Back to Journals » Cancer Management and Research » Volume 12
Major Hepatectomy in Elderly Patients with Large Hepatocellular Carcinoma: A Multicenter Retrospective Observational Study
Authors Chen ZL, Zhang CW, Liang L , Wu H, Zhang WG, Zeng YY, Gu WM, Chen TH, Li J, Zhang YM, Wang H, Zhou YH, Li C , Diao YK, Lau WY, Wu MC, Shen F, Yang T , Liang YJ
Received 14 April 2020
Accepted for publication 12 June 2020
Published 9 July 2020 Volume 2020:12 Pages 5607—5618
DOI https://doi.org/10.2147/CMAR.S258150
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Ahmet Emre Eşkazan
Zheng-Liang Chen,1,* Cheng-Wu Zhang,2,* Lei Liang,2,* Han Wu,3,* Wan-Guang Zhang,4 Yong-Yi Zeng,5 Wei-Min Gu,6 Ting-Hao Chen,7 Jie Li,8 Yao-Ming Zhang,9 Hong Wang,10 Ya-Hao Zhou,11 Chao Li,2 Yong-Kang Diao,2 Wan Yee Lau,3,12 Meng-Chao Wu,3 Feng Shen,3 Tian Yang,3 Ying-Jian Liang1
1Department of Hepatobiliary Surgery, The First Affiliated Hospital of Harbin Medical University, Heilongjiang, People’s Republic of China; 2Department of Hepatobiliary, Pancreatic and Minimal Invasive Surgery, Zhejiang Provincial People’s Hospital, People’s Hospital of Hangzhou Medical College, Zhejiang, People’s Republic of China; 3Department of Hepatobiliary Surgery, Eastern Hepatobiliary Surgery Hospital (Navy Medical University), Second Military Medical University, Shanghai, People’s Republic of China; 4Department of Hepatic Surgery, Tongji Hospital, Huazhong University of Science and Technology, Wuhan, People’s Republic of China; 5Department of Hepatobiliary Surgery, Mengchao Hepatobiliary Hospital, Fujian Medical University, Fujian, People’s Republic of China; 6The First Department of General Surgery, The Fourth Hospital of Harbin, Heilongjiang, People’s Republic of China; 7Department of General Surgery, Ziyang First People’s Hospital, Sichuan, People’s Republic of China; 8Department of Hepatobiliary Surgery, Fuyang People’s Hospital, Anhui, People’s Republic of China; 9The 2nd Department of Hepatobiliary Surgery, Meizhou People’s Hospital, Guangdong, People’s Republic of China; 10Department of General Surgery, Liuyang People’s Hospital, Hunan, People’s Republic of China; 11Department of Hepatobiliary Surgery, Pu’er People’s Hospital, Yunnan, People’s Republic of China; 12Faculty of Medicine, The Chinese University of Hong Kong, Shatin, New Territories, Hong Kong, SAR, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Ying-Jian Liang
Department of Hepatobiliary Surgery, The First Affiliated Hospital of Harbin Medical University, No. 23, Youzheng Road, Heilongjiang 150006, People’s Republic of China
Email [email protected]
Tian Yang
Department of Hepatobiliary Surgery, Eastern Hepatobiliary Surgery Hospital, Second Military Medical University (Navy Medical University), No. 225, Changhai Road, Shanghai 200438, People’s Republic of China
Email [email protected]
Background: With an increase in life expectancy and improvement of surgical safety, more elderly patients with hepatocellular carcinoma (HCC), even with large tumors, are now considered for hepatectomy. This study aimed to clarify the impact of age on short- and long-term outcomes after major hepatectomy (≥ 3 segments) for large HCC (≥ 5 cm).
Patients and Methods: Using a multicenter database, patients who underwent curative-intent major hepatectomy for large HCC between 2006 and 2016 were identified. Postoperative morbidity and mortality, overall survival (OS) and recurrence-free survival (RFS) were compared between the elderly (≥ 65 years) and younger (< 65 years) patients. Univariable and multivariable Cox-regression analyses were performed to identify the risk factors of OS and RFS in the entire and elderly cohorts, respectively.
Results: Of 830 patients, 92 (11.1%) and 738 (88.9%) were elderly and younger patients, respectively. There were no significant differences in postoperative 30-day mortality and morbidity between the two groups (5.4% vs 2.6% and 43.5% vs 38.3%, both P> 0.05). The 5-year OS and RFS rates in elderly patients were also comparable to younger patients (35.0% vs 33.2% and 20.0% vs 20.8%, both P> 0.05). In the entire cohort, multivariable Cox-regression analyses identified that old age was not independently associated with OS and RFS. However, in the elderly cohort, preoperative alpha-fetoprotein level > 400 μg/L, multiple tumors, macrovascular invasion and microvascular invasion were independently associated with decreased OS and RFS.
Conclusion: Carefully selected elderly patients benefited from major hepatectomy for large HCC as much as younger patients, and their long-term prognosis was determined by preoperative alpha-fetoprotein level, tumor number and presence of macro- or micro-vascular invasion.
Keywords: hepatocellular carcinoma, hepatectomy, survival, recurrence, elderly
Introduction
Hepatocellular carcinoma (HCC) is the fourth leading cause of cancer-related mortality in adults,1 and is the most common cancer affecting the elderly worldwide.2 The overall prognosis of HCC remains dismal. For a subset of patients receiving curative therapies including local ablation, liver transplantation and partial hepatectomy,3 long-term survival is still possible. Local ablation, albeit less invasive, is only suitable for small HCC, generally considered to be less than 5 cm. Liver transplantation is the treatment of choice for early HCC that meets the Milan criteria. However, the lack of donors limits its application in elderly patients, especially in Asia. Thus, for patients with a large HCC (≥5 cm), especially in elderly patients, the only possible cure is partial hepatectomy.
Advances in surgical techniques, perioperative assessments, anesthesia and medical care have led to notably decrease in postoperative morbidity and mortality following hepatectomy for HCC. In general, selected elderly patients, although having more associated comorbidities and compromised organ reserve, can still well tolerate hepatectomy for HCC with short- and long-term outcomes similar to younger patients. Age by itself did not have any significant negative impact.4–10 Major hepatectomy (≥3 Couinaud segments) for large HCC intrinsically has a higher surgical risk.11 However, so far there have been few studies on whether this operation in elderly patients is safe, efficacious and having long-term oncological outcomes similar to younger patients.12,13
The aim of the present study was to determine safety and efficacy in elderly patients undergoing major hepatectomy for large HCC using a large multicenter database. The short- and long-term outcomes, including long-term overall (OS) and recurrence-free survival (RFS), in elderly patients (≥65 years old) were compared with younger patients (<65 years old).
Patients and Methods
Study Population
Using a multicenter database, patients who underwent curative-intent hepatectomy for HCC at 11 medical institutions in China from January 2006 to December 2016 were identified. These institutions included the First Affiliated Hospital of Harbin Medical University, Zhejiang Provincial People’s Hospital, Eastern Hepatobiliary Surgery Hospital, Tongji Hospital, Mengchao Hepatobiliary Hospital, the Fourth Hospital of Harbin, Ziyang First People’s Hospital, Fuyang People’s Hospital, Meizhou People’s Hospital, Liuyang People’s Hospital, and Pu’er People’s Hospital. Major hepatectomy was defined as partial hepatectomy of three or more Couinaud’s segments. Curative hepatectomy was defined as the removal of all microscopic and macroscopic tumors with a microscopically clear margin (R0 resection). The exclusion criteria included: 1) patient ≤18 years old, 2) combined HCC-cholangiocarcinoma, 3) recurrent HCC, 4) palliative hepatectomy (R1 or R2 resection), 5) HCC with a maximum tumor size <5 cm, 6) minor hepatectomy (<3 segments), 7) loss to follow-up within 3 months after surgery, and 8) missing data on important prognostic variables. Informed consent was obtained from all the patients for their data to be used for clinical research. The data were censored on June 30, 2019. The study was performed according to the Declaration of Helsinki and the Ethical Guidelines for Clinical Studies. Approval from Ethics Committees of each of the individual hospital was obtained.
Preoperative Evaluation
Preoperative evaluation was generally consistent at each participating institution. Liver function was evaluated by biochemistry and Child–Pugh classification. Upper gastrointestinal endoscopy was routinely employed for all HCC patients who were scheduled for operation. Patients older than 60 years and those with significant co-morbid illnesses were routinely sent for formal cardiopulmonary evaluation.14,15 Child–Pugh grade C was considered an absolute contraindication for HCC resection. Resection criteria were constant over the study period, including the number of resectable tumors, presence or absence of gross tumor thrombus, and adequate liver function reserve, as reported in our previous study.14,16
Clinicopathologic Characteristics and Operative Variables
The following patients’ clinicopathologic characteristics were collected, including: age, sex, co-morbidities, American Society of Anesthesiologists (ASA) score, etiology of liver diseases, presence of cirrhosis or portal hypertension, Child–Pugh grading, preoperative alpha-fetoprotein (AFP) level, maximum tumor size, tumor number, presence of satellite nodules, tumor differentiation, presence of macroscopic or microscopic vascular invasion, tumor encapsulation, and resection margin status. Co-morbidities included hypertension, diabetes mellitus, chronic obstructive pulmonary disease, renal dysfunction, and cardiovascular disease. Cirrhosis was confirmed by histopathological examination. Portal hypertension was defined as the presence of either splenomegaly with a decreased platelet count (≤100×109/L) or esophageal varices. Operative variables collected included intraoperative blood loss and intraoperative blood transfusion.
Follow-Up
Patients were followed-up at each participating institution. The routine postoperative surveillance strategy for recurrence included serum AFP level, ultrasonography or contrast-enhanced computed tomography (CT) or magnetic resonance imaging (MRI) of the chest and abdomen once every 2 months for the first 6 months, once every 3 months thereafter for the next 18 months, and then once every 6 months at 2 years and later after resection. When HCC recurrence was suspected, contrast-enhanced CT or MRI, chest CT, bone scan or positron emission tomography were performed as clinically indicated. Tumor recurrence was defined as a new appearance of intra- or extra-hepatic tumor nodule(s) with or without a rise in serum AFP level, as well as the presence of intrahepatic nodules that had typical imaging features with characteristic features of HCC on contrast-enhanced CT or MRI examination. Treatment of HCC recurrence was based on the pattern of recurrence, residual hepatic functional reserve, and general condition of patient.
Study Endpoints
As the present study focused on perioperative safety and long-term survival outcomes of hepatectomy for HCC, the primary endpoints were OS and RFS, while the secondary endpoints were postoperative 30-day mortality and morbidity. OS was defined as the time from surgery to death from any cause, and RFS as the time from surgery to HCC recurrence or death. Postoperative morbidities were classified into five grades based on the Clavien-Dindo classification,17 and minor and major morbidities were defined as Clavien-Dindo <3 and ≥3, respectively.
Statistical Analysis
Statistical analyses were performed using SPSS software version 25.0 (SPSS, Chicago, IL, USA). Categorical variables were expressed as number (n) or proportion (%), while continuous variables were expressed as mean ± standard deviation or median (range). Categorical and continuous covariates were compared using the χ2 test with Yates correction or Fisher’s exact test, and Student’s t test or Mann–Whitney ranked U-test, respectively. The OS and RFS rates were estimated using the Kaplan–Meier curves and compared with the Log-rank test. Univariable and Multivariable Cox-regression analyses were performed to identify risk factors which were independently associated with decreased OS and RFS in the entire cohort, as well as in the elderly cohort. The variable of age, as the most important variable, was forced into the multivariable Cox-regression model. Other variables with a P value <0.1 in univariable analysis were subjected to the multivariable Cox-regression model using a forward stepwise selection. All tests were two-tailed, and a significant P value was defined as <0.05.
Results
The multicenter database contained details of 2133 patients from 11 institutions who underwent partial hepatectomy with the curative intention for HCC during the study period. Using the inclusion criteria, 830 patients who underwent curative major hepatectomy for large HCC were enrolled in this study (Figure 1). Among all the 830 patients identified in the entire cohort, there were 92 elderly patients (≥65 years old, 11.1%) and 738 younger patients (<65 years old, 88.9%), with a median age of 68 (range: 65 to 83) and 49 (range: 21 to 64) years, respectively. Patients’ clinicopathologic characteristics and operative variables among the elderly versus the younger were notable for several differences (Table 1): proportion of male patients, patients with co-morbidities, ASA score > 2, chronic hepatitis B virus (HBV) infection and satellite nodules were significantly higher in the elderly group (all P < 0.05).
 |
Figure 1 Flowchart of study population. HCC, hepatocellular carcinoma. |
Comparisons of Postoperative Morbidity and Mortality
Postoperative short-term outcomes of the elderly and younger patient groups are summarized in Table 1. The postoperative 30-day mortality and morbidity rates were comparable in the two groups (5.443.5% vs 2.6% and 38.3%, P = 0.173 and 0.365, respectively). The postoperative major and minor morbidity rates were also comparable (17.426.1% vs 17.6% and 20.7%, P = 1.000 and 0.280, respectively). Univariable and multivariable logistic regression analyses of risk factors associated with postoperative 30-day morbidity are shown in Table 2.
 |
Table 2 Univariable and Multivariable Logistic Regression Analyses of Risk Factors of Postoperative 30-Day Morbidity After Major Hepatectomy for Large Hepatocellular Carcinoma in the Entire Cohort |
Comparisons of Long-Term Survival and HCC Recurrence
After excluding 24 patients who suffered from postoperative 30-day death, long-term outcomes of the remaining 806 patients were compared between the two groups (Table 3). At a median follow-up of 26.4 months (mean follow-up: 36.8 months), 569 of 806 patients (70.6%) had died and 622 (77.2%) had developed HCC recurrence. The overall mortality and recurrence rates among the elderly versus the younger groups were 72.4 and 70.1% versus 77.7 and 70.7%, respectively (both P > 0.2). The median OS and RFS in the elderly group were 30.6 and 9.8 months, while the median OS and RFS in the younger group were 25.6 and 8.8 months, and there was no significant difference between these two groups (P = 0.739 and 0.632, respectively). As shown in Table 3 and Figure 2, the 1-, 3- and 5-year OS and RFS rates in the elderly group were 71.3%, 43.2% and 35.0%, and 41.4%, 27.3% and 20.0%, respectively, which were comparable to the younger group (68.9%, 42.0% and 33.2%, and 44.0%, 28.3% and 20.8%, respectively).
 |
Figure 2 Cumulative incidence of overall survival (OS, 2A) and recurrence-free survival (RFS, 2B) curves comparisons between elderly and younger patients (calculated by Log-rank test). |
Analyses of Prognostic Factors for OS and RFS in the Entire Cohort
Independent risk factors associated with OS and RFS after major hepatectomy for large HCC were identified by univariable and multivariable Cox-regression analyses (Tables 4 and 5). Multivariable analyses demonstrated that old age was not independently associated with OS and RFS (both P > 0.2), but preoperative AFP level >400 μg/L (hazard ratio [HR] 1.53, 95% confidence interval [CI] 1.29–1.82), satellite nodules (HR 1.75, 95% CI 1.48–2.08), macrovascular invasion (HR 2.48, 95% CI 2.06–2.99), microvascular invasion (HR 2.30, 95% CI 1.91–2.76), and intraoperative blood transfusion (HR 2.34, 95% CI 1.13–1.58) were independent risk factors of decreased OS, while preoperative AFP level >400 μg/L (HR 1.54, 95% CI 1.31–1.81), satellite nodules (HR 1.51, 95% CI 1.28–1.78), macrovascular invasion (HR 2.14, 95% CI 1.76–2.46), microvascular invasion (HR 1.62, 95% CI 1.34–1.95), intraoperative blood transfusion (HR 1.27, 95% CI 1.08–1.49), and resection margin <1 cm (HR 2.08, 95% CI 1.76–2.46) were independent risk factors of decreased RFS after major hepatectomy for large HCC.
Prognostic Analyses for OS and RFS in the Elderly Cohort
Table 6 lists the risk factors identified by univariable and multivariable Cox-regression analyses which were associated with OS after major hepatectomy for HCC in the elderly cohort. Multivariable analyses demonstrated that preoperative AFP level >400 μg/L (HR 1.84, 95% CI 1.04–3.26), multiple tumors (≥3 tumor nodules) (HR 2.07, 95% CI 1.18–3.62), and macrovascular invasion (HR 3.01, 95% CI 1.58–5.74) were independent risk factors of decreased OS after major hepatectomy for elderly patients with a large HCC.
 |
Table 6 Univariable and Multivariable Cox-Regression Analyses of Risk Factors of Overall Survival After Major Hepatectomy for Large Hepatocellular Carcinoma in the 87elderly Patients |
Table 7 lists the risk factors identified by univariable and multivariable Cox-regression analysis which were associated with RFS after major hepatectomy for HCC in the elderly cohort. Multivariable analyses identified preoperative AFP level >400 μg/L (HR 1.82, 95% CI 1.03–3.22), multiple tumors (HR 2.47, 95% CI 1.37–4.44), macrovascular invasion (HR 2.71, 95% CI 1.54–4.77), and microvascular invasion (HR 1.85, 95% CI 1.06–3.21) to be independent risk factors of decreased RFS after major hepatectomy for elderly patients with a large HCC.
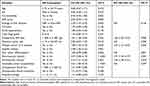 |
Table 7 Univariable and Multivariable Cox-Regression Analyses of Risk Factors of Recurrence-Free Survival After Major Hepatectomy for Large Hepatocellular Carcinoma in the 87 Elderly Patients |
According to the number of three independent risk factors which could be identified before surgery, ie preoperative AFP level >400 μg/L, the presence of macrovascular invasion, and multiple tumor (≥3 nodules), the 87 elderly patients were divided into 3 subgroups: 1) without any risk (n = 43); 2) with any one of the three risks (n = 30); and 3) with ≥2 of the three risks (n = 14; 10 patients with any 2 of the three risks and 4 patients with all three risks). As shown in Figure 3, there were significant differences between OS and RFS among these three subgroups (both P < 0.001). Of note, the 1-year OS and RFS rates of those 14 patients who had any 2 of the three risks were only 35.7% and 14.3%, respectively.
 |
Figure 3 Cumulative incidence of overall survival (OS, 3A) and recurrence-free survival (RFS, 3B) curves comparisons among three subgroups of the elderly patients (calculated by Log-rank test). |
Discussion
With aging populations, prolonged life expectancy, and improvements in perioperative management, the number of elderly patients undergoing hepatectomy for HCC in centers around the world has significantly increased in the past three decades.5–7,10,18,19 However, the safety and effectiveness of major hepatectomy (≥3 segments) for large HCC (≥5 cm) among elderly patients have still not been well defined.20–22 There are several major areas of concern: 1) more comorbidities and compromised organ functional reserve in the elderly; 2) more complicated surgical procedure resulting in higher perioperative risks in major hepatectomy; and 3) uncertain long-term survival outcomes for large HCC.
This large multicenter study of 830 patients with large HCC revealed that major hepatectomy can safely be performed in the elderly (≥65 years old), with postoperative morbidity and mortality rates similar to younger patients of <65 years old; moreover, elderly patients can benefit from major hepatectomy for large HCC, with long-term OS and RFS outcomes similar to younger patients. This study supports the findings that age by itself is not a contraindication to major hepatectomy of large HCC, with oncological benefits and an acceptable safety profile. Major hepatectomy should be offered to selected elderly patients with large HCC. The present study on analyzing the prognostic factors of OS and RFS in the elderly cohort demonstrated that preoperative AFP level >400 μg/L, multiple tumors (≥3 tumor nodules) and macrovascular invasion were independently associated with decreased OS and RFS in elderly patients after major hepatectomy for large HCC. These data are helpful in the surgical decision-making in selecting patients for surgery and in assessing whether adjuvant therapy should be considered for elderly patients with large HCC. To our knowledge, this is the first study to evaluate specifically surgical safety and long-term survival outcomes in elderly patients who underwent major hepatectomy for large HCC. The results from this Multicenter cooperative study may lead to a more widely accepted consensus on the role of major hepatectomy in elderly patients with large HCC.
Malignancies are often considered to be a disease associated with aging.23,24 The probability of developing a malignant tumor in the elderly is higher than in younger populations. The risk of developing HCC is higher among patients over 60~70 years old, and most elderly patients with HCC should have a background of cirrhosis. However, in this study, the proportion of cirrhosis among the elderly in the entire cohort was lower than younger patients (64.1% vs 72.4%, P = 0.111). This is probably related to patient selection during surgical decision-making.
Some tumor-related factors, such as preoperative AFP level >400 μg/L, satellite nodules, macrovascular invasion, and microvascular invasion as identified in the entire cohort of this study were independently associated with decreased OS and RFS after major hepatectomy for large HCC. They have also been demonstrated by previously reported studies to be high-risk factors.25–27 In addition, the surgery-related variable of intraoperative blood transfusion was also identified in this study to be independent risk factors associated with OS and RFS. A possible explanation is that allogenic blood transfusion induces immunosuppression and decreases natural-killer cell and/or helper T-cell activities.28 In fact, the relationship between blood transfusion and long-term prognosis after curative resection of many malignancies, including HCC, remains controversial.16,29 Anyway, avoidance of unnecessary blood transfusions is of importance for other reasons like saving costs, avoiding transfusion reactions and transfusion-related acute lung injury, and reducing risks of blood-transmitting diseases.
In this study of 830 patients with large HCC, 25.6% had macrovascular invasion, 64.4% had microvascular invasion, 58.3% were huge (≥10 cm), and 19.6% were multiple tumors (≥3 tumor nodules). Therefore, it is understandable that the recurrence rate of this cohort was higher than those of previous studies of this kind. As the tumor size increases, the probability of having other advanced malignant pathological characteristics, including macrovascular and microvascular invasion, multiformity, satellite nodules, and incomplete tumor encapsulation, will increase. As shown in Tables 3 and 4, univariable analyses of the entire cohort revealed that there were significant differences of OS and RFS between patients with HCCs of 5.0–9.9 cm and HCCs ≥10 cm (HR: 1.23 and 1.24, P = 0.015 and 0.006, respectively). However, multivariable Cox-regression analyses did not reveal maximum tumor size (≥10 vs 5.0–9.9 cm) as an independent risk factor of OS and RFS, but macrovascular invasion, microvascular invasion and satellite nodules as independent risk factors associated with poorer OS and RFS. In one previous study, for solitary hepatocellular carcinoma without macroscopic vascular invasion, we demonstrated that tumor size did not independently affect long-term OS and RFS after curative resection.30 As we think, although tumor size is also an important prognostic factor of HCC resection, its effect on a cohort of patients with large HCC (≥5 cm) may be somewhat weaker compared with other tumor characteristics, such as macrovascular and microvascular invasion, and satellite nodules, etc.
A deeper understanding of the risk factors associated with long-term oncological survival outcomes in elderly patients subjected to major hepatectomy for HCC can help surgeons on management, decision-making and determine strategies whether to give adjuvant treatment. In the present study, univariable and multivariable Cox-regression analysis performed in the elderly cohort identified four independent risk factors associated with OS and DFS. With the exception of microvascular invasion, these risk factors of preoperative AFP level, tumor number and macrovascular invasion can be identified by preoperative laboratory and imaging examinations. Interestingly, the 14 (16.1%, 14 of 87) patients who had ≥2 of these 3 independent risk factors had 1-year OS and RFS rates of only 35.7% and 14.3%, respectively. Thus, for elderly patients with multiple risk factors, the benefit of major hepatectomy for large HCC is questionable. Future studies are required to better define how postoperative molecular-targeted and emerging immunotherapy drugs may be combined with hepatectomy to provide these patients with better survival outcomes.
This study has several limitations. First, this is a retrospective cohort study that had potential inherent biases. Second, patients in the present study were also treated exclusively in China and, therefore, the majority of patients with HCC had a background of HBV-related cirrhosis. In the United States and Europe,31,32 HCV infection and excessive alcohol are the main etiological factors. As such, data from the present study need to be externally validated in Western patients to ensure whether the results are generalizability to other populations of patients.
List of Abbreviations
HCC, hepatocellular carcinoma; OS, overall survival; RFS, recurrence-free survival; ASA, American Society of Anesthesiologists; AFP, alpha-fetoprotein; CT, computed tomography; MRI, magnetic resonance imaging; HBV, hepatitis B virus; HR, hazard ratio; CI, confidence interval; HCV, hepatitis C virus; MV, multivariable; NA, not available; UV, univariable; OR, odds ratio.
Author Contributions
Conception: Zheng-Liang Chen, Cheng-Wu Zhang, Tian Yang, Ying-Jian Liang, Wan Yee Lau; Study design: Ying-Jian Liang, Zheng-Liang Chen, Cheng-Wu Zhang, Lei Liang, Feng Shen; Administrative support: Cheng-Wu Zhang, Meng-Chao Wu, Feng Shen, Ying-Jian Liang, Tian Yang; Data collection and acquisition: Zheng-Liang Chen, Lei Liang, Han Wu, Wan-Guang Zhang, Yong-Yi Zeng, Wei-Min Gu, Ting-Hao Chen, Jie Li, Yao-Ming Zhang, Hong Wang, Ya-Hao Zhou, Chao Li, Yong-Kang Diao; Data analysis: Ying-Jian Liang, Zheng-Liang Chen, Tian Yang, Yong-Kang Diao; Writing-original draft: Zheng-Liang Chen, Lei Liang, Han Wu, Wan-Guang Zhang, Yong-Yi Zeng, Wei-Min Gu, Ting-Hao Chen, Jie Li, Yao-Ming Zhang, Hong Wang, Ya-Hao Zhou, Chao Li, Yong-Kang Diao; Writing-review & editing: Wan Yee Lau, Feng Shen, Meng-Chao Wu, Ying-Jian Liang, Tian Yang; Final approval of manuscript: All authors. All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Villanueva A. Hepatocellular carcinoma. N Engl J Med. 2019;380(15):1450–1462. doi:10.1056/NEJMra1713263
2. El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132(7):2557–2576. doi:10.1053/j.gastro.2007.04.061
3. Agrawal S, Belghiti J. Oncologic resection for malignant tumors of the liver. Ann Surg. 2011;253(4):656–665. doi:10.1097/SLA.0b013e3181fc08ca
4. Müller-Höcker J, Aust D, Rohrbach H, et al. Defects of the respiratory chain in the normal human liver and in cirrhosis during aging. Hepatology. 1997;26(3):709–719. doi:10.1002/hep.510260324
5. Kaibori M, Yoshii K, Hasegawa K, et al. Treatment optimization for hepatocellular carcinoma in elderly patients in a Japanese nationwide cohort. Ann Surg. 2019;270(1):121–130. doi:10.1097/SLA.0000000000002751
6. Mirici-Cappa F, Gramenzi A, Santi V, et al. Treatments for hepatocellular carcinoma in elderly patients are as effective as in younger patients: a 20-year multicentre experience. Gut. 2010;59(3):387–396. doi:10.1136/gut.2009.194217
7. Cucchetti A, Sposito C, Pinna AD, et al. Effect of age on survival in patients undergoing resection of hepatocellular carcinoma. Br J Surg. 2016;103(2):e9399. doi:10.1002/bjs.10056
8. Ezaki T, Yukaya H, Ogawa Y. Evaluation of hepatic resection for hepatocellular carcinoma in the elderly. Br J Surg. 1987;74(6):471–473. doi:10.1002/bjs.1800740614
9. Nanashima A, Abo T, Nonaka T, et al. Prognosis of patients with hepatocellular carcinoma after hepatic resection: are elderly patients suitable for surgery. J Surg Oncol. 2011;104(3):284–291. doi:10.1002/jso.21932
10. Zhao LY, Huo RR, Xiang X, et al. Hepatic resection for elderly patients with hepatocellular carcinoma: a systematic review of more than 17,000 patients. Expert Rev Gastroenterol Hepatol. 2018;12(10):1059–1068. doi:10.1080/17474124.2018.1517045
11. Wong TC, Cheung TT, Chok KS, et al. Treatment strategy to improve long-term survival for hepatocellular carcinoma smaller than 5 cm: major hepatectomy vs minor hepatectomy. World J Surg. 2014;38(9):2386–2394. doi:10.1007/s00268-014-2601-4
12. Sgourakis G, Sotiropoulos GC, Bockhorn M, et al. Major liver resections for primary liver malignancies in the elderly. Acta Chir Belg. 2009;109(3):340–344. doi:10.1080/00015458.2009.11680436
13. Wang WL, Zhu Y, Cheng JW, et al. Major hepatectomy is safe for hepatocellular carcinoma in elderly patients with cirrhosis. Eur J Gastroenterol Hepatol. 2014;26(4):444–451. doi:10.1097/MEG.0000000000000046
14. Yang T, Zhang J, Lu JH, Yang GS, Wu MC, Yu WF. Risk factors influencing postoperative outcomes of major hepatic resection of hepatocellular carcinoma for patients with underlying liver diseases. World J Surg. 2011;35(9):2073–2082. doi:10.1007/s00268-011-1161-0
15. Yang T, Lin C, Zhai J, et al. Surgical resection for advanced hepatocellular carcinoma according to Barcelona Clinic Liver Cancer (BCLC) staging. J Cancer Res Clin Oncol. 2012;138(7):1121–1129. doi:10.1007/s00432-012-1188-0
16. Yang T, Lu JH, Lau WY, et al. Perioperative blood transfusion does not influence recurrence-free and overall survivals after curative resection for hepatocellular carcinoma: a propensity score matching analysis. J Hepatol. 2016;64(3):583–593. doi:10.1016/j.jhep.2015.10.012
17. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–213. doi:10.1097/01.sla.0000133083.54934.ae
18. Trevisani F, Cantarini MC, Labate AM, et al. Surveillance for hepatocellular carcinoma in elderly Italian patients with cirrhosis: effects on cancer staging and patient survival. Am J Gastroenterol. 2004;99(8):1470–1476. doi:10.1111/j.1572-0241.2004.30137.x
19. Kozyreva ON, Chi D, Clark JW, et al. A multicenter retrospective study on clinical characteristics, treatment patterns, and outcome in elderly patients with hepatocellular carcinoma. Oncologist. 2011;16(3):310–318. doi:10.1634/theoncologist.2010-0223
20. Ishizawa T, Hasegawa K, Aoki T, et al. Neither multiple tumors nor portal hypertension are surgical contraindications for hepatocellular carcinoma. Gastroenterology. 2008;134(7):1908–1916. doi:10.1053/j.gastro.2008.02.091
21. Yau T, Tang VY, Yao TJ, Fan ST, Lo CM, Poon RT. Development of Hong Kong liver cancer staging system with treatment stratification for patients with hepatocellular carcinoma. Gastroenterology. 2014;146(7):1691–1700.e3. doi:10.1053/j.gastro.2014.02.032
22. Imamura H, Matsuyama Y, Tanaka E, et al. Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J Hepatol. 2003;38(2):200–207. doi:10.1016/S0168-8278(02)00360-4
23. Calcinotto A, Kohli J, Zagato E, Pellegrini L, Demaria M, Alimonti A. Cellular senescence: aging, cancer, and injury. Physiol Rev. 2019;99(2):1047–1078. doi:10.1152/physrev.00020.2018
24. Hong H, Wang Q, Li J, Liu H, Meng X, Zhang H. Aging, Cancer and Immunity. J Cancer. 2019;10(13):3021–3027. doi:10.7150/jca.30723
25. Yeh CN, Chen MF, Lee WC, Jeng LB. Prognostic factors of hepatic resection for hepatocellular carcinoma with cirrhosis: univariate and multivariate analysis. J Surg Oncol. 2002;81(4):195–202. doi:10.1002/jso.10178
26. Zhou L, Rui JA, Wang SB, et al. Clinicopathological features, post-surgical survival and prognostic indicators of elderly patients with hepatocellular carcinoma. Eur J Surg Oncol. 2006;32(7):767–772. doi:10.1016/j.ejso.2006.03.050
27. Hanazaki K, Kajikawa S, Koide N, Adachi W, Amano J. Prognostic factors after hepatic resection for hepatocellular carcinoma with hepatitis C viral infection: univariate and multivariate analysis. Am J Gastroenterol. 2001;96(4):1243–1250. doi:10.1111/j.1572-0241.2001.03634.x
28. Cata JP, Wang H, Gottumukkala V, Reuben J, Sessler DI. Inflammatory response, immunosuppression, and cancer recurrence after perioperative blood transfusions. Br J Anaesth. 2013;110(5):690–701. doi:10.1093/bja/aet068
29. Liu L, Wang Z, Jiang S, et al. Perioperative allogenenic blood transfusion is associated with worse clinical outcomes for hepatocellular carcinoma: a meta-analysis. PLoS One. 2013;8(5):e64261. doi:10.1371/journal.pone.0064261
30. Zhang H, Yuan SX, Dai SY, et al. Tumor size does not independently affect long-term survival after curative resection of solitary hepatocellular carcinoma without macroscopic vascular invasion. World J Surg. 2014;38(4):947–957. doi:10.1007/s00268-013-2365-2
31. Lau GK, Leung YH, Fong DY, et al. High hepatitis B virus (HBV) DNA viral load as the most important risk factor for HBV reactivation in patients positive for HBV surface antigen undergoing autologous hematopoietic cell transplantation. Blood. 2002;99(7):2324–2330. doi:10.1182/blood.V99.7.2324
32. Goh GB, Chang PE, Tan CK. Changing epidemiology of hepatocellular carcinoma in Asia. Best Pract Res Clin Gastroenterol. 2015;29(6):919–928. doi:10.1016/j.bpg.2015.09.007
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




