Back to Journals » Clinical Interventions in Aging » Volume 13
Management of AO type 12C humerus proximal metadiaphyseal fractures with minimally invasive plate osteosynthesis in geriatric patients
Authors Seyfettinoğlu F, Oğur HU, Tuhanioğlu Ü , Çiçek H, Kapukaya A
Received 12 January 2018
Accepted for publication 17 March 2018
Published 22 May 2018 Volume 2018:13 Pages 1003—1010
DOI https://doi.org/10.2147/CIA.S162356
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Walker
Firat Seyfettinoğlu, Hasan Ulaş Oğur, Ümit Tuhanioğlu, Hakan Çiçek, Ahmet Kapukaya
Orthopaedics and Traumatology Department, Adana Numune Training and Research Hospital, Adana, Turkey
Background: To evaluate the treatment efficacy and complications of the lateral minimally invasive plate osteosynthesis (MIPO) method in geriatric patients with a humerus diaphyseal fracture with proximal extension.
Patients and methods: The study included a total of 21 patients (18 females, 3 males; mean age 74±6.3 years, range 65–89 years) who underwent surgery with the lateral MIPO technique for a humerus diaphyseal fracture with proximal extension during the period January 2011 to December 2016. None of the patients had additional injuries and all completed regular follow-up. According to the Arbeitsgemeinschaft für Osteosynthesefragen/Association for the Study of Internal Fixation classification system, the fractures were evaluated as 12C1 in 17 cases and 12C3 in 4 cases. All patients were evaluated radiologically and functionally at 6 months and 1 year. In the follow-up evaluations, the Constant–Murley score and the Quick Disabilities of the Arm, Shoulder, and Hand (Q-DASH) score were used.
Results: No non-union, avascular necrosis or infection was seen in any patient. The mean time to union was 15.7 weeks. Impingement syndrome was seen in 2 patients and radial nerve palsy in 2 patients. The mean Constant–Murley score was 70.6±10.2 at 6 months and 84±7.6 at the end of 1 year. The mean Q-DASH score was 38.6±15.1 at 6 months and 21.9±13.1 at the end of 1 year. The increase in the Constant–Murley scores from 6 months to 1 year was statistically significant (p<0.0001). The decrease in the Q-DASH scores between 6 months and 1 year was determined to be statistically significant. In the 2 patients with radial nerve palsy, the functions were seen to completely recover during follow-up. No axillary nerve palsy was seen in any patient.
Conclusion: Metadiaphyseal humerus fractures with proximal extension in the elderly can be successfully treated with the lateral MIPO technique. When applied correctly, it is a method with high rates of union and low rates of complications.
Keywords: metadiaphyseal fractures of proximal humerus, minimal invasive plating, elderly patients
Introduction
Humerus diaphyseal fractures that extend proximally, in other words, proximal metadiaphyseal fractures, are fractures for which treatment is challenging, that have been seen at an increasing frequency in recent years.1 Problems in the treatment of these fractures become more difficult in the geriatric population in particular, as elderly patients have reduced bone quality, increased fragility, and the time to union is prolonged.2,3 With increased mean life expectancy, the likelihood of orthopedists encountering these types of fractures has increased.2 The main philosophy in the current treatment of fractures in the geriatric patient group is early movement and a return to daily living activities as soon as possible. Just as conservative methods can be traditionally applied in the treatment of these fractures, intramedullary nailing and classic plate screw osteosynthesis are also treatment options.1 Conservative treatment has disadvantages, such as patient compliance, difficulties in the mobilization of geriatric patients, and that there cannot be an immediate return to daily living activities.3
The use of intramedullary nailing is limited because of disadvantages, such as difficulties in the control of fracture fragments, especially those extending metaphyseally, distal locking problems, and impingement syndrome.4,5 Furthermore, this indication is not greatly preferred because of changes in the physio-anatomy of geriatric bones. Classic plate-screw osteosynthesis has disadvantages, such as extensive soft tissue dissection and impaired vascularity of the fragments.6 However, in recent years, there has been increased use of the minimally invasive plate osteosynthesis (MIPO) method, especially in the femur and the tibia, followed by humerus shaft and humerus proximal fractures and many successful results have been reported in literatüre.6–10
The philosophy of the MIPO technique is based on the principle of providing relative stability with an acceptable reduction of the fracture with indirect methods with no impairment to soft tissue coverage and blood flow to the fracture fragments.11 Minimally invasive methods in the humerus became popularized a little late and most reports in literature are related to humerus diaphysis and proximal humeral fractures. Information in literature related to proximal metadiaphyseal fractures is relatively limited. Few studies have been published on this subject.12,13 To the best of our knowledge, there has been no previous study in the literature, which has focused on these fractures in the geriatric patient group.
The aim of this study was to evaluate the clinical–radiological results and complications of patients aged >65 years who were treated with the lateral MIPO method for a humerus proximal metadiaphyseal fractures (AO type 12C).
Patients and methods
This study was designed retrospectively. After approval from the ethics committee of Adana Numune Research and Educational Hospital (decision no.: 108 date: 13/9/2017). The study included a total of 21 patients (18 females, 3 males; mean age 74±6.3 years, range, 65–89 years) who underwent surgery with the MIPO technique for a humerus diaphyseal fracture with proximal extension in the period January 2011 to December 2016. None of the patients had additional injuries and all completed regular follow-up. A written informed consent form was obtained from all patients. The demographic data of the patients are shown in Table 1.
  | Table 1 Patient characteristics and results |
According to the Association for Osteosynthesis/Association for the Study of Internal Fixation classification system, the fractures were evaluated as 12C1 in 17 cases and 12C3 in 4 cases. The patients were evaluated radiologically and functionally at 3 and 6 weeks, then at 3 and 6 months. All the patients were evaluated again at the end of 1 year. The time to union was accepted as the visualization of callus on 3 of the 4 cortices on AP and lateral radiographs. In the follow-up evaluations, the Constant–Murley score and the Quick Disabilities of the Arm, Shoulder, and Hand (Q-DASH) score were used. While an increase in the Constant–Murley score shows that the patients are progressing well, a decrease in the Q-DASH score indicates a decrease in disability.
Surgical technique
Under general anesthesia, the patients were positioned in the beach-chair position and C-arm fluoroscopy was positioned on the opposite side to the affected extremity. A skin incision was made beginning at the anterolateral tip of the acromion and extending ~5 cm distal. The skin, subcutaneous tissue, fascia, and deltoid muscle were sharply dissected to partially expose the greater tuberosity. The axillary nerve was not fully exposed but was identified by finger dissection and elevation of the deltoid muscle from the proximal humerus. The skin and subcutaneous tissue were opened with a second distal lateral incision of 5–7 cm depending on the level to which the fracture extended distally. With blunt dissection between the brachialis and the brachioradialis, the radial nerve was located, elevated, and protected. Then, with traction applied from the elbow by making rotation movements with the forearm in supination and the elbow in 60° abduction, the axis was corrected by providing alignment of the biceps muscle to be vertical to the bicondylar axis. The reduction was checked on AP and lateral scopy images.
With an elevator applied from the proximal cut, a submuscular tunnel was opened over the periosteum toward the distal. The plate (unilock proximal humerus plate; Ortopro®, Izmir, Turkey) was advanced from the proximal cut to the distal using a 4.5 mm locking screw held as a guide and was placed in the opened tunnel over the periosteum. A threaded drill sleeve was then inserted into the locking part of a proximal and distal plate hole. Using these sleeves, the position of the plate could be corrected in both the antero-posterior and lateral view before preliminary fixation of the plate with K wires. First, the proximal fragment was fixed to the plate with 4.5 mm locking screws. Then using a non-locking screw first on the distal fragment, the plate was brought to the bone. The other distal screws were used as locking screws. For each fracture fragment, at least 3 screws (sub cortex) were used. The final alignment of the fracture and the implant was checked under image intensifier. After a final check from the distal cut that the radial nerve was intact, the layers were closed. No drain was used in any patient (Figure 1A–D). Postoperatively, all patients were applied with a shoulder-arm sling for 2 weeks. Free active shoulder movements and elbow mobilization were started the day after the operation.
Statistical analysis
Statistical analyses of the study data were made using MedCalc Version 10.3.0 software. Conformity of continuous data to normal distribution was assessed with the Shapiro Wilk test. Continuous variables were stated as mean ± SD and categorical variables as number (n) and percentage (%). In the comparison of the mean values of 2 dependent groups, which conformed to normal distribution, the paired t-test was used and a dot-line graph was drawn. A value of p<0.05 was accepted as statistically significant.
Results
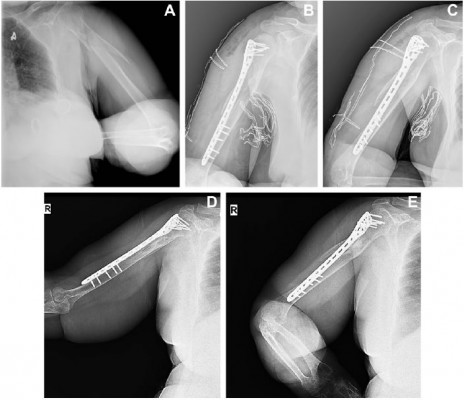
No non-union, avascular necrosis, or infection was seen in any patient. The mean time to union was 15.7 weeks (range, 12–20 weeks) (Figures 2A–E and 3A–E). Anterior impingement syndrome was seen in 2 patients (patient nos. 9 and 16) and radial nerve palsy in 2 patients (patient nos. 2 and 11). Radial nerve palsy is developed after surgery. The mean Constant–Murley score was 70.6±10.2 at 6 months and 84±7.6 at the end of 1 year (Table 2). The mean Q-DASH score was 38.6±15.1 at 6 months and 21.9±13.1 at the end of 1 year (Table 3). The increase in the Constant–Murley scores from 6 months to 1 year was statistically significant (p<0.0001). The decrease in the Q-DASH scores between 6 months and 1 year was determined to be statistically significant. In the 2 patients with radial nerve palsy, the functions were seen to completely recover during follow-up. In the patients with impingement syndrome, the implant was removed from 1 patient and the complaints recovered. Implant removal was recommended for the other patient but the treatment was refused. No axillary nerve palsy was seen in any patient.
  | Figure 2 (A) A 66-year-old female patient. AP X-ray showing fractures of left proximal shaft of the humerus (12C1) case number: 3 in Table 1. (B, C) AP and lateral X-rays showing early postoperatively graphies. (D, E) X-rays 6 months after the operation showing the consolidated fracture. (Constant–Murley score: 71). |
  | Figure 3 (A) A 77-year-old female patient. X-ray showing fracture of right proximal shaft of the humerus (12C1) case number: 14 in Table 1. (B, C) Early postoperative graphics. (D, E) X-rays 12 months after the operation showing the consolidated fracture. (Constant–Murley score: 86). |
  | Table 2 Constant–Murley scores at 6 and 12 months |
  | Table 3 Q-DASH scores at 6 and 12 months |
Discussion
The vast majority of humerus shaft fractures can be treated with traditional conservative methods.1–3 However, there are disadvantages to conservative treatment, such as restricted movement in the shoulder and elbow joints, delayed union or non-union, and plaster cast-related complications.3 A series of negative effects of conservative treatment of fragmented diaphyseal fractures that extend proximally have led orthopedists to search for other methods. Although there are many reports in literature of successful results with the MIPO method in femur and tibia fragmented fractures, biological methods in the humerus become popular later.14–16 A factor in this has been the possibility of axillary nerve damage in the proximal and radial nerve damage in the distal.17,18
Therefore, the anterior approach has been recommended for biological plating of AO group humerus diaphyseal fractures.8 In this way, plating can be applied distant from the axillary nerve in the proximal and from the radial nerve in the distal. However, metaphysodiaphyseal fractures require a little more care as the proximal fragment tends to be displaced laterally with the effect of the deltoid muscle.12 Moreover, proximal extension may also require a screw to be advanced to the humerus head. Previous studies have reported that in diaphyseal fractures with proximal extension in particular, there are advantages, such as lateral placement of the plate facilitates reduction of the proximal fragment abducted by the deltoid muscle and there is no requirement for recontouring the anatomic plate.12–14 In this study, the lateral MIPO method was used.
For humerus fractures, the MIPO method is used more for proximal humerus fractures. There are many reports in literature of successful results in proximal humerus fractures using the MIPO method.10,11,19 Similarly, several reports of humerus shaft fractures have shown pleasing results from the MIPO method.6,8,17 However, knowledge related to the MIPO method in humerus proximal metadiaphyseal fractures is more limited. There are few publications and although good results have been reported, there has been no study on this subject in the geriatric population. James et al evaluated the results of 24 geriatric patients treated with open reduction and conventional plating for a complex metaphysodiaphyseal fracture and reported successful results.20 However, as open reduction and conventional plating was used in that study, the current study can be said to be the first to report the use of the MIPO method to treat metadiaphyseal fractures in geriatric patients. As mean life expectancy will increase in the future, this subject will be of greater importance. Therefore, in this study, it was aimed to focus on the geriatric population in particular.
For the use of the MIPO technique on humerus fractures with proximal extension, there has been debate in the literature on subjects, such as the incision site, the plate length, plate location, radial and axillary nerve protection, and whether or not the plate should be contoured.13,14,18,21,22 While some authors have used a deltoid split in the proximal and lateral approach in the distal, others have preferred plating with a deltopectoral approach. With regard to the choice of plate, PHILOS plate, helical plate, and humerus proximal plates with specific distal contouring can be used. Moon et al used helical plates in their studies and Brunner et al used the PHILOS plate with an anterior distal curve.18,22 The authors reported that in this way, safe plating could be applied distant from the radial nerve as the distal of the plate comes onto the anterior surface of the humerus.18
In the lateral plating method, the plate helps the anatomic reduction. The important point of this is that the axillary nerve is not injured in the proximal and the radial nerve is not injured in the distal.12 Knowledge of the anatomic localization of the axillary and radial nerves is the most important way of avoiding complications. The axillary nerve courses from the posterior to the anterior of the humerus neck at mean 6.1±0.7 cm distal to the uppermost point of the humerus head.23 While some surgeons elevate both nerves, others have reported that exploration, elevation, and protection of the radial nerve only is sufficient.12,13,18 Aksu et al used the deltoid-split approach on a series of 13 patients and reported no axillary or radial nerve palsy with elevation for the protection of both nerves.12 In a study by Rancan et al using the deltoid-split approach, it was reported that the axillary nerve was protected with the finger without visualization in the proximal. In the distal, however, the radial nerve was explored.13 In the current study, the radial nerve in the distal was routinely explored and protected.
The axillary nerve was not routinely elevated but was protected with the finger as recommended by Rancan et al. In a study of MIPO technique used on 17 patients by Lau et al, it was reported that the axillary nerve in the proximal and the radial nerve in the distal were not explored.14 To avoid the need to explore the radial nerve in the distal, plate length was selected so that distal of the plate would remain 8 cm above the lateral epicondyle. Despite this, temporary radial palsy complication was reported in 3 patients.14 In the current study, the radial nerve was routinely explored and protected. Although the main aim of this was not to cause any damage to the radial nerve, it also ensured that secondary exploration was not necessary to confirm that the radial nerve was intact in potential radial palsy, which could develop in the postopertive period.
As the nerve is visualized during the operation, the radial palsy that occurs can be evaluated as neurapraxia. In the anterior placement of the plate, there is no need for radial nerve exploration. However, screws going from anterior to posterior can damage the radial nerve. In a study by Huri et al, the anterior MIPO technique was applied to 14 patients and because of radial nerve palsy developing in 1 patient, secondary exploration had to be applied.8 If anatomic variations of the radial nerve are added into the calculation, plating according to the epicondylar distance without visualization of the nerve could be risky. In the study by Lau et al where the MIPO technique was applied without visualization of the nerve, radial palsy was encountered in 3 patients.14 Therefore, in the current study, to ensure that the radial nerve was intact, it was considered necessary to explore and protect the nerve under all conditions. The situation was a little different, however, for the axillary nerve. In deltopectoral plating, the nerve is not at risk.21,22 In the deltoid-split approach, plating can be applied protecting the nerve without exploration.13,18 In the current study, routine exploration of the axillary nerve was not considered necessary.
Subacromial impingement syndrome is a complication often seen after surgical treatment of proximal humerus fractures.8–10 In various studies in literature, the frequency has been reported as 2%–7%.16,17 In the geriatric patient group in particular, impingement syndrome may sometimes severely restrict daily living activities.20 Removal of the implant may be required in treatment.22 Brunner et al reported that it was necessary to remove the implant in 3 patients of a series of 15.18 In the current series, subacromial impingement syndrome developed in 2 patients. Of these, the implant was removed in 1 and the complaints recovered and in the other case, the recommendation of implant removal was not accepted by the patient.
Traditionally, conservative methods are used in the treatment of humerus shaft fractures as the humerus is a bone with a high potential for union and because orthopedists wish to avoid radial nerve palsy.1,3 However, generally successful union results and times have been reported in osteosynthesis with the MIPO method.12–14 Brunner, Zhou, and Moon all reported union rates of 100%.18,21,22 Rancan et al reported non-union in only 1 patient of 29.13 In the current study, full bone union was obtained in all the patients. The mean time to union was consistent with literature at 15.7 weeks despite the patients being in the geriatric age group.
In literature, various scoring systems, such as the Constant–Murley score, the Mayo Elbow score, and the Q-DASH score, have been used to objectively evaluate the shoulder and upper extremity functional status after proximal humerus fracture surgery.17–22 The aim of this is to calculate the effect of radiological healing on the functional status and daily living activities. In the current study, the Constant–Murley and the Q-DASH scores were used. Both scores were calculated again at 6 months and 1 year. In the current study, the increase in the Constant–Murley score and the decrease in the Q-DASH score at both 6 months and 1 year were statistically significant. The increase in functional scores of the patients at 1 year compared with the 6-month values and the decrease in the disability scores demonstrated that the patients had recovered functionally after 6 months.
Limitations
Limitations of this study can be said to be the relatively low number of patients and that there was no control group. Nevertheless, this study can be considered a guide for these types of fractures, which are increasingly seen in the geriatric patient group.
Conclusion
Metadiaphyseal humerus fractures with proximal extension can be successfully and safely treated with the lateral MIPO technique. When applied correctly in accordance with the principles, it can be considered a method with high rates of union and low complication rates.
Disclosure
The authors report no conflicts of interest in this work.
References
McKee MD. Fractures of the shaft of the humerus. In: Bucholz RW, Heckman JD, Court-Brown C, editors. Fractures in Adults. 6th ed. Philadelphia, PA: Lippincott Williams & wilkins; 2006:1118–1159. | ||
Nguyen TV, Center JR, Sambrook PN, Eisman JA. Risk factors for proximal humerus, forearm, and wrist fractures in elderly men and women: the Dubbo Osteoporosis Epidemiology Study. Am J Epidemiol. 2001;153(6):587–595. | ||
Rüedi T, Moshfegh A, Pfeiffer KM, Allgöwer M. Fresh fractures of the shaft of the humerus-conservative or operative treatment? Reconstr Surg Traumatol. 1974;14(0):65–74. | ||
Blum J, Engelmann R, Küchle R, Hansen M, Rommens PM. Intramedullary nailing of humeral head and humeral shaft fractures. Eur J Trauma Emerg Surg. 2007;33(2):149–158. | ||
Petsatodes G, Karataglis D, Papadopoulos P, Christoforides J, Gigis J, Pournaras J. Antegrade interlocking nailing of humeral shaft fractures. J Orthop Sci. 2004;9(3):247–252. | ||
Bhandari M, Devereaux PJ, McKee MD, Schemitsch EH. Compression plating versus intramedullary nailing of humeral shaft fractures – a meta-analysis. Acta Orthop. 2006;77(2):279–284. | ||
Kim JW, Oh CW, Byun YS, Kim JJ, Park KC. A prospective randomized study of operative treatment for noncomminuted humeral shaft fractures: conventional open plating versus minimal invasive plate osteosynthesis. J Orthop Trauma. 2015;29(4):189–194. | ||
Huri G, Biçer ÖS, Öztürk H, Deveci MA, Tan I. Functional outcomes of minimal invasive percutaneous plate osteosynthesis (MIPPO) in humerus shaft fractures: a clinical study. Acta Orthop Traumatol Turc. 2014;48(4):406–412. | ||
Röderer G, Erhardt J, Graf M, Kinzl L, Gebhard F. Clinical results for minimally invasive locked plating of proximal humerus fractures. J Orthop Trauma. 2010;24(7):400–406. | ||
Falez F, Papalia M, Greco A, et al. Minimally invasive plate osteosynthesis in proximal humeral fractures: one-year results of a prospective multicenter study. Int Orthop. 2016;40(3):579–585. | ||
Koljonen PA, Fang C, Lau TW, Leung F, Cheung NW. Minimally invasive plate osteosynthesis for proximal humeral fractures. J Orthop Surg (Hong Kong). 2015;23(2):160–163. | ||
Aksu N, Karaca S, Kara AN, Işiklar ZU. Minimally invasive plate osteosynthesis (MIPO) in diaphyseal humerus and proximal humerus fractures. Acta Orthop Traumatol Turc. 2012;46(3):154–160. | ||
Rancan M, Dietrich M, Lamdark T, Can U, Platz A. Minimal invasive long PHILOS®-plate osteosynthesis in metadiaphyseal fractures of the proximal humerus. Injury. 2010;41(12):1277–1283. | ||
Lau TW, Leung F, Chan CF, Chow SP. Minimally invasive plate osteosynthesis in the treatment of proximal humeral fracture. Int Orthop. 2007;31(5):657–664. | ||
Paluvadi SV, Lal H, Mittal D, Vidyarthi K. Management of fractures of the distal third tibia by minimally invasive plate osteosynthesis – A prospective series of 50 patients. J Clin Orthop Trauma. 2014;5(3):129–136. | ||
Doshi HK, Wenxian P, Burgula MV, Murphy DP. Clinical outcomes of distal femoral fractures in the geriatric population using locking plates with a minimally invasive approach. Geriatr Orthop Surg Rehabil. 2013;4(1):16–20. | ||
Kobayashi M, Watanabe Y, Matsushita T. Early full range of shoulder and elbow motion is possible after minimally invasive plate osteosynthesis for humeral shaft fractures. J Orthop Trauma. 2010;24(4):212–216. | ||
Brunner A, Thormann S, Babst R. Minimally invasive percutaneous plating of proximal humeral shaft fractures with the Proximal Humerus Internal Locking System (PHILOS). J Shoulder Elbow Surg. 2012;21(8):1056–1063. | ||
Acklin YP, Jenni R, Walliser M, Sommer C. Minimal invasive PHILOS(®)-Plate osteosynthesis in proximal humeral fractures. Eur J Trauma Emerg Surg. 2009;35(1):35–39. | ||
James IB, Farrell DJ, Evans AR, Siska PA, Tarkin IS. Open reconstruction of complex proximal metadiaphyseal fragility fractures of the humerus. Geriatr Orthop Surg Rehabil. 2014;5(1):9–13. | ||
Zhou ZB, Gao YS, Tang MJ, Sun YQ, Zhang CQ. Minimally invasive percutaneous osteosynthesis for proximal humeral shaft fractures with the PHILOS through the deltopectoral approach. Int Orthop. 2012;36(11):2341–2345. | ||
Moon JG, Kwon HN, Biraris S, Shon WY. Minimally invasive plate osteosynthesis using a helical plate for metadiaphyseal complex fractures of the proximal humerus. Orthopedics. 2014;37(3):e237–e243. | ||
Bono CM, Grossman MG, Hochwald N, Tornetta P 3rd. Radial and axillary nerves. Anatomic considerations for humeral fixation. Clin Orthop Relat Res. 2000;(373):259–264. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

