Back to Journals » Patient Related Outcome Measures » Volume 10
Measurement properties of the Fear-Avoidance Belief Questionnaire for physical activity in patients with shoulder impingement syndrome
Authors Trolle N, Christiansen DH
Received 22 October 2018
Accepted for publication 1 January 2019
Published 19 March 2019 Volume 2019:10 Pages 83—87
DOI https://doi.org/10.2147/PROM.S191782
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Lynne Nemeth
Nûno Trolle,1 David H Christiansen1,2
1Danish Ramazzini Centre, Regional Hospital West Jutland, Department of Occupational Medicine, University Research Clinic, Herning, Denmark; 2Department of Clinical Medicine, Health, Aarhus University, Aarhus, Denmark
Background: The Fear-Avoidance Belief Questionnaire for physical activity (FABQ-PA) was originally developed for patients with low-back pain. Whether the FABQ-PA is suitable for use among patients with other musculoskeletal disorders has been sparsely evaluated.
Purpose: To evaluate test–retest reliability, measurement error, construct validity, and responsiveness of the FABQ-PA in patients with shoulder impingement syndrome (SIS).
Methods: This prospective cohort study included 45 patients with SIS. Data were collected with questionnaires at baseline, after 2–4 days, and at 3 months, which included the Danish versions of the FABQ-PA and the Oxford Shoulder Score (OSS). Test–retest reliability was assessed by intraclass correlation, and standard error of measurement was estimated and converted into the minimal detectable change (MDC). Construct validity was investigated by analyzing the correlation between the baseline scores of the FABQ-PA and the OSS. Responsiveness was investigated from longitudinal construct validity using a correlation analysis reflecting changes over time.
Results: Test–retest reliability showed an intraclass correlation of 0.80, and examination of the measurement error showed no systematic differences and a MDC of 7.95 (95% CI 6.57–10.07). Construct validity showed a correlation of –0.60 (95% CI –0.76 to –0.37) between the FABQ-PA and OSS at baseline. A weaker correlation between FABQ-PA- and OSS-change scores was observed (–0.43, 95% CI –0.67 to –0.12).
Conclusion: The Danish version of the FABQ-PA is suitable for assessing fear-avoidance beliefs in groups of patients with SIS, but its ability to evaluate individual patients and changes over time may be more limited.
Keywords: outcome measures, validity, reliability, measurement error, responsiveness
Background
Shoulder impingement syndrome (SIS) is one of the most common causes of shoulder pain.1,2 SIS is often a recurrent problem, with a low recovery rate.3 This indicates that SIS can lead to chronic pain, which can affect the patient both physically and mentally. The fear-avoidance model of exaggerated pain perception describes how pain-related fear can impact outcomes. The model argues that avoiding physical activity due to fear of pain (fear-avoidance behavior) can have negative consequences for patients with musculoskeletal pain by contributing to chronic pain development.4 One of the most commonly used questionnaires to asses fear avoidance in patients with musculoskeletal pain is the Fear-Avoidance Belief Questionnaire (FABQ) developed by Waddell et al.5 The FABQ screening tool was originally developed for patients with low-back pain (LBP). The subscale for physical activity (Fear-Avoidance Belief Questionnaire for physical activity [FABQ-PA]) has been shown to be a reliable and valid measure of fear-avoidance behavior in patients with LBP.6 A recent study argued that the FABQ is the most suitable measure also for assessing fear-avoidance behavior in patients with shoulder pain.7 The study showed high test–retest reliability of the FABQ-PA, but several important aspects of the measurement properties, such as measurement error and responsiveness, were not established.8 Furthermore, measurement properties may vary across countries, and should thus be evaluated in the population in which they are going to be utilized.8 The FABQ-PA has been translated and cross-culturally adapted to the Danish population among patients with LBP,9 but its measurement properties have not been evaluated in SIS patients. The aim of the present study was thus to evaluate reliability, measurement error, construct validity, and responsiveness of the Danish version of the FABQ-PA.
Methods
Design and population
Subjects included in this prospective cohort study were patients with SIS recruited from rehabilitation units, physical therapy clinics, and one hospital in the Central Denmark Region.10 We included patients who were aged 18 years or more and diagnosed with SIS by a medical doctor or physical therapist. Exclusion criteria included other shoulder pathologies, any surgical treatment in the affected shoulder during the past 12 months, mental disorders, or insufficient Danish-language skills to communicate and complete the questionnaires.
Procedure
Patients were recruited in between October 31 and December 15, 2011. Patients completed questionnaires at three time points: baseline (T0), 2–4 days after baseline (T1), and at 3 months (T2). The questionnaire included the FABQ-PA and the Oxford Shoulder Score (OSS). The FABQ-PA contains five items, of which four are added to a sum score of 0–24, with 0 being the best outcome. The OSS questionnaire has been developed to assess patients with degenerative or posttraumatic shoulder diseases.11 It contains 12 items related to pain and functional ability, and the sum score ranges from 0 to 48, with 48 being the best outcome. The OSS has shown acceptable validity and reliability11 and a good level of responsiveness.12
Statistical analysis
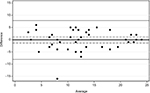
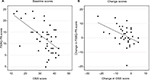
A minimum sample size of 50 subjects was recommended in a method-comparison study for sufficient precision.8 Descriptive statistics were calculated for all variables. Test–retest reliability was investigated using an intraclass correlation coefficient (ICC) with 95% CI calculated in long format 2.1. The test–retest interval was between T0 and T1. Paired t-tests were used to assess systematic differences between T0 and T1 scores on the FABQ-PA. Measurement error was assessed by test–retest and is presented as 95% limits of agreement. Bland–Altman plots were made by plotting differences between the two measurements against the mean of the two sum scores, showing 95% limits of agreement and 95% CI. Minimal detectable change (MDC) was estimated by first calculating the standard error of measurement (SEM) between the T0 score and the T1 score (SEM = SD/√2). SEM was then converted into MDC (MDC = 1.96 × √2 × SEM).8 Construct validity was evaluated by correlation analysis (Pearson) of T0 scores of the FABQ-PA and the OSS. Last responsiveness was assessed as longitudinal construct validity by calculating Pearson’s correlation coefficient of change scores from T0 to T2 of the FABQ-PA with the OSS.8 We hypothesized an acceptable test–retest reliability corresponding to an ICC >0.70 based on applicable standards.8 Correlation coefficients of FABQ-PA and OSS scores were interpreted as weak (r<0.3) to moderate (r>0.3 and<0.6) correlations. For statistical analysis, Stata version 15 software was used.
Results
Descriptive statistics
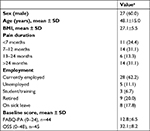
A total of 74 patients were assessed for eligibility, of whom 9 were excluded, 3 did not show up, 2 withdrew, 2 became ill, and 13 declined participation.10 The final study population thus included 45 patients. Baseline characteristics of the included patients are presented in Table 1. One patient failed to complete the FABQ-PA questionnaire at T0 and T1 and was excluded from analysis. A total of 37 patients completed the follow-up questionnaire at 3 months.
Measurement properties
Test–retest reliability displayed an ICC of 0.80 (95% CI 0.70–0.91). No statistically significant systematic differences were found between T0 and T1 on the FABQ-PA (–0.14, 95% CI –1.37 to 1.10), 95% limits of agreement were estimated to be –8.07 to 7.81 (Figure 1), and the MDC was 7.95 (95% CI 6.57–10.07). Assessment of construct validity at T0 between the FABQ-PA and OSS showed r= –0.60 (95% CI –0.76 to –0.37) (Figure 2A). Absolute mean changes from T0 to T2 for the FABQ-PA were –1.86 (95% CI –4.05 to 0.33) and 4.57 (95% CI 2.59, 6.54) for the OSS. Change scores from T0 to T2 for the FABQ-PA and the OSS (Figure 2B) displayed r= –0.43 (95% CI –0.67 to –0.12).
Discussion
Measurement properties for the Danish version of the FABQ-PA were established in patients with SIS. Test–retest reliability was found to be acceptable, and construct validity was confirmed by a moderate correlation with the OSS. In patient-reported outcomes, it is generally recommended that reliability coefficients at least exceed 0.70 to distinguish between groups in clinical trials and 0.90 to assess individual patients.13 According to these recommendations, the FABQ-PA may be most suitable for evaluation at group level. The estimated MDC indicates that a minimum of 8 points are needed to detect a “true” within-person change in the total score of 24 points. Although construct validity was confirmed by a moderate level of correlation between the FABQ-PA and OSS at baseline, the weaker correlation observed for change scores may suggest the longitudinal construct validity (responsiveness) to be more limited. The results of the present study are in line with those of a previous study,6 which reported an ICC of 0.88 (95% CI 0.75–0.93) for the FABQ-PA in patients with shoulder pain. To our knowledge, the present study is the first to evaluate measurement error and responsiveness of the FABQ in patients with shoulder pain. The construct validity and measurement error of the FABQ-PA have previously been evaluated in Norwegian patients with LBP, where a moderate correlation with disability and an MDC of 8.95 points were found.6 Equivalent findings were obtained in the present study. Grotle et al found a moderate level of responsiveness for the FABQ-PA. Our results may suggest a weaker level of responsiveness for the FABQ-PA in patients with SIS, corresponding to what has previously been reported for patients with LBP.14 Limitations of the present study include that our findings may be generalized only to patients with symptoms of SIS. Another limitation is that the time interval between T0 and T1 was shorter than what was suggested by one author,15 while others16 proposed time intervals similar to those used in the present study. The time interval was chosen in order to minimize changes in the patients’ clinical condition, as all patients were attending physiotherapy treatment. Additionally, it was determined that the time interval was long enough to minimize recall bias. Finally, a limitation is that the sample size in the present study did not completely fulfill general recommendations for method-comparison studies.8 This may have affected the precision of our estimates.
Conclusion
The present study found acceptable test–retest reliability and confirmed construct validity of the Danish version of the FABQ-PA in patients with symptoms of SIS. However, the FABQ-PA questionnaire may be more suited for group evaluation than individual patients, and the relatively large measurement error and low responsiveness needs to be taken into account when evaluating change over time.
Ethics approval and informed consent
The study was approved by the Danish Data Protection Agency (2015-41-4343), and all participants signed written informed consent forms. The Regional Research Ethics Committee determined that formal ethical approval was not required for this study.17
Data sharing statement
The data set from the current study cannot be made publicly available according to Danish regulations. Data are however available from the authors upon reasonable request and permission of the Danish Data Protection Agency.
Author contributions
Both authors contributed toward data analysis, drafting and critically revising the paper, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Acknowledgments
The authors wish to thank Birgitte O Simonsen, RN and Julie Boje, RN for valuable assistance in the study. The authors received no financial support for the research, authorship, or publication of this article.
Disclosure
The authors report no conflicts of interest in this work.
References
Pope DP, Croft PR, Pritchard CM, Silman AJ. Prevalence of shoulder pain in the community: the influence of case definition. Ann Rheum Dis. 1997;56(5):308–312. | ||
Mitchell C, Adebajo A, Hay E, Carr A. Shoulder pain: diagnosis and management in primary care. BMJ. 2005;331(7525):1124–1128. | ||
van der Windt DA, Koes BW, Boeke AJ, Devillé W, De Jong BA, Bouter LM. Shoulder disorders in general practice: Prognostic indicators of outcome. Br J Gen Pract. 1996;46(410):519–523. | ||
George SZ. Fear: a factor to consider in musculoskeletal rehabilitation. J Orthop Sports Phys Ther. 2006;36(5):264–266. | ||
Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A fear-avoidance beliefs questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52(2):157–168. | ||
Grotle M, Brox JI, Vøllestad NK. Reliability, validity and responsiveness of the fear-avoidance beliefs questionnaire: methodological aspects of the Norwegian version. J Rehabil Med. 2006;38(6):346–353. | ||
Mintken PE, Cleland JA, Whitman JM, George SZ. Psychometric properties of the Fear-Avoidance Beliefs Questionnaire and Tampa scale of kinesiophobia in patients with shoulder pain. Arch Phys Med Rehabil. 2010;91(7):1128–1136. | ||
Terwee CB, Bot SD, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42. | ||
Jacobsen JS, Mogensen KM. Fear-Avoidance Beliefs Questionnaire - Translation into Danish and test of the Danish version on ten low back pain patients. Available from: http://docplayer.dk/5246746-Fear-avoidance-beliefs-questionnaire.html. Published 2007. Accessed February 12, 2018. | ||
Moeller AD, Thorsen RR, Torabi TP, et al. The Danish version of the modified Constant-Murley shoulder score: reliability, agreement, and construct validity. J Orthop Sports Phys Ther. 2014;44(5):336–A5. | ||
Dawson J, Rogers K, Fitzpatrick R, Carr A. The Oxford shoulder score revisited. Arch Orthop Trauma Surg. 2009;129(1):119–123. | ||
Christiansen DH, Frost P, Falla D, Haahr JP, Frich LH, Svendsen SW. Responsiveness and minimal clinically important change: a comparison between 2 shoulder outcome measures. J Orthop Sports Phys Ther. 2015;45(8):620–625. | ||
Fayers PM, Machin D, editors. Quality of Life: The assessment, analysis and interpretation of patient-reported outcomes. 2nd ed. Chichester: John Wiley & Sons Ltd; 2007. | ||
Chapman JR, Norvell DC, Hermsmeyer JT, et al. Evaluating common outcomes for measuring treatment success for chronic low back pain. Spine (Phila Pa 1976). 2011;36(21 Suppl):S54–S68. | ||
Scholtes VA, Terwee CB, Poolman RW. What makes a measurement instrument valid and reliable? Injury. 2011;42(3):236–240. | ||
Huber W, Hofstaetter JG, Hanslik-Schnabel B, Posch M, Wurnig C. The German version of the Oxford shoulder score – cross-cultural adaptation and validation. Arch Orthop Trauma Surg. 2004;124(8):531–536. | ||
NVK [homepage on the Internet] Act on Research Ethics Review of Health Research Projects. Available from: http://www.nvk.dk/english/act-on-research. Accessed March 8, 2018. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.