Back to Journals » International Medical Case Reports Journal » Volume 14
Management of Free-Floating Thrombus in the Vertebral Artery in a Middle-Aged Smoker with Secondary Polycythemia Vera
Authors Alhashim A, Hadhiah K , Itani SA, Alshurem M , Alabdali M, Aljaafari D, AlQarni M
Received 16 June 2021
Accepted for publication 3 September 2021
Published 22 September 2021 Volume 2021:14 Pages 663—668
DOI https://doi.org/10.2147/IMCRJ.S325133
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas
Ali Alhashim,1 Kawther Hadhiah,1 Sarah A Itani,2 Mohammed Alshurem,1 Majed Alabdali,1 Danah Aljaafari,1 Mustafa AlQarni1
1Neurology Department, College of Medicine, Imam Abdulrahman Bin Faisal University, Dammam, 34212, Saudi Arabia; 2College of Medicine, Imam Abdulrahman Bin Faisal University, Dammam, 34212, Saudi Arabia
Correspondence: Ali Alhashim
Neurology Department, College of Medicine, Imam Abdulrahman Bin Faisal University, Dammam, 34212, Saudi Arabia
Tel +966 509444833
Email [email protected]; [email protected]
Abstract: Free-floating thrombus (FFT) of the cervicocranial arteries is a rare neurovascular condition. Up to now, there is no standardized definition for FFT. Therefore, FFT is occasionally mistaken for intraluminal thrombus (ILT) or smooth mural thrombus. The most precise and ideal definition of FFT would be a long-extended intraarterial thrombus that is attached to the arterial wall with its one end, while its other end is surrounded by blood flow and moves freely with the cardiac cycle. FFT usually manifests as an ischemic stroke, thus it is considered as an emergency case. Herein, we report a rare case of symptomatic FFT in the left vertebral artery extending from V0 to V2 segments in a middle-aged smoker, who presented with multiple embolic strokes in different territories of posterior circulation and was successfully treated medically. This case sheds light on the challenges of the clinical approach of FFT in the vertebral artery and it is an attempt to draw attention to the necessity of conducting a large-scale study to find out the ideal approach to manage such conditions.
Keywords: stroke, free-floating thrombus, FFT, secondary polycythemia vera, PV, dual antithrombotic
Introduction
Free-floating thrombosis (FFT) is an uncommon etiology of ischemic stroke and its backbone literature is based on case reports and series, where most papers primarily discuss internal carotid artery free-floating thrombus. In the recent literature there have been extremely few reported cases about vertebral artery FFT. Nevertheless, these are regrettably inconsistent due to the lack of a unified morphological definition and standardized radiological diagnostic features of the FFT. FFT has a male predilection, with a 2:1 male-to-female ratio, and it is more common in younger age groups.3 The manifestation in middle age and the consequences of neurological deficits mean FFT is a matter of great significance to be studied. The exact pathogenesis of FFT is still uncertain. Hypercoagulability and atherosclerosis are the highest probable etiologies in most reports.2,3 The mechanism behind atherosclerosis is debated to be either due to plaque erosion or plaque rupture. Other causes such as dissection and drug abuse are rarely reported.7,9 Whereas FFT could be asymptomatic and found incidentally,1,3 patients typically present with acute neurological deficits as a sequela of cerebral ischemic insult in context of transient ischemic attack (TIA) or well-established stroke. Some patients even develop evolving or current stroke.3,5 In this paper we describe a case of symptomatic FFT in the vertebral artery and we highlight the diagnostic as well as the therapeutic challenges that might be faced in approaching FFT.
Case Presentation
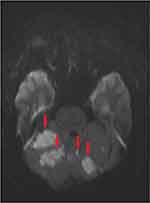
A 47-year-old Indian man who works as a private driver presented to our emergency department with acute vertigo, nausea, and vomiting after he had eaten in a public restaurant. He had been initially misdiagnosed as a case of gastroenteritis and discharged home. On the following day, he presented again with acute-onset focal neurologic deficits, described as a feeling of imbalance and falling to the right side, associated with a difficulty in speaking. The patient has not reported any history of headache nor other focal neurological deficits. He was a smoker (20 pack-years), however substance abuse, including drug and alcohol, was credibly denied. He was not known to have any other medical illnesses nor did he take any medications. Social as well as family history were unremarkable. Upon examination, the patient was conscious and oriented to time, place, and person. He exhibited right limb ataxia as seen on finger–nose and heel–shin tests as well as dysarthria, with a total NIH stroke scale (NIHSS) of 3. His blood pressure was slightly elevated (155/94), respiratory rate was 23/minute, temperature was 36.5C°, and pulse was 80 bpm. Laboratory tests were done at presentation (Table 1), which revealed an elevated hemoglobin (18.7 g/dL), hematocrit (62.5%), partial thromboplastin time (43.2 seconds), and Prothrombin time (14.4 seconds). Due to a high suspicion of acute cerebrovascular insult, a non-contrast cerebral neuroimaging via computed tomography (CT) (Figure 1) was performed and showed multiple areas of acute and subacute ischemic stroke in different territories including the posterior cerebral artery (PCA), superior cerebellar artery (SCA), posterior inferior cerebellar artery (PICA), and anterior inferior cerebellar artery (AICA) bilaterally. The cerebral CT-angiogram (CTA), from arch to vertex, showed a long segment of filling defect in the left vertebral artery, extending from V0 up to V2 segments, which is suggestive of a long, fresh, free-floating thrombus with the classical donut sign appearance (Figures 2 and 3). Based on clinico-radiographic findings, a diagnosis of multiple cerebral as well as cerebellar ischemic strokes due to arterio-arterial embolization was made. Acute management of stroke with thrombolysis and endovascular therapy was ineligible since the presentation was outside the thrombolysis window (over 24 hours from symptoms onset). To characterize the etiology of stroke we conducted a transthoracic echocardiogram (TTE) and long-term electrocardiogram (ECG) monitoring, which could not detect any evidence of cardiogenic embolic sources. Particularly, there was no evidence of atrial fibrillation, intracardial thrombus, regional wall motion abnormalities, atrial septal anomalies, or valvular dysfunction. Furthermore, extensive laboratory investigations, including thrombophilia and vasculitis screening, were unremarkable. Hematological colleagues were consulted and they attributed blood changes to heavy smoking and made a diagnosis of secondary polycythemia vera due to smoking.
 |
Table 1 Blood Work-Up Done for the Patient at Presentation |
 |
Figure 1 An axial view of a non-contrast computed tomography scan showing multiple areas of acute and subacute ischemic strokes in different territories. |
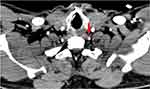 |
Figure 2 An axial view of computed tomography angiography scan showing a donut sign in the left vertebral artery, suggestive of free-floating thrombus at the level of V1. |
 |
Figure 3 A coronal view of computed tomography angiography scan showing a long, fresh, free-floating thrombus in V1 and V2. |
The patient was admitted to the stroke unit for close monitoring and was started on dual antiplatelet with aspirin 100 mg and clopidogrel 75 mg as well as thrombosis prophylaxis anticoagulation with enoxaparin 40 mg and atorvastatin 80 mg. He was also maintained on good hydration (100–120 mg/hour) and underwent phlebotomy. In the follow-up laboratory test, the hemoglobin and hematocrit fell to 14.2 g/dL and 42.8%, respectively. Throughout his stay in the hospital, he remained stable with evident improvement in his symptoms (NIHSS dropped to 1 point). The CTA follow-up (Figure 4) and doppler sonography showed complete canalization of the thrombus in the left vertebral artery. In addition, the follow-up neuroimaging via magnetic resonance imaging (MRI) showed no new ischemic insult in comparison to the initial cerebral CT (Figure 5).
 |
Figure 4 A coronal view of computed tomography angiography scan, showing complete canalization of the thrombus in the left vertebral artery 7 days post initiation of therapy. |
Discussion
FFT of cervicocranial arteries is an uncommon entity. Its incidence has been reported to be 1.53% among stroke patients.5 The occurrence of FFT was reported in the vast majority of case reports to be in the anterior extracranial circulation and more commonly in the internal carotid artery (ICA) (75%).3 In contrast, extremely few vertebral artery FFT (VA-FFT) cases were reported.
FFT is an acute neurological emergency that requires immediate attention and is usually symptomatic.3,4 However, few asymptomatic cases were reported in the literature.1 Our patient was symptomatic with recurrent strokes in the posterior circulation prior to therapy initiation.
Atherosclerosis and hypercoagulability are considered the likely etiologies in most reports.2,3 In this case, the underling etiopathogenesis of FFT was the hyperviscosity due to increased cellular component of blood in the context of secondary polycythemia vera (PV), which results in a hypercoagulable status.6 To our knowledge, there have not been any reports about the association of FFT and PV. So, the rarity of FFT occurrence in vertebral artery combined with the association with PV gives this case some uniqueness.
CTA is helpful in diagnosing FFT as it shows the characteristic donut sign8 and the length of the thrombus. Moreover, it can aid in estimating the associated stenosis in these patients; a measurement threshold of more than 3.8 mm on CTA was found to be highly specific and sensitive for FFT diagnosis.12 Further delineation of the free-floating thrombus can be done by doppler ultrasound of the carotid or vertebral arteries, as it is handy and easily available. Duplex scan and digital subtraction angiography (DSA) had sensitivities of 62.5% and 100%, respectively.4
In the published literature there has been a diversity in the therapeutic approach with satisfactory outcomes reported. These approaches vary from medical therapy with either single or dual antithrombotic (anticoagulation and/or antiplatelet) to urgent surgical intervention via carotid endarterectomy (CEA) or endovascular therapy (EVT). Up to date, the best available evidence for FFT treatment would be from a systematic literature review by Fridman et al.5 It has shown a trend favoring the medical approach with anticoagulants over the surgical approach; however, due to the lack of high-quality evidence from the literature published hitherto, no robust conclusion could be made. Likewise, a small retrospective study of FFT treatment in the proximal aorta and supra-aortic branches tended to the medical approach. It showed 90% resolution of FFT without adverse events under medical therapy with anticoagulant and/or antiplatelet.9 Nevertheless, a successful surgical intervention via EVT in ICA-FFT and VA-FFT has also been reported.1,11 A published review article by Bahtti et al3 failed to show any superiority of either approach. As the therapeutic guideline for FFT has not been established yet, each patient should be approached, for the time being, individually in an interdisciplinary manner (neurology, neurosurgery, and neuroradiology) as we have done with our patient. All therapeutic options were discussed and the decision went against EVT in fear of dislodging of the thrombus, since it was very extensive. However, EVT would be the first-line therapy if spontaneous migration of the thrombus in the basilar artery occurred. Despite the favoring of anticoagulation therapy in most reported studies, we were reluctant to begin anticoagulation in fear of developing hemorrhagic transformation, as the patient had multiple moderately sized infarctions in the cerebellum. After weighing the risks against the benefits, we decided to go for dual antiplatelet therapy with aspirin and clopidogrel along with the adjuvant therapy of repetitive phlebotomy with a target hematocrit below 45%10 and adequate hydration to reduce blood hyperviscosity and prevent progression of the thrombus. Within a few days of admission, the patient’s symptoms improved dramatically and no new further events occurred. The follow-up CTA on day 7 showed resolution of FFT.
Conclusion
The significance of FFT cases involving cervicocranial arteries lies in the seriousness of the condition as well as natural age of manifestation, since it may cause a stroke in middle-aged, well-functioning patients and result in devastating disability. For that reason, the neurologist should be aware of such a special entity and its consequences, monitor the patients closely, and treat them more aggressively using either the medical or surgical approach. For further studies, we recommend more research in the form of randomized controlled clinical trials for evaluating the efficacy, safety, and duration of aggressive medical therapy. Furthermore, a head-to-head study is needed to compare the superiority of either aggressive medical therapy or invasive surgical therapy; or otherwise, the indications of each.
Statement of Ethics
The subject has provided his informed consent for the creation of this manuscript with full knowledge that his clinical findings and treatment are utilized herein for educational and peer-reviewed publication purposes. Ethical approval from the institutional review board at Imam Abdulrahman Bin Faisal University was not required to publish the details of this case.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Disclosure
The authors have declared no conflicts of interest for this work.
References
1. Al-Jehani H, Alhamid MA, Alkhalaf Y, Alabbas F. A case of coincidental free floating thrombus in the vertebral artery in a patient presenting with an anterior circulation stroke and literature review. Neurointervention. 2020;15(3):144–153. doi:10.5469/neuroint.2020.00087
2. Monteiro A, Cunha Y, Cortez CM, Sauvageau E, Hanel R. Spontaneous resolution of carotid stenosis with free floating thrombus: a brief overview of possible mechanisms and management. Cureus. 2020;12(4):e7602.
3. Bhatti AF, Leon LR, Labropoulos N, et al. Free-floating thrombus of the carotid artery: literature review and case reports. J Vasc Surg. 2007;45(1):199–205. doi:10.1016/j.jvs.2006.09.057
4. Ferrero E, Ferri M, Viazzo A, et al. Free-floating thrombus in the internal carotid artery: diagnosis and treatment of 16 cases in a single center. Ann Vasc Surg. 2011;25(6):805–812. doi:10.1016/j.avsg.2011.02.030
5. Fridman S, Lownie SP, Mandzia J. Diagnosis and management of carotid free-floating thrombus: a systematic literature review. Int J Stroke. 2019;14(3):247–256. doi:10.1177/1747493019828554
6. Artoni A, Bucciarelli P, Martinelli I. Cerebral thrombosis and myeloproliferative neoplasms. Curr Neurol Neurosci Rep. 2014;14(11):496. doi:10.1007/s11910-014-0496-y
7. Cosenza M, Panza L, Califano AP, et al. Carotid thrombosis in a crack cocaine smoker woman. Case Rep Vasc Med. 2020;2020:4894825.
8. Menon BK, Singh J, Al-Khataami A, Demchuk AM, Goyal M; Calgary CTA Study Group. The donut sign on CT angiography: an indicator of reversible intraluminal carotid thrombus? Neuroradiology. 2010;52(11):1055–1056. doi:10.1007/s00234-010-0738-x
9. Gülcü A, Gezer NS, Men S, Öz D, Yaka E, Öztürk V. Management of free-floating thrombus within the arcus aorta and supra-aortic arteries. Clin Neurol Neurosurg. 2014;125:198–206. doi:10.1016/j.clineuro.2014.08.008
10. Berk PD, Goldberg JD, Donovan PB, Fruchtman SM, Berlin NI, Wasserman LR. Therapeutic recommendations in polycythemia vera based on Polycythemia Vera Study Group protocols. Semin Hematol. 1986;23(2):132–143.
11. Park JW, Lee DH, Choi CG, Kim SJ, Suh DC. Various endovascular approaches to the management of free floating carotid thrombi: a technical report. J Neurointerv Surg. 2012;4(5):336–338. doi:10.1136/neurintsurg-2011-010023
12. Jaberi A, Lum C, Stefanski P, et al. Computed tomography angiography intraluminal filling defect is predictive of internal carotid artery free-floating thrombus. Neuroradiology. 2014;56(1):15–23.0. doi:10.1007/s00234-013-1298-7
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.