Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 13
Maintenance inhaler preference, attribute importance, and satisfaction in prescribing physicians and patients with asthma, COPD, or asthma–COPD overlap syndrome consulting for routine care
Authors Ding B , Small M, Scheffel G, Holmgren U
Received 19 October 2017
Accepted for publication 19 February 2018
Published 16 March 2018 Volume 2018:13 Pages 927—936
DOI https://doi.org/10.2147/COPD.S154525
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Bo Ding,1 Mark Small,2 Gina Scheffel,3 Ulf Holmgren3
1Medical Evidence and Observational Research, AstraZeneca Gothenburg, Mölndal, Sweden; 2Real World Research (Respiratory), Adelphi Real World, Bollington, UK; 3Global Payer Evidence and Pricing, AstraZeneca Gothenburg, Mölndal, Sweden
Background: In respiratory disorders, patient- and physician-perceived satisfaction with the maintenance inhaler device is an important factor driving treatment compliance and outcomes. We examine inhaler preferences in asthma and COPD from patient and physician perspectives, particularly focusing on the relative importance of individual device attributes and patient characteristics guiding inhaler choice.
Materials and methods: Real-world data from >7,300 patients with asthma, COPD, or asthma–COPD overlap syndrome (ACOS) consulting for routine care were derived from respiratory Disease Specific Programs conducted in Europe, USA, Japan, and China. Outcome variables included current pattern of inhaled maintenance therapy and device type, physician preference, patient-reported device attribute importance, and satisfaction.
Results: The most commonly prescribed inhalers for maintenance therapy of asthma, COPD, and ACOS were dry powder inhalers (62.8%–88.5% of patients) and pressurized metered dose inhalers (18.9%–35.3% of patients). One-third of physicians stated no preference for maintenance device when prescribing treatment, and less than one-third of patients reported being “extremely satisfied” with any attribute of their device. Instructions being “simple and easy to follow” was the inhaler attribute most commonly selected as important. For approximately one-third of patients across all groups, “ease of use/suitability of inhaler device” was a reason for the prescribing decision, as stated by the physician. Device characteristics were more likely to impact the prescribing decision in older patients (in asthma and COPD; P<0.01) and those with worse disease severity (in COPD; P<0.001).
Conclusion: A relatively high proportion of physicians had no preference for inhaler type across asthma, COPD, and ACOS. Simplicity of use was the most important inhaler attribute from a patient’s perspective. Physicians appeared to place most importance on ease of use and device suitability when selecting inhalers for older patients and those with more severe disease, particularly in COPD.
Keywords: inhaler preference, patient preference, maintenance therapy, COPD, asthma, routine care
Introduction
Inhaled medications form the mainstay of maintenance treatment in patients with asthma and COPD, both in terms of symptom control and exacerbation risk reduction.1,2 For patients with asthma, regular treatment with a low dose of inhaled corticosteroid (ICS), with or without a bronchodilator (long-acting β2-agonist [LABA] and/or long-acting muscarinic antagonist [LAMA]), has been shown to reduce symptoms and exacerbations, improve lung function, and enhance quality of life.1 Similar benefits are observed following inhaled maintenance treatment for COPD, although the magnitude of the effect on lung function may not be as large as for asthma.2
Typically, the choice of therapeutic agent and delivery platform will fall to the prescribing physician. An ever-increasing number of inhaled delivery options currently exists for respiratory medicines, including variations of pressurized metered dose inhalers (pMDIs), dry powder inhalers (DPIs), breath-actuated MDIs (baMDIs), and a soft mist inhaler (SMI). The choice of inhaler has an important bearing on the outcome of any treatment regimen, given that poor inhaler technique has been associated with suboptimal drug delivery, increased adverse events and, consequently, poor adherence and/or impaired disease control.1,3 It is, therefore, important to tailor the selection of the inhaler device to the individual patient, taking into account their needs, functional ability, and the complexity of the medication regimen.1,2 A study investigating inhaler preference, acceptability, and usability of different inhalers, including a single-dose inhaler and multi-dose inhalers, found that patients were quicker to learn how to correctly use multi-dose devices, which required fewer maneuvers prior to actuation.4 Availability and the cost of the inhaler device will also factor into any treatment decision.3,5
Certain patient characteristics can guide the choice of inhaler device. For example, in COPD, the selection of a device that is not breath-actuated (eg, pMDI, SMI) may be preferable to a DPI in patients with poor lung function parameters (ie, forced expiratory volume in 1 second [FEV1] and forced vital capacity) and a consequent reduced ability to inhale efficiently;6,7 particularly, elderly patients.6 Similarly, some groups of patients may be more suited to certain devices than others.2,8 For example, elderly patients with arthritis, muscle weakness, or impaired vision may encounter difficulties with large or bulky inhalers, or may be confused by complex medication regimens requiring multiple devices.9 Young children tend to show a preference for medium–high resistance inhalers that are easy to handle and have an oblong mouthpiece.10 It is the responsibility of the physician to ensure that patients are competent in the use of their inhaler and that they understand the importance of good inhaler technique.3,8 Provision of training in correct inhaler usage can greatly improve inhalation technique in patients.11 Additionally, provision of training to physicians themselves can help to improve inhalation technique in their patients.12
Patient-perceived satisfaction with their maintenance inhaler device is an important factor for driving treatment compliance in COPD, with inhaler satisfaction closely linked to improved health status.13 Indeed, health care professionals cite patient satisfaction as one of the most important attributes of an inhaler.14 It follows that the identification of specific inhaler features of particular importance to the patient could help to improve adherence and, ultimately, disease control.3 Previous studies have identified durability, ergonomics, and ease of use as important inhaler characteristics.4,10,13
In this cross-sectional analysis of data derived from the respiratory Disease Specific Program (DSP), we examine inhaler preferences in asthma and COPD, from both a patient’s and a physician’s perspective, with a particular focus on the relative importance of individual device attributes and patient characteristics guiding inhaler choice.
Materials and methods
The respiratory DSP is a cross-sectional survey of patients with asthma, COPD, or asthma–COPD overlap syndrome (ACOS) consulting for routine care, conducted in the USA, Europe (France, Germany, Italy, Spain, UK), Japan, and China. It is designed to provide impartial observations of real-world clinical practice from a physician’s and a matched-patient’s perspective, with a view to improving standards of care.15 Quantitative and qualitative patient and physician data together provide an accurate snapshot of the perception of a particular disease within a real-world setting, without preselection of patients. The survey can be viewed as four discrete stages. In Stage A, primary care and specialist physicians are screened and recruited with a view to obtaining nationally representative samples. This is followed by individual face-to-face interviews with the physician (Stage B). Stage C is the prospective completion of patient record forms by the physician for the next five consecutive patients with asthma and the next five patients with COPD (including ACOS). Finally, in Stage D patients fill out a self-completion record, with no influence or input from a health care professional.15 The respiratory DSPs were conducted in the fourth quarter of 2013 in France, Germany, Italy, Spain, UK, and the USA; the fourth quarter of 2012 in Japan (patient record form data only); and the fourth quarter of 2010 in China (specialists only).
Study populations
Patients and physicians
The patient population comprised three groups: asthma-only (patients >12 years of age with a physician-confirmed diagnosis of asthma), COPD-only (patients >40 years of age with confirmed airflow obstruction and a diagnosis of COPD that included emphysema and chronic bronchitis), and patients with ACOS who had a dual diagnosis of asthma and COPD. All patients were currently prescribed at least one inhaler for maintenance therapy (ICS, LAMA, ICS/LABA, LABA/LAMA, or LABA) at the time of enrollment.
Physicians were eligible for participation in the study if they became medically qualified within the last 5–35 years and were responsible for the treatment of both patients with asthma and patients with COPD, with the exception of allergists, who treated only patients with asthma.
Variables
Outcome variables were recorded directly by the patient or physician, or were derived from the physician- or patient-completed record form (which included the COPD Assessment Test and the modified Medical Research Council breathlessness scale). Descriptive variables included age, gender, time since diagnosis, physician-perceived severity of respiratory disease, comorbidities, most recent FEV1 (% predicted), and current treatment/device type. Patient preferences were measured according to perceived satisfaction with, and importance of, individual inhaler attributes. Physicians also provided information pertaining to their specialty, maintenance inhaler type preference, and inhaler prescribing practice.
Patient satisfaction and perceived importance of individual inhaler attributes
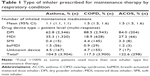
Patients indicated the three most important attributes in an inhaler from a predefined list of 12 attributes (detailed in Figure 1). For each of the 12 inhaler-specific attributes, patients were then asked to rate their satisfaction on a scale of 1 (not at all satisfied) to 5 (extremely satisfied).
  | Figure 1 Inhaler attributes as reported by patients by diagnosis (extremely satisfied). |
Statistical analyses
The use of the various inhaler devices (pMDI, baMDI, DPI, and SMI) was described in terms of the proportion of patients receiving each inhaler type. Physician-reported preference for inhaler device was described for the entire population, and was also stratified according to physician specialty (primary care physician [PCP], pulmonologist, or allergist [asthma-only]). Device attribute importance and satisfaction were determined using a five-point Likert scale. Disease groups were stratified as to whether or not “ease of use or suitability of inhaler device” was considered by the physician as a reason for the prescribing decision and a univariate test (Mann–Whitney) was used to determine whether the difference between the “yes” and “no” groups was statistically significant. All analyses were performed using Stata 13.1 (StataCorp LP, College Station, TX, USA; 2013).
Ethics approval and consent to participate
The DSP was conducted as a survey adhering to market research guidelines and codes of conduct according to the International Chamber of Commerce/European Society for Opinion and Marketing Research international code on observational research. Therefore, ethics approval was not necessary to obtain and was not sought. Patients provided informed consent to participate in the survey via a tick box on the front of the patient self-completion questionnaire.
Results
Study population
The 1,205 participating physicians included 449 PCPs, 646 pulmonologists, and 110 allergists. Of the total patient sample from the respiratory DSP survey who had data collected within the observation period, 7,305 patients were eligible for inclusion in the study population (asthma, n=3,736; COPD, n=3,326; ACOS, n=243). Most of these patients suffered from comorbidities; no comorbidities were reported for 26.4%, 19.3%, and 11.4% of patients with asthma, COPD, and ACOS, respectively. The most frequently reported comorbidities overall were hypertension, allergic rhinitis, elevated cholesterol, anxiety, gastroesophageal reflux disease, and diabetes (Table S1). The mean (95% CI) numbers of concomitant daily medications that were prescribed were 1.6 (1.5, 1.7), 3.4 (3.3, 3.5), and 4.3 (3.8, 4.7) for patients with asthma, COPD, and ACOS, respectively.
Current pattern of inhaled maintenance therapy
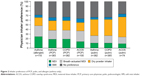
Globally, a DPI was the most commonly used inhaler for maintenance therapy, prescribed to 62.8%, 88.5%, and 84.0% of patients with asthma, COPD, and ACOS, respectively (Table 1). DPIs were also the most commonly prescribed inhaler type in each of the countries included in the survey (Table S2). MDIs were the next most commonly used maintenance device and among patients with asthma, approximately one-third (35.3%) of prescribed devices were MDIs, with slightly lower proportions among patients with COPD and ACOS (18.9% and 27.2%, respectively; Table 1). The proportions of patients using an SMI and baMDIs were much lower across all groups (Table 1).
Physician device preferences
Roughly one-third of physicians stated no preference for maintenance device when prescribing treatment, regardless of respiratory condition (Figure 2). Similarly, the device preferences of pulmonologists and PCPs were consistent across all three respiratory conditions. In asthma management, the preferences of allergists were more closely aligned with those of PCPs than with pulmonologists (Figure 2).
Patient device satisfaction
From the patients’ perspective, “instructions are simple and easy to follow” was the inhaler attribute considered the most important across indications (Table 2 and Table S3). While the relative importance of device attributes differed, the robustness of the inhaler, its ease of handling, and transportability were consistently rated as important (Table 2). Less than one-third of patients reported being extremely satisfied with any single attribute of their device (Figure 1). Across indications, the highest relative dissatisfaction was reported for the attributes “inhaler locking when empty”, “being able to reuse the inhaler for more than one month”, and “feedback on whether the dose has been inhaled correctly” (see Figure S1). Other secondary areas of dissatisfaction included irritation in the mouth and throat, inability to see how many doses are left, and having to breathe in while simultaneously pressing the inhaler, or breathing hard to inhale the medicine (see Figure S1). The proportions of patients satisfied or dissatisfied with specific attributes were generally consistent across indications, with the exception of the need to load the inhaler before use, for which the satisfaction rates were lowest for patients with COPD (Figures 1 and S1).
  | Table 2 Top five inhaler attributes as reported by patients by condition |
Physician’s prescribing decision
From the perspective of the physician, “ease of use/suitability of inhaler device” formed the basis of the prescribing decision for approximately one-third of patients across indications. Increases in patient age (in asthma and COPD; P<0.01) and disease severity (in COPD; P<0.001) played a significant role in consideration of device type when making a prescribing decision (Table 3). The time elapsed since diagnosis also had a significant effect on the likelihood of prescribing an inhaler for these criteria (P<0.0001 and P<0.05 for asthma and COPD, respectively). Patients with asthma or COPD had been diagnosed for significantly longer where the physician selected “ease of use/suitability of inhaler device” as a reason for the prescribing choice (Table 3).
For patients with COPD, higher impact of symptoms (assessed using the COPD Assessment Test and the modified Medical Research Council dyspnea scale) was also associated with “ease of use/suitability of inhaler device” forming part of the prescribing decision (P<0.05; Table 3). However, post-bronchodilator FEV1 was not associated with the physician’s decision to prescribe a device based on ease of use/suitability (P=0.406).
“Ease of use/suitability of inhaler device” was associated with a reason for prescribing in both asthma and COPD for patients with one or more comorbidities (P<0.0001 in each case; see Table S4). Conversely, for patients with no comorbidities, “ease of use/suitability of inhaler device” was associated with “not” being a reason for prescribing in asthma and COPD (asthma P<0.0001; COPD P<0.005; see Table S4). In terms of the current device type being associated with the likelihood of a physician selecting “ease of use/suitability of inhaler device” as a reason for prescribing choice for patients with COPD, no significant difference was found except for the SMI (P=0.1278, P=0.5214, and P=0.0672 for the MDI, baMDI, and DPI, respectively; SMI P=0.0202; see Table S5).
Discussion
This study investigated the prescribing patterns for inhaled maintenance medications among patients with asthma and/or COPD, with particular emphasis on the impact of device type, patient and clinical characteristics, and patient and physician preferences on the choice of inhaler device.
The most commonly prescribed maintenance inhaler device type was a DPI, with this trend most pronounced for patients with COPD. This may have been due, in part, to the wide global availability of DPI maintenance products compared with products for MDIs. The leading LAMA, tiotropium, has, for example, been primarily available in a single-dose DPI to date. The comparatively low numbers of SMIs and baMDIs currently prescribed to patients reflect the fact that they are less widely available and, in the case of an SMI, not approved in all markets.
At the first glance, these observations appear inconsistent with findings from a retrospective evaluation of inhaler sales in Europe between 2002 and 2008, using data from the IMS sales database, in which pMDIs accounted for 47.5% of the total sales (DPIs and nebulizers taking 39.5% and 13% of the market, respectively).16 However, the retrospective evaluation included short-acting β-adrenergic and short-acting anti-muscarinic bronchodilators in the analysis, which are almost exclusively prescribed in an MDI, whereas this study excluded the inhaler type for short-acting bronchodilators. While the pMDI was the most frequently prescribed inhaler for bronchodilators, sales of DPIs and pMDIs were similar for ICSs.16 DPI sales were higher in the case of inhalers with a combined long-acting β-agonist and corticosteroid.16 Overall, the high variability in inhaler prescription between European countries was ascribed not only to differences in health policy, costs, and reimbursement, but also to prescriber and patient preference.
Physician preferences and prescribing decisions
In our study, around two-thirds of physicians stated a preference for inhaler type. Given that physicians were unlikely to prescribe the same medication in two different types of inhaler, it could be that inhaler choice was reflective of underlying prescribing habits rather than a conscious, evidence-based decision. Within specialties, pulmonologists demonstrated some preference for DPIs across all indications compared with other inhaler types, while PCPs and allergists did not establish a consensus on a preferred device. These differences may reflect the type of patient most often encountered in clinical practice, with people seeking, or being referred to specialist care from, a pulmonologist tending to be more severely affected by their disease. Pulmonologists may prescribe more combination products, which are more readily available in DPIs. Despite the increasing number of inhalers available, one-third of physicians stated no current preference for the type of inhaler they prescribe.
Given that medication and inhaler are so often inherently linked, it can be difficult to determine whether the inhaler type truly forms an integral part of the prescribing decision. Examination of physician-reported feedback revealed that the inhaler type influenced prescribing choice for around one-third of patients across indications. The association between increasing age and disease severity (in COPD-only) and the inhaler attribute “ease of use/suitability” is perhaps reflective of the awareness by physicians of the unique physical challenges faced by these patients. Older patients are more likely to have comorbidities as they are more prone to arthritis and general muscle weakness, as well as deficits in vision and cognition, which may limit the viability of certain inhaler types.1 Here, an inverse association was observed between comorbidities and “ease of use/suitability”, meaning that “ease of use/suitability” was less likely to influence prescribing decisions in patients with no comorbidities than in those with comorbidities.
The link between lung function parameters (FEV1 and forced vital capacity) and a patient’s inhalation capacity means that inhalation efficiency is likely to be impaired in severe cases of COPD in which lung function is more heavily compromised.7 Suboptimal peak inspiratory flow rates have been reported in ~20% of patients with advanced COPD >60 years of age using a DPI.6 If the physician is cognizant of this association, they may be more likely to prescribe a pMDI or an SMI, devices that are not reliant on flow rate for optimal delivery of medication. Younger children are also more likely to have reduced inspiratory flow than adults, so may not be able to actuate DPIs.10 This may, in part, explain the greater prescribing levels for pMDIs versus DPIs in patients with asthma (includes patients >12 years), compared with patients with COPD (includes patients >40 years). The absence of an association between asthma severity and prescribing based on the ease of use of inhaler device is perhaps reflective of the limited availability of medications in a range of delivery devices.
Our finding that the ease of use/suitability as a reason for choosing a particular inhaler is linked to time since diagnosis suggests that physicians are prioritizing these device attributes for those patients who have been diagnosed for longer. If a patient is comfortable using an inhaler and is experiencing clinical benefit, they may be reluctant to switch to alternative devices that are less familiar. Non-consensual switching of inhaler device can result in patient discontent, reduced confidence in the medication, and uncertainty regarding the degree of disease control.5 Furthermore, when a patient is non-consensually switched to a new device, they may be more likely to show poor inhalation technique, unless adequate training is provided.17 Physicians are more likely to prioritize other device attributes in more recently diagnosed patients who will not have yet settled into a therapeutic routine and may be more open to change or experimentation.
Patient preference and satisfaction
From the perspective of the patient, the simplicity of the inhaler operating instructions was the attribute of greatest importance across all indications. This finding is consistent with an online survey of patients with COPD and health care professionals, in which ease of use was cited as an important attribute by patients and physicians alike,14 and it highlights the importance of providing patients with simple and easy-to-follow instructions for their device. Studies comparing single-dose and multi-dose DPIs found that patients were more satisfied with, and preferred, multi-dose devices compared to single-dose devices.18–20 In our study, patient prioritization of other inhaler attributes differed according to respiratory condition, with patients with asthma ranking convenience highly (portability and minimal preparation of dose), in contrast to patients with COPD who favored robustness of the inhaler and reliability and reproducibility of dose. Differences between inhaler attribute preferences of patients with COPD and patients with asthma were also noted in a study of 294 patients, wherein those with asthma most valued fewer dose preparation steps, while patients with COPD most valued an inhaler that could be used during episodes of breathing difficulties.21 It is important to recognize the perhaps subtle differences between what patients with asthma and COPD are looking for in an inhaler device.
There was a broad range in the level of satisfaction that patients reported with their inhaler device, with each attribute associated with high and low levels of satisfaction. Typically, patients reported low satisfaction with the feedback mechanism on their inhaler that indicated correct inhalation of medication, and reported irritation of the mouth as an adverse event. Both of these characteristics can be indicative of suboptimal inhaler technique and may suggest that the patient has not been adequately trained in the correct use of the inhaler,1 emphasizing the importance of training patients to improve their inhalation technique.11 It is not clear if patients were dissatisfied with how the feedback mechanism indicated whether the inhalation was correct or not, or if patients were dissatisfied with its lack of availability on all devices. Although it has been reported that patients would prefer an inhaler that provided feedback on their performance after use,22 the feedback mechanism was not ranked as one of the five most important attributes in any patient group in this study.
From the published literature, key drivers of inhaler device preference include ergonomic design, mouthpiece fit, dose counter visibility, and ease of interpretation of the dose counter.23 Lack of dose counter on an inhaler was an issue raised by patients with asthma concerned about not having sufficient medication left in the device.22 These features link closely to the grievances reported in our study, given that a device that patients find comfortable and easy to use would help to improve inhaler technique. It should be recognized that while patients may have preferences for certain inhaler types or functions, they may not have access to them due to reimbursement restrictions operating in their locality. This may lead to a poorer outcome for the patient if the inhaler does not match their preferences and they consequently do not achieve optimal use.
Across patient populations, levels of satisfaction with individual inhaler attributes were broadly similar, with the exception of preloading of the inhaler prior to use. Patients with COPD showed the highest level of dissatisfaction for this feature, which may relate to the common use of single-dose DPIs in this patient group and ties in with the physician-reported preference for ease of use in patients with COPD who have advanced disease severity, as well as the fact that there are both single- and multi-dose DPIs available. If a patient is experiencing difficulties using their device, these are likely to be worsened by the need to reload the device before every use as is required with single-dose DPIs. Published studies reveal higher rates of patient satisfaction with multi-dose over single-dose inhalers and with some, but not all, reporting lower rates of critical inhaler error when using multi-dose devices.18–20 In particular, patients with asthma have been noted as valuing devices with a single dose preparation step compared to numerous steps.21 However, analysis of inhaler technique in patients with COPD and asthma has shown high rates of inhaler error, regardless of whether a preferred inhaler was being used or not,24 or whether the patient was satisfied with their inhaler.22 This emphasizes the importance of correct instruction from the prescribing physician. Previous studies have shown that provision of training can improve competence in inhaler use in patients, with different types of training leading to different levels of improvement. Patients who received training as part of a group were less likely to make errors, with 97% of these patients showing good inhalation technique 6 months after training had been delivered.11
The importance of patient satisfaction with an inhaler device should not be underestimated. In COPD, patient satisfaction with inhaler characteristics is rated more highly than factors such as complexity of medication regimen and severity of symptoms, and is inextricably linked to overall medication adherence or compliance.13 Patient compliance plays a key role in maximizing the efficacy of the medication regimen. Failing to understand the correct use of an inhaler represents a common form of unintentional noncompliance on the part of the patient, which can negatively impact disease control.25 Patients need fewer attempts to learn how to correctly use device types requiring fewer maneuvers prior to actuation, suggesting that such devices are more likely to be used successfully, and that such devices are usually preferred by patients.4
The relationship between satisfaction with inhaler and clinical efficacy may be more complex than it initially appears, with a lack of evidence available for a correlation between these factors.26 A systematic literature review of randomized controlled trials in COPD showed an apparent disconnect between patient satisfaction and improvement in clinical efficacy.27 It, therefore, appears that an individualized approach to device selection should be utilized with consideration to the patient’s ability to effectively use an inhaler.28 Further investigation within real-world treatment settings will help to more clearly delineate the role of the inhaler in treatment outcomes for respiratory conditions. Studies that show benefits to the patients, in addition to improving their satisfaction, will likely strengthen the appeal of these new devices to both patients and physicians alike.
Study limitations
There are some potential limitations associated with this study. While “ease of use” or “suitability” of the inhaler covers a number of device attributes, it may not cover all the attributes a physician considers important. As such, the impact of the inhaler as part of the prescribing decision process may be higher than reported here. It is also important to note that the list of inhaler attributes is not a validated one, although it has been developed by respiratory experts. Furthermore, patients could only rank attributes based on knowledge of inhaler types they currently or previously used, without experience of all available inhaler types. There is also a possibility that other attributes not assessed in the current study were of importance to patients and/or physicians. This study evaluated maintenance inhaler preference only, and a potential difference in preference between maintenance and reliever inhalers was not evaluated. This could be a further area to research in order to understand whether there are any differences in inhaler preference characteristics between maintenance and reliever inhalers. Additionally, inhaler devices are an area of increasing promotion by pharmaceutical companies with the introduction of several new devices since 2013. As the DSPs were conducted between 2010 and 2013, physician preferences could potentially have developed further since the conclusion of our studies; however, this would only affect physician preference and not the other analyses of importance and satisfaction.
Nevertheless, this study offers valuable insight into both physician- and patient-led preferences that could be used to inform the development of next-generation inhaler devices for respiratory disease.
Conclusion
A high proportion of physicians had no preference for the inhaler type, irrespective of the disease state, and when preferences were stated, there was no clear consensus on a particular device type. For patients, the most important attribute of an inhaler was that its instructions were easy and simple to follow. Physicians appeared to be placing most importance on ease of use and suitability of device type when selecting inhalers for older patients and those with more severe disease, particularly in COPD. Given that patients and physicians value ease of use and suitability of device to patient needs (both subjective measures), it is important that a variety of device types are available for all classes of maintenance therapy.
Data sharing statement
The data from this study is not available as open access, but the raw data files can be requested depending on the purpose for obtaining these files. For example, additional analysis using the data would not be permitted unless conducted by Adelphi Real World.
Acknowledgments
Medical writing support, under the direction of the authors, was provided by Thomas Owens PhD and Caroline Shepherd BPharm of CMC CONNECT, a division of Complete Medical Communications Ltd, Macclesfield, UK, funded by AstraZeneca, Cambridge, UK, in accordance with Good Publication Practice (GPP3) guidelines.29 The authors wish to thank James Pike, a senior statistician and employee of Adelphi Real World, who provided analytical support. The study was supported by AstraZeneca. Data in this paper were, in part, presented at the American Thoracic Society International Conference, San Francisco, CA, USA, 13–18 May 2016 as a poster presentation. The poster’s abstract was published in the abstract issue of Am J Respir Crit Care Med 2016;193:A1685: http://www.atsjournals.org/doi/abs/10.1164/ajrccm-conference.2016.193.1_MeetingAbstracts.A1685.
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
BD, GS, and UH are employees of AstraZeneca. MS is an employee of Adelphi Real World. The authors report no other conflicts of interest in this work.
References
Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for Asthma Management and Prevention, Global Initiative for Asthma (GINA) [updated 2015]. Available from: http://www.ginasthma.org/. Accessed June 16, 2016. | ||
Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management and Prevention of COPD [updated 2017]. Available from: http://www.goldcopd.org. Accessed September 8, 2017. | ||
Dolovich MB, Ahrens RC, Hess DR, et al. Device selection and outcomes of aerosol therapy: evidence-based guidelines. American College of Chest Physicians/American College of Asthma, Allergy, and Immunology. Chest. 2005;127(1):335–371. | ||
Dal Negro RW, Povero M. Acceptability and preference of three inhalation devices assessed by the Handling Questionnaire in asthma and COPD patients. Multidiscip Respir Med. 2016;11:7. | ||
Bjermer L. The importance of continuity in inhaler device choice for asthma and chronic obstructive pulmonary disease. Respiration. 2014;88(4):346–352. | ||
Mahler DA, Waterman LA, Gifford AH. Prevalence and COPD phenotype for a suboptimal peak inspiratory flow rate against the simulated resistance of the Diskus® dry powder inhaler. J Aerosol Med Pulm Drug Deliv. 2013;26(3):174–179. | ||
Prime D, de Backer W, Hamilton M, et al. Effect of disease severity in asthma and chronic obstructive pulmonary disease on inhaler-specific inhalation profiles through the ELLIPTA® dry powder inhaler. J Aerosol Med Pulm Drug Deliv. 2015;28(6):486–497. | ||
Laube BL, Janssens HM, de Jongh FHC, et al. What the pulmonary specialist should know about the new inhalation therapies. Eur Respir J. 2011;37(6):1308–1331. | ||
Lavorini F, Mannini C, Chellini E, Fontana GA. Optimising inhaled pharmacotherapy for elderly patients with chronic obstructive pulmonary disease: the importance of delivery devices. Drugs Aging. 2016;33(7):461–473. | ||
Lexmond AJ, Kruizinga TJ, Hagedoorn P, Rottier BL, Frijlink HW, de Boer AH. Effect of inhaler design variables on paediatric use of dry powder inhalers. PLoS One. 2014;9(6):e99304. | ||
van der Palen J, Klein JJ, Kerkhoff AH, van Herwaarden CL, Seydel ER. Evaluation of the long-term effectiveness of three instruction modes for inhaling medicines. Patient Educ Couns. 1997;32(1 Suppl):S87–S95. | ||
Leung J, Bhutani M, Leigh R, Pelletier D, Good C, Sin DD. Empowering family physicians to impart proper inhaler teaching to patients with chronic obstructive pulmonary disease and asthma. Can Respir J. 2015;22(5):266–270. | ||
Chrystyn H, Small M, Milligan G, Higgins V, Gil EG, Estruch J. Impact of patients’ satisfaction with their inhalers on treatment compliance and health status in COPD. Respir Med. 2014;108(2):358–365. | ||
Molimard M, Colthorpe P. Inhaler devices for chronic obstructive pulmonary disease: insights from patients and healthcare practitioners. J Aerosol Med Pulm Drug Deliv. 2015;28(3):219–228. | ||
Anderson P, Benford M, Harris N, Karavali M, Piercy J. Real-world physician and patient behaviour across countries: disease-specific programmes–a means to understand. Curr Med Res Opin. 2008;24(11):3063–3072. | ||
Lavorini F, Corrigan CJ, Barnes PJ, et al. Retail sales of inhalation devices in European countries: so much for a global policy. Respir Med. 2011;105(7):1099–1103. | ||
Roggeri A, Micheletto C, Roggeri DP. Inhalation errors due to device switch in patients with chronic obstructive pulmonary disease and asthma: critical health and economic issues. Int J Chron Obstruct Pulmon Dis. 2016;11:597–602. | ||
Pascual S, Feimer J, De SA, et al. Preference, satisfaction and critical errors with Genuair and Breezhaler inhalers in patients with COPD: a randomised, cross-over, multicentre study. NPJ Prim Care Respir Med. 2015;25:15018. | ||
van der Palen J, Ginko T, Kroker A, et al. Preference, satisfaction and errors with two dry powder inhalers in patients with COPD. Expert Opin Drug Deliv. 2013;10(8):1023–1031. | ||
van der Palen J, van der Valk P, Goosens M, Groothuis-Oudshoorn K, Brusse-Keizer M. A randomised cross-over trial investigating the ease of use and preference of two dry powder inhalers in patients with asthma or chronic obstructive pulmonary disease. Expert Opin Drug Deliv. 2013;10(9):1171–1178. | ||
Hawken N, Torvinen S, Neine ME, et al. Patient preferences for dry powder inhaler attributes in asthma and chronic obstructive pulmonary disease in France: a discrete choice experiment. BMC Pulm Med. 2017;17(1):99. | ||
Jahedi L, Downie SR, Saini B, Chan HK, Bosnic-Anticevich S. Inhaler technique in asthma: how does it relate to patients’ preferences and attitudes toward their inhalers? J Aerosol Med Pulm Drug Deliv. 2017;30(1):42–52. | ||
Svedsater H, Dale P, Garrill K, Walker R, Woepse MW. Qualitative assessment of attributes and ease of use of the ELLIPTA dry powder inhaler for delivery of maintenance therapy for asthma and COPD. BMC Pulm Med. 2013;13:72. | ||
Chorão P, Pereira AM, Fonseca JA. Inhaler devices in asthma and COPD–an assessment of inhaler technique and patient preferences. Respir Med. 2014;108(7):968–975. | ||
Rau JL. Determinants of patient adherence to an aerosol regimen. Respir Care. 2005;50(10):1346–1356. | ||
Levy ML, Dekhuijzen PN, Barnes PJ, et al. Inhaler technique: facts and fantasies. a view from the Aerosol Drug Management Improvement Team (ADMIT). NPJ Prim Care Respir Med. 2016;26:16017. | ||
Ninane V, Vandevoorde J, Cataldo D, et al. New developments in inhaler devices within pharmaceutical companies: a systematic review of the impact on clinical outcomes and patient preferences. Respir Med. 2015;109(11):1430–1438. | ||
Dekhuijzen PN, Lavorini F, Usmani OS. Patients’ perspectives and preferences in the choice of inhalers: the case for Respimat® or HandiHaler®. Patient Prefer Adherence. 2016;10:1561–1572. | ||
Battisti WP, Wager E, Baltzer L, et al. Good publication practice for communicating company-sponsored medical research: GPP3. Ann Intern Med. 2015;163(6):461–464. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.