Back to Journals » Patient Preference and Adherence » Volume 15
Maternal Knowledge Associated with the Prevalence of Iron and Folic Acid Supplementation Among Pregnant Women in Muntinlupa, Philippines: A Cross-Sectional Study
Authors Yamashita T , Roces RED, Ladines-Llave C , Reyes Tuliao MT, Wanjira Kamau M , Yamada C , Tanaka Y, Shimazawa K, Iwamoto S, Matsuo H
Received 13 November 2020
Accepted for publication 30 January 2021
Published 1 March 2021 Volume 2021:15 Pages 501—510
DOI https://doi.org/10.2147/PPA.S291939
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Tadashi Yamashita,1 Ramon Emilio Daniel Roces,2 Cecilia Ladines-Llave,2 Maria Teresa Reyes Tuliao,3 Mary Wanjira Kamau,4 Chika Yamada,5,6 Yuko Tanaka,7 Kyoko Shimazawa,1 Saori Iwamoto,1 Hiroya Matsuo6
1Kobe City College of Nursing, Kobe, Japan; 2Hospital of Muntinlupa, Muntinlupa, Philippines; 3City Health Office, City Government of Muntinlupa, Muntinlupa, Philippines; 4School of Nursing Sciences, University of Nairobi, Nairobi, Kenya; 5Department of Environment Coexistence, Center for Southeast Asian Studies, Kyoto University, Kyoto, Japan; 6Department of Public Health, Graduate School of Health Sciences, Kobe University, Kobe, Japan; 7Department of School Health Sciences, Institute of Biomedical Sciences, Tokushima University, Tokushima, Japan
Correspondence: Tadashi Yamashita
Kobe City College of Nursing, 3-4 Gakuennishi-Machi, Nishi-Ku, Kobe, 651-2103, Japan
Tel/Fax +81-78-794-8079
Email [email protected]
Purpose: The World Health Organization advocates that all pregnant women in areas where anemia is prevalent receive supplements of iron and folic acid. However, owing to a myriad of factors, the uptake of iron and folic acid supplementation (IFAS) is still low in many countries. Therefore, this study was conducted to assess the prevalence of IFAS and its associated factors among pregnant women.
Patients and Methods: A cross-sectional study was conducted at a hospital in Muntinlupa, Philippines, between March and August 2019 among 280 pregnant women. A systematic random sampling technique was used to select participants. Data were collected using interviewer-administered questionnaires. Multivariable logistic regression analyses were employed to identify factors associated with the prevalence of IFAS among pregnant women.
Results: Among 280 pregnant women, a majority (85.6%, n= 238) took IFAS during pregnancy. Among the respondents, 128 (45.9%) women had knowledge about signs and symptoms of anemia, 126 (45.3%) had knowledge of the benefits associated with IFAS, and 42 (15.4%) had knowledge about side effects associated with IFAS. The main sources of information about IFAS were health care providers (41.8%), followed by community health workers (CHWs) (14.6%). Maternal knowledge concerning IFAS benefits (OR = 2.50, CI = 1.04– 5.97, p=0.04) was positively associated with the prevalence of IFAS.
Conclusion: Maternal knowledge about the benefits of taking IFAS was significantly associated with the prevalence of IFAS among pregnant women in Muntinlupa, Philippines. There is a pressing need to improve health education on the benefits of IFAS among pregnant women to increase its prevalence. This emphasizes the necessity of increased involvement of health care providers and CHWs to increase women’s knowledge of IFAS benefits and support them through pregnancy.
Keywords: anemia, pregnancy, health education, health care providers, community health workers
Introduction
The World Health Organization (WHO) estimates that worldwide, 613 million women at reproductive age are anemic, and a vast majority of anemic pregnant women reside in Asia and Africa.1 In the Philippines, anemia prevalence among pregnant women remains high as shown in the National Nutrition Surveys in 2003 (43.9%), 2008 (42.5%), and 2013 (25.2%).2,3 Anemia during pregnancy (ie hemoglobin level less than 11 g/dL) can lead to adverse maternal and perinatal outcomes, including mortality.4–13 The WHO recommends that all pregnant women in areas where anemia is prevalent should receive iron and folic acid supplementation (IFAS).1,14 Despite the WHO recommendations, the utilization of IFAS is still low in many countries, especially those with low economic resources.11,15
The Philippines’ national guideline for the prevention of micronutrient deficiencies highlights the need for daily IFAS during pregnancy.16 Various factors such as socio-demographic and health factors determine the IFAS regime for pregnant women in some areas including the Philippines. These factors include forgetfulness, travel, age, literacy, socioeconomic status, cost of iron and folic acid tablets, perceived side effects, supplement stock-outs, birth order, difficult accessing and poor utilization of antenatal health care services, and comprehensive knowledge of anemia as well as quality of counselling on IFAS during pregnancy.17–34 Nevertheless, supplementation is the most widely employed strategy to alleviate iron deficiency, both globally and locally.3,35 Women take IFAS during pregnancy to prevent specific micronutrient deficiencies under the programs provided by the government of the Philippines.3,35,36 In the Philippines, Patient-level care is provided at widely utilized barangay (village) health stations (BHS) that are operated by trained midwives. The midwife in each BHS identified all the pregnant women who had received IFAS from that BHS during their pregnancy.37 At each monthly prenatal visit to the BHS, IFAS is provided free of charge to pregnant women.35,38 The Philippines National Survey in 2008, which measured the uptake of IFAS, found consumption of 82.4% of prescribed pills among pregnant women.39,40 Thus, taking iron and folic acid supplements is an important strategy to prevent anemia among pregnant women. The present research is one of the studies that seek to check the effectiveness of the current Philippines program with the strategy whereby women would receive free IFAS from the BHS during pregnancy.
However, no published data exist to assess the administration of such supplementation and its associated factors among pregnant women in the Philippines. The Muntinlupa City of the Philippines is located in the Luzon region and divided into nine districts, and the city has a public city hospital—the Muntinlupa City hospital. The hospital provides health services at the lowest possible costs; therefore, in Muntinlupa, not only rich but also poor pregnant women use public hospitals. Although it is often difficult to approach poor pregnant women in studies, this study was able to approach pregnant women across all economic levels by conducting the study at the hospital. Thus, this study was conducted specifically to assess the prevalence of IFAS among pregnant women and its associated factors in Muntinlupa, Philippines.
Patients and Methods
Study Site and Design
A cross-sectional study was conducted at the women’s health center in the hospital of Muntinlupa City and data were collected between March and August 2019. In addition, 900 pregnant women were receiving antenatal care during the data collection period based on a search of electronic records. Muntinlupa City has nine districts, each with one or two government health centers, including an outpatient clinic. The Muntinlupa City hospital provides health services at the lowest possible costs. In addition, the women’s health center in the hospital provides counseling to all women living in the area.
Sample Size Determination and Sampling Procedure
The required sample size for this study was determined using the single population proportion estimation formula and considering the following assumptions: the rate of taking IFAS among pregnant women was 82.4% in 2008 in the Phillippines,39 a 95% confidence interval, and 5% acceptable margin of error. The calculated sample size required 267 participants. Finally, considering a 10% non-response rate, the final sample size was set at 280. After the proportional allocation of pregnant women in the women’s health center, a systematic random sampling technique was employed to include 280 participants. Sampling fraction (K) was N/n = 900/280 = 3.2. Thereafter, the lottery method was employed to identify the first pregnant woman for an interview and upon selection, every third pregnant woman thereafter was chosen to commence the interview. Consequently, all women were identified.
Study Population and Sampling
The study population consists of pregnant women, aged 18–45 years, attending antenatal check-ups in the respective hospital and living in Muntinlupa City. Each participant provided written, informed consent. Women who were seriously ill at the time of data collection were excluded. The interview was conducted just after receiving the antenatal care service.
Data Collection Methods
Data were collected using the interviewer-administered questionnaire. A structured, interviewer-administered questionnaire consisting of 26 closed-ended questions were developed, pretested, and used in this study. Questions were categorized into: socio-demographic characteristics (6), maternal knowledge on taking IFAS and knowledge on major signs and symptoms of anemia (19), and current practices towards IFAS (1). To ensure the reliability of the questionnaire, we adopted a test-retest method where a repeat pre-test was conducted after two weeks, while Cohen’s kappa statistic was used to measure the level of agreement between the results from the pre-tests. Since all the questions had a kappa value of above 0.7 after the comparison, the questionnaire was considered reliable, thus, all the questions were retained. To ensure validity, the tool was shared and discussed with experts from the division of nutrition of the City Government Office, as well as the study supervisors. The obtained feedback was used to refine the tool. The questionnaires, which were written in Tagalog (ie the national language of the Philippines), were administered by trained research assistants to all pregnant women who met the inclusion criteria and consented to the study.
Data Analyses
Descriptive statistics were employed to describe the study population in relation to socio-demographic and other relevant variables and to display findings through means, percentages, and 95% confidence intervals. The primary outcome variable for this study was the prevalence of IFAS, which was assessed with the question: “Have you taken IFAS during the current pregnancy?” To assess the level of knowledge about IFAS during pregnancy, respondents were asked three questions including (1) major signs and symptoms of anemia during pregnancy, (2) the benefits of taking IFAS, and (3) side-effects of taking IFAS. The respondents’ level of knowledge was computed by summing up seven items with respect to the signs and symptoms of anemia (“Feels weak,” “Looks pale,” “Palpitations,” “Headaches,” “Dizziness,” “Tiredness and easily fatigued,” and “Swollen legs”), five items concerning the benefits of IFAS (“Prevents anemia among pregnant women,” “Protects mother from sicknesses,” “Gives mother strength during delivery,” “Increases the amount of blood,” and “Facilitates the fetus to grow healthy and strong”), and seven items regarding the side-effects of IFAS (“Epigastric pain,” “Abdominal pain,” “Nausea,” “Vomiting,” “Diarrhea,” “Constipation,” and “Feces may turn black”). A correct answer for each item was scored as “1” and the incorrect answer was scored as “0.” Pregnant women were classified as highly knowledgeable and slightly knowledgeable about the benefits and side effects of taking IFAS and major signs and symptoms of anemia during pregnancy. Those who scored greater than or equal to the mean value were considered as highly knowledgeable and those who scored less than the mean value were considered as slightly knowledgeable. The distribution of the knowledge scores was approximately normal; therefore, the average value was used for the analysis. To test for multicollinearity among independent variables, we ran collinearity diagnostics to calculate the variance inflation factor and tolerance for each variable. Bivariate logistic regression analyses were carried out to evaluate the unadjusted associations between dependent variables and each of the independent variables. Significant variables in the bivariate logistic regression analyses (p-value < 0.01) were incorporated into the multivariable logistic regression analyses to identify factors associated with the prevalence of IFAS among pregnant women.
In this study, pregnant women who did not answer questions about their age, gestation, and whether they took IFAS were excluded from the analysis. Data were analyzed using the Statistical Package for the Social Sciences (SPSS) 26.0 (IBM Corp., Armonk, NY, USA).
Ethical Considerations
The study was conducted by following per under the declaration of Helsinki. The study was approved by the Hospital of Muntinlupa, Research Operation Office (No. 2019–02), and Kobe City College of Nursing, Ethics, and Research Committee (No. 18112–05). Participation in the study was purely voluntary. The study participants provided verbal and written informed consent before the commencement of the interview. Participants were told they could withdraw from the study anytime without any consequences. The purpose of the study and the assurance of confidentiality of information were explained to participants. They were also told they could decide not to answer any question they felt uncomfortable with.
Results
A total of 280 pregnant women participated in the study. The mean age of the study participants was 28.3 (SD ± 6.5) years, with a majority (51.1%, n=143) between 25 and 34 years of age. Regarding their occupational status, 35.6% (n=98) were employed. Relating to the highest level of education attained by the respondents, a majority (88.2%, n=246) had a secondary school degree or above. The highest proportion of respondents (59.6%, n=159) earned an average household monthly income below 9999 Philippines pesos. The poverty threshold of the Philippines in 2018 was 10,000 Philippines pesos.41 More than half of the women were multipara (59.3%, n=166). Furthermore, the mean gestational age of pregnant women was 29.9 (SD = ±8.7) weeks, and the majority of the participants were in their third trimester (78.2%, n=219) (Table 1).
 |
Table 1 Socio-Demographic Characteristics, Prevalence of IFAS, and Maternal Knowledge of Pregnant Women (n=280) |
Among the respondents, the majority (85.6%, n=238) were taking IFAS during their current pregnancy. Those found knowledgeable in the assessment of various aspects of IFAS were categorized as follows: knowledge on signs and symptoms of anemia: 45.9% (n=128), benefits of taking IFAS: 45.3% (n=126), and side effects of IFAS: 15.4% (n=42) (Table 1). The highest proportion of knowledge related to the various benefits of IFAS among pregnant women was for “Prevents anemia among pregnant women” (76.4%), followed by “Increases the amount of blood” (50.7%), “Facilitates the fetus to grow healthy and strong” (46.1%), “Protects mother from sicknesses” (43.9%), and “Gives mothers strength during delivery” (41.1%) (Figure 1).
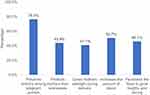 |
Figure 1 Knowledge status on benefits of iron and folic acid supplementation among pregnant women. |
Pregnant women reported various sources of IFAS information. The main source of information was health care providers (41.8%). Other sources of information included community health workers (CHWs) (14.6%), relatives/friends/neighbors (8.6%), the Internet (6.8%), posters/television/radio (5.4%), newspapers/magazines/books (1.4%), and community leaders (0.4%) (Figure 2).
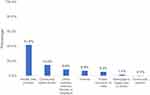 |
Figure 2 Sources of iron and folic acid supplementation information. |
In the logistic regression analysis (Table 2), maternal knowledge on benefits of taking IFAS was significantly associated with iron-folic acid consumption (OR=2.50, 1.04–5.97, P=0.04).
 |
Table 2 Multivariate Regression Analyses of IFAS Prevalence Status Among Pregnant Women |
Discussion
This study sought to assess the prevalence of IFAS among pregnant women and its associated factors. The main findings of the study were: (1) The majority of the women took IFAS during pregnancy; (2) less than half of the respondents had a high level of IFAS knowledge; (3) the main source of IFAS information was health care providers; (4) maternal knowledge on benefits of taking IFAS was the main factor significantly associated with prevalence of IFAS.
Notably, the prevalence rate of IFAS in this study (85.6%) was almost the same as the rate of the Philippines National Survey (82.4%) in 2008.39 Similar findings on the prevalence of IFAS have also been reported in neighboring countries, such as Cambodia42 and Nepal.43 This study found that pregnant women who were highly knowledgeable regarding the benefits of taking IFAS were more likely to continue taking IFAS than those who were slightly knowledgeable. These findings are consistent with reports on IFAS from similar rural settings in low and medium-income countries (LMIC), such as Indonesia,44 Ethiopia,23,45 and other countries (ie Afghanistan, Kenya, Nigeria, and Senegal).46 Thus, successful uptake of IFAS is linked to knowledge pertaining to the benefits of taking IFAS during pregnancy. Findings from this study show that such knowledge during pregnancy has a significant effect on the prevalence of IFAS. Knowledge about IFAS is a crucial channel for taking iron and folic acid during pregnancy. Therefore, the observed relationship between the level of knowledge concerning IFAS and the prevalence of IFAS is as expected. This finding is consistent with studies conducted in other areas of the Philippines and other countries.21,26,35,47–49
From this study, it was found that less than half of the women did not know that IFAS benefits include strengthening mothers during delivery and facilitates the fetus to grow healthy and strong. Few studies discussed the detailed content of the educational messages used to describe the benefits of taking IFAS. Most research conclude that women need to be motivated to take IFAS but focus on “benefit” messages such as “stronger” mothers, “healthier” babies, and reinforcing the belief that iron “increases the production of blood.”50 Further, this study showed that many pregnant women did not know about the side effects of taking IFAS. It has been reported that side effects and management of taking IFAS are important for improving prevalence of IFAS.23 Education about taking IFAS through antenatal care services is effective, but education focused on strengthening the benefit message as well as the side effects and its management are also expected. Moreover, these findings necessitate counseling on specific IFAS aspects concerning pregnant women and are supported by studies conducted in Ethiopia,51,52 Iran,53 and Pakistan.54
When aggregated by source, the majority of women in this study reported their source of information was the health care provider. This was followed by CHWs, friends/neighbors, the Internet, poster/television/radio, books, and finally community leaders. Health care providers could play a major role in advocating counseling for IFAS to increase knowledge about IFAS among pregnant women; about one-third of health care providers were CHWs. Interestingly, friends, the Internet, and television/radio was not the main source of information. Possible explanations for this finding may include that (a) CHWs are closer to the community resulting in better interpersonal communication and hence better explanations to women about IFAS;55 (b) information that passes through friends, the Internet, and television/radio is not usually prepared by professionals who know how to effectively reach the community with messages. In the Philippines, CHWs are known as Barangay Health Workers (BHW). Our previous publication reported that the BHWs play a potentially important role in supporting women during pregnancy and postpartum through home-visit services in the community56 Therefore, increasing refresher training on IFAS among CHWs to enhance their IFAS knowledge is important as they are a common source of IFAS information as in addition to health care providers.
It has been also reported that pregnant women’s husbands or family members contribute to the success of managing anemia in pregnancy.57 Therefore, it is important for health care providers to educate not only pregnant women but also their husbands and family members. There is a need to constantly provide pregnant women and their family members with information, education, and communication materials on IFAS, which they can always refer to and refresh their knowledge. Additionally, it might be necessary to provide a counseling program that improves the knowledge of not only pregnant women but also their husbands and families by utilizing CHWs.
Limitations
This study has some limitations. First, a few of the women in the first trimester might not have had taken IFAS yet because they had not received their first antenatal care session for receiving IFAS in BHS. Second, the small sample size limited the logistic regression analysis. Third, the study samples were selected from a hospital-based setting, and the level of knowledge could be different from a community-based setting. Fourth, the level of knowledge regarding IFAS among pregnant women was determined using a self-report survey, which is prone to bias and might affect the estimation of the actual level of knowledge of the target population. Finally, the types of factors considered to be associated with IFAS were limited.
Conclusion
Maternal knowledge about the benefits of taking IFAS was significantly associated with the prevalence of IFAS among pregnant women. The main source of IFAS information was health care providers and CHWs. Thus, there is a pressing need to improve health education on the benefits of IFAS among pregnant women to increase its prevalence. This underscores the knowledge level needed to support women through enhancing the involvement of health care providers and CHWs.
Acknowledgments
Our gratitude goes to all study participants in the hospital of Muntinlupa for their time and willingness to share their experiences. We thank the team of the Sentrong Aruga Para Sa Kababaihan for their support. We thank the Japan Society for the Promotion of Science KAKENHI for sponsoring this study.
Author Contributions
TY and HM were involved in the conception and design of the study, protocol development, data collection, data entry, interpretation of the data, and drafting the manuscript. REDR, MTRT, MWK, CY, YT, KS, and SI were involved in the design and review of protocol development, interpretation of the data, and review of the manuscript. All authors read and approved the final manuscript. All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Japan Society for the Promotion of Science KAKENHI, grant number 19K11277.
Disclosure
The authors declare no conflicts of interest.
References
1. World Health Organization. Nutritional anaemias: tools for effective prevention and control. 2017. Available from: https://www.who.int/publications/i/item/9789241513067.
2. Republic of the Philippines, Food, and Nutrition Research Institute. The 8th National Nutrition Survey. 2015. Available online: http://122.53.86.125/NNS/8thNNS.pdf.
3. Republic of the Philippines, Department of Health, National Nutrition Council. Philippines Plan of Action for Nutrition 2017–2022. 2017. Available online: http://www.nnc.gov.ph/downloads/technical-papers?download=870:philippine-plan.
4. Ali AA, Rayis DA, Abdallah TM, Elbashir MI, Adam I. Severe anaemia is associated with a higher risk for preeclampsia and poor perinatal outcomes in Kassala hospital, eastern Sudan. BMC Res Notes. 2011;4:311. doi:10.1186/1756-0500-4-311
5. Ayoya MA, Bendech MA, Zagre NM, Tchibindat F. Maternal anaemia in West and Central Africa: time for urgent action. Public Health Nutri. 2012;15:916–927. doi:10.1017/s1368980011002424
6. World Health Organization, Department of Making Pregnancy Safer and Department of Reproductive Health and Research. Standards for maternal and neonatal care Group 1: general standards of care for healthy pregnancy and childbirth. 2007. Available online: https://www.who.int/reproductivehealth/publications/maternal_perinatal_health/a91272/en/.
7. Kidanto HL, Mogren I, Lindmark G, Massawe S, Nystrom L. Risks for preterm delivery and low birth weight are independently increased by severity of maternal anaemia. South African Med J. 2009;99:98–102.
8. Rohilla M, Raveendran A, Dhaliwal LK, Chopra S. Severe anaemia in pregnancy: a tertiary hospital experience from northern India. J Obstet Gynaecol. 2010;30:694–696. doi:10.3109/01443615.2010.509821
9. Adam I, Elhassan EM, Haggaz AE, Ali AA, Adam GK. A perspective of the epidemiology of malaria and anaemia and their impact on maternal and perinatal outcomes in Sudan. J Infect Devel Countries. 2011;5:83–87. doi:10.3855/jidc.1282
10. Sengpiel V, Bacelis J, Myhre R, et al. Folic acid supplementation, dietary folate intake during pregnancy and risk for spontaneous preterm delivery: a prospective observational cohort study. BMC Pregnancy Childbirth. 2014;14(1):375. doi:10.1186/s12884-014-0375-1
11. Ogundipe O, Hoyo C, Ostbye T, et al. Factors associated with prenatal folic acid and iron supplementation among 21,889 pregnant women in Northern Tanzania: a cross-sectional hospital-based study. BMC Public Health. 2012;12(1):481. doi:10.1186/1471-2458-12-481
12. Daru J, Zamora J, Fernandez-Felix BM, et al. Risk of maternal mortality in women with severe anaemia during pregnancy and post partum: a multilevel analysis. Lancet Global Health. 2018;6(5):e548–e554. doi:10.1016/s2214-109x(18)30078-0
13. Wagner KS, Ronsmans C, Thomas SL, et al. Women who experience obstetric haemorrhage are at higher risk of anaemia, in both rich and poor countries. Trop Med Int Health. 2012;17(1):9–22. doi:10.1111/j.1365-3156.2011.02883.x
14. World Health Organization. Daily iron and folic acid supplementation in pregnant women. 2012. Available online: https://apps.who.int/iris/bitstream/handle/10665/77770/9789241501996_eng.pdf?sequence=1.
15. Maina-Gathigi L, Omolo J, Wanzala P, Lindan C, Makokha A. Utilization of folic acid and iron supplementation services by pregnant women attending an antenatal clinic at a regional referral hospital in Kenya. Matern Child Health J. 2013;17(7):1236–1242. doi:10.1007/s10995-012-1120-x
16. World Health Organization. Action - Nutrition International - Philippines - Maternal Nutrition Program - Iron and folic acid supplementation - Pregnant women. 2016. Available online: https://extranet.who.int/nutrition/gina/en/node/26253.
17. Leung BM, Kaplan BJ. Perinatal depression: prevalence, risks, and the nutrition link–a review of the literature. J Am Dietetic Assoc. 2009;109:1566–1575. doi:10.1016/j.jada.2009.06.368
18. Nilsen RM, Vollset SE, Gjessing HK, et al. Patterns and predictors of folic acid supplement use among pregnant women: the Norwegian Mother and Child Cohort Study. Am J Clin Nutr. 2006;84:1134–1141. doi:10.1093/ajcn/84.5.1134
19. Timmermans S, Jaddoe VW, Mackenbach JP, Hofman A, Steegers-Theunissen RP, Steegers EA. Determinants of folic acid use in early pregnancy in a multi-ethnic urban population in The Netherlands: the Generation R study. Prevent Med. 2008;47:427–432. doi:10.1016/j.ypmed.2008.06.014
20. Knudsen VK, Hansen HS, Ovesen L, Mikkelsen TB, Olsen SF. Iron supplement use among Danish pregnant women. Public Health Nutr. 2007;10:1104–1110. doi:10.1017/s136898000769956x
21. Lutsey PL, Dawe D, Villate E, Valencia S, Lopez O. Iron supplementation compliance among pregnant women in Bicol, Philippines. Public Health Nutr. 2008;11:76–82. doi:10.1017/S1368980007000237
22. Seck BC, Jackson RT. Determinants of compliance with iron supplementation among pregnant women in Senegal. Public Health Nutr. 2008;11:596–605. doi:10.1017/s1368980007000924
23. Gebremedhin S, Samuel A, Mamo G, Moges T, Assefa T. Coverage, compliance and factors associated with utilization of iron supplementation during pregnancy in eight rural districts of Ethiopia: a cross-sectional study. BMC Public Health. 2014;14:607. doi:10.1186/1471-2458-14-607
24. Kassa ZY, Awraris T, Daba AK, Tenaw Z. Compliance with iron folic acid and associated factors among pregnant women through pill count in Hawassa city, South Ethiopia: a community based cross-sectional study. Reprod Health. 2019;16:14. doi:10.1186/s12978-019-0679-8
25. Gebremariam AD, Tiruneh SA, Abate BA, Engidaw MT, Asnakew DT. Adherence to iron with folic acid supplementation and its associated factors among pregnant women attending antenatal care follow up at Debre Tabor General Hospital, Ethiopia, 2017. PLoS One. 2019;14:e0210086. doi:10.1371/journal.pone.0210086
26. Kamau MW, Mirie W, Kimani S. Compliance with iron and folic acid supplementation (IFAS) and associated factors among pregnant women: results from a cross-sectional study in Kiambu County, Kenya. BMC Public Health. 2018;18:580. doi:10.1186/s12889-018-5437-2
27. Johnston EO, Sharma AJ, Abe K. Association between maternal multivitamin use and preterm birth in 24 states, pregnancy risk assessment monitoring system, 2009–2010. Matern Child Health J. 2016;20:1825–1834. doi:10.1007/s10995-016-1985-1
28. Barbosa L, Ribeiro Dde Q, de Faria FC, Nobre LN, Lessa Ado C. Factors associated with folic acid use during pregnancy. Revista Brasileira De Dinecologia e Obstetricia. 2011;33:246–251.
29. Miranda VIA. The use of folic acid, iron salts and other vitamins by pregnant women in the 2015 Pelotas birth cohort: is there socioeconomic inequality? BMC Public Health. 2019;19:889. doi:10.1186/s12889-019-7269-0
30. Nisar YB, Dibley MJ, Mir AM. Factors associated with non-use of antenatal iron and folic acid supplements among Pakistani women: a cross sectional household survey. BMC Pregnancy Childbirth. 2014;14:305. doi:10.1186/1471-2393-14-305
31. Lunet N, Rodrigues T, Correia S, Barros H. Adequacy of prenatal care as a major determinant of folic acid, iron, and vitamin intake during pregnancy. Cad Saude Publica. 2008;24:1151–1157. doi:10.1590/s0102-311x2008000500022
32. Yu SM, Keppel KG, Singh GK, Kessel W. Preconceptional and prenatal multivitamin-mineral supplement use in the 1988 National Maternal and Infant Health Survey. Am J Public Health. 1996;86:240–242. doi:10.2105/ajph.86.2.240
33. Jasti S, Siega-Riz AM, Cogswell ME, Hartzema AG, Bentley ME. Pill count adherence to prenatal multivitamin/mineral supplement use among low-income women. J Nutri. 2005;135:1093–1101. doi:10.1093/jn/135.5.1093
34. Risonar MG, Rayco-Solon P, Tengco LW, Sarol JN, Paulino LS, Solon FS. Effectiveness of a redesigned iron supplementation delivery system for pregnant women in Negros Occidental, Philippines. Public Health Nutr. 2009;12:932–940. doi:10.1017/s1368980008003418
35. Paulino LS, Angeles-Agdeppa I, Etorma UM, Ramos AC, Cavalli-Sforza T. Weekly iron-folic acid supplementation to improve iron status and prevent pregnancy anemia in Filipino women of reproductive age: the Philippine experience through government and private partnership. Nutr Rev. 2005;63:S109. doi:10.1301/nr.2005.dec.s109-s115
36. Department of Health, Republic of the Philippine. Micronutrient Program. 2010. Available online: https://www.doh.gov.ph/micronutrient-program. (
37. The Department of Health, Center for Health Development, Cordillera Administrative region. Iron Deficiency Anemia. 2014. Available online: http://caro.doh.gov.ph/wp-content/uploads/2014/09/IDA.pdf.
38. Kavle JA, Landry M. Community-based distribution of iron-folic acid supplementation in low- and middle-income countries: a review of evidence and programme implications. Public Health Nutr. 2018;21(2):346–354. doi:10.1017/S1368980017002828
39. United States Agency for International Development. A Rapid Initial Assessment of the Distribution and Consumption of Iron-Folic Acid Tablets through Antenatal Care in the Philippines. 2014. Available online: https://www.spring-nutrition.org/publications/briefs/iron-folic-acid-assessment-philippines. (
40. United States Agency for International Development. Spring Nutrition Technical Brief: A Simple Method for Making a Rapid, Initial Assessment of the Consumption and Distribution of Iron-Folic Acid Supplements Among Pregnant Women in Developing Countries. Spring Nutr Tech Brief Series; 2014.
41. Philippines Statistics Authority. Proportion of Poor Filipinos registered at 21.0 percent in the First Semester of 2018. 2019. Available online: https://psa.gov.ph/content/proportion-poor-filipinos-registered-210-percent-first-semester-2018.
42. Lacerte P, Pradipasen M, Temcharoen P, Imamee N, Vorapongsathorn T. Determinants of adherence to iron/folate supplementation during pregnancy in two provinces in Cambodia. Asia-Pacific J Public Health. 2011;23:315–323. doi:10.1177/1010539511403133
43. Rai SS, Ratanasiri T, Arkaravichien T, Thapa P, Koju R. Compliance and its determinants regarding iron and folic acid supplementation during pregnancy in Kathmandu, Nepal. Kathmandu Univ Med J. 2016;14:311–317.
44. Titaley CR, Dibley MJ. Factors associated with not using antenatal iron/folic acid supplements in Indonesia: the 2002/2003 and 2007 Indonesia Demographic and Health Survey. Asia Pacific Clin Nutr. 2015;24:162–176. doi:10.6133/apjcn.2015.24.1.10
45. Arega Sadore A, Abebe Gebretsadik L, Aman Hussen M. Compliance with iron-folate supplements and associated factors among antenatal care attendant mothers in Misha District, South Ethiopia: community based cross-sectional study. J Environ Public Health. 2015;781973. doi:10.1155/2015/781973
46. Siekmans K, Roche M, Kung’u JK, Desrochers RE, De-Regil LM. Barriers and enablers for iron folic acid (IFA) supplementation in pregnant women. Matern Child Nutr. 2018;14(Suppl 5):e12532. doi:10.1111/mcn.12532
47. Mithra P, Unnikrishnan B, Rekha T, et al. Compliance with iron-folic acid (IFA) therapy among pregnant women in an urban area of south India. Afr Health Sci. 2014;14:255–260. doi:10.4314/ahs.v14i1.39
48. Nasir BB, Fentie AM, Adisu MK. Adherence to iron and folic acid supplementation and prevalence of anemia among pregnant women attending antenatal care clinic at Tikur Anbessa Specialized Hospital, Ethiopia. PLoS One. 2020;15:e0232625. doi:10.1371/journal.pone.0232625
49. Gebremichael TG, Welesamuel TG. Adherence to iron-folic acid supplement and associated factors among antenatal care attending pregnant mothers in governmental health institutions of Adwa town, Tigray, Ethiopia: cross-sectional study. PLoS One. 2020;15:e0227090. doi:10.1371/journal.pone.0227090
50. Moore M, Riono P, Pariani S. A Qualitative Investigation of Factors Influencing Use of Iron Folate Tablets by Pregnant Women in West Java: A Summary of Findings. Arlington, VA: MotherCare Project, Jphn Snow, Inc; 1991.
51. Desta M, Kassie B, Chanie H, et al. Adherence of iron and folic acid supplementation and determinants among pregnant women in Ethiopia: a systematic review and meta-analysis. Reprod Health. 2019;16:182. doi:10.1186/s12978-019-0848-9
52. Molla T, Guadu T, Muhammad EA, Hunegnaw MT. Factors associated with adherence to iron folate supplementation among pregnant women in West Dembia district, northwest Ethiopia: a cross sectional study. BMC Res Notes. 2019;12:6. doi:10.1186/s13104-019-4045-2
53. Siabani S, Siabani S, Siabani H, Moeini Arya M, Rezaei F, Babakhani M. Determinants of compliance with iron and folate supplementation among pregnant women in West Iran: a population based cross-sectional study. J Family Reprod Health. 2018;12:197–203.
54. Nisar YB, Alam A, Aurangzeb B, Dibley MJ. Perceptions of antenatal iron-folic acid supplements in urban and rural Pakistan: a qualitative study. BMC Pregnancy Childbirth. 2014;14:344. doi:10.1186/1471-2393-14-344
55. Carmichael SL, Mehta K, Raheel H, et al. Effects of team-based goals and non-monetary incentives on front-line health worker performance and maternal health behaviours: a cluster randomised controlled trial in Bihar, India. BMJ Glob Health. 2019;26(4):e001146. doi:10.1136/bmjgh-2018-001146
56. Yamashita T, Suplido SA, Llave C, Tuliao MT. Tanaka Y Matsuo H. Understanding postpartum healthcare services and exploring the challenges and motivations of maternal health service providers in the Philippines: a qualitative study. Trop Med Health. 2015;43(2):123–130.
57. Widyawati W, Jans S, Utomo S, van Dillen J, Janssen ALML. A qualitative study on barriers in the prevention of anaemia during pregnancy in public health centres: perceptions of Indonesian nurse-midwives. BMC Pregnancy Childbirth. 2015;15:47. doi:10.1186/s12884-015-0478-3
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
