Back to Journals » Risk Management and Healthcare Policy » Volume 14
Magnitude of Self-Reported Syndromes of Sexually Transmitted Infections and Its Associated Factors Among Young Incarcerated Persons (18–29 Years) in Correctional Facilities of Gamo Gofa Zone, Southern Ethiopia
Authors Getachew M, Haile D , Churko C , Alemayehu Gube A
Received 5 October 2020
Accepted for publication 10 December 2020
Published 6 January 2021 Volume 2021:14 Pages 21—29
DOI https://doi.org/10.2147/RMHP.S285289
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Marco Carotenuto
Muluken Getachew,1 Dereje Haile,2 Chuchu Churko,3 Addisu Alemayehu Gube4
1Gofa Zone Health Department, Gofa, Southern Ethiopia; 2Reproductive Health and Nutrition Department, School of Public Health, College of Medicine and Health Sciences, Wolaita Sodo University, Sodo, Southern Ethiopia; 3Department of Public Health, School of Public Health, College of Medicine and Health Science, Arba Minch University, Arba Minch, Southern Ethiopia; 4Department of Public Health, College of Medicine and Health Science, Dilla University, Dilla, Southern Ethiopia
Correspondence: Dereje Haile Email [email protected]
Background: Sexually transmitted infection is an infection that is typically transmitted by sexual contact and may either end or develop into a sexually transmitted disease. Today, young people are recognized as groups with special health-related vulnerabilities like drug use, unprotected sex and sexually transmitted infections. Despitea number of strategies which focused on young people’s health, there was limited evidence of sexually transmitted infection among young incarcerated persons. Thus, the aim of this study was to assess the self-reported syndromes of sexually transmitted infections and associated factors among young incarcerated persons (18– 29 years) in correctional facilities of the Gamo Gofa Zone, Southern Ethiopia.
Methods: A facility-based cross-sectional study was conducted from March 1 to 15, 2019. Simple random sampling was used to select a total of 414 prisoners. The data were entered into Epi.info version 7 and exported and analyzed using SPSS version 20. Bivariate and multivariate logistic regression analysis were carried out. Statistical significance was declared by using the p value of < 0.05 at 95% confidence interval.
The Results: In this study, 403 respondents participated with the response rate of 97.3%. The overall prevalence of self-reported STIs was 35 (8.7%). STI syndromes before incarceration (AOR: 5.267 (95% CI: 1.863, 14.893)), not having family support (AOR; 6.645 (95% CI: 2.327, 18.975)), history of imprisonment (AOR; 2.871 (95% CI: 1.065, 7.42)), not always using condom (AOR; 7.417, (95% CI 2.526, 21.781)), alcohol use (AOR; 5.926, (95% CI 2.282, 15.392)), chat use (AOR; 4.736, (95% CI (1.387, 16.172)) and having sex with commercial sex workers (AOR; 2.764, (95% CI 1.034, 7.388)) were significantly and independently associated with self-reported STIs.
Conclusion: Prevalence of self-reported syndromes of STI was high. Attention is needed about sexually transmitted infections for incarcerated young people by concerned bodies, including governmental and non-governmental organizations.
Keywords: STI, sexually transmitted infection, young, prison, Ethiopia
Background
Sexually transmitted infection (STI) is an infection that is typically transmitted by sexual contact and may either end or develop into a sexually transmitted disease (STD).1,2
There are three approaches to STI case management; these are etiologic, clinical and syndromes. Syndromic management is based on the identification of a group of symptoms and easily recognized signs associated with well-defined pathogens. The commonly known syndromes include: urethral discharge, genital ulcer, vaginal discharge, lower abdominal pain in women, inguinal bubo, scrotal swelling, and neonatal conjunctivitis.3
Worldwide, more than 1 million sexually transmitted infections (STIs) are acquired every day.4,5 Besides, globally, young populations make up only one fourth of the sexually active population, but they acquire 50% of all STIs.6 Moreover, young incarcerated persons were more at risk because of high rates of sexual activity, more sex with at-risk partners, earlier initiation of sexual behavior, and less condom use.7–9 The latest World Health Organization estimate indicates that one in 20 young people is believed to contract STI each year.10
STI has a number of long term effects on health like ectopic pregnancy, cervical cancer, infertility and neonatal and infant deaths.11,12 Moreover, based on some evidence, younger population groups (18–29), are faced with different problems like STIs, early pregnancy, STIs/AIDS, drug abuse, and unemployment.13 Developing STIs highly increases the transmission of HIV. This interrelatedness contributed to 40% or above related to HIV acquiring.11
Ethiopia has been implementing a syndrome based approach since 2001 by adopting the WHO generic guidelines to serve as a national guideline for the management of STIs, which is reducing the duration of patients’ infectiousness and decreases the incidence and prevalence of STIs in the population.3
In addition, recently there was a universal sustainable development goal-3, which targets ending communicable disease, including, STI, AIDS, and TB by 2030.14 Ethiopian government has initiatives in the plan of HSTP which focused provision of maternal, neonatal, child, and young health services.15 Moreover, the Ethiopian national reproductive health strategy 2016–2020 revealed that strengthening the integration of STI/HIV prevention, detection and treatment in reproductive, maternal, newborn, adolescents and youth health service is one of the guidelines developed by the concerned bodies to reduce STI related morbidity and mortality.16
Evidences on STIs among incarcerated young people are limited in Ethiopia, therefore conducting research on STIs in general and among young people in particular in prison is an important input to design policy and strategy aimed at preventing and controlling sexually transmitted infections. In Ethiopia, few studies have been conducted regarding STIs prevalence among young persons and associated factors. Therefore, this study was aimed to assess the prevalence of self-reported sexually transmitted syndrome and associated factors among young incarcerated persons in the Gamo Gofa Zone, Southern Ethiopia.
Methods and Materials
Study Area and Period
The study was conducted in all Gamo Gofa Zone correctional facilities. In the zone, there are three prisons: Arbaminch, Chencha and Gofa. There is a total of 4642 individuals in the correctional facilities, out of which 231 were females. There were clinics in all prisons in the zone. The study was conducted from March 1–15, 2019.
Study Design
A facility based cross sectional study design was used.
Populations
All young incarcerated persons (18–29 years) in all Gamo Gofa Zone prisons were considered as source population. The study populations selected were all young incarcerated persons in all prisons.
Eligibility Criteria
Prisoners who are in the age group 18–29 years old and detained for two months or more were included in this study, whereas prisoners who were critically ill or have psychiatric problems, and those unable to read and write, were excluded from the study.
Sample Size Determination
For the first objective, the sample size was calculated by using single population proportion formula, by using the following assumptions 95% confidence interval, the degree of precision 5%, the prevalence of STIs from Gonder study, 13.7%,17 none response rate of 15% which gives a sample size of 209.
However, to obtain maximum sample size, double population proportion formula was used by taking P1 about 37.5% and AOR =1.86, power of 80%, which gives sample size of 360 but after adding non-response rate of 15%, the final sample size was 414.17
Sampling Procedure
All the prisons in the Gamo Gofa zone were identified and the total number of the prisoners per each prison was defined. The total sample size was proportionally allocated to all prisons. To select the young incarcerated person who fulfill the inclusion criteria from registration, the simple random sampling method was used by using computer generated numbers. Thus, 201 respondents from Arbaminch prison, 53 from Chencha prison, and 160 from Gofa prison were included in this study.
Dependent Variables
Self-reported STI Syndromes (yes/no).
Independent Variables
Age, sex, residence, occupation, family support, level of education and income.
Alcohol use, chat use and selling drugs for primary income.
History of sexual intercourse, access to information, history of STIs, age of first intercourse, and previous imprisonment.
Contact with commercial sex workers (CSW), inconsistent use of condoms, unsafe sex, practicing sex with a commercial sex worker and having multiple sexual partners.
Period of confinement and previous imprisonment.
Definitions and Measurement of Variables
Self-Reported Syndromes of STIs
For this study, one or more of the following syndromes: urethral discharge in men, genital ulcer, vaginal discharge, lower abdominal pain in women, inguinal bubo (swelling in groin region), and scrotal swelling.3
Young Incarcerated Persons
The population in the age group 18–29 years old among inmates confined in a prison or correctional facility.
Data Collection Procedure (Instrument, Personnel)
Six clinical nurse health professionals who have prior experience in data collection collected the data. Three public health officers from the different Woreda Health Facilities supervised data collectors daily. All data collectors and supervisors were trained adequately in one day and performed practical exercises to be familiar with the questionnaire. The study participants were informed by the data collectors about their voluntary participation, purpose of the study with its importance as well as the significance of true information provision and confidentiality issues.
Data Quality Management
The data were collected using pre-tested structured self-administered questionnaires. The questionnaire was developed and adapted from EDHS 2016 and other published literature. Pre-testing was done in 5% population out of the study area (Wolayita Sodo prison). In addition, the data collector ensured their data collection procedure. The completeness of daily data collection was cheeked by supervisors every day. It was initially prepared in English. The English version was translated to the Amharic local language and back translated to English by language experts to ensure consistency. The developed questionnaire was evaluated by an experienced researcher. Follow up was also made to them during data collection. Moreover, the overall data collection process, its completeness and correctness was made by the supervisors and principal investigator.
Data Processing and Analysis
The data were coded, cleaned and entered into Epi-Info version 7 and exported to statistical package for social science (SPSS) version 20.0 for analysis. Descriptive statistics including graphs, charts, tables and proportion was used to describe the data. Bivariate and multivariable logistic regression was performed to see the association between outcome and explanatory variables. Variables that are found to be statistically significant in the bivariate analysis (p-value <0.25) were entered into the multivariable logistic regression model. Finally, multivariable logistic regression analysis was done to identify factors associated with self-reported syndromes of STIs of young people. An effort was made to assess whether the necessary assumptions for the application of multivariable analysis was fulfilled. Adjusted odds ratio along with 95% Confidence Interval (CI) and p-value less than 0.05 were used to assess the significance level between explanatory variables and self-reported STI prevalence.
Ethical Considerations
Ethical approval was obtained from an ethical review committee of Arbaminch University, College of Medicine and Health Sciences. Following the approval, official letter of co-operation was written to concerned bodies by the department of Public Health of Arbaminch University. Explanation of the objective of the research was provided to the concerned personnel at Zonal level. Support letter submitted to prison was obtained from the Zonal Security Department to prisons. Finally, the data were collected after assuring the confidential nature of responses and obtaining oral consent from the respondents. All the study participants were encouraged to participate in the study and at the same time they were ensured that they have the right not to participate. Moreover, the participants were informed about the purpose of the study. We confirmed that the study was conducted in accordance with the Declaration of Helsinki.
Result
Socio-Demographic Characteristics of the Respondents
From out of 414 samples a total of 403 respondents filled the questionnaire with the response rate of 97.3%. The majority of the respondents, 224 (55.6%), were in the age group of 24–29 years, 171 (42.4%) were from orthodox religion, and 217 (53.8%) were Gamo ethnic group. The majority, 199 (49.4%) of the respondents had educated grade (5–8), 239 (59.3%) were unmarried, and 321 (79.7%) did not have income. Nearly one fourth of respondents reported that they live alone before incarceration (95, 23.6%). Around one third, 242 (60%), were unemployed (Table 1).
 |
Table 1 Socio-Demographic Characteristic of Self-Reported Syndromes of STIs Among Young Incarcerated Persons (18–29 Years) in Correctional Facilities of Gamo Gofa Zone, Southern Ethiopia. March, 2019 |
Prison Condition of the Study Subjects
This study revealed that 79 (19.6%) of the respondents stayed in the current prison for 3–10 months, 129 (32%) stayed for 11–20 months, 195 (48.4%) stayed for more than 20 months. A majority of respondents, 281 (69.7%), reported that 111 and above inmates live in one room, while only 51 (12.7%) respondents reported that 27–47 inmates live in one room. Out of all partners responded, 57 (14.1%) reported that they spend none of the time outside their prison area, while 48 (11.9%) spend more than two hours outside the prison area. The majority of participants, 220 (54.6%), were sleeping alone with own bed/mattress on the floor, where as 183 (45.4%) sleep with inmates together in a group on the mattress. Most of the respondents, 162 (40.2%), reported that they do not have family support, and 276 (68.5%) had a history of imprisonments (Table 2).
Behavioral Characteristics of the Respondents
This study showed that 43 (10.7%) of the respondents had never had sexual intercourse, 360 [89.3%] had ever had sexual intercourse. Regarding age at first sex, 299 (74.2%) had first sex at age 15–19 and 61 (15.1%) had first sex at age 20–24 years; 274 (68%) of the respondents had first sex with boy/girlfriends where as 5 (1.2%) were with commercial sex workers. Before incarceration, 118 (29.3%) of the respondents had ever had sex with commercial sex workers and the other 285 (70.7%) had never had sex with a commercial sex worker. Concerning condom use, 186 (46.2%) reported that their partner used a condom every time during sex whereas 217 (53.8%) did not use.
Before incarceration, a majority (225, 55.8%) of the respondents had ever used chat, and 121 (30%) of the respondents had ever used alcohol, whereas 178 (44.2%) and 282 (70%) did not use chat and alcohol respectively (Table 3).
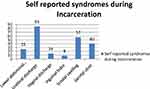
Prevalence of Self-Reported Syndromes of STIs
The overall prevalence of self-reported STI syndromes was 35 (8.7%) (95% CI: 6.0%, 11.4%). Out of syndromes of STIs during incarceration, 9 (25.7%) said lower abdominal pain, 20 (57.1%) said scrotal swelling, 3 (8.6%) said inguinal bubo, 30 (85.7%) said urethral discharge, 5 (14.3%) said have a vaginal discharge and 14 (40%) said have genital ulcers during incarceration (Figure 1).
Factors Associated with Self-Reported STI Syndromes
During bivariate analysis, factors like sex, marital status, living condition before incarceration, work before incarceration, duration of confinement in current prison, sleeping situation, no family support, history of imprisonment, get information, not using condoms every time during sexual intercourse, alcohol use, multiple partner, commercial sex and STI syndromes before incarceration had p-value 0.20 and less.
In multivariable logistic regression analysis, history of STI syndromes before incarceration, not having family support, history of imprisonment, not using condoms consistently, alcohol use, chat use, and having sex with commercial sex workers was associated with self-reported STI syndromes.
Those participants who have STI syndromes before incarceration were 5 times more likely to have STI syndromes during incarceration when compared to those who did not have a history of STI syndromes before incarceration [AOR: 5.267 [95% CI: 1.863, 14.893]].
Respondents who do not have family support were 6.6 times more likely to have self-reported STI syndromes compared to those supported by family [AOR; 6.645 [95% CI: 2.327, 18.975].
A participant who had a history of imprisonment before was 3 times more likely to have self-reported STI syndromes compared to participants who have no history of imprisonment [AOR; 2.871 [95% CI: 1.065, 7.42]].
According to this study, participants who did not use condoms every time during sexual intercourse were 7.4 times [AOR; 7.417, 95% CI [2.526, 21.781] more likely to have self-reported STI syndromes compared to partner who uses a condom during sexual intercourse.
A participant using chat and alcohol before incarceration were 4.8 and 6 times more likely to have self-reported STI syndromes compared to those participants who did not use chat and alcohol before incarceration [AOR; 4.736, 95% CI (1.387, 16.172)] and [AOR; 5.926, 95% CI (2.282, 15.392)] respectively.
A participant who practices sex with commercial sex workers was 2.7 times more likely to have self-reported STI syndromes when compared to those who did not practice sex with commercial sex workers [AOR; 2.764, 95% CI [1.034, 7.388]] (Table 4).
 |
Table 4 Factors Associated with Self-Reported STI Syndromes Among Young Incarcerated Persons (18–29 Years) in Correctional Facilities of Gamo Gofa Zone, Southern Ethiopia, 2019 |
Discussion
In this study, the prevalence of self-reported STI syndromes among young incarcerated prisoners was 8.7%. This finding was higher than studies conducted in Hawassa Tabor prison in southern Ethiopia (3.8%),18 and Malawi (4.2%).19 This might be due to variation in the study period and socioeconomic difference. However, this finding was lower than study conducted in Gondar.17 This might be due to the difference in health education and prevention interventions among the study areas. But in line with a study conducted in Addis Ababa (9.2%).20
According to this study, respondents who did not have family support were 6.6 times more likely to have self-reported STI syndromes compared to those who had family support. In contrast, in a study done in Addis Ababa, there was no association between family support and STI syndromes.20 This finding implies that the government should focus availability and its implementation of behavioral change communication at the prison. Moreover, they should avail health education sessions on parenting style to parents through community health extension workers at the community level and through min-media at school level for young people. This might be due to families who support the study participants advising them and giving mental rest leading to good hopes for the future life of the respondents.
Participants who had been imprisoned before were 3 times more likely to have self-reported STI syndromes when compared to participants who have no history of imprisonment. This is in line with a study conducted in Gondar Town.17 This might be due to the risk taking behaviors among young people and the presence of a history of high risk behaviors among inmates before their detention. This finding implies that the government should avail exit and entry screening of prisoners for STIs at all prisons. The policy makers and other concerned bodies should consider its availability. Moreover, this finding indicated that the need of strong STI management at the prison and availability of strong linkage between prison and public health facilities.
Consistent use of condoms determines the level of self-reported STI syndromes. Individuals who did not use condoms every time during sexual intercourse were 7.4 times more likely to have STIs when compared to particitpants who use a condom during sexual intercourse. This study agrees with a study done in Hawassa Tabor prison.18 The reasons might be due to the clients refused to use condoms, having sex using condom with regular and non-paying partners do not feel comfortable. This finding is also supported by the recommendation for those young persons not abstaining from sex and cannot have a mutually faithful relationship.21
Partners who use chat before incarceration were 4.7 times more likely to have STI syndromes when compared to those who did not use chat and alcohol users were 6 times more likely to be affected by STI syndromes than those who did not use alcohol. This finding was similar to the findings of a study done in Hawassa Tabor prison.18 The reason might be increased alcohol and chat use was more likely to engage in unsafe sex, multiple sexual partnerships, rape and early initiation of sex.
In this study partners who practice sex with commercial sex workers were 2.8 times more likely to have self-reported STI syndromes when compared to those who did not practice sex with commercial sex workers. In contrast, sex with commercial sex workers was not significant in a study conducted in Hawassa Tabor prison.18 The reason might be due to commercial sex workers being highly prone to STI syndromes than any other person and having sex with those people will transmit the syndromes. This finding implies that the need of availing routine education session at the prison on safe sex practice and dangers of unsafe sex.
Strength and Limitation of the Study
Since there is no study conducted in the study area, this research is the first of its kind. The limitation of this study is social desirability bias due to highly sensitive questions related to sexuality, which may lead to an underestimate of the actual prevalence. Recall bias and information bias may be another limitation. The other limitation of this study was excluding those participants who were unable read and write. Moreover, since this study was cross sectional, it may not allow for the establishment of a causal link to self-reported syndrome of STI.
Conclusion
The prevalence of self-reported syndromes of STI in the study area was high. The factors no family support, history of imprisonment, not using condom every time, chat use, alcohol use, STI syndromes before incarceration and sex with commercial sex worker were significantly associated with self-reported STI syndromes during incarceration. Special attention should be given to prison to end communicable disease like STI. Moreover, health education strategies that target parenting style of the family and behavioral change communication should be considered in the correctional facilities.
Abbreviations
AOR, adjusted odds ratio; WHO, World Health Organization; STD, sexually transmitted syndrome; STI, sexually transmitted infection; TB, tuberculosis.
Data Sharing Statement
The data used to support the findings of this study are available from the corresponding author upon request with an email address of [email protected].
Acknowledgment
We are thankful to the Arba Minch University, College of Medicine and Health Sciences for providing ethical clearance for this study. Gratitude also goes to our data collectors, supervisors, and the study participants.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No funding was obtained.
Disclosure
The authors report no conflicts of interest for this work and declare that there is no conflict of interest regarding the publication of this paper.
References
1. Gisela K. Requirements for healthy development of adolescent youth. Adolescence. 1973;8(31):24.
2. Shim BS. Current concepts in bacterial sexually transmitted diseases. Korean J Urol. 2011;52:589–597.
3. Health FDRoEMo. National Guidelines for the Management of Sexually Transmitted Infections Using Syndromic Approach. July, 2015.
4. WHO. Report on Global Sexually Transmitted Infection Surveillance, 2018. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO]. 2018.
5. Rowley J, Vander Hoorn S, Korenromp E, Low N, et al. Global and regional estimates of the prevalence and incidence of four curable sexually transmitted infections in 2016. WHO Bulletin. 2019.
6. Butler P. Progress in Reproductive Health Research. UNDP/UNFPA/WHO/World Bank Special Program of Research Training in Human Reproduction (HRP) Department of Reproductive Health. Vol. 64. Geneva, Switzerland: World Health Organization; 2008.
7. Morris RE, Harrison EA, Knox GW, et al. Health risk behavior survey from 39 juvenile correctional facilities in the United States. J Adolesc Health. 1995;17:334–344.
8. Crosby R, DiClemente R, Wingood G, Rose E, Levine D. Adjudication history and African American adolescents’ risk for acquiring sexually transmitted disease. Sex Transm Dis. 2003;30.
9. WHO. Report on Global Sexually Transmitted Infection Surveillance. 2015.
10. WHO. Global prevalence and incidence of selected curable sexually transmitted infections. 2014. Available from: http://appswhoint/iris/bitstream/10665/75181/1/9789241503839_engpdf?ua=1.
11. WHO. Global Strategy for the Prevention and Control of Sexually Transmitted Infections: 2006–2015. 2007.
12. CDC. Reported STDs in the United States. 2016.
13. HIV and Sexual Behavior Among young South Africans. National survey of 15–24 years old. University of Witwatersrand and Accessed on 17/23/2005.
14. NATIONS U. Transforming our world: the 2030 agenda for sustainable development. 2015/2016.
15. Health FMo. Health Sector Development Programme IV 2010/11–2014/15. 2010.
16. FMOH. National RH Strategy. October, 2016.
17. Berihun BTA. Prevalence of sexually transmitted diseases and associated factors among prisoners in Gondar town, North West Ethiopia. Institution Based Cross Sectional Study. 2014;5(1):3874–3878.
18. Zewdie BSO. Assessment of magnitude of sexually transmitted infections, sexual and reproductive health status among prisoners aged between 18–49 years in Tabor Prison, Hawassa, Ethiopia. Momona Ethiop J Sci. 2016;8(1):89–97.
19. Zachariah R, Harries AD, Chantulo AS, Yadidi AE, Nkhoma W, Maganga O. Sexually transmitted infections among prison inmates in a rural district of Malawi. Trans R Soc Trop Med Hyg. 2002;96(6):617–619.
20. Alem A. Assessment of Sexual and Reproductive Health Problems Among Prisoners Aged 15–29 Years in Addis Ababa. August 24, 2009.
21. FMOH. Prevention and Control Strategies of HIV/AIDS/STIs in Ethiopia. 2015/2016.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.