare: a Delphi consensual study. Epilepsy Behav. 2019;98:129–138. doi:10.1016/j.yebeh.2019.07.034
13. Tseng A, Foisy M, Hughes CA, et al. Role of the pharmacist in caring for patients with HIV/AIDS: clinical practice guidelines. Can J Hosp Pharm. 2012;65(2):125. doi:10.4212/cjhp.v65i2.1120
14. Alanazi AS, Alfadl AA, Hussain AS. Pharmaceutical care in the community pharmacies of Saudi Arabia: present status and possibilities for improvement. Saudi J Med Med Sci. 2016;4(1):9–14. doi:10.4103/1658-631X.170881
15. Alfadl AA, Alrasheedy AA, Alhassun MS. Evaluation of medication counseling practice at community pharmacies in Qassim region, Saudi Arabia. Saudi Pharm J. 2018;26(2):258–262. doi:10.1016/j.jsps.2017.12.002
16. Rasheed MK, Hasan SS, Babar ZUD. Community pharmacist’s knowledge, attitude, roles and practices towards patient-centred care in Saudi Arabia: a systematic review of the literature. J Pharmaceut Health Serv Res. 2019;10(1):101–115. doi:10.1111/jphs.12264
17. Alaqeel S, Abanmy NO. Counseling practices in community pharmacies in Riyadh, Saudi Arabia: a cross-sectional study. BMC Health Serv Res. 2015;15(1):1–9. doi:10.1186/s12913-015-1220-6
18. Gillani SW, Rahman SAU, Mohammad Abdul MI, Sulaiman SAS. Assessment of community pharmacists’ perceptions of healthcare services in Saudi Arabia. J Pharmaceut Health Serv Res. 2017;8(4):269–274. doi:10.1111/jphs.12183
19. Al-Hassan MI. A look at community pharmacy practice in Saudi Arabia. Res J Med Sci. 2009;3(3):111–114.
20. Alshahrani A. Readiness of community pharmacists to play a supportive and advocacy role in the fight against corona virus disease. Risk Manag Healthc Policy. 2020;13:3121. doi:10.2147/RMHP.S282825
21. Alshahrani AM, Alotaibi TM, Alrabie NS, et al. The viewpoint of community pharmacists about their professional role in dispensing beauty products: a study from Western Region of Saudi Arabia. Pharmacol Pharm. 2021;12(3):63–72. doi:10.4236/pp.2021.123006
22. Fathelrahman AI. Pharmacy students’ perception of their preparedness to counsel patients about medical devices: an exploratory study from Saudi Arabia. Arch Pharm Pract. 2020;11(4):94–99.
23. Fathelrahman AI. Readiness of Sudanese pharmacists to counsel patients about medical devices. Adv Pharmacol Pharm. 2020;8(4):59–65. doi:10.13189/app.2020.080401
24. AlRuthia Y, Alsenaidy MA, Alrabiah HK, AlMuhaisen A, Alshehri M. The status of licensed pharmacy workforce in Saudi Arabia: a 2030 economic vision perspective. Hum Resour Health. 2018;16(1):1–8. doi:10.1186/s12960-018-0294-8
25. IBM SPSS statistics for windows, version 22.0. US: IBM Corp.
26. Vella M, Grima M, Wirth F, et al. Consumer perception of community pharmacist extended professional services. J Pharmaceut Health Serv Res. 2015;6(2):91–96. doi:10.1111/jphs.12094
27. Okai GA, Abekah-Nkrumah G, Asuming PO. Perceptions and trends in the use of community pharmacies in Ghana. J Pharmaceut Policy Pract. 2019;12(1):1–9. doi:10.1186/s40545-019-0186-x
28. Kember J, Hodson K, James DH. The public’s perception of the role of community pharmacists in Wales. Int J Pharm Pract. 2018;26(2):120–128. doi:10.1111/ijpp.12375
29. Ooi GS, Hassali MA, Shafie AA, Kong DC, Mak VS, Chua GN. Consumers’ perspectives of Malaysian community pharmacists as health educators: a qualitative insight. J Pharm Pract Res. 2017;47(3):186–192. doi:10.1002/jppr.1219
30. Soubra R, Hlais S, Houmani N, et al. Health seeking behaviour among Lebanese population: a highlight on seeking care from pharmacists. Eur J Gen Pract. 2021;27(1):51–59. doi:10.1080/13814788.2021.1917541
31. Newman TV, Hernandez I, Keyser D, et al. Optimizing the role of community pharmacists in managing the health of populations: barriers, facilitators, and policy recommendations. J Manag Care Special Pharm. 2019;25(9):995–1000. doi:10.18553/jmcp.2019.25.9.995
32. Luisetto M. The medical devices pharmacists management role and pharmaceutical care. J App Pharm. 2016;8:e113.
33. Shah AR, Goyal RK. Current status of the regulation for medical devices. Indian J Pharm Sci. 2008;70(6):695. doi:10.4103/0250-474X.49085
34. Entwistle VA, Carter SM, Cribb A, McCaffery K. Supporting patient autonomy: the importance of clinician-patient relationships. J Gen Intern Med. 2010;25(7):741–745. doi:10.1007/s11606-010-1292-2
35. Rothman DJ. The origins and consequences of patient autonomy: a 25-year retrospective. Health Care Anal. 2001;9(3):255–264. doi:10.1023/A:1012937429109
36. Levin LS, Idler EL. Self-care in health. Annu Rev Public Health. 1983;4(1):181–201. doi:10.1146/annurev.pu.04.050183.001145
37. Evangelista LS, Shinnick MA. What do we know about adherence and self-care? J Cardiovasc Nurs. 2008;23(3):250. doi:10.1097/01.JCN.0000317428.98844.4d
38. Bhuyan KK. Health promotion through self-care and community participation: elements of a proposed programme in the developing countries. BMC Public Health. 2004;4(1):1–2. doi:10.1186/1471-2458-4-11
39. Erku DA, Mekuria AB, Surur AS, Gebresillassie BM. Extent of dispensing prescription-only medications without a prescription in community drug retail outlets in Addis Ababa, Ethiopia: a simulated-patient study. Drug Healthc Patient Saf. 2016;8:65. doi:10.2147/DHPS.S106948
40. Kalungia AC, Burger J, Godman B, Costa JD, Simuwelu C. Non-prescription sale and dispensing of antibiotics in community pharmacies in Zambia. Expert Rev Anti Infect Ther. 2016;14(12):1215–1223. doi:10.1080/14787210.2016.1227702
41. Bahnassi A. A qualitative analysis of pharmacists’ attitudes and practices regarding the sale of antibiotics without prescription in Syria. J Taibah Univ Med Sci. 2015;10(2):227–233. doi:10.1016/j.jtumed.2014.09.001
42. Soumya R, Devarashetty V, Jayanthi CR, Sushma M. Drug dispensing practices at pharmacies in Bengaluru: a cross-sectional study. Indian J Pharmacol. 2016;48(4):360. doi:10.4103/0253-7613.186204
43. Caamaño F, Tomé-Otero M, Takkouche B, Gestal-Otero JJ. Influence of pharmacists’ opinions on their dispensing medicines without requirement of a doctor’s prescription. Gac Sanit. 2005;19(1):9–14. doi:10.1157/13071811
44. Sabry NA, Farid SF, Dawoud DM. Antibiotic dispensing in Egyptian community pharmacies: an observational study. Res Soc Admin Pharm. 2014;10(1):168–184. doi:10.1016/j.sapharm.2013.03.004
45. Al-Mohamadi A, Badr A, Mahfouz LB, Samargandi D, Al Ahdal A. Dispensing medications without prescription at Saudi community pharmacy: extent and perception. Saudi Pharm J. 2013;21(1):13–18. doi:10.1016/j.jsps.2011.11.003
46. Rasheed MK, Alqasoumi A, Hasan SS. The community pharmacy practice change towards patient-centered care in Saudi Arabia: a qualitative perspective. J Pharmaecut Policy Pract. 2020;13(1):1–9. doi:10.1186/s40545-020-00267-7
47. Almaghaslah D, Alsayari A, Asiri R, Albugami N. Pharmacy workforce in Saudi Arabia: challenges and opportunities: a cross‐sectional study. Int J Health Plann Manage. 2019;34(1):e583–e593. doi:10.1002/hpm.2674
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
