Back to Journals » OncoTargets and Therapy » Volume 12
MAP3K1 rs889312 genotypes influence survival outcomes of Chinese gastric cancer patients who received adjuvant chemotherapy based on platinum and fluorouracil regimes
Authors Yang J, Zheng W, Xu Z, Chen J
Received 15 February 2019
Accepted for publication 30 July 2019
Published 22 August 2019 Volume 2019:12 Pages 6843—6855
DOI https://doi.org/10.2147/OTT.S205438
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sanjeev K. Srivastava
Jian Yang,1,2,* Wei Zheng,3,* Zhi Xu,1,4 Jinfei Chen1,5,6
1Department of Oncology, Nanjing First Hospital, Nanjing Medical University, Nanjing 210006, People’s Republic of China; 2Department of Oncology, The Affiliated Yixing Hospital of Jiangsu University, Yixing 214200, People’s Republic of China; 3Department of General Surgery, The Affiliated Yixing Hospital of Jiangsu University, Yixing 214200, People’s Republic of China; 4ICR Medical Affairs, ICON Plc, Shanghai 200003, People’s Republic of China; 5Cancer Center, TaiKang Xianlin Drum Tower Hospital, Nanjing University School of Medicine, Nanjing 210046, People’s Republic of China; 6Collaborative Innovation Center for Cancer Personalized Medicine, Nanjing Medical University, Nanjing 210006, People’s Republic of China
Correspondence: Jinfei Chen
Department of Oncology, Nanjing First Hospital, Nanjing Medical University, 68 Changle Road, Nanjing 210006, People’s Republic of China
Tel +86 258 535 8120
Fax +86 258 535 8120
Email [email protected]
*These authors contributed equally to this work
Background: For patients with gastric cancer (GC), adjuvant chemotherapy is a standard therapy. However, the responses to the treatment are quite different. Mitogen-activated protein kinase (MAPK) pathway is a core pathway that modulates the efficacy of anticancer drugs. The purpose of our study was to investigate the clinical significance of one pivotal functional gene polymorphism in the MAPK pathway – MAP3K1 rs889312 – in patients with stage II GC to stage III GC.
Methods: The genotypes of MAP3K1 rs889312 were analyzed in 591 GC patients enrolled in this study who had received radical gastrectomy. Among them, 204 patients accepted adjuvant chemotherapy based on platinum and fluorouracil (PF) regimens after an operation. Cox regression analysis, log-rank test and Kaplan–Meier method were used to explore the link between MAP3K1 rs889312 variant and overall survival (OS) of GC.
Results: Compared with the AA genotype (mean OS of 68.12 months), MAP3K1 rs889312 AC/CC significantly reduced the mean OS of 56.83 months in patients who received adjuvant chemotherapy only. In addition, AC/CC genotype had a negative impact on OS of patients who received oxaliplatin-based therapy (HR, 8.253; 95% CI: 1.119–60.853, log-rank p=0.013). Stratification analysis showed that MAP3K1 rs889312 AC/CC significantly reduced OS of patients with tumors smaller than or equal to 5 cm in size (HR, 3.706; 95% CI: 1.329–10.335, p=0.012), poorly differentiated tumors (HR, 3.002; 95% CI: 1.076–8.377, p=0.036) and intestinal tumors (HR, 4.780; 95% CI: 1.138–20.073, p=0.033).
Conclusion: Our findings suggested that MAP3K1 rs889312 single-nucleotide polymorphism may be considered as a biomarker for adjuvant chemotherapy reaction and can predict prognosis of GC patients who received PF-based therapy.
Keywords: MAP3K1 rs889312, gastric cancer, biomarker, single-nucleotide polymorphism, adjuvant chemotherapy
Introduction
Although the mortality rate of cancer patients has declined over the past decade, gastric cancer (GC) remains a devastating disease, especially in Asia.1 It is estimated that 679,100 new GC cases and 498,000 deaths occurred in 2015 in China.2 Currently, combination therapies including surgery, chemotherapy and local radiotherapy are options for most patients with locally advanced GC, whilst surgery remains the only curative therapy. Postoperative chemotherapy and chemoradiation could bring further benefits, with a 5-year survival rate increased by 8–15%.3–5 So far, adjuvant chemotherapy based on platinum and fluorouracil (PF) has been considered to be the most effective treatment for stage II and stage III GC after an operation. The response rate is less than 50%, though.6 There is no clear evidence – including conventional clinicopathological parameters and molecular classification – that can possibly distinguish patients who are likely to benefit from PF regimen. Therefore, the identification of new biomarkers is of great importance for guiding personalized treatment and avoiding unnecessary toxicity and economic burden.
Nowadays, accumulative evidence has demonstrated the pivotal genetic effects of single-nucleotide polymorphisms (SNPs) on GC development and progression. Investigating SNPs in a biological pathway – rather than individual genes – may provide a better chance to identify the genes and mechanisms underlying disease pathogenesis.7 In our previous research, functional SNPs in cancer initiation and progression pathways were selected systematically through literature review and pooled analysis results. Finally, the associations between more than 20 SNPs and survival of GC were checked in a Chinese population.8–15 Based on the concept that variation in genes involved in pathways such as the repair of DNA damage may be important in both the mechanisms of tumor formation and proliferation and in the response to DNA damage induced by chemotherapy, we hypothesized that genetic determinants of GC outcome might be associated with chemotherapy reaction.16,17 The polymorphisms of one-carbon metabolism pathway-associated genes were also suggested as predictive factors for the GC patients’ treatment with 5-FU-based chemotherapy in our previous study.18,19
All cell types express the mitogen-activated protein kinases (MAPKs). They regulate various physiological processes such as cell growth, differentiation, metabolism, death, etc.20 Thus far, four independent MAPK pathways have been characterized, including ERK, c-Jun N-terminal kinase (JNK), p38 signaling and Big MAP kinase-1 families whose relevancies with response and resistance to antitumor agents have been recognized.21–23 For example, activated MAPK/ERK pathway has a survival advantage for squamous tumor cells treated with cisplatin.24 P38α MAPK has been identified as a mediator of resistance to 5-fluorouracil and cisplatin chemotherapy in colorectal cancer patients.25
Mitogen-activated protein kinase kinase kinase 1 (MAP3K1) is a serine/threonine kinase. As it localizes upstream of all three of the ERK, JUK and p38 signaling pathways, MAP3K1 may play a pivotal role in the network of phosphorylating enzymes. Large case–control and case–case studies have shown that SNPs in MAP3K1 can have an influence on both the molecular biology of the tumor and the prognosis of the patients. It was noted that MAP3K1 rs889312 polymorphism was associated with increased risk of distant metastasis development in breast cancer.26 Patients with lymph node metastasis had a lower mutation frequency of MAP3K1 rs702689 (GA/AA) than patients without lymph node metastasis in colorectal cancer.27 Distant or lymph node metastasis may reduce the survival rate and worsen the prognosis of cancer. More direct evidences showing the correlation between MAP3K1 rs889312 and prognosis of tumors were identified. For instance, among premenopausal women with breast cancer, MAP3K1 rs889312 (CC) was significantly associated with poor distant disease-free survival (DDFS), disease-free survival (DFS) or overall survival (OS).28 And the SNP rs889312 in MAP3K1 showed a significant improvement in DDFS for heterozygotes of this SNP and appears to demonstrate a dominant effect in early-onset breast cancer patients.29
In our previous study, we revealed that MAP3K1 rs889312 AC variant genotype was associated with a statistically significant 30% decrease in survival of GC patients compared to the AA/CC homozygotes.30 Based on the previous research, we hypothesized that MAP3K1 polymorphism may be associated with outcomes of adjuvant chemotherapy in GC based on PF. Here, we explored the clinical significance of the functional MAP3K1 rs889312 polymorphism in Chinese patients who received PF-based adjuvant chemotherapy after GC surgery and compared them with those who did not receive adjuvant chemotherapy. We also investigated the prognostic associations of MAP3K1 rs889312 polymorphism in certain subtypes of GC.
Materials and methods
Ethics statement
All patients gave their written informed consents. The study has been approved by the Institutional Ethical Review Board of Nanjing Medical University, Nanjing, China.
Study patients
Totally 591 GC patients retrospectively analyzed in this study received their operations between 1999 and 2006 in Yixing People’s Hospital (Yixing, Jiangsu Province). They had been confirmed as stage II–III diseases by histopathological diagnosis. Survival time of GC patients ranged from operation date to death or the last follow-up in March 2009. The median follow-up time was 68.5 months. All patients had not received radiochemotherapy or radiotherapy before or after surgery. Two hundred and seven of the patients underwent PF-based adjuvant chemotherapy within 1 month after the operation. The patients’ clinical features including sex, age, alcohol consumption, smoking, tumor site and size, invasion, lymph node metastasis, histological type and differentiation were collected and summarized in Table 1. People who had smoked daily for over 1 year were considered smokers. And all patients who had consumed one or more glasses of alcohol weekly for at least 1 year were considered drinkers. According to Lauren’s criteria, tumors were classified as intestinal or diffuse type. The stage was assessed according to Cancer Staging Manual of the American Joint Committee on Cancer, 7th Edition.
 |
Table 1 Clinicopathological features of GC patients in both cohorts |
Treatment plan
Patients received PF-based chemotherapy, including fluorouracil plus cisplatin or oxaliplatin, for at least four cycles. Chemotherapy was initiated within 1 month after the operation. Patients given adjuvant chemotherapy were required to satisfy the following conditions: 1) leukocyte count was greater than or equal to 4×109/L, 2) platelet count was greater than or equal to 80×109/L, 3) hemoglobin level was greater than or equal to 8 g/dL and 4) there were no signs of organ toxicities.
SNP genotyping
The surgical specimens were treated immediately after the operation. They were fixed in buffered paraformaldehyde and then embedded in paraffin. By proteinase K digestion, isopropyl alcohol extraction and ethanol precipitation, we extracted genomic DNA from the paraffin sections. MAP3K1 SNP genotyping was performed using the ABI 7900HT Real Time PCR System (Applied Biosystems, Foster City, CA, USA). The sequences of the primers used for PCR were F-primer (5ʹ-GAGATGCCCCTGCTGGAGAAAG-3ʹ) and R-primer (5ʹ-AAGGACACAGATTTATGGGAAGGAGTC-3ʹ). SNPs were analyzed by ABI3130 gene analyzer and genotypes were determined by Genemapper 4.0 software (Applied Biosystems). For quality control, two independent researchers performed genotype analyses blindly. We also selected 10% of the samples randomly for genotype verification. The results were 100% consistent.
Bioinformatics analysis
HaploReg v4.1 (https://pubs.broadinstitute.org/mammals/haploreg/haploreg.php) was used to predict the potential functions of MAP3K1 rs889312.31 This online tool gives information on SNPs that are in linkage disequilibrium (LD) with the queried SNP and also provides information on which of these SNPs lie in promoter histone marks, enhancer histone marks, DNAse sites and protein binding regions. Sequence conservation across mammals, the effects of SNPs on regulatory motifs and expression from eQTL studies are also informed. All SNPs in LD (r2>0.8, 1000G Phase 1 Asian population) with MAP3K1 rs889312 were also selected for function annotation and prediction.
Statistical analysis
All statistical tests were performed with two sides using the SPSS software (version 21; SPSS Inc. Chicago, IL). If p-value <0.05, sufficient statistical significance was considered. Dominant, recessive and codominant models were used to estimate the genetic effects of MAP3K1 rs889312 SNP. Pearson’s chi-squared test was performed to confirm the correlations between MAP3K1 rs889312 SNP and clinicopathologic parameters. The log-rank test and Kaplan–Meier method were utilized for survival analysis. Cox regression analysis was carried out to determine the independence of effects for GC prognosis.
Results
Study patients’ characteristics and survival
In this study, 591 samples were recruited after curative surgery. Among them, 207 cases received PF-based adjuvant chemotherapy, while the remaining 384 cases did not accept chemotherapy. The average age of patients carried out chemotherapy is 59 years, while those over 60 years tended not to receive postoperative chemotherapy, with a mean age of 61.64 years (p=0.002). As shown in Table 1, the remaining clinical pathological characteristics did not differ between the two groups. Due to lack of genotype information, 16 patients were excluded for further MAP3K1 analysis. The frequency distribution of MAP3K1 (rs889312) genotype was 22.6% (130 cases) for AA, 52.3% (301 cases) for AC and 25.0% (144 cases) for CC. There was no difference in this SNP’s genotype distribution between the two groups. The observed frequencies were 48.8% for allele A and 51.2% for allele C, matching the expected frequencies in an East Asian population (https://www.ncbi.nlm.nih.gov/snp/).
A flowchart of survival analysis is shown in Figure 1. Survival analysis showed a definite link between TNM stage and survival time of patients. Lymph node metastasis also significantly influenced survival outcome. The median OS was 62 months (95% CI: 48.8–75.2) in all patients. And patients who received adjuvant chemotherapy had a mean OS of 61.55 years. The OS was longer than that of patients without chemotherapy (59 months), though the difference is insignificant (p=0.489). In the treated group, 105 patients had a cisplatin plus fluorouracil (CF) regimen and 90 patients accepted oxaliplatin plus fluorouracil regimen. No significant difference was found in survival time between patients treated with cisplatin-based and oxaliplatin-based regimens (p=0.144). The details are shown in Table 2.
 |
Table 2 Relationships between clinicopathological variables and survival of GC patients |
 |
Figure 1 The flowchart of patients included in the survival analysis. |
MAP3K1 rs889312 polymorphism predicted OS in GC patients who received adjuvant chemotherapy based on PF
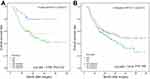
In order to confirm the role of this polymorphism in predicting clinical prognosis, log-rank test, Cox regression analyses and Kaplan–Meier survival curves were used to assess and display relationships between MAP3K1 rs889312 genotypes and OS of the two groups in different genetic models (Table 3). When adjusted by demographic and pathological variables, including sex, age, tumor features and TNM stage, MAP3K1 rs889312 could act as an independent prognostic factor for patients who had adjuvant chemotherapy (Figure 2A). Patients carrying MAP3K1 rs889312 AA genotype had a mean OS of 68.12 months, which was longer than that of patients with AC/CC genotype (56.83 months). And compared with AA genotype, MAP3K1 rs889312 AC/CC genotype increased mortality risk (HR, 3.308; 95% CI: 1.434–7.629). The post hoc tests showed similar results. Compared with AA genotype, MAP3K1 rs889312 AC and CC genotype both increased mortality risk of patients who received PF-based chemotherapy (AC vs AA: HR, 2.960; 95% CI: 1.409–6.218; CC vs AA: HR, 2.467; 95% CI: 1.102–5.520). And compared with AC genotype, CC genotype decreased the risk, but without significance (HR, 0.875; 95% CI: 0.538–1.424). However, for those who did not receive adjuvant chemotherapy, MAP3K1 rs889312 was not related to OS (Figure 2B).
 |
Table 3 Associations between MAP3K1 rs889312 SNP and OS of GC patients in various genetic models for both cohorts |
Stratified analysis of patients by chemotherapy regimens
Patients were stratified by chemotherapy based on cisplatin or oxaliplatin. And then, we explored the impact of MAP3K1 rs889312 genotypes in stratified patients’ OS. As shown in Table 4, AC/CC genotype negatively affected OS in patients who underwent oxaliplatin-based chemotherapy in dominant models (HR, 8.253; 95% CI: 1.119–60.853, log-rank p=0.013). The results demonstrated that the C allele may be a risk factor for the prognosis of patients who received oxaliplatin-based chemotherapy compared with the A allele. However, cisplatin-based chemotherapy subgroup did not show similar results. Figure 3 shows the survival curves of the two subgroups using the Kaplan–Meier method.
 |
Table 4 Associations between MAP3K1 rs889312 SNP and OS of GC patients among chemotherapy subgroups in dominant model |
Stratified analysis of patients with certain subtypes of GC
Further stratified analysis of tumors’ clinicopathologic features were done to explore the relationships between MAP3K1 rs889312 genotypes and survival of patients who received adjuvant chemotherapy (Table 5). Compared to the AA genotype, MAP3K1 rs889312 AC/CC genotype significantly reduced the OS time of patients with tumors smaller than or equal to 5 cm (HR, 3.706; 95% CI: 1.329–10.335, p=0.012), poorly differentiated tumors (HR, 3.002; 95% CI: 1.076–8.377, p=0.036) or intestinal tumors (HR, 4.780; 95% CI: 1.138–20.073, p=0.033).
 |
Table 5 Stratified analysis of patients with certain subtypes of GC |
Functional prediction
Rs889312 overlaps with an enhancer in 12 tissue types. H3K4me1, H3K27ac and H3K9ac are all contributing to the chromatin state assignment at this SNP in these cell types. It also overlaps some motifs (Pou2f2, Zfp187) but not those corresponding to TFs with overlapping binding sites. And there is only a ChIP-seq result reported, GATA3 protein bound by ChIP-seq as well as 16 eQTL results. From the eQTL results, we found that rs889312 was correlated with STED9 expression in gastric tissues. There are 7 SNPs in LD2>0.8 with rs889312. Only rs6450401 of them overlap TF-binding sites, enhancer marks, promoter marks and DNse peaks, and would be worth further investigation.
Discussion
PF-based chemotherapy after surgery in patients with advanced GC is well accepted worldwide.32 Nowadays, clinical stage and metastatic setting are considered as the main clinical prognostic factors. And we ascertain the treatment decision under pathological diagnoses. When given a treatment regimen, a standard protocol is usually prescribed. However, even stratified according to histology and other clinical information, survival outcomes are still quite heterogeneous. It highlights the need for further improvements in predictive markers.
MAP3K1 mutations were frequently found in GC with a percentage of 35.0%, higher than that of other tumors.33 For nasopharyngeal adenocarcinoma, the frequency was 10%.34 Koh J et al determined somatic mutational profiles of stage II/III GCs according to their tumor microenvironment immune types (TMITs), which classify cancer based on co-assessment of PD-L1 expression and CD8+ tumor infiltrating lymphocytes. And MAP3K1 mutations were enriched in the TMIT II (48.0%) and III (50.0%) groups.33 Therefore, variants of MAP3K1 may play a certain role in the occurrence and development of GC. However, there were few studies that discussed the role of it in GC and there were controversies. MAP3K1 rs16886448 was significantly associated with GC risk in both the pooled and meta-analysis results, whereas heterogeneity across the analyses was found.35 And only at a high enterolactone level the A allele of MAP3K1 rs252902 was associated with a reduced risk of GC.35 In our previous study, we revealed that MAP3K1 rs889312 AC variant genotype was associated with a statistically significant 30% decrease in survival of GC patients compared to the AA/CC homozygotes.30
MAP3K1 may also guide personalized treatment. For example, in epirubicin-treated triple negative breast cancer (TNBC) samples and cells, MAP3K1 was obviously enriched, possibly contributing to the epirubicin resistance in TNBC.36 The genetic variants of MAP3K1 may also predict chemotherapy reactions. For non-small cell lung cancer patients who received platinum plus taxane treatment, 4 SNPs, rs17661089, rs16886403, rs726501 in MAP3K1 gene were significantly associated with OS.37 Patients with rare homozygote genotypes of these variants in MAP3K1 had significantly poorer OS. MAP3K1 rs889312 (CC) was significantly associated with poor DDFS and DFS in breast cancer patients receiving adjuvant chemotherapy.28
In this work, we explored the clinical and prognostic significance of MAP3K1 rs889312 polymorphism in Chinese GC patients. Independent of personal characteristics, tumor features and pathological variables, MAP3K1 rs889312 could act as a significant prognostic biomarker for GC patients accepted PF-based chemotherapy after surgery. Maybe there are some mechanisms to explain it.
Insensitivity or resistance to chemotherapy drugs is a persistent problem. Either intrinsic or acquired resistance caused by genetic or epigenetic events may develop, seriously compromising the drugs’ efficacy. All events within cancer cells or by extracellular cues may activate the signaling pathways regulating the growth and survival of cancer cells.38,39 One mechanism of anticancer drugs resistance is capable of surging from alterations in the lethal signaling pathways triggered by molecular lesions.40,41
MAPK pathway is a core pathway that acts independently in cell cycle control and additively drives tumor initiation mainly via phosphorylation.42 The classical MAPK families consist of ERK, JNK as well as p38.43 Activated MAPK pathways seem to vary extensively in tumors and play an important role in the reaction to drug therapy.44–46 For example, the MAPK/ERK pathway could induce drug resistance in cancer cells. The reason may be partially due to the imbalance of functional PTEN and p53.47 The responses of chemotherapeutic agents were also impacted by the JNK/MAPK pathway, which may control cell apoptosis and autophagy.48 The inhibitory effect of p38-MAPK reduced chemotherapeutic resistance by inhibiting the activity or expression of P-glycoprotein.49 Moreover, in human lung cancer cells, p38-MAPK also induced the degradation of mouse double-minute 2. It could confer paclitaxel resistance mainly by the regulation of EGFR.50 Therefore, specific interactions between MAPKs and their substrates are crucial for mediating signaling input and output and then could influence chemosensitivity and chemoresistance.
MAP3K1 localized upstream of the MAPK signaling pathways. MAPK kinase kinase protein is encoded by MAP3K1. It can be activated by lots of stimuli like growth factors, mild hyperosmolarity, proinflammatory cytokines, cold temperature, etc. and then phosphorylates and activates the MAPK kinase (MAPK2) and in turn phosphorylates the MAPK. The MAPK finally regulates the effects of downstream signaling on multiple cancer genes.51,52 MAP3K1 rs889312 SNP was first identified in 2007 and confirmed as a susceptibility locus for breast cancer.53,54 The SNP rs889312 is located in the region containing the MAP3K1 gene. The AC/CC genotype may alter the translation of MAP3K1 gene and increase the expression of translated protein, consequently activate the MAPK signaling pathway and induce drug resistance.
PIK3CA mutations are known to confer resistance to chemotherapy.7,53 SNP variants at the MAP3K1/SETD9 locus 5q11.2 were found to be associated with somatic PIK3CA variants in breast cancers. A direct association between both MAP3K1 and SETD9 overexpression and PIK3CA somatic mutation (SM) status were found.54 The bioinformatics analysis of MAP3K1 rs889312 indicated its potential link with the regulation of the expression of SETD9 in gastric tissue. We hypothesized that MAP3K1 rs889312 may influence the expression of SETD9, consequently alter the status of PIK3CA SM and affect drug reaction. However, the exact mechanisms are largely unknown and need further investigation.
Further stratification analysis showed that patients who received oxaliplatin-based chemotherapy could benefit from longer survival times with MAP3K1 rs889312 AA genotype. Cisplatin and oxaliplatin are widely prescribed compounds with antineoplastic effects. All platinum drugs form adducts with tumor DNA. However, compared with other platinum, the cytotoxicity of oxaliplatin added. And it forms fewer DNA adducts.55 Mutations in MAPK/ERK pathway, including mutations of MAP3K1, were not associated with survival or response to carboplatin-based therapy in non-small cell lung cancer. In our study, the prediction of MAP3K1 rs889312 was not significant in the cisplatin-based therapy. DNA repair pathway may be more important than MAPK pathway for the efficacy of cisplatin. However, the expression of MAP3K1 was correlated with cisplatin GI50 (concentration that causes 50% growth inhibition) values, but not with carboplatin and/or oxaliplatin GI50.56 It may be one of the gene signatures for cisplatin. The intrinsic properties of the platinum drugs lead to differences in their activity and resistance profiles. The exact underlying cause remains to be elucidated.
In our previous study, rs889312 heterozygous AC genotype was significantly associated with an increased rate of mortality among patients with diffuse-type GC.30 Further, stratified analysis found that that no significant influence of rs889312 in diffuse-type GC patients who received PF-based therapy was revealed. However, the relationship between rs889312 heterozygous AC genotype and diffuse-type GC outcome was still significant in patients without PF-based therapy (HR, 1.431; 95% CI: 1.033–1.983, p=0.031). We considered that PF-based chemotherapy may improve the prognosis of patients with rs889312 heterozygous AC genotype. However, due to the limited number of patients in our study, the interpretations should be treated with caution. Further validation of our findings in a larger cohort is warranted.
As we have seen, this may be the first report revealing the relationship between MAP3K1 rs889312 polymorphism and survival of advanced GC patients performed adjuvant treatment based on PF regimen. However, our study has some limitations. First of all, we only examined MAP3K1 rs889312, leaving other MAPK pathway polymorphisms and their synergistic effects untested. Secondly, Helicobacter pylori infection participated in the occurrence and development of GC. And Her-2 status was considered as an important aspect of the therapy regimens. However, the status of H. pylori infection and Her-2 was not included due to lack of medical records. Thirdly, to validate our results, longer follow-up time and more samples are needed.
In conclusion, MAP3K1 rs889312 polymorphism may serve as a prognostic biomarker for stage II and III GC patients with PF-based chemotherapy after surgery. Moreover, MAP3K1 rs889312 genetic models have specific effects on the outcomes of PF-based chemotherapy in certain subtypes of GC. Combined with clinical pathological parameters, MAP3K1 rs889312 SNP could help us to make a clinical decision for personalized treatment. The underlying mechanisms and further prospective clinical trials should be performed to validate our findings.
Ethics
We confirmed that this study was conducted in accordance with the Declaration of Helsinki.
Acknowledgments
Our work was supported by grants from the National Natural Science Foundation of China (grant number 81572928 and 81772978) and from Jiangsu Provincial Special Program of Medical Science (grant number BE2017611).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34. doi:10.3322/caac.21551
2. Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–132. doi:10.3322/caac.21338
3. Van Den Ende T, Ter Veer E, Machiels M, et al. The efficacy and safety of (Neo) adjuvant therapy for gastric cancer: a network meta-analysis. Cancers (Basel). 2019;11(1):80. doi:10.3390/cancers11010080
4. Fornaro L, Vasile E, Aprile G, et al. Locally advanced gastro-oesophageal cancer: recent therapeutic advances and research directions. Cancer Treat Rev. 2018;69:90–100. doi:10.1016/j.ctrv.2018.06.012
5. Sasako M, Sakuramoto S, Katai H, et al. Five-year outcomes of a randomized phase III trial comparing adjuvant chemotherapy with S-1 versus surgery alone in stage II or III gastric cancer. J Clin Oncol. 2011;29(33):4387–4393. doi:10.1200/JCO.2011.36.5908
6. Sadighi S, Mohagheghi MA, Montazeri A, Sadighi Z. Quality of life in patients with advanced gastric cancer: a randomized trial comparing docetaxel, cisplatin, 5-FU (TCF) with epirubicin, cisplatin, 5-FU (ECF). BMC Cancer. 2006;6:274. doi:10.1186/1471-2407-6-274
7. Wang K, Li M, Hakonarson H. Analysing biological pathways in genome-wide association studies. Nat Rev Genet. 2010;11(12):843–854. doi:10.1038/nrg2884
8. Ma G, Gu D, Lv C, et al. Genetic variant in 8q24 is associated with prognosis for gastric cancer in a Chinese population. J Gastroenterol Hepatol. 2015;30(4):689–695. doi:10.1111/jgh.12801
9. Zhang Y, Zhu H, Zhang X, et al. Clinical significance of MYT1L gene polymorphisms in Chinese patients with gastric cancer. PLoS One. 2013;8(8):e71979. doi:10.1371/journal.pone.0071979
10. Zhang X, Gu D, Du M, et al. Associations of NR5A2 gene polymorphisms with the clinicopathological characteristics and survival of gastric cancer. Int J Mol Sci. 2014;15(12):22902–22917. doi:10.3390/ijms151222902
11. Zhang X, Zhu H, Wu X, et al. A genetic polymorphism in TOX3 is associated with survival of gastric cancer in a Chinese population. PLoS One. 2013;8(9):e72186. doi:10.1371/journal.pone.0072186
12. Zhao T, Oho AUID, Huo X, Chen J. Genetic polymorphism of rs9564966 G > A on 13q22.1 predicts poor survival for Chinese patients with gastric cancer. Cancer Med. 2019;8(1):428–436. doi:10.1002/cam4.1693
13. Gu D, Zheng R, Xin J, et al. Evaluation of GWAS-identified genetic variants for gastric cancer survival. EBioMedicine. 2018;33:82–87. doi:10.1016/j.ebiom.2018.06.028
14. Xu Z, Zhu H, Luk JM, et al. Clinical significance of SOD2 and GSTP1 gene polymorphisms in Chinese patients with gastric cancer. Cancer. 2012;118(22):5489–5496. doi:10.1002/cncr.27599
15. Zhang G, Gu D, Zhao Q, et al. Genetic variation in C12orf51 is associated with prognosis of intestinal-type gastric cancer in a Chinese population. Biomed Pharmacother. 2015;69:133–138. doi:10.1016/j.biopha.2014.11.009
16. Zhou J, Liu ZY, Li CB, et al. Genetic polymorphisms of DNA repair pathways influence the response to chemotherapy and overall survival of gastric cancer. Tumour Biol. 2015;36(4):3017–3023. doi:10.1007/s13277-014-2936-3
17. Zhang H, Zhao W, Gu D, et al. Association of antioxidative enzymes polymorphisms with efficacy of platin and fluorouracil-based adjuvant therapy in gastric cancer. Cell Physiol Biochem. 2018;48(6):2247–2257. doi:10.1159/000492642
18. Zhao T, Gu D, Xu Z, et al. Polymorphism in one-carbon metabolism pathway affects survival of gastric cancer patients: Large and comprehensive study. Oncotarget. 2015;6(11):9564–9576. doi:10.18632/oncotarget.3259
19. Zhao T, Xu Z, Gu D, et al. The effects of genomic polymorphisms in one-carbon metabolism pathways on survival of gastric cancer patients received fluorouracil-based adjuvant therapy. Sci Rep. 2016;6:28019. doi:10.1038/srep28019
20. Johnson GL, Lapadat R. Mitogen-activated protein kinase pathways mediated by ERK, JNK, and p38 protein kinases. Science. 2002;298(5600):1911–1912. doi:10.1126/science.1072682
21. Keshet Y, Seger R. The MAP kinase signaling cascades: a system of hundreds of components regulates a diverse array of physiological functions. Methods Mol Biol. 2010;661:3–38. doi:10.1007/978-1-60761-795-2_1
22. Grossi V, Peserico A, Tezil T, Simone C. p38alpha MAPK pathway: a key factor in colorectal cancer therapy and chemoresistance. World J Gastroenterol. 2014;20(29):9744–9758. doi:10.3748/wjg.v20.i29.9744
23. Zhao BX, Sun YB, Wang SQ, et al. Grape seed procyanidin reversal of p-glycoprotein associated multi-drug resistance via down-regulation of NF-kappaB and MAPK/ERK mediated YB-1 activity in A2780/T cells. PLoS One. 2013;8(8):e71071. doi:10.1371/journal.pone.0071071
24. Kong LR, Chua KN, Sim WJ, et al. MEK inhibition overcomes cisplatin resistance conferred by SOS/MAPK pathway activation in squamous cell carcinoma. Mol Cancer Ther. 2015;14(7):1750–1760. doi:10.1158/1535-7163.MCT-15-0062
25. Berger MD, Stintzing S, Heinemann V, et al. Impact of genetic variations in the MAPK signaling pathway on outcome in metastatic colorectal cancer patients treated with first-line FOLFIRI and bevacizumab: data from FIRE-3 and TRIBE trials. Ann Oncol. 2017;28(11):2780–2785. doi:10.1093/annonc/mdx412
26. Shan J, Mahfoudh W, Dsouza SP, et al. Genome-Wide Association Studies (GWAS) breast cancer susceptibility loci in Arabs: susceptibility and prognostic implications in Tunisians. Breast Cancer Res Treat. 2012;135(3):715–724. doi:10.1007/s10549-012-2202-6
27. Xie N, Yao Y, Wan L, Zhu T, Liu L, Yuan J. Next-generation sequencing reveals lymph node metastasis associated genetic markers in colorectal cancer. Exp Ther Med. 2017;14(1):338–343. doi:10.3892/etm.2017.4464
28. Kuo SH, Yang SY, You SL, et al. Polymorphisms of ESR1, UGT1A1, HCN1, MAP3K1 and CYP2B6 are associated with the prognosis of hormone receptor-positive early breast cancer. Oncotarget. 2017;8(13):20925–20938. doi:10.18632/oncotarget.14995
29. Tapper W, Hammond V, Gerty S, et al. The influence of genetic variation in 30 selected genes on the clinical characteristics of early onset breast cancer. Breast Cancer Res. 2008;10(6):R108. doi:10.1186/bcr2213
30. Wei X, Zhang E, Wang C, et al. A MAP3k1 SNP predicts survival of gastric cancer in a Chinese population. PLoS One. 2014;9(4):e96083. doi:10.1371/journal.pone.0096083
31. Ward LD, Kellis M. HaploReg: a resource for exploring chromatin states, conservation, and regulatory motif alterations within sets of genetically linked variants. Nucleic Acids Res. 2012;40(Database issue):D930–D934. doi:10.1093/nar/gkr917
32. Noh SH, Park SR, Yang HK, et al. Adjuvant capecitabine plus oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): 5-year follow-up of an open-label, randomised phase 3 trial. Lancet Oncol. 2014;15(12):1389–1396. doi:10.1016/S1470-2045(14)70473-5
33. Koh J, Nam SK, Roh H, et al. Somatic mutational profiles of stage II and III gastric cancer according to tumor microenvironment immune type. Genes Chromosomes Cancer. 2019;58(1):12–22. doi:10.1002/gcc.22683
34. Ali SM, Yao M, Yao J, et al. Comprehensive genomic profiling of different subtypes of nasopharyngeal carcinoma reveals similarities and differences to guide targeted therapy. Cancer. 2017;123(18):3628–3637. doi:10.1002/cncr.30781
35. Yang JJ, Cho LY, Ko KP, et al. Interaction effects between genes involved in the AKT signaling pathway and phytoestrogens in gastric carcinogenesis: a nested case-control study from the Korean multi-center cancer cohort. Mol Nutr Food Res. 2012;56(11):1617–1626. doi:10.1002/mnfr.201200169
36. Huang J, Luo Q, Xiao Y, Li H, Kong L, Ren G. The implication from RAS/RAF/ERK signaling pathway increased activation in epirubicin treated triple negative breast cancer. Oncotarget. 2017;8(64):108249–108260. doi:10.18632/oncotarget.22604
37. Li Y, Sun Z, Cunningham JM, et al. Genetic variations in multiple drug action pathways and survival in advanced stage non-small cell lung cancer treated with chemotherapy. Clin Cancer Res. 2011;17(11):3830–3840. doi:10.1158/1078-0432.CCR-10-2877
38. Martz CA, Ottina KA, Singleton KR, et al. Systematic identification of signaling pathways with potential to confer anticancer drug resistance. Sci Signal. 2014;7(357):ra121. doi:10.1126/scisignal.aaa1877
39. Nussinov R, Tsai CJ, Jang H. A new view of pathway-driven drug resistance in tumor proliferation. Trends Pharmacol Sci. 2017;38(5):427–437. doi:10.1016/j.tips.2017.02.001
40. Galluzzi L, Vitale I, Michels J, et al. Systems biology of cisplatin resistance: past, present and future. Cell Death Dis. 2014;5:e1257.
41. Dasari S, Tchounwou PB. Cisplatin in cancer therapy: molecular mechanisms of action. Eur J Pharmacol. 2014;740:364–378. doi:10.1016/j.ejphar.2014.07.025
42. Pham TT, Angus SP, Johnson GL. MAP3K1: genomic alterations in cancer and function in promoting cell survival or apoptosis. Genes Cancer. 2013;4(11–12):419–426. doi:10.1177/1947601913513950
43. Dhillon AS, Hagan S, Rath O, Kolch W. MAP kinase signalling pathways in cancer. Oncogene. 2007;26(22):3279–3290. doi:10.1038/sj.onc.1210421
44. Lu H, Liu S, Zhang G, et al. PAK signalling drives acquired drug resistance to MAPK inhibitors in BRAF-mutant melanomas. Nature. 2017;550(7674):133–136. doi:10.1038/nature24040
45. Amaral T, Sinnberg T, Meier F, et al. MAPK pathway in melanoma part II-secondary and adaptive resistance mechanisms to BRAF inhibition. Eur J Cancer. 2017;73:93–101. doi:10.1016/j.ejca.2016.12.012
46. Ma Y, Wang L, Neitzel LR, et al. The MAPK pathway regulates intrinsic resistance to BET inhibitors in colorectal cancer. Clin Cancer Res. 2017;23(8):2027–2037. doi:10.1158/1078-0432.CCR-16-0453
47. Milosevic Z, Pesic M, Stankovic T, et al. Targeting RAS-MAPK-ERK and PI3K-AKT-mTOR signal transduction pathways to chemosensitize anaplastic thyroid carcinoma. Transl Res. 2014;164(5):411–423. doi:10.1016/j.trsl.2014.06.005
48. Sui X, Kong N, Ye L, et al. p38 and JNK MAPK pathways control the balance of apoptosis and autophagy in response to chemotherapeutic agents. Cancer Lett. 2014;344(2):174–179. doi:10.1016/j.canlet.2013.11.019
49. Guo X, Ma N, Wang J, et al. Increased p38-MAPK is responsible for chemotherapy resistance in human gastric cancer cells. BMC Cancer. 2008;8:375. doi:10.1186/1471-2407-8-172
50. Park SH, Seong MA, Lee HY. p38 MAPK-induced MDM2 degradation confers paclitaxel resistance through p53-mediated regulation of EGFR in human lung cancer cells. Oncotarget. 2016;7(7):8184–8199. doi:10.18632/oncotarget.6945
51. Witowsky JA, Johnson GL. Ubiquitylation of MEKK1 inhibits its phosphorylation of MKK1 and MKK4 and activation of the ERK1/2 and JNK pathways. J Biol Chem. 2003;278(3):1403–1406. doi:10.1074/jbc.C200616200
52. Xue Z, Vis DJ, Bruna A, et al. MAP3K1 and MAP2K4 mutations are associated with sensitivity to MEK inhibitors in multiple cancer models. Cell Res. 2018;28(7):719–729. doi:10.1038/s41422-018-0044-4
53. Wang Q, Shi YL, Zhou K, et al. PIK3CA mutations confer resistance to first-line chemotherapy in colorectal cancer. Cell Death Dis. 2018;9(7):739. doi:10.1038/s41419-018-1111-y
54. Puzone R, Pfeffer U. SNP variants at the MAP3K1/SETD9 locus 5q11.2 associate with somatic PIK3CA variants in breast cancers. Eur J Hum Genet. 2017;25(3):384–387. doi:10.1038/ejhg.2016.179
55. Woynarowski JM, Faivre S, Herzig MC, et al. Oxaliplatin-induced damage of cellular DNA. Mol Pharmacol. 2000;58(5):920–927. doi:10.1124/mol.58.5.920
56. Mucaki EJ, Zhao J, Lizotte DJ, Rogan PK. Predicting responses to platin chemotherapy agents with biochemically-inspired machine learning. Signal Transduct Target Ther. 2019;4:1. doi:10.1038/s41392-018-0034-5
57. Washington K. 7th edition of the AJCC cancer staging manual: stomach. Ann Surg Oncol. 2010;17(12):3077–3079.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.