Back to Journals » International Journal of General Medicine » Volume 13
Malignant Arrhythmias as the Unmasked Manifestation of Thyroid Storm
Received 3 June 2020
Accepted for publication 5 August 2020
Published 24 September 2020 Volume 2020:13 Pages 693—698
DOI https://doi.org/10.2147/IJGM.S265833
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Wen Shang, Qing-Bian Ma
Department of Emergency, Perking University Third Hospital, Beijing 100191, People’s Republic of China
Correspondence: Qing-Bian Ma
Department of Emergency, Perking University Third Hospital, 49 Huayuan North Road, Beijing 100191, People’s Republic of China
Tel +86-10-82264047
Fax +86-10-82264040
Email [email protected]
Abstract: Thyroid storm is usually due to a severe exacerbation of a preexisting thyrotoxicosis, which later leads to decompensation in different organ systems. Thyroid storm with malignant arrhythmia is rare, but the mortality rate is high. Malignant arrhythmia has usually occurred in some patients with hypokalemia or ischemic heart disease. The presentation of these arrhythmias in the initial phase of the disease is much less common, and only a few isolated cases are described in the scientific literature. This paper analyzes and summarizes the clinical characteristics of this disease through literature reviews, for clinicians early detection and diagnosis of this disease. We report a 51-year-old woman with diarrhoea, fever, thyroid storm, ventricular fibrillation and no potential heart disease. The case report is discussed using relevant data from literature. A total of 9 patients were reported in the literature, totalling 10 cases with ours, including 7 cases of ventricular fibrillation and 3 cases of ventricular tachycardia. Most of the treatments were antithyroid drugs, hormones and beta-receptor blockers, and 3 death cases. Patients with thyroid crisis need to be closely monitored for malignant arrhythmias. Early diagnosis and treatment may save lives.
Keywords: thyroid storm, malignant arrhythmia, ventricular tachycardia
Introduction
Thyroid storm is characterized by multiple-system involvement and complex illness, and the mortality rate is 8–30%.1 Multiple-organ failure, congestive heart failure and respiratory failure are the main causes of death; however, malignant ventricular arrhythmias, which are potentially fatal, are much more unusual in thyroid storms. They are more common in patients with hypokalaemia, prolonged QT interval, or myocardial ischemia. So far, the mechanism of the two is unclear, and there are no pathological features to help doctors make early diagnoses.
Case
A 51-year-old woman was admitted to the emergency department complaining of diarrhoea and fever for four days. She had a history of hyperthyroidism and atrial fibrillation for 20 years with irregular intake of medications but stopped taking them 6 months previously. The patient’s initial vital signs were as follows: temperature, 38.9°C; heart rate, 131 beats per minute (bpm); blood pressure, 155/86 millimetres of mercury (mmHg); respiratory rate, 24 ventilations per minute; and SpO2 100% on a 2 L non-rebreather mask. Physical examination revealed mild fainting, proptosis, goitre, and jaundice. The patient’s lungs were clear. Her heart sounds were unremarkable except for tachycardia and irregularity. Her extremities were warm and sweaty. The remaining examination was normal. The admission and subsequent biochemical parameters are listed in Table 1 and Figure 1. Her thyroid function was assessed in our hospital, and it showed high serum levels of free T3 of 13.01 pg/mL (2.3–4.2) and free T4 of 4.43 ng/dl (0.89–1.8) and suppressed TSH of 0.01 nU/mL (0.55–4.78). Anti-thyroid peroxidase antibody was markedly elevated at > 1300 U/mL (< 60), anti-TSH receptor antibody was 34.2 IU/L (≤ 1.75), and anti-thyroglobulin antibody was 105.2 IU/mL (<60). Echocardiography showed enlargement of the left and right atria, mitral regurgitation (moderate), tricuspid regurgitation (severe), pulmonary hypertension (moderate), PASP of 70 mmHg, aortic regurgitation (mild), LVEF55%, widened inferior vena cava diameter, and decreased respiratory mobility. The patient’s Burch-Wartofsky(BWPS) score was 80. Therefore, thyroid storm disease was diagnosed. Diuresis with intravenous therapy was initiated along with beta-blockers, propylthiouracil, and corticosteroid therapy (Figure 2). After treatment, her temperature was normal, her heart rate dropped to 100–110 beats per minute, and her consciousness recovered. However, on the fifth day of admission, she had a fever of 39°C with cough and weakness. A review of the chest radiograph showed an exudative lesion of the left lung and left pleural effusion. She then lost consciousness from ventricular fibrillation. Cardiopulmonary resuscitation was done in time, and after amiodarone 300 g intravenous injection, the patient’s circulation recovered. Blood gas analysis showed pH 7.24, PCO2 43 mmHg, and PO2 123 mm Hg. Laboratory tests showed Lac >15 mmol/L, HCO3–18.4 mmol/L, BE −9 mmol/L, SO2 98%, K 4.3 mmol/L, and Glu 5.1 mmol/L. Electrocardiogram after resuscitation showed atrial fibrillation, ST-T changed and QTC 0.415 s (Figure 3). However, the patient’s spontaneous circulation could not be maintained, and she died of cardiac arrest.
 |
Table 1 Summary of the Laboratory Data |
 |
Figure 1 Electrocardiogram at admission. Atrial fibrillation, mild ST segment depression in leads V 3–6.T wave inversion. |
 |
Figure 2 Diagnosis and treatment of the patient. |
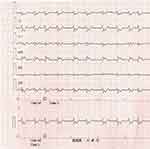 |
Figure 3 Electrocardiogram after resuscitation. Still atrial fibrillation, ST segment depression was significantly deepened and ST segment elevation in aVR lead. |
Methods
We searched PubMed, Wed of Science, Scopus and Embase with “thyroid storm” and “ventricular arrhythmia” or “cardiac arrest” as key words. The inclusion criteria matched the definite diagnosis of thyroid storm and malignant arrhythmia, except ventricular asystole or hypokalaemia, long-QT syndrome and malignant arrhythmia caused by organic heart disease. We collected datas on age, sex, causes of thyrotoxicosis, symptom, inducer of thyroid storm, BWPS score, type of arrhythmia, time from admission to ventricular fibrillation, treatment and prognosis (Table 2).
 |
Table 2 Clinical Characteristics of Thyroid Storm and Malignant Arrhythmia |
Result
A total of 10 patients were collected, with a male to female ratio of 3:7 and an average age of 28.9 years. The majority of the causes of thyrotoxicosis were Graves’ disease, accounting for 7 cases. In terms of malignant arrhythmia, ventricular fibrillation was found in 7 cases, accounting for the majority, and ventricular tachycardia, including tip-torsion ventricular tachycardia, in 3 cases. The time from admission to malignant arrhythmia was mostly short, ranging from a few minutes to a few days; the longest was 5 days, with an average time of 62.52 hours. Treatment included antithyroid drugs, hormones, beta-blockers, and iodine. Prognosis: 3 patients died, and 7 were discharged or improved, for a mortality rate of 30%. The patients who died were all patients with ventricular fibrillation, with an average age of 51.33 years, older than the average age (Table 2).
Discussion
Thyroid storm is a rare, life-threatening endocrine emergency that requires timely diagnosis and active treatment. The diagnosis is based on clinical symptoms and signs, including disturbance of consciousness, fever, heart failure, diarrhoea, and jaundice. The incidence of thyroid storm in patients with hyperthyroidism ranges from 1% to 2%, while the mortality rate from thyroid storm is between 20% and 30%.1 Malignant ventricular arrhythmias are much more unusual but fatal.2 Our patient did not have ischemic cardiomyopathy, prolonged QT interval, or hypokalaemia. Therefore, thyroid storm can also cause malignant arrhythmias such as ventricular fibrillation in patients without hypokalaemia and potential heart disease. Even now, the mechanism for this is unclear.
Our patient had no relief of symptoms of hyperthyroidism and discontinued thyroid hormone and thyroid drugs. Her BPWS score was 80. She had a clear diagnosis of thyroid storm and improved after treatment, but she had ventricular fibrillation on hospitalization day 5. The first reason is that the patient may have ischemic heart disease. The patient has a 20-year history of hyperthyroidism, the echocardiography shows changes in heart structure, and the electrocardiogram shows changes in ST-T after resuscitation, so the patient may have organic heart disease. Unfortunately, coronary angiography was not performed to confirm myocardial ischemia. The patient’s infection was aggravated and pneumonia appeared, and the infection induced the thyroid storm. Although the patient had drugs to treat the thyroid storm, the hormone was discontinued. In the course of reducing the dosage of the remaining drugs, the reinfection was aggravated, causing the release of thyroxin again in large quantities into the blood, and the combination of the two caused ventricular fibrillation after thyroid storm.
In our literature review, a total of 9 patients with thyroid storm had no underlying heart disease or hypokalaemia but had malignant arrhythmias.3–7 Ventricular tachycardia has been registered in hyperthyroid patients suffering from Grave’s disease and it has been associated with the interaction of autoantibodies of the 1-adrenergic, the M2 muscarinic, and the TSH-receptors.3 So we consider two possibilities likely. One is that a large amount of thyroid hormone is secreted when the thyroid storm comes on, and an important effect on the electrophysiological properties of myocardial cells is that Na+/K+/ATP enzyme activity increased, Ca2+/ATP enzyme activity increased in the sarcoplasmic reticulum, slow cardiac calcium channel activation promoted calcium influx to enhance myocardial contractility, oxygen consumption increased, and conduction system ischemia and hypoxia grew, leading to severe arrhythmia, endangering the patients’ lives.1,8,9 The second mechanism considers that Graves disease is a systemic autoimmune disease that involves the cardiovascular system and may involve autoimmune myocarditis in the heart. Autoimmunity may alter the myocardial electrical properties promoting idiopathic ventricular arrhythmia. The dysregulating effects of the autoantibodies against the calcium and potassium ion channels can play the basis for autoimmune phenocopies of genetic cardiac channelopathies. Autoimmune cardiac channelopathies have been suggested as a novel mechanism in the development of cardiac arrhythmias.10 Chen et al autopsied a 46-year-old patient with heart failure after a thyroid storm.11 Lymphocytic myocarditis was found on dissection, and autoimmune myocarditis may be involved in the occurrence of malignant arrhythmias in patients with hyperthyroidism.1,12 It should also be noted that the infection is associated with inflammation and could contribute to occurrence of Ventricular fibrillation in individuals with thyroid dysfunction.
Conclusion
Although the arrhythmia caused by thyroid storm is mostly supraventricular, it has recently been reported as a ventricular arrhythmia. Therefore, strict ECG monitoring is needed. Early identification and treatment may save lives. The mechanism of the relationship between thyroid storm and ventricular arrhythmia needs further research. However, physicians should also pay more attention to subjects with thyroid dysfunction to prevent thyroid profile misbalance and hence cardiac arrhythmias, both atrial and ventricular. This fact should be noted as well.
Consent for Publication
Written informed consent has been provided by the patient’s daughter to have the case details and any accompanying images published.
Ethics and Consent Statement
Our institution does not require ethical approval for reporting individual cases.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors have no conflicts of interest to declare for this work.
References
1. Anjo D, Maia J, Carvalho AC, et al. Thyroid storm and arrhythmic storm: a potentially fatal combination. Am J Emerg Med. 2013;31:
2. Ueno A, Yamamoto T, Sato N, et al. Ventricular fibrillation associated with early repolarization in a patient with thyroid storm. J Interv Card Electrophysiol. 2010;29(2):93–96. doi:10.1007/s10840-010-9507-3
3. Jao YTFN, Chen Y, Lee W-H, et al. Thyroid storm and ventricular tachycardia. South Med J. 2004;97(6):604–607. doi:10.1097/00007611-200406000-00020
4. Nakashima Y, Kenzaka T, Okayama M, et al. A case of thyroid storm with cardiac arrest. Int Med Case Rep J. 2014;7:89–92. doi:10.2147/IMCRJ.S63475
5. Wolfson B, Smith K. Cardiac arrest following minor surgery in unrecognized thyrotoxicosis - a case report. Anesth Analg. 1968;47(6):
6. Munoz-Camacho JF, Jaime S-S. Malignant ventricular arrhythmias as the initial manifestation of hyperthyroidism. Rev Esp Cardiol. 2007;60(4):449–450.
7. Korte AK, Derde L, van Wijk J, et al. Sudden cardiac arrest as a presentation of Brugada syndrome unmasked by thyroid storm. BMJ Case Rep. 2015;2015:bcr2015212351.
8. Leonard S, Lilly MD. Braunwald’s Heart Disease Review and Assessment E-Book.
9. KleinI OK. Mechanisms of disease: thyroid hormone and the cardiovascular system. N Engl J Med. 2001;344(7):501–509. doi:10.1056/NEJM200102153440707
10. Chen YT, Yang GG, Hsu YH. Thyroid storm and lymphocytic myocarditis. Intern Med. 2010;49(6):593–596. doi:10.2169/internalmedicine.49.2504
11. Alper AT, Hasdemir H, Akyol A, et al. Incessant ventricular tachycardia due to subacute thyroiditis. Int J Cardiol. 2007;116(1):e22–e24. doi:10.1016/j.ijcard.2006.08.068
12. Danzi S, Klein I. Thyroid abnormalities in heart failure. Heart Fail Clin. 2020;16(1):
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
