Back to Journals » International Journal of General Medicine » Volume 13
Management of Hepatitis B Surface Antigen and Hepatitis C Antibody-Positive Patients by Departments Not Specializing in Hepatology at a Suburban University Hospital in Japan: A Single-Center Observational Study
Authors Tokushima Y, Tago M , Tokushima M, Katsuki NE , Iwane S, Eguchi Y, Yamashita S
Received 24 June 2020
Accepted for publication 27 August 2020
Published 1 October 2020 Volume 2020:13 Pages 743—750
DOI https://doi.org/10.2147/IJGM.S268857
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Yoshinori Tokushima, 1,* Masaki Tago, 1,* Midori Tokushima, 1 Naoko E Katsuki, 1 Shinji Iwane, 2 Yuichiro Eguchi, 3 Shu-ichi Yamashita 1
1Department of General Medicine, Saga University Hospital, Saga, Japan; 2Fujioka Hospital, Saga, Japan; 3Eguchi Hospital, Saga, Japan
*These authors contributed equally to this work
Correspondence: Masaki Tago
Department of General Medicine, Saga University Hospital, 5-1-1 Nabeshima, Saga 849-8501, Japan
Tel +81 952 34 3238
Fax +81 952 34 2029
Email [email protected]
Objective: To investigate effects of an altered medical environment between 2010 and 2015 on viral hepatitis treatment behaviors of doctors who were not hepatology specialists.
Methods: Charts of patients who were identified as hepatitis B surface antigen (HBs-Ag)-positive or hepatitis C virus antibody (HCV-Ab)-positive by university hospital departments not specializing in hepatology from January to December 2015 were retrospectively reviewed. Patients were assigned to a “referred” group or a “non-referred” group based on whether they were subsequently referred to the Hepatology Department. Age, sex, type of department visited (one of various internal medicine departments, or a different department), and blood test results were compared in the two groups.
Results: Among 7,824 patients screened for HBs-Ag, 82 were positive. Twenty-nine (35.4%) had subsequently been referred to the Hepatology Department, which was higher than the 2010 referral rate (20.6%). In multivariate analysis, patients in the referred group were significantly more likely to have visited one of various internal medicine departments, and they had higher levels of platelet count and γ-glutamyl transpeptidase. Among 7,778 patients screened for HCV-Ab, 279 were positive. Only 33 (11.8%) had subsequently been referred to the Hepatology Department, which was lower than the 2010 referral rate (18.7%). In multivariate analysis, patients in the referred group were significantly more likely to have visited an internal medicine department.
Conclusion: HCV-antibody-positive patients screened by departments not specializing in hepatology were not managed adequately in 2015. This suggests a need for education of doctors not specializing in hepatology, particularly those not working in internal medicine departments.
Keywords: hepatitis B virus, hepatitis C virus, hepatitis B, hepatitis C, referral, department
Corrigendum for this paper has been published
Introduction
In 2018 the number of newly diagnosed cases of hepatocellular carcinoma (HCC) was reportedly 781,631 and the annual all-cause mortality associated with it was 841,080, equating to a projected mortality rate as high as 0.93.1 HCC is reportedly the fourth highest cause of death due to malignant neoplasms in the world,2 and the fifth most common cause of death in Japan.3 Although non-B, non-C hepatitis has gradually been increasing as a cause of HCC, hepatitis B virus (HBV) and hepatitis C virus (HCV) still account for approximately 80% of cases,4 rendering detection of infection with either of these viruses crucial for preventing the development of HCC.
Evidently, the earlier HCC is detected the better its prognosis tends to be,5 which also applies to chronic HCV infection.6 Although the complications and prognoses of HBV and HCV patients with chronic hepatitis are diverse due to variation in their baseline diseases, patients diagnosed by gastroenterology or hepatology specialists are reportedly more likely to receive appropriate treatment than those diagnosed by other practitioners.7 Therefore, when HBV or HCV is incidentally detected by a doctor who is not a specialist in hepatology, referring them to a relevant specialist as early as possible for the instigation of optimal cooperative treatment is essential.8 Regrettably, in a previous study, we in 2010 at a university hospital 79% of patients diagnosed with hepatitis B surface antigen (HBs-Ag) and 82% diagnosed with HCV anti-body (HCV-Ab) ≥ 4.0 S/CO were not referred to hepatologists.9
By 2015 the treatment of viral hepatitis had changed significantly from that in 2010, with the advent of new anti-HBV and HCV drugs that evidently markedly improve prognoses.10,11 Highly efficacious anti-HCV medications that were suitable for use in patients with chronic HCV hepatitis had become available, including patients who had previously been considered inappropriate candidates because they were refractory to treatment with interferon, had liver cirrhosis or another preclusive complication, or were of advanced age.10 In Japan, new treatment guidelines for hepatitis C and hepatitis B were published in 2012 and 2013, respectively.10,11 Meanwhile, in other countries, the American Association for the Study of Liver Diseases (AASLD) produced a guideline for chronic hepatitis B in 2007,12 and worked with the Infectious Diseases Society of America (IDSA) to produce a guideline for chronic hepatitis C in 2014,13 which have been appropriately revised and updated. The indications for antiviral treatment in chronic hepatitis B without liver fibrosis in the 2013 Japanese guideline were ALT ≥ 31 U/L and HBV DNA ≥ 4 log copies/mL, which were wider than those in the 2009 AASLD guideline, ALT ≥ twice the normal limit and HBV DNA ≥ 5 log copies/mL.11,12 Similarly, the indications for treatment of chronic hepatitis in the 2012 Japanese guideline, which were applied to all patients with hepatitis C, were wider than those in the 2014 AASLD guideline, requiring the consideration of comorbidities and degree of liver fibrosis.10,14 Nevertheless, observing any of these guidelines would improve the referral rate to hepatologists, because the types and timings for introduction of antiviral medicines and response rates are almost equivalent in all of the guidelines.10–15 In Japan, the public subsidy system for treatment of hepatitis B or C with interferon began in 2008. Although HBs-Ag-positive or HCV-Ab-positive patients had to seek permission for treatment from the municipal government, all applications were usually approved. Once approved, most medical expenses for treatment of hepatitis were exempted except for negligible amounts of self-payment, which were further reduced in 2010. Furthermore, when new medicines were developed, the rules of the subsidy system were changed to include them in the system.16 Collectively these developments mentioned above should have functioned to substantially increase the rates of referral of newly diagnosed HBV and HCV patients to hepatologists.
In the current study, the management of patients diagnosed with HBs-Ag or medium to higher-titer HCV-Ab detected by non-hepatologists at the same aforementioned suburban university hospital in Japan in 2015 was investigated, and the results were compared with those acquired in 2010.9
Methods
The records of both in-patients and out-patients whose HBs-Ag and HCV-Ab status were assessed by a non-hepatologist at Saga University Hospital in suburban Saga in the southern part of Japan from January to December 2015 were retrospectively reviewed. The prevalences of HBs-Ag-positive patients and presumptive HCV carriers were reported to be higher in Saga prefecture than in Japan. According to data from a nationwide health checkup of Japanese people, the prevalences of HBs-Ag-positive patients were 0.7% in Japan and 1.2% in Saga prefecture, and those of presumptive HCV carriers were 0.4% in Japan and 0.9% in Saga prefecture.17 In addition, we have shown the prevalence of HBs-Ag-positive patients according to age in Japan in S1 Table, and the prevalences of presumptive HCV carriers according to age in both Saga prefecture and Japan in S1 and S2 Tables.17,18
HBs-Ag positivity was defined as ≥0.05 IU/mL. HCV-Ab positivity was defined as ≥1.0 S/CO, but titers were further divided into three categories—low (≥1.0, <4.0 S/CO), medium (≥4.0, <12.0 S/CO), and high (≥12.0 S/CO)19—and only patients in the medium and high groups were considered positive for the purposes of subsequent analyses. This was in accordance with our aforementioned previous study conducted at the same hospital,9 and the rationale is that HCV-Ab titers <4.0 are reportedly associated with an HCV-RNA positivity rate of almost 0%.19 In patients in whom multiple HBs-Ag and/or HCV-Ab tests had been performed during the study period, only the first test of each type was included. Tests performed in patients who were regularly seen by the Hepatology Department were excluded, even if they had been assessed by a non-hepatologist at some point during the study period. The data obtained from medical records included age, sex, whether or not the patient had visited any one of a number of different internal medicine departments, platelet count (PLT), and levels of aspartate aminotransferase (AST), alanine aminotransferase (ALT), and γ-glutamyl transpeptidase (γ-GTP).
In addition to the Hepatology Department, the Departments of General Medicine, Gastroenterology, Cardiology, Nephrology, Respiratory Diseases, Rheumatology, Hematology and Oncology, Neurology, and the Division of Infectious Disease/Control and Prevention were defined as internal medicine departments. The Departments of General and Gastrointestinal Surgery, Cardiovascular Surgery, General Thoracic Surgery, Neurosurgery, Orthopedic Surgery, Plastic and Reconstructive Surgery, Ophthalmology, Otolaryngology—Head and Neck Surgery, Gynecology and Obstetrics, Urology, Dermatology, Dentistry and Oral Surgery, Neuropsychiatry, Pediatrics, Anesthesiology and Critical Care Medicine, Emergency Medicine, and Radiology were defined as non-internal medicine departments. The department to which the doctor who had ordered the HBs-Ag or HCV-Ab test belonged to was defined as the department associated with the test. If a doctor from one department where a patient was seen sought a consultation about that patient with a doctor from another department and that second doctor subsequently ordered the test, the latter department was regarded as the department associated with the test.
Patients were assigned to a “referred” (RF) group or a “non-referred” (non-RF) group based on whether they had been referred to the Hepatology Department after being identified as HBs-Ag-positive or HCV-Ab-positive with medium or high titer. Throughout the period of the current study (2015), whether patients were referred to the Hepatology Department was at the sole discretion of the doctor in charge of the patient, and there was no mechanism incorporated into the electronic chart system designed to call the doctor’s attention to the patient’s HBs-Ag or HCV-Ab positivity.
In Japan, all citizens and most foreign residents are covered by some sort of public health insurance, which makes it possible for people to see doctors at any medical institutions as many times as they like. Although many higher medical institutions that provide advanced treatments, such as university hospitals, require a referral letter, patients can still see a doctor they like if they pay a non-expensive amount of extra fee. Furthermore, a referral letter is not mandatory to see specialists belonging to hospitals other than higher medical institutions. There are also no strict regulations concerning which doctors should write referral letters. Once a doctor has seen a patient, they can write a referral letter for the patient to any kind of specialist. However, in our hospital, doctors belonging to departments other than the Hepatology Department are usually required to write a referral letter for the patient’s electronic medical records, which are commonly used by all departments, while making a reservation at the outpatient clinic of the Hepatology Department.
In univariate analyses, continuous variables (age, PLT, AST, ALT, γ-GTP, HBs-Ag, and HCV-Ab) were compared between the RF and non-RF groups by a t-test, and categorical variables (sex and internal medicine department) were compared by the chi-square test. In a subsequent multivariate analysis, binomial variables (categorical variables) and continuous variables with values of p < 0.15 in univariate analyses were assessed using a forced-entry logistic model. IBM SPSS version 23 was used to conduct statistical analyses. p < 0.05 was deemed to indicate statistical significance.
The non-RF group was further subdivided into four groups (group 1 in non-RF to group 4 in non-RF) based on descriptions of patients’ viral hepatitis derived from all the relevant medical records, including text that doctors had written, referral letters to other hospitals written when patients were discharged from our hospital, or templates in which all the medical personnel wrote, e.g., those for obtaining informed consent from patients or their family members. In the group 1 in non-RF the doctor had recorded at least one of the following in the history, without writing anything in the problem list: “Diagnosis of chronic hepatitis caused by HBV”, “Diagnosis of chronic hepatitis caused by HCV”, “HBs-Ag-positive”, or “HCV-Ab-positive with moderate to high titer”. In the group 2 in non-RF the doctor had recorded at least one of the items in the problem list, without referring any further therapeutic strategies. In the group 3 in non-RF the doctor had recorded at least one of the items in the problem list, and had also referred to further therapeutic strategies at our hospital or the names of other hospitals at which the patient was subsequently going to be seen. In the group 4 in non-RF, the doctor had recorded nothing at all pertaining to any of the four issues.
The present study was conducted in accordance with the Declaration of Helsinki, and it was approved by the Ethics Committee of Saga University Hospital (approval ID 2017–09-jinsoku-03). We obtained consent from all patients by a comprehensive agreement method in the hospital, and anonymity of patients was protected.
Results
HBs-Ag-Positive Patients
A total of 7,824 patients were screened for HBs-Ag, of whom 151 tested positive. Of these patients, 82 fulfilled the above-described inclusion criteria. The background characteristics of the patients are shown in Table 1. The mean age ± standard deviation was 62.1 ± 17.7 years, 36 were male (43.9%), and 16 (19.5%) were detected by an internal medicine department. The five departments that ordered the highest numbers of tests were orthopedic surgery (1,241), emergency medicine (849), ophthalmology (659), gynecology and obstetrics (507), and general and gastrointestinal surgery (487). The five departments with the highest numbers of HBs-Ag-positive patients were emergency medicine (13, RF 31%), orthopedic surgery (12, RF 31%), general and gastrointestinal surgery (12, RF 25%), otolaryngology—head and neck surgery (8, RF 63%), and ophthalmology (7, RF 0%). A total of 29 of the 82 patients (35.4%) were subsequently referred to the Hepatology Department. In the univariate analyses, patients who were subsequently referred to the Hepatology Department had a higher proportion of initially being seen by an internal medicine department (odds ratio [OR] 8.6, 95% confidence interval [CI] 2.5–30.5, p = 0.001), and had a higher platelet count than non-RF patients. In the multivariate analysis including type of department visited, age, platelet count, and γ-GTP as covariates, patients who were subsequently referred to the Hepatology Department were significantly more likely to have initially been seen by an internal medicine department (OR 14.8, 95% CI 3.2–68.0, p = 0.001), have a higher platelet count (OR 1.1, 95% CI 1.0–1.2, p = 0.012), and have a higher γ-GTP level (OR 1.0, 95% CI 1.0–1.0, p = 0.034) (Table 2). The rate of referral to the Hepatology Department was 35.4%, which was significantly higher than the 2010 rate of 20.6% (chi-square test, OR 2.1, 95% CI 1.1–3.9, p = 0.024).9 The distribution of patients in the non-RF subgroups was group 1 in non-RF 8 patients (15%), group 2 in non-RF 12 patients (23%), group 3 in non-RF 9 patients (17%), and group 4 in non-RF 24 patients (45%) (Table 3).
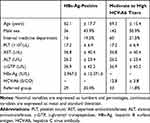 |
Table 1 Characteristics of Hepatitis B Surface Antigen-Positive Patients and with Moderate to High Titers of Hepatitis C Virus Antibodies |
 |
Table 2 Univariate and Multivariate Analyses of Results Derived from Hepatitis B Surface Antigen-Positive Patients |
 |
Table 3 Details Contained in the Medical Charts of Patients Who Were Not Referred to the Hepatology Department |
HCV-Ab-Positive Patients with Medium or High Titers
A total of 7,778 patients were screened for HCV-Ab, of whom 507 tested positive. Of those, 279 had medium or high titers and were thus included in subsequent analysis. The background characteristics of the patients are shown in Table 1. The mean age ± standard deviation was 69.3 ± 15.4 years, 142 were male (50.9%), and 60 (21.5%) were detected by an internal medicine department. The five departments that ordered the highest numbers of tests were orthopedic surgery (1,229), emergency medicine (854), ophthalmology (663), gynecology and obstetrics (507), and general and gastrointestinal surgery (487). The five departments with the highest numbers of HCV-Ab-positive patients with medium or high titers were orthopedic surgery (53, RF 7.5%), emergency medicine (41, RF 17%), ophthalmology (21, RF 0%), general and gastrointestinal surgery (17, RF 5.9%), and gastroenterology (17, RF 0%). A total of 33 of the 279 patients (11.8%) were subsequently referred to the Hepatology Department. In univariate analyses, a higher proportion of patients who were subsequently referred to the Hepatology Department were initially seen by an internal medicine department (OR 2.4, CI 1.1–5.1, p = 0.040). In the multivariate analysis including type of department visited, ALT, and γ-GTP as covariates, patients who were subsequently referred to the Hepatology Department were significantly more likely to have initially been seen by an internal medicine department (OR 2.7, 95% CI 1.2–6.0, p = 0.016) (Table 4). The rate of referral to the Hepatology Department was 11.8%, which was significantly lower than the 2010 rate of 18.7% (chi-square test, OR 0.6, 95% CI 0.39–0.95, p = 0.028).9 The distribution of patients in the non-RF subgroups was group 1 in non-RF 48 patients (20%), group 2 in non-RF 33 patients (13%), group 3 in non-RF 85 patients (35%), and group 4 in non-RF 80 patients (33%) (Table 3). The results of the analyses using the same method as our previous study, in which the continuous variables were classified into binomial variables, are shown in S3 and S4 Tables with a description of the statistical method.
 |
Table 4 Univariate and Multivariate Analyses in Patients with Moderate and High Titers of Hepatitis C Virus Antibody |
Discussion
The rate of referral to the Hepatology Department in patients identified as HBs-Ag-positive by non-hepatology departments increased significantly from 2010 (20.6%) to 2015 (35.4%).9 We had expected an increase due to increased awareness of de novo hepatitis B among doctors who were not hepatology specialists—especially those treating patients with malignancies or immune-mediated diseases—and new hepatitis B treatment guidelines published by the Japan Society of Hepatology recommending immediate referral to a hepatology specialist following an HBs-Ag-positive test.11 These facts may have contributed to the increased detection of HBs-Ag-positive patients and increased rates of referral to hepatology specialists by the Department of Otolaryngology—Head and Neck Surgery (63%). That department specializes in and treats large numbers of patients with malignant tumors in the head and neck area, and is frequently involved in anti-cancer chemotherapy before and after surgeries. We surmise that the above-described increased detection and referral rates reflect increased HBs-Ag testing of patients in order to prevent the development of de novo hepatitis B, rather than to prevent transmission to surgeons.
In contrast to HBs-Ag, the rate of referral of patients identified with medium to high HCV-Ab titers to a hepatologist decreased significantly from 2010 (18.7%) to 2015 (11.8%).9 Notably the proportion of patients in the group 3 in non-RF —in which further therapeutic strategies were described in medical charts by non-hepatologists after HCV-Ab testing—increased from 3% in 2010 to 35% in 2015.9 The Japanese Ministry of Health, Labor and Welfare reported that approximately 19,000 patients had received national subsidies within 2010 to 2015 for chronic hepatitis C treatment,16 suggesting the possible presence of larger numbers of patients who had already been treated and were in a state of sustained virologic response (SVR) in the group 3 in non-RF in 2015 than in 2010. It may be that the risk of HCC development in patients in a state of SVR was considered relatively low by non-hepatologists, and this may have prevented them from referring such patients to a hepatologist.20,21 In addition to the above-mentioned reasons, another reason for the lower rate of referral of patients with HCV-Ab positivity was considered to be the presence of physicians who did not have adequate knowledge of the treatments and side effects of antiviral medications.22 Before 2010, the duration of our previous study, interferon therapy was the mainstay of treatment for hepatitis C, but had a low response rate of only 50% with high incidence of strong side effects, thus limiting the indications for such therapy.10 Because the present study was conducted in 2015, shortly after the release of new medicines with improved response rates and lower incidences of side effects, the information on such medications was not spread among physicians in non-specialist departments, resulting in a lower rate of referral.22
Notably, negative HCV-RNA results were recorded in some patients’ records as the reason why the doctor had not referred the patient to a hepatologist. However, a state of SVR does not equate to being free of the risk of HCC development, and rates of 2.3–8.8% per 5 years, and 3.1–11.1% per 10 years have been reported.23 Furthermore, in one retrospective cohort study the 5-year survival rate in patients who had achieved SVR status and had undergone abdominal ultrasonographic cancer screening every 6 months was 93%, but it was only 60% in those who had not undergone regular screening.24 Based on the above-described observations and reports, we emphasize that patients identified as HCV-Ab positive with medium or high titers should be followed up via regular imaging, even if they are in a state of SVR. Regular abdominal ultrasonography may also clarify the ongoing efficacy of the therapeutic strategies being administered to the patient.
The guidelines for treating hepatitis B and C have been revised frequently due to rapid developments in treatments, particularly those pertaining to new drugs.10,11 This has rendered it comparatively difficult for non-hepatologists to remain abreast of all relevant advances in hepatitis treatments, and instigate optimal treatments unassisted.25 Unsurprisingly, patients with viral hepatitis who are diagnosed by hepatologists reportedly tend to receive more effective pharmacotherapies than those diagnosed by doctors who are not hepatologists.7 Furthermore, general internal medicine doctors evidently failed to prescribe appropriate treatments to approximately half of the patients who were potential candidates for anti-viral medications.7 Thus, we truly cannot emphasize the importance of cooperative and coordinated treatment between hepatologists and non-hepatologists enough.8
In HBs-Ag-positive patients and patients with moderate to high HCV-Ab titers the proportions subsequently referred to hepatologists were much higher in those who were initially diagnosed by doctors working in internal medicine departments. This was also the case at the same hospital in 2010.9 With regard to HBs-Ag-positive patients, the referral rates by the Department of Orthopedic Surgery and the Department of Ophthalmology to the Hepatology Department were especially low, despite the high rates at which those departments encountered such patients; which had not changed significantly since 2010.9 These low rates of referral to the Hepatology Department may have been caused by the fact that patient hepatitis virus screening tests prior to surgery were traditionally performed in order to prevent transmission to medical staff,26 which would render referral to the Hepatology Department or consideration of indications for anti-viral treatments unlikely. In one report discussions about treatment strategies for their viral hepatitis were only conducted with half of the patients who tested positive in tests ordered by doctors specializing in fields other than hepatology, gastroenterology, or internal medicine.7 That same report suggests that some patients who tested positive when screened in conjunction with an emergency room visit or in preoperative examinations were not even informed of their positive results.7
An alert mechanism incorporated into electrical medical chart systems that informs doctors who are not hepatologists about the necessity of subsequent examinations and treatments in patients who tested positive for HBs-Ag or HCV-Ab may improve referral rates.27,28 Introducing such a system may be expensive, and the resulting benefits associated with doing so may differ depending on the quality of it and the extent to which it operates, including the way it displays notifications and/or identifies relevant patients.27–29 Such an alert system was introduced into the electronic medical chart network at our hospital in December 2019, which now notifies doctors of patients who require follow-up by hepatologists. The system automatically prints out the results of screening examinations in conjunction with a hard-copy document that doctors fill in. Therein the doctor documents the patient’s condition, and lists medical institutions that have past records of regular follow-ups of patients with viral hepatitis or treatments with anti-viral medications covered by national subsidies. Other than an alert mechanism, assignment of physicians who are dedicated to checking all results for HBV-Ag and HCV-Ab tests and referring positive patients to the Department of Hepatology, or to holding regular training workshops for physicians who are not hepatologists, could improve the referral rate. However, the effectiveness of these methods remains to be proved, and thus further studies are warranted.
The present study had several limitations. The disparities in the background characteristics of the target populations between the studies conducted in 2010 and 2015 could have affected the differences in the referral rates. With regard to HCV-Ab, we only included patients with medium to high titers in the analysis, and rates of referral to hepatologists would be different if patients with low HCV-Ab titers were included. In addition, the actual rates of patients with HBs-Ag positivity or HCV-Ab with moderate to high titers who were appropriately treated could have been higher than the referral rate shown in this study, because of the possible presence of patients referred to hepatologists without a referral letter, patients who had already been treated at another hospital before screening, and patients who were treated appropriately by the department that performed the screening, in the “non-referred” group.
Conclusions
The proportion of HBs-Ag-positive patients screened by other departments that were subsequently referred to the Hepatology Department in 2015 was greater than the corresponding proportion in 2010 at the same suburban hospital in Japan. Conversely, the opposite was the case with regard to patients diagnosed with medium or higher titers of HCV-Ab. Patients with chronic hepatitis C thus may not have received the full benefits of improved viral hepatitis diagnosis and treatment modalities, and relatively recent changes in the national subsidies system in Japan within 2010 to 2015. These considerations suggest that enlightenment of doctors who are not specialists in hepatology, especially those who are also not specialized in internal medicine, will yield substantial health benefits.
Acknowledgment
We thank Dr. Owen Proudfoot from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Global Cancer Observatory. Cancer tomorrow. International agency for research on cancer; 2018. Available from: https://gco.iarc.fr/tomorrow/home.
2. Akinyemiju T, Abera S, Ahmed M, et al. The burden of primary liver cancer and underlying etiologies from 1990 to 2015 at the global, regional, and national level: results from the Global Burden of Disease Study 2015. JAMA Oncol. 2017;3(12):1683–1691. doi:10.1001/jamaoncol.2017.3055
3. Cancer Registry and Statistics. Cancer Information service, national cancer center, Japan (vital statistics of Japan). Available from: https://ganjoho.jp/reg_stat/statistics/dl/index.html#mortality.
4. The Japan Society of Hepatology: Kangan hakusho. 2015. Available from: https://www.jsh.or.jp/files/uploads/Liver%20Cancer%202015.pdf.
5. Oeda S, Iwane S, Takasaki M, et al. Optimal follow-up of patients with viral hepatitis improves the detection of early-stage hepatocellular carcinoma and the prognosis of survival. Intern Med. 2016;55(19):2749–2758. doi:10.2169/internalmedicine.55.6730
6. Moorman AC, Xing J, Ko S, et al. Late diagnosis of hepatitis C virus infection in the Chronic Hepatitis Cohort Study (CHeCS): missed opportunities for intervention. Hepatology. 2015;61(5):1479–1484. doi:10.1002/hep.27365
7. Rocca LG, Yawn BP, Wollan P, Kim WR. Management of patients with hepatitis C in a community population: diagnosis, discussions, and decisions to treat. Ann Fam Med. 2004;2(2):116–124. doi:10.1370/afm.62
8. Volk ML. Antiviral therapy for hepatitis C: why are so few patients being treated? J Antimicrob Chemother. 2010;65(7):1327–1329. doi:10.1093/jac/dkq157
9. Furukawa EN, Kawaguchi Y, Oeda S, et al. Current management practices for HBs antigen or anti-HCV antibody positive individuals in non-hepatology departments at a university hospital. Kanzo. 2013;54(5):307–316. doi:10.2957/kanzo.54.307
10. The Japan Society of Hepatology. Drafting committee for hepatitis management guidelines: guidelines for the treatment of hepatitis C (7th edition). Japanese. Available from: https://www.jsh.or.jp/medical/guidelines/jsh_guidlines/hepatitis_c.
11. The Japan Society of Hepatology. Drafting committee for hepatitis management guidelines: guidelines for the treatment of hepatitis B (3.2 edition). Japanese. Available from: https://www.jsh.or.jp/medical/guidelines/jsh_guidlines/hepatitis_b.
12. Lok AS, McMahon BJ. Chronic hepatitis B: update 2009. Hepatology. 2009;50(3):661–662. doi:10.1002/hep.23190
13. Ghany MG, Morgan TR. AASLD-IDSA hepatitis C guidance panel. Hepatitis C guidance 2019 update: American association for the study of liver diseases-infectious diseases society of America recommendations for testing, managing, and treating hepatitis C virus infection. Hepatology. 2020;71(2):686–721. doi:10.1002/hep.31060
14. AASLD/IDSA HCV Guidance Panel. Hepatitis C guidance: AASLD-IDSA recommendations for testing, managing, and treating adults infected with hepatitis C virus. Hepatology. 2015;62(3):932–954. doi:10.1002/hep.27950
15. World Gastroenterology Organization Global Guidelines. Diagnosis, management, and prevention of hepatitis C. Available from: https://www.worldgastroenterology.org/guidelines/global-guidelines/hepatitis-c/hepatitis-c-english.
16. Ministry of Health, Labour and Welfare. Information examination medical treatment enlightenment: medical expenses subsidy for hepatitis treatment (interferon treatment, interferon-free treatment, nucleic acid analog treatment). Japanese. Available from: https://www.mhlw.go.jp/bunya/kenkou/kekkaku-kansenshou09/080328_josei.html.
17. Ministry of Health, Labour and Welfare. Information examination medical treatment enlightenment: results of hepatitis virus screening and other events as part of the 2015 health promotion program. Japanese. Available from: https://www.mhlw.go.jp/bunya/kenkou/kekkaku-kansenshou09/pdf/kensa-17.pdf.
18. Isoda H, Oeda S, Takamori A, et al. Generation gap for screening and treatment of hepatitis C virus in Saga prefecture, Japan: an administrative database study of 35,625 subjects. Intern Med. 2020;59(2):169–174. doi:10.2169/internalmedicine.3248-19
19. Nakayama M, Morita Y, Ogata H, et al. Verification study of anti-HCV assay on the japanese health check program -from the experience of liver disease health check program at Saga Prefecture-. Igakukennsa. 2005;54(9):1194–1199.
20. Morgan RL, Baack B, Smith BD, Yartel A, Pitasi M, Falck-Ytter Y. Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma: a meta-analysis of observational studies. Ann Intern Med. 2013;158(5 Pt 1):329–337. doi:10.7326/0003-4819-158-5-201303050-00005
21. Li DK, Ren Y, Fierer DS, et al. The short-term incidence of hepatocellular carcinoma is not increased after hepatitis C treatment with direct-acting antivirals: an ERCHIVES study. Hepatology. 2018;67(6):2244–2253. doi:10.1002/hep.29707
22. McGowan CE, Monis A, Bacon BR, et al. A global view of hepatitis C: physician knowledge, opinions, and perceived barriers to care. Hepatology. 2013;57(4):1325–1332. doi:10.1002/hep.26246
23. Hiramatsu N, Oze T, Takehara T. Suppression of hepatocellular carcinoma development in hepatitis C patients given interferon-based antiviral therapy. Hepatol Res. 2015;45(2):152–161. doi:10.1111/hepr.12393
24. Yamashita N, Ohho A, Yamasaki A, Kurokawa M, Kotoh K, Kajiwara E. Hepatocarcinogenesis in chronic hepatitis C patients achieving a sustained virological response to interferon: significance of lifelong periodic cancer screening for improving outcomes. J Gastroenterol. 2014;49(11):1504–1513. doi:10.1007/s00535-013-0921-z
25. Thomson M, Konerman MA, Choxi H, Lok AS. Primary care physician perspectives on hepatitis C management in the era of direct-acting antiviral therapy. Dig Dis Sci. 2016;61(12):3460–3468. doi:10.1007/s10620-016-4097-2
26. Ahmed R, Bhattacharya S. Universal screening versus universal precautions in the context of preoperative screening for HIV, HBV, HCV in India. Indian J Med Microbiol. 2013;31(3):219–225. doi:10.4103/0255-0857.115623
27. Fujii H, Yamaguchi S, Kurai O, et al. Putting “sticky notes” on the electronic medical record to promote intra-hospital referral of hepatitis B and C virus-positive patients to hepatology specialists: an exploratory study. BMC Infect Dis. 2016;16:410. doi:10.1186/s12879-016-1765-y
28. Yoshioka N, Okumura A, Yamamoto Y, et al. Promoting notification and linkage of HBs antigen and anti-HCV antibody-positive patients through hospital alert system. BMC Infect Dis. 2017;17(1):330. doi:10.1186/s12879-017-2438-1
29. Shimomura Y, Fujii Y, Ikeda F, et al. Sufficient management of alert system of positive test results for HBV and HCV infection in electronic medical chart for facilitating hepatological consultation. Kanzo. 2017;58(8):427–434. doi:10.2957/kanzo.58.427
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
