Back to Journals » International Journal of Women's Health » Volume 6
Maternal and perinatal outcomes of delivery after a previous Cesarean section in Enugu, Southeast Nigeria: a prospective observational study
Authors Ugwu G, Iyoke CA , Onah H, Egwuatu V, Ezugwu F
Received 17 October 2013
Accepted for publication 14 January 2014
Published 13 March 2014 Volume 2014:6 Pages 301—305
DOI https://doi.org/10.2147/IJWH.S56147
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
George O Ugwu,1 Chukwuemeka A Iyoke,1 Hyacinth E Onah,1 Vincent E Egwuatu,2 Frank O Ezugwu2
1Department of Obstetrics and Gynaecology, University of Nigeria Teaching Hospital (UNTH), Ituku-Ozalla, Enugu, Nigeria; 2Department of Obstetrics and Gynaecology, Enugu State University Teaching Hospital (ESUTH), Parklane, Enugu, Nigeria
Background: Obstetricians in developing countries appear generally reluctant to conduct vaginal delivery in women with a previous Cesarean because of lack of adequate facilities for optimal fetomaternal monitoring.
Objective: To describe delivery outcomes among women with one previous Cesarean section at a tertiary hospital in Southeast Nigeria.
Methods: This was a prospective observational study to determine maternal and perinatal outcomes of attempted vaginal birth after Cesarean sections (VBAC) following one previous Cesarean section. Analysis was done with SPSS statistical software version 17.0 for Windows using descriptive and inferential statistics at 95% level of confidence.
Results: Two thousand six hundred and ten women delivered in the center during the study period, of whom 395 had one previous Cesarean section. A total of 370 women with one previous Cesarean section had nonrecurrent indications, of whom 355 consenting pregnant women with one previous Cesarean section were studied. A majority of the women (320/355, 90.1%) preferred to have vaginal delivery despite the one previous Cesarean section. However, only approximately 54% (190/355) were found suitable for trial of VBAC, out of whom 50% (95/190 had successful VBAC. Ninety-five women (50.0%) had failed attempt at VBAC and were delivered by emergency Cesarean section while 35 women (9.8%) had emergency Cesarean section for other obstetric indications (apart from failed VBAC). There was no case of uterine rupture or neonatal and maternal deaths recorded in any group. Apgar scores of less than 7 in the first minute were significantly more frequent amongst women who had vaginal delivery when compared to those who had elective repeat Cesarean section (P=0.03).
Conclusion: Most women who had one previous Cesarean delivery chose to undergo trial of VBAC, although only about half were considered suitable for VBAC. The maternal and fetal outcomes of trial of VBAC in selected women with one previous Cesarean delivery for nonrecurrent indications were good. Obstetricians in this area should do more to allow VBAC in women with one previous Cesarean section for nonrecurrent indications.
Keywords: previous Cesarean section, vaginal birth, pregnancy, VBAC
Introduction
As a result of improvements in obstetric care. it is now relatively safe for an attempt at vaginal birth after Cesarean section (VBAC). VBAC is thus being recommended as a relatively safe way of decreasing the ever rising rate of Cesarean delivery globally.1,2 Vaginal delivery is associated with fewer risks, requires less anesthesia, poses a lower potential for postpartum morbidity, involves a shorter hospital stay, is more affordable, and encourages earlier and better bonding between mother and infant.3 These advantages are significant, especially in our resource poor setting where sociocultural aversion to Cesarean delivery is common.4
Successful vaginal birth has been reported in 60%–80% of cases reported in published studies of women attempting vaginal birth after a previous Cesarean section.5–9 The recommended criteria10–12 for selecting candidates suitable for VBAC are potentially applicable in tertiary centers in developing countries, but there are many inadequacies in meeting them in our environment.13 Such inadequacies may include the unavailability of anesthesiologists and neonatologists on demand during labor/delivery, lack of adequate blood transfusion services, and at times a lack of other basic facilities and the personnel needed to carry out a timely Cesarean section. Perhaps because of this, anecdotal evidence shows that the attitude of many obstetricians towards practice of VBAC appears guarded.
Meanwhile, a Cesarean section rate of over 25% has been reported in our study center.14,15 There is a growing concern over the rising rate of Cesarean section in developing countries; Cesarean section rates have been significantly linked to the practice of VBAC.13,15 In Nigeria many women are poor and may not easily afford Cesarean delivery. Many also dislike Cesarean section for sociocultural reasons. Increased application of VBAC where appropriate should therefore be actively encouraged in our area. However, previous studies show that the problem associated with attempting VBAC in Nigeria includes a lack of facilities for continuous fetal monitoring and inadequate manpower and facilities for emergency Cesarean section, which result in long decision–operation intervals.9,13–17,19 The aim of this study was to describe the maternal and perinatal outcomes of delivery in women with one prior Cesarean section seen at a tertiary hospital in Enugu, South East Nigeria.
Methods
Study center
The study was carried out in the obstetric unit of the University of Nigeria Teaching Hospital (UNTH), Ituku-Ozalla, Enugu, Southeast Nigeria, a referral center for high-risk obstetric cases in the south eastern part of the country and beyond. The hospital provides both general and specialist services to the people of Enugu state and its environs. It conducts about 1,500 deliveries annually, with a reported Cesarean section rate of 25%.
Study period
The study took place between May 1, 2010 and April 30, 2012.
Study design
This was a prospective study involving consecutive eligible women with one previous Cesarean section at the University of Nigeria Teaching Hospital, Ituku Ozalla, Enugu, Southeast Nigeria.
Sampling
The sampling technique was purposeful and patients were enrolled consecutively. There was individual counseling of each woman recruited for the study, after which her written consent was obtained. The women were not paid to participate in the study. Women who had one previous Cesarean section and were in the second or third trimester of pregnancy were recruited in the study. Each study participant was given a number (or tag) to enable specific follow-up. Women who had two or more Cesarean sections or a uterine scar (myomectomy or uterine rupture) were excluded. Women who had Cesarean sections for a reason that would typically lead to another Cesarean delivery in subsequent pregnancies (recurrent indications) were also excluded. Such recurrent indications included women with radiological evidence of pelvic contraction, previous classical Cesarean section, and previous repair of vaginal fistula. Selection of candidates for VBAC by the obstetrician was based on the 2004 American College of Obstetricians and Gynecologists’ (ACOG) recommendation10 which specified that such a candidate should have no more than one prior lower segment Cesarean delivery, clinically adequate pelvis, no other uterine scars or previous rupture, and the availability of obstetricians and anesthetists and other requisite personnel to monitor the active labor and carry out a timely Cesarean delivery.
Data collection
Data collection was achieved using a proforma. Data obtained included bio data, sociodemographic characteristics, details of the previous Cesarean section, mode of delivery, outcome, and possible complications of each delivery. All women included in the study were followed through delivery and for at least 48 hours after delivery. Information was sought directly from the women and recorded in a proforma. The main outcome measure was the delivery outcome in the index pregnancy. Secondary outcome measures included perinatal complications and maternal complications as well. Each labor was monitored closely using a partogram and regular auscultation of the fetal heart at least once every 30 minutes. For the single case of induction of labor, cervical ripening was done by intra cervical catheter and the entire process of induction was physically monitored by a senior obstetrician. Syntocinon was used for the labor induction and also for the few patients who had augmentation.
All data collected were keyed into Statistical Package for Social Science (IBM Corporation, Armonk, NY, USA) computer software version 17.0 for analysis. Maternal and perinatal outcomes were compared between women who had VBAC, those who had elective repeat Cesarean delivery, those who had successful VBAC, and those who had failed VBAC. Categorical variables were compared using the chi-square test (or Fisher’s exact test where appropriate). P-values less than or equal to 0.05 were considered significant.
The study was approved by the Research Ethics Committee of the hospital.
Results
Two thousand six hundred and ten women delivered in the center during the study period, out of which 395 had one previous Cesarean section. The prevalence of women with one previous Cesarean section in this study was therefore 15.1%. Twenty five women with one previous Cesarean declined consent to participate in the study. Of 370 women who consented to participate in the study, only 355 women presented for delivery in the study center and their data were used for analysis.
The sociodemographic characteristics of the study population indicate that the average age of the women was 32.1±4.7 years (range: 23–44 years). Most of the patients were married (98.6%), Christian (95.8%), and of Igbo ethnicity (98.6%). Sixty-nine percent of the patients studied had tertiary education. Details of the sociodemographic characteristics are shown in Table 1.
The leading indications for the one previous Cesarean were prolonged labor in 90 women (25.4%), pre-eclampsia in 55 (15.5%), and 35 each of failed induction and abnormal lie (9.9%).
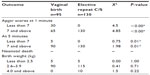
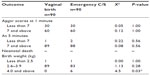
Table 2 summarizes the comparison of maternal and fetal outcomes between women who had VBAC and those who had elective repeat Cesarean section. The majority of the women (320, 90.1%) preferred to have vaginal delivery despite the one previous Cesarean section. As regards the planned mode of delivery determined by the obstetrician, 190 (53.5%) of the women were assessed as suitable to allow an attempt at vaginal birth; of these 190 women 95 (50.0%) eventually had successful vaginal birth, while the remaining 95 (50.0%) failed to deliver successfully via VBAC and delivered by emergency Cesarean section. Of the remaining 165 (46.5%) women, 130 (35.7%) had elective repeat Cesarean section while thirty-five (9.8%) women had emergency Cesarean section for other obstetric indications (apart from failed VBAC). There was no case of uterine rupture, neonatal, or maternal deaths recorded in any group.
Table 3 summarizes the comparison of maternal and perinatal outcomes between women who had successful trial of VBAC and those who had failed attempt at VBAC. Apgar scores of less than seven in the first minute were significantly more frequent amongst those with vaginal delivery when compared to those with elective repeat Cesarean section (P=0.00). Apgar scores less than seven in the first minute were more frequent in those with failed VBAC than vaginal delivery (successful VBAC); however, the difference was not statistically significant (P=0.082) (Table 3). Among those allowed trial of labor, 30 (31.6%) failed VBAC had birth weight 4.0 kg or greater compared to none (0%) of those with successful VBAC (P=0.03).
Discussion
The prevalence of one previous Cesarean section of 15.1% in this study is higher but still comparable to the 11.9% documented in a private hospital in Lagos, Nigeria.7 This marginally higher prevalence may be due to the fact that high risk cases including previous Cesarean section are referred to and managed in our teaching hospital. The clear preference for vaginal delivery (90.1%) among the women was expected due to strong cultural aversion for Cesarean delivery, which even formal education does not seem to alter.4
Only about half (53.3%) of the women with one previous Cesarean section were allowed to attempt VBAC despite a high Cesarean section rate in the hospital and overwhelming preference for vaginal delivery by the women. This percentage is high compared to the less than 10% recorded in Enugu in 1989.13 Our results are similar to the reports from Benin, Nigeria17 but much lower than the 70.7% in a recent similar study in Lagos.7
The lower proportion of women allowed to attempt a VBAC in this study may be due to a combination of reasons. The medical, legal, and ethical concerns related to the responsibility of monitoring a high risk labor after a previous Cesarean section without the appropriate tools and facilities may be a factor. Necessary conditions including personnel – especially anesthetists and neonatologists – and the facilities needed for emergency Cesarean section (eg, blood for transfusion) are often not available on demand. The absence of adequate facilities for electronic fetal monitoring in the study center makes fetal monitoring in labor less intensive. Another factor may be the relocation of the hospital to its permanent site about 21 kilometers from the city where senior obstetricians are resided. This may have lowered the threshold for elective Cesarean section as a precautionary measure.
Out of those allowed to attempt VBAC, only half achieved successful vaginal birth. This finding is higher than the 34% success rate recorded in Pakistan18 and Benin, Nigeria,17 but much lower than the more recent studies from Ibadan and Lagos that had successful vaginal deliveries in the range of 60%–80%.7,19 These higher success rates are similar to a previous report from Enugu.9 It must be noted that these local studies with higher success rates had increased fetal and maternal complications compared to our finding. The lower success rate of VBAC in this work may be due to early and abrupt recourse to emergency Cesarean section occasioned by medical or legal concerns and conceivable complications in the face of suboptimal facilities for intrapartum care. Only one woman in our series had induction of labor and three had cautious augmentation of labor, all with good outcome. It may be that more liberal application of induction and augmentation of labor when indicated may have increased the rate of successful VBAC in our hospital. A study to determine the safety and impact of liberal use of induction and augmentation of labor in women with one previous Cesarean in this area is needed.
Good fetal and maternal outcomes of labor were recorded among women who had trial of VBAC in this study with no case of uterine rupture or perinatal and maternal deaths. Previous retrospective reviews from Nigeria had recorded one to five cases of uterine rupture and one to three cases of neonatal death with no maternal death but with higher rates of successful VBAC.7,9 In those reviews, a greater proportion of women with one previous Cesarean were allowed trial of VBAC than in this study, and this may explain the inability of this study to detect these complications.
The strengths of this work include its prospective design which enabled verification of data directly from the women. The main weakness was that the study involved only one center (due to logistic reasons); it may have been better to have more participating institutions to get a wider picture in the zone and country.
Conclusion
In conclusion, it remains a challenge to strike a balance between concern for safety and the need to decrease Cesarean section rates. Due to limited facilities for fetal monitoring, most obstetricians tended to have a low threshold for elective repeat Cesarean section; hence, only about half of women with a previous Cesarean were allowed attempt at VBAC. This is a sharp contrast to the less restrictive guidelines by both the Royal College of Obstetricians and Gynaecologists and the ACOG.20,21 In the recently revised document ACOG recommended that trial of labor after previous Cesarean delivery (TOLAC) is safe and appropriate for most women with previous Cesarean delivery, including those with two previous lower segment transverse incisions, twin pregnancy, and those with unknown type of scar. Together with a recent meta-analysis22 that reported over 70% successful vaginal births after two Cesareans, all these recommendations may not influence practice in our environment in the near future unless there is improvement in our intrapartum care in terms of personnel, facilities, and our capacity to carry out a timely Cesarean section.
Disclosure
The authors report no conflicts of interest in this work.
References
Miller DA, Diaz FG, Paul RH. Vaginal birth after cesarean: a 10-year experience. Obstet Gynecol. 1994;84(2):255–258. | |
Flamm BL, Newman LA, Thomas SJ, Fallon D, Yoshida MM. Vaginal birth after cesarean delivery: results of a 5-year multicenter collaborative study. Obstet Gynecol. 1990;76(5 Pt 1):750–754. | |
Ainbinder SW. Operative Delivery. In: De Cherny AH, Nathan L, editors. Current Obstetrics and Gynecologic Diagnosis and Treatment. 9th ed. New York: McGraw-Hill Publishing Co; 2003:499–530. | |
Onah HE. Formal Education does not improve the acceptance of caesarean section among pregnant Nigerian Women. Int Gynecol Obstet, 2002;76(3):321–323. | |
Hibbard JU, Ismail MA, Wang Y, Te C, Karrison T, Ismail MA. Failed vaginal birth after a cesarean section: how risky is it? I. Maternal morbidity. Am J Obstect Gynecol. 2001;184(7):1365–1371. | |
Omigbodun AO. Vaginal birth after caesarean section. In: Kwawukume EY, Emuveyan EE, editors. Comprehensive Obstetrics in the Topics Ghana. Accra: Asante and Hittscher Printing Press Ltd; 2002:122–128. | |
Ezechi OC, Kalu EE, Njokanma FO, Ndububa CA, Nwokoro CA, Okeke GCE. Trial of labour after previous caesarean delivery: a private hospital experience. Annals of African Medicine. 2005;4(3):113–117. | |
Weinstein D, Benshushan A, Tanos V, Zilberstein R, Rojansky N. Predictive score for vaginal birth after caesarean section. Am J Obstet Gynecol. 1996;174(1 Pt 1):192–198. | |
Egwuatu VE, Ezeh IO. Vaginal delivery in Nigerian women after a previous cesarean section. Int J Gynecol Obset. 1990;32(1):1–6. | |
American College of Obstetricians and Gynecologists (ACOG). ACOG Practice bulletin no. 115: Vaginal birth after previous cesarean delivery. Obstet Gynecol. 2010;116(2 Pt 1):450–463. | |
Royal College of Obstetricians and Gynecologists of Canada (SOGC) N Predictive score for vaginal birth after caesarean section. Am J Obstect Gynecol. 1996;174(1 Pt 1):192–198. | |
Society of Obstetricians and Gynaecologists of Canada. SOGC clinical practice guidelines. Guidelines for vaginal birth after previous caesarean birth. Number 155 (Replaces guideline Number 147), February 2005. Int J Gynaecol Obstet. 2005;89(3):319–331. | |
Ikechebelu JI, Mbamara SU, Afuba AN. Vaginal birth after one caesarean section: A review of the practice at Nnewi, Southeast Nigeria. J Med Med Sci. 2010;1(7):309–313. | |
Ugwu EO, Obioha KC, Okezie OA, Ugwu AO. A five-year survey of caesarean delivery at a Nigerian tertiary hospital. Ann Med Health Sci Res. 2011;1(1):77–83. | |
Nkwo PO, Onah HE. Feasibility of reducing the caesarean section rate at the University of Nigeria Teaching Hospital, Enugu Nigeria Teaching Hospital, Enugu Nigeria. Trop J Obstet Gynecol. 2002; 19(2):86–89. | |
Resnik R. Can a 29% Cesarean delivery rate possibly be justified? Obstet Gynecol. 2006;107(4):752–754. | |
Okpere EE, Orosanye AV, Imoedmher DAG. Pregnancy and Delivery after caesarean section: a review of 494 cases. Trop J Obstet Gynecol. 1981;3:45–48. | |
Nisa M, Hassan L. Trend of vaginal delivery after one previous caesarean section in a tertiary care hospital. Pakistan J Med Res. 2004;43(2). | |
Ilesanmi AO, Odukogbe A, Olaleye DO. Vaginal delivery after one caesarean section in Nigeria women. J Obstet and Gynaecol. 1997;17(2):139–142. | |
Royal College of Obstetricians & Gynaecologists. Birth After Previous Caesarean Section. Green-top Guideline No. 45. 2007. Available from: http://www.rcog.org.uk/files/rcog-corp/GTG4511022011.pdf. Accessed August 13, 2013. | |
American College of Obstetricians and Gynecologists (ACOG) bulletin no 115. Obstet Gynecol. 2010;116(2):450–463. | |
Tahseen S, Griffiths M. Vaginal birth after two caesarean section (VBAC 2) – a systematic review with meta-analysis of success rate and adverse outcome of VBAC -2 Versus VBAC -1 and repeat (third) caesarean sections. BJOG. 2010;117(1):5–19. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.