Back to Journals » Therapeutics and Clinical Risk Management » Volume 14
Medial comminution as a risk factor for the stability after lateral-only pin fixation for pediatric supracondylar humerus fracture: an audit
Authors Kwak YH , Kim JH , Kim YC, Park KB
Received 18 February 2018
Accepted for publication 18 April 2018
Published 6 June 2018 Volume 2018:14 Pages 1061—1066
DOI https://doi.org/10.2147/TCRM.S165825
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Garry Walsh
Yoon Hae Kwak,1 Jae-Hyun Kim,2 Young-Chang Kim,2 Kun-Bo Park3
1Department of Orthopaedic Surgery, Hallym Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea; 2Department of Orthopedic Surgery, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea; 3Division of Orthopaedic Surgery, Severance Children’s Hospital, Yonsei University College of Medicine, Seoul, Korea
Background and purpose: Closed reduction and lateral-only pin fixation is one of the common treatment methods for displaced supracondylar fracture in children. However, several risk factors related to the stability have been reported. The aim of this study was to evaluate the medial comminution as a potential risk factor related to the stability after appropriate lateral-only pin fixation for Gartland type III supracondylar humerus fracture.
Methods: Sixty-seven patients with type III supracondylar fractures who were under the age of 12 years were included. Immediate postoperative and final Baumann and humerocapitellar angles were measured. Pin separation at fracture site was evaluated to estimate the proper pin placement. Presence of the medial comminution was recorded when two pediatric orthopedic surgeons agreed to the loss of cortical contact at the medial column by the small butterfly fragment or comminuted fracture fragments. Factors including age, sex, body mass index, pin number, pin separation at fracture site, and medial comminution were analyzed.
Results: Medial comminution was noted in 20 patients (29.8%). The average pin separation at fracture site was significantly decreased in patients with medial comminution compared to patients without medial comminution (P=0.017). A presence of medial comminution was associated with a 4.151-fold increase in the log odds for the Baumann angle changes of more than average difference between immediate postoperative and final follow-up angle (P=0.020).
Conclusion: When lateral-only pin fixation is applied for Gartland type III supracondylar humerus fracture in children, the medial comminution may be a risk factor for the stability because of the narrow pin separation at fracture site. We recommend additional medial pin fixation for supracondylar humerus fracture with medial comminution.
Keywords: humerus, supracondylar fracture, pin fixation
Introduction
Supracondylar humerus fracture is the most common elbow fracture in children.1,2 The standard treatment for displaced supracondylar fracture is closed reduction and percutaneous pin fixation, but there is controversy regarding ideal pin configuration in terms of stability and safety.3–6 When the pin is placed on the medial epicondyle, the stability increases but so does the risk of iatrogenic ulnar nerve injury. Although several previous clinical studies4,7–9 stated that there was no difference in maintenance of the reduction between cross pinning and lateral-only pinning, a previous biomechanical study10 suggested that cross-pin fixation provides greater torsional strength.
In the literature, loss of reduction has ranged from 0.3% to 0.6% after pin fixation.11,12 Some of the previous clinical studies4,13,14 reported that proper pin fixation is essential for maintaining the stability and that inappropriate lateral pin fixation is responsible for the loss of reduction. Besides surgical technique, other factors responsible for loss of reduction were reported including unstable fracture patterns such as the medial comminution, high fracture lines, or oblique fracture lines.15–19 In supracondylar fracture with oblique fracture line or high fracture line, lateral-only pin fixation is sometimes impossible or very difficult, so cross-pin fixation is preferred. However, in supracondylar fracture with medial comminution, lateral-only pin fixation is possible, and there is a trend toward lateral-only pin fixation.20
We hypothesized that medial comminution may be a risk factor for the stability after lateral-only pin fixation. The purpose of our study is to compare the surgical outcome between supracondylar fracture with and without medial comminution and to identify whether the medial comminution is related to the stability after lateral-only pin fixation.
Methods
Ethics approval and informed consent
This was a retrospective study of children with a Gartland21 type III supracondylar fracture based on radiography and medical records. All data were deidentified. This study did not need any kind of consents to participate and was approved by the Ethics Committee of Haeundae Paik Hospital (129792-2015-034).
Patients
This was a retrospective study in children with a Gartland21 type III supracondylar fracture. We retrospectively reviewed prospectively collected data of 111 patients from the period between March 2010 and June 2016. The inclusion criteria were age of <12 years, >6 months follow-up, and lateral-only pin fixation. The exclusion criteria were unstable pin fixation, such as 1) failure to engage both fragments with two or more pins; 2) failure to achieve bicortical fixation; and 3) failure to achieve pin separation >2 mm at the fracture.13 Sixty-seven patients were included in this study. The average age was 5 years 7 months (range, 1–11 years). Forty-three patients were boys and 24 were girls.
Surgical procedure
All fractures were fixed using the lateral-only fixation technique. First, two pins were inserted from the lateral aspect of elbow to the medial cortex. One pin was placed in the lateral column and the other pin had to be placed in the central column.4,14 The operator checked the stability by flexion and extension or gentle rotation. If the stability was not reliable, additional lateral fixation was added. At 3 weeks postoperative, radiographs were evaluated and the day for the removal of pin and cast was decided according to the fracture healing. After removal of the pin and cast, the patients start active daily living and range of motion exercise without passive physical therapy. Final follow-up radiography was performed at 6 months postoperative.
Variables
For radiographic analyses, the immediate postoperative and final follow-up anteroposterior (AP) and lateral radiographs were used. All AP radiographs were obtained with the upper arm flat on the cassette, the forearm in supine position and elbow at 45° flexion, because the elbow could not achieve full extension immediately after surgery, and after taking the cast off. Radiologic indices were measured by two orthopedic surgeons and averaged. The Baumann angle was calculated on the AP radiograph using the method of Williamson et al.22 The angle between the humeral shaft and the capitellum on a lateral radiograph defined as the humerocapitellar angle.16 Pin separation at fracture site was defined as the length between medial and lateral pin divided by the humerus width at the fracture site (Figure 1).18,23 Medial comminution was defined as a lack of cortical contact on the medial column by small butterfly fragment or comminuted small fragments after operation,18,19 and the presence or absence of medial comminution was recorded when two pediatric orthopedic surgeons agreed (Figure 2).
  | Figure 1 Pin separation was calculated using the formula: (B/A) × 100. |
  | Figure 2 Examples of medial comminution and the lack of cortical contact on medial column in anteroposterior radiography. |
Statistics
Statistical analyses were performed using SAS software (version 9.1; SAS Institute, Cary, NC, USA). Measurement reliability for the Baumann angle, humerocapitellar angle, and pin separation at fracture site was expressed as intraclass correlation coefficient, which ranged from 0.763 to 0.869. Independent t-test was used to compare continuous data between supracondylar fracture with medial comminution (Group I) and supracondylar fracture without medial comminution (Group II). Chi-squared test was used to compare categorical data. There was very small difference between immediate postoperative angle and final follow-up angle in Baumann angle and humerocapitellar angle. We defined the significant angle change during fracture healing period as a change of more than average difference between immediate postoperative angle and final follow-up angle. Multivariable logistic regression analysis was done to find factors related to the significant change of Baumann angle in age, sex, body mass index (BMI), pin number, pin separation at fracture site, and medial comminution. Values are presented as the mean ± SD, and the level of significance was defined at P<0.05.
Results
All patients showed complete union without significant complication. Average time from injury to operation was 25 ± 7 hours and average operation time was 32 ± 17 min. Average cast fixation period was 29.2 ± 4.5 days. One patient had a distal radius fracture on the same side. Two patients needed an open reduction. Before the operation, one patient showed median nerve palsy with radial nerve palsy, one patient had anterior interosseous nerve palsy, and two patients had radial nerve palsy. They all completely recovered without additional surgery. Two patients had superficial pin site infection, but it was improved after pin removal and bony union.
Usually, three Kirshner wires (range, 2–4) were used. Average pin separation at fracture site was 36.8% ± 6.8%. Average postoperative Baumann angle was 72.6° ± 5.3° and final Baumann angle was 71.8° ± 4.7°. Average Baumann angle difference was 4.0° ± 2.2°. All differences were <10°. Average postoperative humerocapitellar angle was 33.9° ± 11.3° and final humerocapitellar angle was 32.6° ± 9.9°. Average humerocapitellar angle difference was 1.3° ± 3.6°.
Medial comminution was noted in 20 patients. Twenty patients were classified as Group I and others were classified to Group II. There was no significant difference between groups, except the pin separation at fracture site (P=0.017) (Table 1). In multivariable logistic regression that evaluate the significant Baumann angle change (Nagelkerke R2 0.195), only the medial comminution was related to the Baumann angle change (OR =4.151 [95% CI 1.249–13.800], P=0.020) (Table 2).
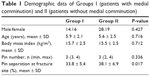  | Table 1 Demographic data of Groups I (patients with medial comminution) and II (patients without medial comminution) |
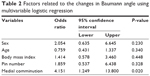  | Table 2 Factors related to the changes in Baumann angle using multivariable logistic regression |
Discussion
In 2001, Skaggs et al8 compared the cross-pinning and lateral pinning in Gartland type II and III fractures, and they recommend “do not use the routine cross pin”, because there was no difference in the maintenance of reduction. However, the maintenance of reduction after pinning for supracondylar humerus fracture is still surgeon’s concern in terms of the higher reliability of fixation. In a quantitative study,7 the rate of displacement after lateral-only pin fixation was 0.7%. A recent meta-analysis showed an overall loss of reduction rate of 4% for lateral entry-pin constructs and 2% for cross-pin constructs, although there was heterogeneity in data.24 However, to our knowledge, there has been no study about the risk factor for the loss of reduction after lateral-only pin fixation. We evaluated the medial comminution as a potential risk factor for the stability after lateral-only pin fixation.
The more important reason for the preference of the lateral-only pin fixation is avoidance of iatrogenic ulnar nerve injury. Topping et al9 found no loss of reduction in both methods and one ulnar nerve injury in cross-pinning. In a randomized prospective study with 52 patients, Kocher et al4 stated that there was no difference in loss of reduction and iatrogenic ulnar nerve injury between lateral and cross-pinning. The rate of iatrogenic ulnar nerve injury from cross-pinning was 3.4% in a systematic review12 and also the relative risk factor was 0.30 in another meta-analysis.6 Another study reported an 8-fold increase in the ulnar nerve injury after cross-pinning.25 In our series, there was no iatrogenic ulnar nerve injury, like the results of previous study with lateral-only pin fixation.14 The lateral-only fixation method is better than cross-pinning for the prevention of iatrogenic ulnar nerve injury.
A recent prospective study showed no iatrogenic injury after medial pin fixation and stated the importance of the preventive technique with a small incision on medial side and elbow extension during medial pin fixation.26 However, the technical points are similarly important in lateral-only fixation in terms of stability. Previous studies proposed a principle that distal humerus is separated into lateral, central, and medial columns, and that the lateral pin should engage at least two different columns.4,14 If the lateral fixation rule is followed, supracondylar humerus fractures can be treated stably without the risk of ulnar nerve injury. We have been followed the lateral fixation rule and aimed to identify risk factors related to the stability after accurate lateral-only pin fixation. Sankar et al13 highlighted three technical reasons for loss of reduction, and these were exclusion criteria in this study. Recently, the pin spread has been mentioned as an important factor associated with preventing loss of reduction.18,23 Pennock et al23 reported 4.2% loss of reduction rate with a definition of 10° differences. However, they reported no loss of reduction in 36% pin spread, which is similar to our 36.8% pin spread. In our series, the lateral pin fixation was technically appropriate.
In this study, medial comminution was evaluated as the risk factor for the stability after lateral-only pin fixation. De Boeck et al17 described the importance of medial column collapse. They reported cases of patients with medial column impaction as a cause of cubitus varus and the reason for this is that the injury is easily misdiagnosed as a simple supracondylar fracture with minimal displacement, requiring no reduction. Medial column is also important in the stability after lateral-only fixation because of the bicortical fixation.13 In terms of stability, considering the need for bicortical fixation when treating supracondylar fractures, medial comminution should be considered as an important issue, because that make pin spread narrow (Figure 3). In our study, the pin spread at fracture site in patients with medial comminution was significantly decreased compared to those in patients without medial comminution.
  | Figure 3 Due to medial comminution (white arrow), medial pin is more vertical than ideal position (dotted line). |
Medial comminution was also reported as a factor related to the loss of reduction in the previous study,18 although they compared cross-pinning and lateral-only pinning. The effect of medial column comminution to reduction loss was also demonstrated by biomechanical testing.19 Testers described the lack of support on medial column was related to the reduction loss. We selected cases that thoroughly followed the stable lateral pin fixation rule, and all the Baumann angle differences were below 10°. So, we tried to find any factor related to the Baumann angle change of more than average difference, and medial comminution was noted as a risk factor in the logistic regression analysis, although the difference was very small. If supracondylar humerus fracture with medial comminution was fixed with lateral-only pin fixation, there is a chance of Baumann angle change until bone union. So, more stable fixation than lateral-only pin fixation will be better, and we recommend additional medial pin fixation.
Our study has several limitations. This was a retrospective study including lateral-only pin fixation. Bahk et al16 reported that fractures with substantial degrees of obliquity (coronal obliquity >10° or sagittal obliquity >20°) may be more prone to rotational or extension malunion and should receive the most stable pin construct, whether it be a cross-pin configuration or a third lateral pin. We did not evaluate the fracture line, however, medial comminution may be a risk factor for the stability after lateral-only fixation in any fracture pattern. For pin fixation, we excluded cases with unstable pin fixation that were described by Sankar et al13 and this may have led to another selection bias. But, because of this selection, we can conclude that the only medial comminution is related to the stability after stable lateral-only pin fixation.
Conclusion
When lateral-only pin fixation is applied for Gartland type III supracondylar humerus fracture, medial comminution may be a risk factor of the stability because of the narrow pin separation at fracture site. Supracondylar humerus fracture with medial comminution should be fixed more carefully, and we recommend additional medial pin fixation.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
This work was supported by a grant from Research year of Inje University 2015 (20140648).
The authors wish to thank Dong-Su Jang, MFA (medical illustrator) for his help with the electronic artwork, and Min-Kyung Oh, PhD for her help with the statistical analysis.
Author contributions
KBP and YCK conceived and designed this research. JHK and KBP acquired the data. KBP and YHK drafted the manuscript. KBP revised the manuscript. All authors read and approved the final manuscript. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
Farnsworth CL, Silva PD, Mubarak SJ. Etiology of supracondylar humerus fractures. J Pediatr Orthop. 1998;18:38–42. | ||
Otsuka NY, Kasser JR. Supracondylar fractures of the humerus in children. J Am Acad Orthop Surg. 1997;5:19–26. | ||
Gaston RG, Cates TB, Devito D, et al. Medial and lateral pin versus lateral-entry pin fixation for Type 3 supracondylar fractures in children: a prospective, surgeon-randomized study. J Pediatr Orthop. 2010;30:799–806. | ||
Kocher MS, Kasser JR, Waters PM, et al. Lateral entry compared with medial and lateral entry pin fixation for completely displaced supracondylar humeral fractures in children. J Bone Joint Surg Am. 2007;89:706–712. | ||
Ozturkmen Y, Karamehmetoglu M, Azboy I. Closed reduction and percutaneous lateral pin fixation in the treatment of displaced supracondylar fractures of the humerus in children. Acta Orthop Traumatol Turc. 2005;39:396–403. | ||
Zhao J-G, Wang J, Zhang P. Is lateral pin fixation for displaced supracondylar fractures of the humerus better than crossed pins in children? Clin Orthop Relat Res. 2013;471:2942–2953. | ||
Maity A, Saha D, Roy DS. A prospective randomised, controlled clinical trial comparing medial and lateral entry pinning with lateral entry pinning for percutaneous fixation of displaced extension type supracondylar fractures of the humerus in children. J Orthop Surg Res. 2012;7:6. | ||
Skaggs DL, Hale JM, Bassett J, Kaminsky C, Kay RM, Tolo VT. Operative treatment of supracondylar fractures of the humerus in children. J Bone Joint Surg Am. 2001;83(5):735–740. | ||
Topping RE, Blanco JS, Davis TJ. Clinical evaluation of crossed-pin versus lateral-pin fixation in displaced supracondylar humerus fractures. J Pediatr Orthop. 1995;15:435–439. | ||
Zionts LE, McKellop HA, Hathaway R. Torsional strength of pin configurations used to fix supracondylar fractures of the humerus in children. J Bone Joint Surg Am. 1994;76(2):253–256. | ||
Bashyal RK, Chu JY, Schoenecker PL, Dobbs MB, Luhmann SJ, Gordon JE. Complications after pinning of supracondylar distal humerus fractures. J Pediatr Orthop. 2009;29:704–748. | ||
Brauer CA, Lee BM, Bae DS, Waters PM, Kocher MS. A systematic review of medial and lateral entry pinning versus lateral entry pinning for supracondylar fractures of the humerus. J Pediatr Orthop. 2007;27:181–186. | ||
Sankar WN, Hebela NM, Skaggs DL, Flynn JM. Loss of pin fixation in displaced supracondylar humeral fractures in children: causes and prevention. J Bone Joint Surg Am. 2007;89(4):713–717. | ||
Skaggs DL, Cluck MW, Mostofi A, Flynn JM, Kay RM. Lateral-entry pin fixation in the management of supracondylar fractures in children. J Bone Joint Surg Am. 2004;86(4):702–707. | ||
Alton TB, Werner SE, Gee AO. Classifications in brief: the Gartland classification of supracondylar humerus fractures. Clin Orthop Relat Res. 2015;473:738–741. | ||
Bahk MS, Srikumaran U, Ain MC, et al. Patterns of pediatric supracondylar humerus fractures. J Pediatr Orthop. 2008;28:493–499. | ||
De Boeck H, De Smet P, Penders W, De Rydt D. Supracondylar elbow fractures with impaction of the medial condyle in children. J Pediatr Orthop. 1995;15:444–448. | ||
Reisoglu A, Kazimoglu C, Hanay E, Agus H. Is pin configuration the only factor causing loss of reduction in the management of pediatric type III supracondylar fractures? Acta Orthop Traumatol Turc. 2017;51:34–38. | ||
Silva M, Knutsen AR, Kalma JJ, et al. Biomechanical testing of pin configurations in supracondylar humeral fractures: the effect of medial column comminution. J Orthop Trauma. 2013;27(5):275–280. | ||
Sinikumpu JJ, Pokka T, Sirviö M, Serlo W. Gartland Type II supracondylar humerus fractures, their operative treatment and lateral pinning are increasing: a population-based epidemiologic study of extension-type supracondylar humerus fractures in children. Eur J Pediatr Surg. 2017;27(5):455–461. | ||
Gartland JJ. Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet. 1959;109(2):145–154. | ||
Williamson DM, Coates CJ, Miller RK, Cole WG. Normal characteristics of the Baumann (humerocapitellar) angle: an aid in assessment of supracondylar fractures. J Pediatr Orthop. 1992;12(5):636–639. | ||
Pennock AT, Charles M, Moor M, Bastrom TP, Newton PO. Potential causes of loss of reduction in supracondylar humerus fractures. J Pediatr Orthop. 2014;34:691–697. | ||
Woratanarat P, Angsanuntsukh C, Rattanasiri S, Attia J, Woratanarat T, Thakkinstian A. Meta-analysis of pinning in supracondylar fracture of the humerus in children. J Orthop Trauma. 2012;26:48–53. | ||
Abbott MD, Buchler L, Loder RT, Caltoum CB. Gartland type III supracondylar humerus fractures: outcome and complications as related to operative timing and pin configuration. J Child Orthop. 2014;8(6):473–477. | ||
Kwak-Lee J, Kim R, Ebramzadeh E, Silva M. Is medial pin use safe for treating pediatric supracondylar humerus fractures? J Orthop Trauma. 2014;28:216–221. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
