Back to Journals » Clinical Ophthalmology » Volume 16
Management Strategies of Juvenile Idiopathic Arthritis-Associated Chronic Anterior Uveitis: Current Perspectives
Authors Paroli MP , Del Giudice E , Giovannetti F, Caccavale R, Paroli M
Received 30 March 2022
Accepted for publication 18 May 2022
Published 28 May 2022 Volume 2022:16 Pages 1665—1673
DOI https://doi.org/10.2147/OPTH.S342717
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Maria Pia Paroli,1 Emanuela Del Giudice,2 Francesca Giovannetti,1 Rosalba Caccavale,3 Marino Paroli3
1Uveitis Service, Ophthalmologic Unit, Department of Sense Organs, Sapienza University of Rome, Rome, Italy; 2Pediatric Rheumatology Unit, Department of Maternal Infantile and Urological Sciences, Sapienza University of Rome, Rome, Italy; 3Clinical Immunology Unit, Department of Clinical, Anesthesiological and Cardiovascular Sciences, Sapienza University of Rome, Rome, Italy
Correspondence: Maria Pia Paroli, Uveitis Service, Ophthalmologic Unit, Department of Sense Organs, Sapienza University of Rome, Rome, Italy, Tel/Fax +39-06-519-3220, Email [email protected]
Abstract: Juvenile idiopathic arthritis (JIA) is the most common extraocular disease associated with pediatric uveitis. Despite the growing knowledge about the pathogenetic and clinical characteristics of the disease, it still remains a challenge for both the pediatric rheumatologist and ophthalmologist. Since uveitis is asymptomatic in most cases, it is generally detected by parents in a late phase of the disease when complications have occurred with consequent severe vision loss. Improvement in attentive screening and early treatment initiation to suppress inflammation has considerably reduced the sight-threatening outcomes of JIA-associated chronic anterior uveitis (JIA-CAU). Initial treatment with topical steroids is effective in most cases. However, more severe cases require the use of periocular or systemic corticosteroids, possibly leading to long-term complications. These include growth retardation, cataract and glaucoma. Systemic immunosuppressive agents are then employed in patients resistant to first-line therapy or to reduce steroid-associated complications. In this review, we will discuss the immunosuppressant agents currently employed for the treatment of the disease, including anti-tumor necrosis factor (TNF)α biologics approved or not by the regulatory agencies. We will also highlight how new therapeutic options like biologic targeting cytotoxic T-lymphocyte antigen-4 (CTLA-4) co-stimulatory molecule, interleukin-6 receptor (IL-6R) or B lymphocytes might represent exciting new options for patients resistant to conventional therapy. Finally, the potential use of janus kinase (JAK) inhibitors recently approved for the treatment of several inflammatory rheumatic diseases in adults will be also discussed.
Keywords: juvenile idiopathic arthritis, uveitis, biologics, JAK inhibitors
Introduction
Juvenile idiopathic arthritis (JIA) is a progressive rheumatic disease characterized by chronic joint inflammation of unknown etiology.1 The condition begins typically before the age of 16 and lasts at least six weeks. JIA global prevalence is about 1:1000.2 Epidemiological studies have shown that the disease occurs more frequently in certain areas including North America, Scandinavia, United Kingdom and Germany.3
Based on the course of the disease, the International League of Associations of Rheumatology (ILAR) has recognized 7 subtypes:4 a) systemic JIA; b) oligoarthritis; c) rheumatoid factor (RF)-negative polyarthritis; d) RF-positive polyarthritis; e) psoriatic arthritis (PsA); f) enthesitis-related arthritis (ERA); g) undifferentiated arthritis (UA).
JIA is by far the systemic disease most frequently associated with anterior uveitis in the pediatric population, accounting for up to 47% of all types of uveitis seen in children.3,5 With regard to the different subtypes, it has been reported that about 20% of patients affected by oligoarticular JIA and 10% by RF-negative polyarticular JIA are affected by CAU. In addition, ERA and PsA subtypes have been found to be at high risk of acute and recurrent forms of uveitis. In the remaining JIA subtypes uveitis is rare.1 Both eyes may be affected within the first year of JIA, but in these cases ocular inflammation is often asymptomatic,6–8 while uveitis precedes arthritis in only 3–7% of cases.9
Patients with antinuclear antibody (ANA)-positive juvenile idiopathic arthritis constitute a homogeneous subgroup irrespective of the course of joint disease. One-third of ANA-positive, early-onset JIA patients develop CAU within the first 5 years of the disease.10
A number of risk factors for developing uveitis by JIA patients have been identified. These include: female gender, the oligoarticular form, early onset, ANA positivity, presence of HLA-DRB1*11 or HLA-DRB1*13 and RF-negative test.11 Since the disease is asymptomatic in most cases, it can be detected by parents only when complications such as band keratopathy or strabismus occur or by failed vision screening. Thus, slit-lamp screening is mandatory to prevent sight-threatening complications, especially in the first two years after diagnosis. The eye may be severely inflamed even though it appears entirely white. When symptoms are present, they may include eye discomfort, photophobia and blurring. Clinical signs include bilateral non-granulomatous inflammation with fine keratic precipitates (KP), inflammatory cells and posterior synechiae. Conversely, ciliary injection and hypopyon are rare. Complications resulting from either CAU or prolonged use of local steroid drops include cystoid macular edema, band keratopathy, amblyopia, cyclitic membranes, secondary glaucoma and, although less frequently, phthisis. All these events are responsible for the reduction of visual acuity. Risk of cataract development among children with juvenile idiopathic arthritis-related uveitis treated with topical corticosteroids is also increased.12 Posterior synechiae, band keratopathy and cataracts are often observed at presentation, while glaucoma, hypotony and macular edema may be detected during follow-up.13 Therefore, it is of great import that, while the development of new treatments has markedly improved the prognosis of arthritis in JIA patients, chronic uveitis may still lead to severe visual impairment in a significant proportion of patients if ocular disease is not detected at an early stage and is treated properly.14 It has been reported that up to one in four children with JIA may progress to blindness.15
The purpose of this review is to describe current management and treatment options including promising new therapies of JIA-CAU in the context of multidisciplinary care from both rheumatologist and ophthalmologist.
Management
As outlined above, CAU is often asymptomatic in JIA patients, or young children may be preverbal and unable to express discomfort. The classic signs and symptoms of anterior uveitis like red eye, pain, photophobia and blurred vision are frequently absent. Irregular or infrequent monitoring of children with JIA can lead to serious consequences due to undetected development or exacerbation of intraocular inflammation.16,17 The frequency of severe and irreversible visual impairment is still very high in young patients with JIA-CAU. Therefore, accurate screening and early treatment are needed to avoid sight-threatening complications.18
In 2019 the American College of Rheumatology/Arthritis Foundation (ACR/AF) issued recommendations for the screening, monitoring and treatment of uveitis in children with JIA.19 Visual acuity testing according to the age of the patient, slit lamp examination, with evaluation of cells and flare in the anterior chamber, intraocular pressure measurement and dilated examination of the posterior pole are needed in every evaluation.
Ophthalmic screening every three months is also recommended for high-risk children such as those with oligoarticular and RF-negative polyarticular JIA as well as for patients who have psoriatic arthritis or undifferentiated arthritis with a positive ANA test, are younger than 7 years of age at JIA onset, have JIA duration of 4 years or less and for children and adolescents with JIA and stable uveitis.
Children who are considered at low to moderate risk, namely those who are ANA-negative, aged 7 years of age or older at JIA onset, have a JIA duration of more than 4 years and those with systemic JIA, RF-positive polyarthritis and ERA can be evaluated every 6 to 12 months.
When patients suffer from uncontrolled chronic anterior uveitis, regular monitoring may be needed as frequently as every 2 to 6 weeks, based on degree of inflammation and presence of other complications.
Table 1 summarizes the recommended frequencies of ophthalmologic screening depending on JIA subtypes and associated risk to develop CAU.
 |
Table 1 JIA Subtype Risk of Developing CAU and Ophthalmologic Screening Criteria |
Standard Treatment
The main goal of treatment is to reduce or resolve chronic intraocular inflammation while limiting the side effects of treatment which are the main risk factors for visual impairment.20
Topical glucocorticoids (prednisolone acetate 1%) are the first line of treatment for anterior uveitis and are used in 90% of patients with JIA-CAU. However, long-term steroid use can lead to well-known complications such as ocular hypertension, glaucoma and cataracts, especially in children with posterior synechiae, anterior chamber (AC) flare ≥1+ and abnormal intraocular pressure (IOP) at presentation.21 Therefore, continued monitoring of IOP is mandatory as well as thorough screening for the presence of cataract, band keratopathy or macular edema.15
While tapering or discontinuing topical therapy, American College of Rheumatology/Arthritis Foundation (ACR/AF) strongly advise that an AC assessment must be done within one month after each change in order to detect possible relapses.
According to ACR/AF guidelines it is preferred to increase topical steroid treatment frequency for a short period of time rather than administration of systemic glucocorticoids. In general, glucocorticoid injections and implants are not recommended in children with JIA-CAU. However, the institution of systemic therapy is recommended for those patients who still require 1–2 drops per day for uveitis control. Systemic immunosuppressive therapy initiation is mostly indicated to allow drop tapering when 1–2 drops per day are needed to maintain control of intraocular inflammation for 3 months or longer with an elevated risk of IOP increase and/or cataract development.19
Methotrexate (MTX), a folate analogue which inhibits the enzyme dihydrofolate reductase, is a well-established first-line immunosuppressant in pediatric uveitis patients. Simonini et al conducted an extended meta-analysis concluding that an improvement of intraocular inflammation in children affected by refractory chronic anterior uveitis treated with MTX can be achieved in around 73% of cases, with the most frequent side effects being gastrointestinal discomfort and more rarely the elevation of liver enzymes.14
Other conventional disease-modifying anti-rheumatic drugs (cDMARDs) that can be considered for patients with JIA-CAU are azathioprine, leflunomide, mycophenolate and cyclosporine. Their use remains limited also because of intolerability due to adverse effects and common inefficacy in patients with refractory uveitis after MTX therapy.22–24
Innovative Treatments
Biologics
Biologics are drugs which have revolutionized the treatment of chronic inflammatory rheumatic diseases. They are proteins produced through a process of genetic engineering which specifically inhibit the inflammatory response targeting either cytokines, cytokine receptors, T-cell co-stimulatory molecules or B-cell surface receptors. Their use enabled good outcomes in many patients affected by rheumatic diseases including rheumatoid arthritis (RA), psoriatic arthritis and ankylosing spondylitis (AS). Biologics available so far are in different forms including monoclonal antibodies, receptor antagonists, soluble receptors or fusion proteins.21
In active CAU with sight-threatening complications such as the presence of ocular structural changes or severe side effects of topical steroid therapy MTX combination with an anti-tumor necrosis factor (TNF)α biologic is recommended over MTX monotherapy according to ACR/AF recommendation.19 Actually, about 15% to 50% of JIA-CAU patients under MTX alone are likely to have treatment-refractory uveitis.25
Although the TNFα soluble receptor etanercept was the first biologic approved by the US Food and Drug Administration (FDA) for the treatment of JIA, this drug has been associated with new-onset uveitis.26 Therefore, etanercept is not recommended for treatment of JIA-CAU. At present humanized monoclonal antibody adalimumab is the only biologic approved for treatment of uveitis including children and adolescents. The clinical effectiveness, safety and cost effectiveness of adalimumab in combination with MTX for the treatment of juvenile idiopathic arthritis-associated uveitis (SYCAMORE) randomized controlled trial established that treatment with adalimumab and MTX significantly delayed the time to treatment failure as compared with MTX alone.27
In a meta-analysis aimed to evaluate the efficacy and safety of anti-TNFα therapy for JIA-CAU, adalimumab was shown to be significantly more efficacious than infliximab and etanercept in the control of intra-ocular inflammation. No statistical difference between infliximab and etanercept was found.28 According to the SHARE guidelines,29 adalimumab is recommended over infliximab as the first-line biologic DMARD (bDMARD), although randomized controlled clinical trials were performed only for adalimumab.30,31 Head-to-head studies between infliximab and adalimumab are difficult to carry out due to the high variation in dose and frequency commonly required for infliximab administration. However, adalimumab was found to perform better than infliximab in improving or stabilizing visual acuity and in maintaining uveitis remission during 40 months of follow-up in an open-label comparative study.32 These results have been confirmed by other studies showing that adalimumab had a better efficacy and safety profile than infliximab for the treatment of JIA-CAU.33,34
Importantly, anti-TNFα agents have been shown to have a satisfactory safety profile with rare adverse reactions. For example, to the best of our knowledge, development of malignancy during the JIA-CAU treatment due to their immunosuppressive activity has not been yet reported.32,35
One of the main causes of treatment failure is the development of anti-drug antibodies (ADA) with consequent adalimumab or infliximab neutralization. Therefore, the combination of biologic therapy with MTX or another cDMARD is recommended to minimize this possibility.36 Moreover, data from studies of patients with HLA B27-associated uveitis demonstrated that both infliximab and adalimumab are efficacious in the treatment of ocular inflammation.37
When treatment with adalimumab fails even at above-standard dose and/or frequency, ACR/AF recommends changing to another off-label monoclonal anti-TNFα antibody. In addition to infliximab, the newest anti-TNFα human monoclonal antibody golimumab and humanized monoclonal antibody Fab fragment certolizumab currently have been shown to be a possible alternative in controlling intraocular inflammation in case of failure of first-line biologics. Although these biologics have not yet been officially approved by the regulatory international agencies for JIA-CAU treatment, a significant body of evidence exists indicating that these biologics might be very effective in the disease.35
Another possible option for primary or secondary failure of anti-TNFα treatment is the anti-IL-6R humanized monoclonal antibody tocilizumab, which has been approved for treatment of rheumatoid arthritis (RA) and more recently of JIA, though not for uveitis. Although a specific indication for the use of this treatment for JIA-CAU is still lacking, it has been shown in preliminary studies that tocilizumab is particularly beneficial for treatment of uveitis in the presence of macular edema in adults who did not respond to anti-TNFα treatments.38 In a case series of 25 patients, it has been reported that intravenous administration of tocilizumab is efficacious for treatment of severe JIA-CAU refractory to anti-TNFα.39 In the APTITUDE study, a phase 2 clinical trial which aimed to establish the efficacy of subcutaneous tocilizumab with MTX in children with JIA-CAU refractory to MTX and anti-TNFα, seven of 21 children showed response to treatment, but the threshold to proceed to a phase 3 clinical trial was not met. Nevertheless, efficacy signals for inflammation control were reported, including reduction of macular edema.40 These partially conflicting findings indicate that further studies are needed to determine the efficacy of both intravenous and subcutaneous tocilizumab for treatment of anti-TNFα refractory JIA-CAU.
CTLA-4 inhibitor abatacept, a selective T-cell co-stimulation modulator, is another molecule that may possibly be used as second-line alternative after failure of anti-TNFα therapy, as suggested by results from a randomized, double-blind, placebo-controlled withdrawal trial.41 In other studies, it was found that a significant remission rate and decrease in frequency of uveitis flares and ocular complications occurred when abatacept was used as first-line or second-line treatment.42–44
Finally, in few case series the anti-CD20 monoclonal antibody rituximab which specifically depletes B-cells has demonstrated the ability to achieve remission for some refractory cases of JIA-CAU. In a retrospective, multicenter study one cycle of rituximab treatment led to uveitis inactivity in 7 out of 10 patients with improvement in macular edema. In the same study, however, four patients required additional treatment for recurrence of uveitis during the follow-up period. It has been hypothesized by the authors that relapses possibly occurred after restoration of B-cell number and that poor response in some patients might be related to the persistence of autoreactive plasma cells that are the predominant source of antibodies.45
It is of note that the use of biologics as observed in adults with rheumatic diseases is associated with an increased risk of infection including the reactivation of latent tuberculosis and occult hepatitis B. A careful screening of these possible pre-existing conditions is therefore mandatory before starting therapy with biologics.46 In Table 2, current FDA-approval for either JIA or non-infectious uveitis (UIA) for all biologics treated in this section has been specified.
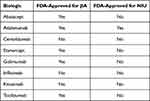 |
Table 2 Current FDA-Approval of Biologics for JIA and/or Non-Infectious Uveitis (NIU) Treatment |
Janus Kinase Inhibitors
Janus kinases (JAKs) are four cytoplasmic enzymes (JAK1, JAK2, JAK3 and TYK2) which are associated with the intracellular domain of several cytokine receptors. After cytokine/receptor interaction, JAKs are activated and phosphorylate signal transducer and activator of transcription (STATs) proteins. Activated STATs translocate to the nucleus where they induce transcription of target genes. This eventually leads to amplification of the inflammatory cascade.
A number of synthetic drugs called JAK inhibitors (JAKinhibs) have been developed to block the activation of JAKs and the consequent intracellular molecular cascade. JAKinhibs have been proven to be highly effective in the treatment of many inflammatory rheumatic diseases in adults including rheumatoid arthritis (RA), psoriatic arthritis (PsA) and ankylosing spondylitis (AS). However, their possible use in other inflammatory immune-mediated diseases is under investigation.47,48
In an experimental autoimmune uveitis model, topical treatment with JAKinhib tofacitinib (0.03%) three times a day was found to improve uveitis, clinically and histologically, and to reduce the intravitreous levels of inflammatory cytokines and their gene expression in both the iris ciliary body and the retina/choroid.49 Other findings have provided evidence that tofacitinib can modulate pro-inflammatory T-cell populations in a uveitis mouse model.50 In the clinical setting, a single case report has provided evidence for the first time of improvement in JIA-CAU and macular edema resistant to several conventional and biologic DMARDs when treated with tofacitinib 5 mg twice daily orally.51 Other case reports have been published suggesting a possible future role of tofacitinib in JIA-CAU.52–54
In a recent case series, Miserocchi et al reported the outcome of four patients with JIA and uveitis refractory to multiple immunosuppressive agents who were treated with either JAK1/JAK2 inhibitor baricitinib or pan-JAKinhib tofacitinib. They observed a significant reduction in ocular inflammatory activity by treatment with both drugs within their cohort with no serious systemic side effects.55
An international, multicenter, open-label, active-controlled study (JUVE-BRIGHT) of the safety and efficacy of baricitinib for patients with active JIA-associated uveitis is ongoing.56 The use of JAK inhibitors has been recently related with the onset of drug-specific relevant side effects in adults. These include an increased rate of herpes zoster virus (HZV) infection, thrombosis and risk to develop lung cancer.57,58 More studies on the safety of these drugs are therefore necessary also because of their potential use in child populations.
Conclusions
The management of JIA-related uveitis remains a relevant clinical challenge. Since patients are typically asymptomatic, timely and effective treatment and control of inflammation can improve visual outcomes and prevent vision loss. Regular ophthalmic screening of children with JIA is highly recommended because of the risk of uveitis. The frequency of screening should be based on individual risk factors. The prognosis of JIA-CAU has been greatly improved during the last decade, and current therapies can reduce uveitis recurrences and the need for cataract and glaucoma surgery.59
Topical glucocorticoids should be used as initial treatment to achieve control of inflammation. While MTX is the first-line corticosteroid-sparing treatment, other therapies must be considered for severe and/or refractory uveitis. Biologics blocking TNFα activity in combination with MTX are now recommended for the management of severe uveitis in the case of MTX failure. The timely addition of biologic drugs targeting IL-6R or CTLA-4, namely tocilizumab and abatacept, respectively, is a promising therapeutic tool to maintain uveitis control in children who are at continued risk of vision loss and do not respond adequately to anti-TNFα biologic agents. Anti-CD20 monoclonal antibodies targeting B-cells are also a possible future treatment option of JIA uveitis. JAKinhibs are a promising new frontier for the treatment of JIA-CAU after failure of biologic therapy. New advanced studies aimed to identify predictive biomarkers of response could critically help to individualize the optimal therapeutic approach for each patient. In this context, it must be underlined that a multidisciplinary team of ophthalmologists and rheumatologists is crucial to take care of patients affected by JIA-CAU. Finally, basic research on the pathogenesis of intraocular inflammation is warranted to identify new treatment options to satisfy the many unmet needs of this highly debilitating condition.
Disclosure
The authors report no financial interest or other conflicts of interest in this work.
References
1. Martini A, Lovell DJ, Albani S, et al. Juvenile idiopathic arthritis. Nat Rev Dis Primers. 2022;8(1):5. doi:10.1038/s41572-021-00332-8
2. Jabs DA, Nussenblatt RB, Rosenbaum JT. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140(3):509–516. doi:10.1016/j.ajo.2005.03.057
3. Smith JA, Mackensen F, Sen HN, et al. Epidemiology and course of disease in childhood uveitis. Ophthalmology. 2009;116(8):1544–1551, 1551 e1. doi:10.1016/j.ophtha.2009.05.002
4. Petty RE, Southwood TR, Manners P, et al. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol. 2004;31(2):390–392.
5. Del Giudice E, Swart JF, Wulffraat NM. Juvenile idiopathic arthritis. In: El Miedany Y, editor. Comorbidity in Rheumatic Diseases. Springer International Publishing. 2017:265–288.
6. Haasnoot AM, Kuiper JJ, Hiddingh S, et al. Ocular fluid analysis in children reveals interleukin-29/interferon-λ1 as a biomarker for juvenile idiopathic arthritis-associated uveitis. Arthritis Rheumatol. 2016;68(7):1769–1779. doi:10.1002/art.39621
7. Kolomeyer AM, Crane ES, Tu Y, Liu D, Chu DS. Adult patients with uveitis associated with juvenile idiopathic arthritis: a retrospective review. Can J Ophthalmol. 2017;52(5):458–462. doi:10.1016/j.jcjo.2017.01.011
8. Marvillet I, Terrada C, Quartier P, Quoc EB, Bodaghi B, Prieur AM. Ocular threat in juvenile idiopathic arthritis. Joint Bone Spine. 2009;76(4):383–388. doi:10.1016/j.jbspin.2008.10.015
9. Clarke SL, Sen ES, Ramanan AV. Juvenile idiopathic arthritis-associated uveitis. Pediatr Rheumatol Online J. 2016;14(1):27. doi:10.1186/s12969-016-0088-2
10. Ravelli A, Felici E, Magni-Manzoni S, et al. Patients with antinuclear antibody-positive juvenile idiopathic arthritis constitute a homogeneous subgroup irrespective of the course of joint disease. Arthritis Rheum. 2005;52(3):826–832. doi:10.1002/art.20945
11. Gregory AC 2nd, Kempen JH, Daniel E, et al. Risk factors for loss of visual acuity among patients with uveitis associated with juvenile idiopathic arthritis: the systemic immunosuppressive therapy for eye diseases study. Ophthalmology. 2013;120(1):186–192. doi:10.1016/j.ophtha.2012.07.052
12. Thorne JE, Woreta FA, Dunn JP, Jabs DA. Risk of cataract development among children with juvenile idiopathic arthritis-related uveitis treated with topical corticosteroids. Ophthalmology. 2010;117(7):1436–1441. doi:10.1016/j.ophtha.2009.12.003
13. Paroli MP, Abbouda A, Restivo L, Sapia A, Abicca I, Pivetti Pezzi P. Juvenile idiopathic arthritis-associated uveitis at an Italian tertiary referral center: clinical features and complications. Ocul Immunol Inflamm. 2015;23(1):74–81. doi:10.3109/09273948.2013.855798
14. Simonini G, Paudyal P, Jones GT, Cimaz R, Macfarlane GJ. Current evidence of methotrexate efficacy in childhood chronic uveitis: a systematic review and meta-analysis approach. Rheumatology. 2013;52(5):825–831. doi:10.1093/rheumatology/kes186
15. Angeles-Han ST, McCracken C, Yeh S, et al. Characteristics of a cohort of children with Juvenile Idiopathic Arthritis and JIA-associated Uveitis. Pediatr Rheumatol Online J. 2015;13:19. doi:10.1186/s12969-015-0018-8
16. Grassi A, Corona F, Casellato A, Carnelli V, Bardare M. Prevalence and outcome of juvenile idiopathic arthritis-associated uveitis and relation to articular disease. J Rheumatol. 2007;34(5):1139–1145.
17. Lerman MA, Lewen MD, Kempen JH, Mills MD. Uveitis reactivation in children treated with tumor necrosis factor alpha inhibitors. Am J Ophthalmol. 2015;160(1):193–200 e1. doi:10.1016/j.ajo.2015.04.016
18. Heiligenhaus A, Michels H, Schumacher C, et al. Evidence-based, interdisciplinary guidelines for anti-inflammatory treatment of uveitis associated with juvenile idiopathic arthritis. Rheumatol Int. 2012;32(5):1121–1133. doi:10.1007/s00296-011-2126-1
19. Angeles-Han ST, Ringold S, Beukelman T, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the screening, monitoring, and treatment of juvenile idiopathic arthritis-associated uveitis. Arthritis Rheumatol. 2019;71(6):864–877. doi:10.1002/art.40885
20. Bou R, Adan A, Borras F, et al. Clinical management algorithm of uveitis associated with juvenile idiopathic arthritis: interdisciplinary panel consensus. Rheumatol Int. 2015;35(5):777–785. doi:10.1007/s00296-015-3231-3
21. Thomas AS. Biologics for the treatment of noninfectious uveitis: current concepts and emerging therapeutics. Curr Opin Ophthalmol. 2019;30(3):138–150. doi:10.1097/ICU.0000000000000562
22. Doycheva D, Deuter C, Stuebiger N, Biester S, Zierhut M. Mycophenolate mofetil in the treatment of uveitis in children. Br J Ophthalmol. 2007;91(2):180–184. doi:10.1136/bjo.2006.094698
23. Goebel JC, Roesel M, Heinz C, Michels H, Ganser G, Heiligenhaus A. Azathioprine as a treatment option for uveitis in patients with juvenile idiopathic arthritis. Br J Ophthalmol. 2011;95(2):209–213. doi:10.1136/bjo.2009.173542
24. Kilmartin DJ, Forrester JV, Dick AD. Cyclosporin A therapy in refractory non-infectious childhood uveitis. Br J Ophthalmol. 1998;82(7):737–742. doi:10.1136/bjo.82.7.737
25. Yu EN, Meniconi ME, Tufail F, Baltatzis S, Foster CS, Christen WG. Outcomes of treatment with immunomodulatory therapy in patients with corticosteroid-resistant juvenile idiopathic arthritis-associated chronic iridocyclitis. Ocul Immunol Inflamm. 2005;13(5):353–360. doi:10.1080/09273940590951061
26. Smith JA, Thompson DJ, Whitcup SM, et al. A randomized, placebo-controlled, double-masked clinical trial of etanercept for the treatment of uveitis associated with juvenile idiopathic arthritis. Arthritis Rheum. 2005;53(1):18–23. doi:10.1002/art.20904
27. Ramanan AV, Dick AD, Benton D, et al. A randomised controlled trial of the clinical effectiveness, safety and cost-effectiveness of Adalimumab in combination with methotrexate for the treatment of juvenile idiopathic arthritis associated uveitis (SYCAMORE Trial). Trials. 2014;15:14. doi:10.1186/1745-6215-15-14
28. Simonini G, Druce K, Cimaz R, Macfarlane GJ, Jones GT. Current evidence of anti-tumor necrosis factor alpha treatment efficacy in childhood chronic uveitis: a systematic review and meta-analysis approach of individual drugs. Arthritis Care Res. 2014;66(7):1073–1084. doi:10.1002/acr.22214
29. Constantin T, Foeldvari I, Anton J, et al. Consensus-based recommendations for the management of uveitis associated with juvenile idiopathic arthritis: the SHARE initiative. Ann Rheum Dis. 2018;77(8):1107–1117. doi:10.1136/annrheumdis-2018-213131
30. Ramanan AV, Dick AD, Jones AP, et al. Adalimumab plus methotrexate for uveitis in juvenile idiopathic arthritis. N Engl J Med. 2017;376(17):1637–1646. doi:10.1056/NEJMoa1614160
31. Quartier P, Baptiste A, Despert V, et al. ADJUVITE: a double-blind, randomised, placebo-controlled trial of Adalimumab in early onset, chronic, juvenile idiopathic arthritis-associated anterior uveitis. Ann Rheum Dis. 2018;77(7):1003–1011. doi:10.1136/annrheumdis-2017-212089
32. Simonini G, Taddio A, Cattalini M, et al. Prevention of flare recurrences in childhood-refractory chronic uveitis: an open-label comparative study of Adalimumab versus infliximab. Arthritis Care Res. 2011;63(4):612–618. doi:10.1002/acr.20404
33. Cecchin V, Zannin ME, Ferrari D, et al. Longterm safety and efficacy of adalimumab and infliximab for uveitis associated with juvenile idiopathic arthritis. J Rheumatol. 2018;45(8):1167–1172. doi:10.3899/jrheum.171006
34. Zannin ME, Birolo C, Gerloni VM, et al. Safety and efficacy of infliximab and Adalimumab for refractory uveitis in juvenile idiopathic arthritis: 1-year followup data from the Italian Registry. J Rheumatol. 2013;40(1):74–79. doi:10.3899/jrheum.120583
35. Li Y, Mao X, Tang X, Mao H. Efficacy and safety of anti-TNFalpha therapy for uveitis associated with juvenile idiopathic arthritis: a systematic review and meta-analysis. Rheumatol Ther. 2021;8(2):711–727. doi:10.1007/s40744-021-00296-x
36. Verstegen RHJ, McMillan R, Feldman BM, Ito S, Laxer RM. Towards therapeutic drug monitoring of TNF inhibitors for children with juvenile idiopathic arthritis: a scoping review. Rheumatology. 2020;59(2):386–397. doi:10.1093/rheumatology/kez285
37. Wakefield D, Clarke D, McCluskey P. Recent developments in HLA B27 anterior uveitis. Front Immunol. 2020;11:608134. doi:10.3389/fimmu.2020.608134
38. Sepah YJ, Sadiq MA, Chu DS, et al. Primary (month-6) outcomes of the STOP-uveitis study: evaluating the safety, tolerability, and efficacy of tocilizumab in patients with noninfectious uveitis. Am J Ophthalmol. 2017;183:71–80. doi:10.1016/j.ajo.2017.08.019
39. Calvo-Rio V, Santos-Gomez M, Calvo I, et al. Anti-interleukin-6 receptor tocilizumab for severe juvenile idiopathic arthritis-associated uveitis refractory to anti-tumor necrosis factor therapy: a multicenter study of twenty-five patients. Arthritis Rheumatol. 2017;69(3):668–675. doi:10.1002/art.39940
40. Ramanan AV, Dick AD, Guly C, et al. Tocilizumab in patients with anti-TNF refractory juvenile idiopathic arthritis-associated uveitis (APTITUDE): a multicentre, single-arm, phase 2 trial. Lancet Rheumatol. 2020;2(3):e135–e141. doi:10.1016/S2665-9913(20)30008-4
41. Ruperto N, Lovell DJ, Quartier P, et al. Abatacept in children with juvenile idiopathic arthritis: a randomised, double-blind, placebo-controlled withdrawal trial. Lancet. 2008;372(9636):383–391. doi:10.1016/S0140-6736(08)60998-8
42. Angeles-Han S, Flynn T, Lehman T. Abatacept for refractory juvenile idiopathic arthritis-associated uveitis- a case report. J Rheumatol. 2008;35(9):1897–1898.
43. Kenawy N, Cleary G, Mewar D, Beare N, Chandna A, Pearce I. Abatacept: a potential therapy in refractory cases of juvenile idiopathic arthritis-associated uveitis. Graefes Arch Clin Exp Ophthalmol. 2011;249(2):297–300. doi:10.1007/s00417-010-1523-6
44. Zulian F, Balzarin M, Falcini F, et al. Abatacept for severe anti-tumor necrosis factor alpha refractory juvenile idiopathic arthritis-related uveitis. Arthritis Care Res. 2010;62(6):821–825. doi:10.1002/acr.20115
45. Heiligenhaus A, Miserocchi E, Heinz C, Gerloni V, Kotaniemi K. Treatment of severe uveitis associated with juvenile idiopathic arthritis with anti-CD20 monoclonal antibody (rituximab). Rheumatology. 2011;50(8):1390–1394. doi:10.1093/rheumatology/ker107
46. Smolen JS, Landewe R, Bijlsma J, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann Rheum Dis. 2017;76(6):960–977. doi:10.1136/annrheumdis-2016-210715
47. Baker KF, Isaacs JD. Novel therapies for immune-mediated inflammatory diseases: what can we learn from their use in rheumatoid arthritis, spondyloarthritis, systemic lupus erythematosus, psoriasis, Crohn’s disease and ulcerative colitis? Ann Rheum Dis. 2018;77(2):175–187. doi:10.1136/annrheumdis-2017-211555
48. Schwartz DM, Kanno Y, Villarino A, Ward M, Gadina M, O’Shea JJ. JAK inhibition as a therapeutic strategy for immune and inflammatory diseases. Nat Rev Drug Discov. 2017;17(1):78. doi:10.1038/nrd.2017.267
49. Sen ES, Ramanan AV. Juvenile idiopathic arthritis-associated uveitis. Clin Immunol. 2020;211:108322. doi:10.1016/j.clim.2019.108322
50. Bing SJ, Lyu C, Xu B, et al. Tofacitinib inhibits the development of experimental autoimmune uveitis and reduces the proportions of Th1 but not of Th17 cells. Mol Vis. 2020;26:641–651.
51. Bauermann P, Heiligenhaus A, Heinz C. Effect of janus kinase inhibitor treatment on anterior uveitis and associated macular edema in an adult patient with juvenile idiopathic arthritis. Ocul Immunol Inflamm. 2019;27(8):1232–1234. doi:10.1080/09273948.2019.1605453
52. Dipasquale V, Atteritano M, Fresta J, Castagna I, Conti G. Tocilizumab for refractory uveitis associated with juvenile idiopathic arthritis: a report of two cases. J Clin Pharm Ther. 2019;44(3):482–485. doi:10.1111/jcpt.12821
53. Paley MA, Karacal H, Rao PK, Margolis TP, Miner JJ. Tofacitinib for refractory uveitis and scleritis. Am J Ophthalmol Case Rep. 2019;13:53–55. doi:10.1016/j.ajoc.2018.12.001
54. Tappeiner C, Mesquida M, Adan A, et al. Evidence for tocilizumab as a treatment option in refractory uveitis associated with juvenile idiopathic arthritis. J Rheumatol. 2016;43(12):2183–2188. doi:10.3899/jrheum.160231
55. Miserocchi E, Giuffre C, Cornalba M, Pontikaki I, Cimaz R. JAK inhibitors in refractory juvenile idiopathic arthritis-associated uveitis. Clin Rheumatol. 2020;39(3):847–851. doi:10.1007/s10067-019-04875-w
56. Ramanan AV, Guly CM, Keller SY, et al. Clinical effectiveness and safety of baricitinib for the treatment of juvenile idiopathic arthritis-associated uveitis or chronic anterior antinuclear antibody-positive uveitis: study protocol for an open-label, Adalimumab active-controlled phase 3 clinical trial (JUVE-BRIGHT). Trials. 2021;22(1):689. doi:10.1186/s13063-021-05651-5
57. Clarke B, Yates M, Adas M, Bechman K, Galloway J. The safety of JAK-1 inhibitors. Rheumatology. 2021;60(Suppl 2):ii24–ii30. doi:10.1093/rheumatology/keaa895
58. Winthrop KL. The emerging safety profile of JAK inhibitors in rheumatic disease. Nat Rev Rheumatol. 2017;13(5):320. doi:10.1038/nrrheum.2017.51
59. Del Giudice E, Simio C, Scala A, et al. Juvenile idiopathic arthritis-associated uveitis in the era of biological therapy: how the disease changed in more than 20 years of observation in a tertiary referral center in Rome (Italy). Int Ophthalmol. 2022;42(3):775–784. doi:10.1007/s10792-021-02043-1
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
