Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 12
Magnitude of Opportunistic Infections and Associated Factors Among HIV-Positive Adults on ART at Selected Public Hospitals in Sidama National Regional State, Southern Ethiopia
Received 3 June 2020
Accepted for publication 9 September 2020
Published 28 September 2020 Volume 2020:12 Pages 479—487
DOI https://doi.org/10.2147/HIV.S265274
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Bassel Sawaya
Demelash Wachamo,1 Fisseha Bonja2
1Department of Public Health, Hawassa College of Health Sciences, Hawassa, South Nations and Nationalities Peoples’ Region, Ethiopia; 2Department of Medical Laboratory, College of Medicine and Health Sciences, Hawassa University, Hawassa, Ethiopia
Correspondence: Demelash Wachamo Department of Public Health
Hawassa College of Health Sciences, P.O. Box 84, Hawassa, South Nations and Nationalities Peoples’ Region, Ethiopia
Email [email protected]
Background: Opportunistic infections are late complications of HIV infection due to the depletion of the immune system. It is a major public health problem and high morbidity AIDS patients die of AIDS-related infections in developing countries like Ethiopia. Identification of opportunistic infections (OIs) is important to develop a specific intervention. Therefore, the aim of this study was to assess the burden and associated factors of opportunistic infections.
Methods: A facility-based cross-sectional study was conducted on 420 randomly selected HIV/AIDS patients taking anti-retroviral therapy. Data were collected from selected hospitals in Sidama Regional State based on population proportion to size. Data were collected by a pre-tested questionnaire and a pre-tested checklist from the medical records of patients. Data were entered and analyzed for descriptive and logistic regression models by SPSS v.23. The result declared as statistically significant at p < 0.05.
Results: The magnitude of opportunistic infections was 39.6%. Major identified OIs were oral candidiasis 23.2%, recurrent bacterial pneumonia 21.5%, herpes zoster 6.3%, and pulmonary tuberculosis 6.0%. The magnitude of opportunistic associated with older age [AOR=3.50, 95% CI:1.85, 6.61], no formal education [AOR=4.54, 95% CI:1.81, 11.37], initial CD4 count less than 200 cells/mm3 [AOR=3.10, 95% CI:1.61, 5.96], who interrupt ART medicines [AOR=3.21, 95% CI:1.86, 5.56] and khat chewing [AOR=4.24, 95% CI:2.07, 8.68] when compared to their counterparts.
Conclusion: The overall magnitude of opportunistic infections was high when compared with other studies. Health officials and clinicians need to give attention to the strengthening of the provision if ART with prophylaxis on early stage and adherence, implementation of the TB/HIV collaboration activity, and early initiation of ART to reduce opportunistic infections.
Keywords: opportunistic infection, HIV/AIDS, WHO clinical stage, Sidama, Ethiopia
Background
Human immune virus (HIV/ADIS), with which 36.7 million people were living and 2.1 million infected at the end of 2016, has been a major health problem throughout the world.1 Around 36.7 million people worldwide are currently living with HIV, of which 52% reside in sub-Saharan Africa (SSA).2 It affected 1 in every 25 Adults (4.4%) is living with the deadly virus, account for nearly 70% of the global burden of HIV.3,4 Although the natural history of HIV inclines to be similar, the patterns of OIs that mainly presented with different clinical manifestation regions to the region.5,6 CDC estimates that in 2015, 15% of the people with HIV in the United States were unaware or asymptomatic of their infections.7,8 The commonly reported opportunistic diseases in sub-Saharan Africa among HIV patients are Candidiasis, Pneumocystis carinii pneumonia (PCP), disseminated Mycobacterium avium complex (MAC) infection, Cryptococcus, Kaposi sarcoma, herpes zoster, and tuberculosis.9,10
The developing countries more suffer from bacterial and protozoal infections due to lack of resources,10,11 HIV diagnosis, poor adherence to Anti-Retroviral Treatment (ART), drug resistance, poverty, poor nutrition, and high exposure to infectious agents.12 The opportunistic infections may favor HIV replication and higher viral loads that lead to lower the quality of life of HIV-infected persons, reduces patients’ response to ART, increases stigma and limit one’s ability to work, high medical care costs, and death.13,14
In Ethiopia, the adult HIV prevalence of Ethiopia was estimated to be 1.1% in 2015, and the second leading cause of death.15 More than 90% of HIV/AIDS deaths are attributable to opportunistic infections and malignancies.11 Even though nationally representative and comprehensive data regarding the magnitude of opportunistic infections lack in Ethiopia, some regional studies have shown the prevalence ranging from 19.7% to 48%.14,16 The prevalence of OIs among HIV patients on ART is still high namely; oral candidiasis 11.8%, followed by chronic diarrhea, 9.9% and tuberculosis 9.7% at Debre Markos referral hospital in Ethiopian.17 Which associated with age, WHO stages of III and IV, chew khat, ART adherence, low level of hemoglobin, and recent weight.17 Hence, it is very important to see the magnitude of opportunistic infections and its determinant factors to reduce the burden. This is important for researchers, clinicians, and health planners.
Methods
Study Setting and Study Population
This study was conducted at Leku, Bona and Yirgalem Hospitals in the Sidama Regional State in southern Ethiopia from February 01, 2019, up to May 01, 2019, which is one of the most densely populated areas in Ethiopia. Former Sidama Zone or current Sidama Regional State located about 275 kilometers away from Addis Ababa. Sidama has a variety of climatic conditions. Warm conditions cover 54% of the area. There are only three well-organized ART facilities at the hospital level. The source of populations were all HIV/AIDS patients who visited the ART clinic of the three hospitals in the Sidama Regional State. All HIV-positive adults who had at least one month follow up on ART unit at selected hospitals within the study period was considered as the study population. All randomly selected HIV-positive adults aged 18 years old and above and who can give informed consent were included in the study. While all adults with HIV/AIDS who, are unable to hear or unable to communicate were excluded from the study. After excluding HIV-infected adults who had incomplete baseline information (CD4 count, WHO clinical stage, diagnosis of OIs) as incomplete records, records of 414 participants were met the criteria and included in the study. Data were extracted from the charts of 414 participants HIV-infected adults on ART.
Sample Size and Sampling Technique
The study was conducted on 420 calculated by a single population proportion formula by taking previously conducted prevalence of opportunistic infections in Debre Markos Referral Hospital, Northwest Ethiopia17 and 10% possible non-response rate.
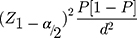
n – Sample size.
Z – Standard normal distribution value at the 95% CI, which is 1.96.
P – The prevalence of Opportunistic infections 45.3%
D – The margin of error, taken as 0.05. Hence,
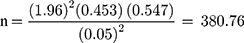 , The final sample size was adjusted as follows:
, The final sample size was adjusted as follows:
Sample size = n (sample size) + (10% non-respondent)
Thus, final sample size (n) was calculated as n = 380.76 + 38.76 = 419.52 ≈ 420.
The stratified sampling technique was used in three ART hospitals. The desired number of sample size from each hospital was selected based on proportional sampling. Individual study participants were selected from each hospital were selected by the random arrival of the ART unit.
Study Variables
The dependent variable of the study was Magnitude of opportunistic infections (diagnosed at least one or more opportunistic infections; any infections of bacteria, viruses, fungi, Parasitic or protozoa or multiple infections reported on their medical record). Independent variables measured in the study were socio-demographic characteristics such as; age, sex, marital status, educational level, occupation, income. Additionally, we collected data on variables measured in the study were Environmental Factor (housing condition, ownership and type, waste refuse, drinking water availability, living with domestic animal and pets, and latrine utilization). Behavioral and Other Factor (hand washing practice, smoking, alcohol use, disclosure status, spouse treatment status, regimen adherence). Individual health-related factors from medical record (Dx for OIs, Co-morbidities, counselling/education received, recent CD4 count, previous CD4 count, taking ART Taking prophylaxis, WHO clinical stage, side effect and adverse reaction reports)
Data Collection Tools, and Procedures
Data were collected by face to face interviews by using a pre-tested questionnaire; a pre-tested checklist to collect information regarding OIs and patients’ clinical records were reviewed. A pre-tested structured questionnaire was utilized to collect socio-demographic characteristics, another clinical information, and other risk factors. The questionnaires were pre-tested and validated before two weeks in the study time in Dore Bafana primary hospital on 5% of HIV positive patients who attend ART clinic which was outside of the study area and some modifications on sequence and arrangement of multiple answer questionnaire were made. Data collectors were five clinical nurses supervised by one BSC nurse supervisor and investigators. Training and practical demonstrations on interview techniques and document extraction procedures based on the checklist were given to data collectors for two consecutive days assessed for competency.
Data Quality Control Measures
Data collectors were trained and the questioners were pre-tested before the study time in similar settings which are not a part of the study area. After the data collection process, the data were checked for completeness and any incomplete or misfiled questionnaires filed again.
Data Analysis
Data entry, cleaning, and analysis were done by SPSS V. 23. Descriptive analysis including frequency distribution and the percentage was made to determine the magnitude of the opportunistic infections, to describe socio-demographic and clinical characteristics. All factors were checked by bivariable logistic regression analysis, the variables with p-value <0.25 are candidates for multiple logistic model to control confounding effects. The Hosmer-Lemeshow goodness-of-fit statistic was used to assess whether the necessary assumptions for the application of multiple logistic regression are fulfilled. Adjusted odds ratios (AOR) with 95% Confidence Intervals (CI) were calculated. Finally, p-value <0.05 declared a significant association.
Terms and Definitions
Opportunistic infection: If the study participant diagnosed at least one or more opportunistic infections; any infections of bacteria, viruses, fungi, Parasitic or protozoa or multiple infections reported on their medical record.7
Adverse effect: an unwanted effect caused by the administration of drugs. Onset may be sudden or developed over time.
Current alcohol consumption: is defined as the use of alcohol at least once during the past 30 days before the survey.
Khat chewing: is defined as the study participants who had chewed the leaves of Khat (Catha edulis) in the last 30 days.
Cigarette smokers: are defined as individuals who had used smoke cigarettes form of tobacco in the last 30 days.18
Results
A total of 420 HIV-positive adults were enrolled in the study in the ART clinic of the selected three hospitals, 414 participants were interviewed yielding a response rate of 98.57%. More than half of the studied participants 234 (56.5%) were female and 171 (41.3%) in the age category of 25–34 years old. The majority of 259 (62.6%) were married and 264 (63.8%) were living with their families. Regarding educational status, 25 (6.0%) have no formal education, 102 (24.6%) had a primary school, and 287 (69.3%) had high school and above education. The working status of the participants 278 (67.1%) was actively working. The monthly income of the households, 223 (53.9%) earned between 300 and 1920 ETB, and 191 (46.1%) earned more than 1920 ETB (Table 1).
 |
Table 1 Socio-Demographic Characteristics of HIV-Positive Adults on ART at Selected Hospitals in Sidama Regional State, Southern Ethiopia, 2019 |
Environmental and Behavioral Related Characteristics
The majority of 273 (65.9%) were living in the cemented floor house. Most of 401 (96.9%) had a latrine, among this 395 (95.4%) were shared with their family and neighbors. More than half of 287 (69.8%) used Garbage can or sac to disposer refuse. The main source of drinking water was 398 (96.1%) pipe water. Regarding behavioral related factors, 27 (6.5%) were used any tobacco products, among this 14 (3.4%) were current cigarette smokers. The prevalence of Khat chewing was 48 (11.6%). Regarding alcohol consumption, 71 (17.1%) were ever drunk alcohol, 63 (15.2%) were drinking alcohol in the last 30 days (Table 2).
 |
Table 2 Environmental and Behavioral Characteristics of HIV-Positive Adults on ART at Selected Hospitals in Sidama Regional State, Southern Ethiopia, 2019 |
Health Care System and Individual Related Characteristics
However, more than half of the participants 263 (63.5%) had doubts about health-care providers. The majority of 376 (90.8%) knew the importance of adherence to ART. Mainly, 352 (85.0%) were believed that using ART improves life and lives longer, 408 (98.6) were agreed that ART can prevent OIs and AIDS. While majority 320 (77.3%) reported that they disclosed their HIV status to their family and relatives (Table S1).
Patient Health Condition Related Factors
Eighty-three (20.0%) of the study participants had a history of side effects on ART drugs and 202 (48.8%) were taken extra drugs additional to ART drugs (Table S2). Nearly half of, 206 (49.8%) were on WHO clinical stage I, while 83 (20.0%) and 31 (7.5%) were on WHO clinical stage III and IV, respectively (Figure 1).
 |
Figure 1 Magnitude of opportunistic infections among HIV/AIDS on ART at selected hospitals in Sidama Regional State, Southern Ethiopia 2019 (n=414). |
The Magnitude of Opportunistic Infections
The overall magnitude of opportunistic infections was 39.6%, [95% CI: 35.0–44.4] were found to be infected by one or more opportunistic infections among HIV/AIDS Patients taking ART at Selected Hospitals in Sidama Regional State, Southern Ethiopia. Major identified opportunistic infections were oral candidiasis 96 (23.2%), recurrent bacterial pneumonia 89 (21.5%), herpes zoster 26 (6.3%), pulmonary tuberculosis 25 (6.0%), extrapulmonary TB 24 (5.8%), and Crypto-coca meningitis 9 (2.2%) (Figure 2).
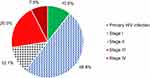 |
Figure 2 WHO clinical staging among HIV/AIDS on ART at selected hospitals in Sidama Regional State, Southern Ethiopia 2019 (n=414). |
Associated Factors for Opportunistic Infections
The highest number of OIs and had statistically significant association on bivariable analysis were among older aged 35 or above years were 78 (50.6%), which followed by 66 (38.6%) were grouped b/n 25–34 years. Also, we assess the highest magnitude of OIs among no formal education 15 (60.0%), attending elementary school 48 (47.1%), and 46 (48.9%) the study respondents who did not disclosed their HIV status to their family and relatives were exposed to OIs with P-value <0.05.
In the multivariate analysis age of respondents, household monthly income, initial CD4 count, education, had no extra medicine additional to ART (prophylaxis), taking ART medicines properly, and Khat chewing remained as the determinant of opportunistic infections. This study result shows that advancing in the age had about 3.5 times more exposed to develop OIs [AOR=3.50, 95% CI:1.85, 6.61], as compared with younger age. No formal education had [AOR=4.54, 95% CI:1.81, 11.37], more exposed to OIs as to their counterparts. Initial CD4 count less than 200 cells/mm3 [AOR=3.10, 95% CI:1.61, 5.96], the study participants who interrupt ART medicines had [AOR=3.21, 95% CI:1.86, 5.56] and Khat chewing [AOR=4.24, 95% CI:2.07, 8.68] were more exposed to OIs when compared to their counterparts (Table 3).
 |
Table 3 Bivariable and Multivariable Logistic Regression Analysis for OIs Among HIV-Positive Adults on ART at Selected Hospitals in Sidama Regional State, Southern Ethiopia, 2019 |
Discussions
This facility-based cross-sectional study revealed that the magnitude of opportunistic infections was 39.6%, [95% CI: 35.0–44.4] were found to be infected by one or more opportunistic infections among HIV/AIDS Patients taking ART at Selected Hospitals in Sidama Regional State, Southern Ethiopia. Major identified opportunistic infections were Oral candidiasis 23.2%, recurrent bacterial pneumonia 21.5%, herpes zoster 6.3%, and Pulmonary Tuberculosis 6.0%. This study result was consistent with the study findings in Wolaita Zone, Southern Ethiopia 45.3%11 and Uganda 43%.9 This result higher when compared to eastern Ethiopia 20.2% had any form of tuberculosis, oral candidiasis, herpes zoster,14 22.4% Nigeria,19 19.7% Northern Ethiopia.20 While it was slightly lower when compared with 61.7% Nigeria,19 47.6% Taiwan,21 and 48% eastern Ethiopia.14 The discrepancy might be due to differences in geographical areas of study participants, high exposure to infectious agents, social-economic status, drug resistance, immunity and nutrition, may affect the magnitude of OIs.
This study result revealed that advancing in the age was more exposes to OIs as compared with younger age. Similar to the United States,22 and Northwest Ethiopia.23 The possible reason maybe, when they grow older the patients’ immune get decreased due to the increased number of viral load and other factors predispose to OIs. In addition to that, the study participants who had no formal education exposes to OIs more as compared with high and above education. This finding was also similar to Debre Markos Referral Hospital, Northwest Ethiopia,23 and eastern Ethiopia.14 This may due to a lack of health-related information about prevention, early symptoms and health benefits. In addition to this, higher education related with income, which directly related to the access to better nutrition, water source and afford the better sanitation materials for the household and personal hygiene of the individuals. This finding implies that health-care providers, needs to give more attention for those HIV-positive adults who had no formal education, and older age needs counseling on transmission, prevention and complication of the OIs may reduce the impact.
The study participants who interrupt ART medicines, and Initial CD4 count less than 200 cells/mm3 had high odds of to develop OIs. This study finding consistent with eastern Ethiopia,14 and Dessie hospital ART clinic, Northeast Ethiopia.24 This might due to OIs could be prevented by using extra drugs additional to ART drugs or prophylaxis. This finding implies that HIV-positive adults need more attention on counseling for early initiation of ART and took their ART drugs as prescribed reduce exposure to the OIs.
This study result showed that Khat chewing was more exposed to OIs. Similarly reported in Northwest Ethiopia23 and eastern Ethiopia.14 This may due to unclean and raw harvested Khat which grows on unclean environment which was not free from open defecation may leads to more exposure to the OIs. The possible reason may be, chewing Khat spent more money and time which may lead to economic problems to afford well-nourished foods and affects health-seeking behavior by temporary relief. This explains that health officials and health-care provider should act by using different strategies to reduce the infection and consequence of the OIs among HIV-positive adults.
This study result shows there was a high prevalence of OIs. This study result shows there was a high prevalence of OIs. This may due to poor socio-economic status, poor adherence or interruption of ART, exposure to potential pathogens and environmental factors may in the area which exposes the patient to OIs. In addition to this, fear to take ART in front of the others or unable to disclose their result to their partner/family or this could be a sign of resistance/treatment failure that needs to be further investigated. This is an indication of inconsistent OIs prevention and control activities needs to address early detection for better prevention, evaluation, and management to reduce OIs. In addition to this health officials and providers needs to collaborate for the implementation of the TB/HIV activity is of vital importance and early initiation of ART. Future research should explore more by triangulating with qualitative study for factors with OIs to design targeted interventions.
This study has potential limitations as the study is cross-sectional in design; it neither represents the seasonal variation of nutritional outcomes nor establishes a causal relationship. In addition to this, the odds ratios of the cross-sectional study did not show the strength of an association. Furthermore, our study population includes HIV-positive adults who had at least one month follow up on ART unit at selected hospitals which might be weak to assess the effect of anti-retroviral therapy on OIs.
Conclusions
This study result shows there was a high prevalence of opportunistic infection among HIV/AIDS patients taking anti-retroviral therapy. The most common opportunistic infections were of oral candidiasis, herpes zoster, and tuberculosis (pulmonary and extrapulmonary). Older age of respondent, initial CD4 count, advancing WHO clinical staging, had no formal education, participants who interrupt ART medicines, and Khat chewing were found determinant factors for opportunistic infections when compared to their counterparts.
Abbreviations
ART, anti-retroviral therapy; CD4, cell with CD-4 marker; ETB, Ethiopian birr; OIs, opportunistic infections; SPSS, Statistical Package for Social Science; STD, sexually transmitted disease; TB, tuberculosis; WHO, World Health Organization.
Data Sharing Statement
There is no remaining data and materials, all information is clearly presented in the main manuscript.
Ethics Approval and Consent to Participate
We took ethical clearance and legal permission from Hawassa University College of Medicine and Health Sciences, and conducted in accordance with the Declaration of Helsinki and was approved by an institutional review board or ethics committee. In addition to this, support letter was also requested from the former Sidama zone health bureau. All participants informed well about purpose, risk, benefit, confidentiality and they had every right to stop participation at any time. Participation was fully voluntary and written informed consent and verbal consent for who cannot read and write respondent was obtained from each participant. They were matured enough (>18 years) to understand and to give consent. The data collector will proceed to the questionnaire if he approved the participants agreement otherwise stop the interview. The patients’ medical records were reviewed anonymously, and all information obtained from medical records was kept confidential. No one other than investigators had access to data.
Acknowledgments
The authors would like to thank Hawassa University, College of Medicine and Health Science for ethical approval. We would like to thanks to former Sidama zone health bureau for their cooperation on providing, information and support letter. The authors are also grateful to all data collectors and study participants for their valuable contributions.
Author Contributions
DW wrote the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas and read and approved the final manuscript. FB approved the proposal with some revisions, participated in data collection, analysis, read and approved the final manuscript. All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
No funding was obtained.
Disclosure
The authors declare that they have no conflict of interests for this work.
References
1. Coleman RL, McLean S. Commentary: the value of PrEP for people who inject drugs. J Int AIDS Soc. 2016;19:21112. doi:10.7448/IAS.19.7.21112
2. CampBinford M, Kahana SY, Altice FL. A systematic review of antiretroviral adherence interventions for HIV-infected people who use drugs. Curr HIV/AIDS Rep. 2012;9(4):287–312. doi:10.1007/s11904-012-0134-8
3. Csete J, Kamarulzaman A, Kazatchkine M, et al. Public health and international drug policy. Lancet (London, England). 2016;387(10026):1427–1480. doi:10.1016/S0140-6736(16)00619-X
4. Heestermans T, Browne JL, Aitken SC, Vervoort SC, Klipstein-Grobusch K. Determinants of adherence to antiretroviral therapy among HIV-positive adults in sub-Saharan Africa: a systematic review. BMJ Glob Health. 2016;1(4):e000125. doi:10.1136/bmjgh-2016-000125
5. Pantoja T, Opiyo N, Lewin S, et al. Implementation strategies for health systems in low-income countries: an overview of systematic reviews. Cochrane Database Syst Rev. 2017;(9):CD011086.
6. Iacob SA, Iacob DG, Jugulete G. Improving the adherence to antiretroviral therapy, a difficult but essential task for a successful HIV treatment—clinical points of view and practical considerations. Front Pharmacol. 2017;8:831. doi:10.3389/fphar.2017.00831
7. Panel on Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. AIDSinfo. 2019;1–5.
8. UNAIDS. Global AIDS Update 2016. Geneva: WHO/UNAIDS; 2016.
9. Rubaihayo J, Tumwesigye NM, Konde-Lule J. Trends in prevalence of selected opportunistic infections associated with HIV/AIDS in Uganda. BMC Infect Dis. 2015;15:187. doi:10.1186/s12879-015-0927-7
10. Hakim J, Maitland K. Oral abstracts of the 21st International AIDS Conference. J Int AIDS Soc. 2017;20(Suppl 5):22253.
11. Alemayehu M, Yisehak Y, Alaro W, Alemayehu B. Opportunistic infections among HIV/AIDS patients taking ante-retroviral therapy at tertiary care hospital in Wolaita Zone, Southern Ethiopia. J AIDS Clin Res. 2017;8:665. doi:10.4172/2155-6113.1000665
12. Rubaihayo J, Tumwesigye NM, Konde-Lule J, Wamani H, Nakku-Joloba E, Makumbi F. Frequency and distribution patterns of opportunistic infections associated with HIV/AIDS in Uganda. BMC Res Notes. 2016;9:501. doi:10.1186/s13104-016-2317-7
13. Jaillette E, Girault C, Brunin G, et al. French Intensive Care Society, International congress – réanimation 2016. Ann Intensive Care. 2016;6(Suppl 1):50.
14. Mitiku H, Weldegebreal F, Teklemariam Z. Magnitude of opportunistic infections and associated factors in HIV-infected adults on antiretroviral therapy in eastern Ethiopia. HIV/AIDS (Auckland, Nz). 2015;7:137–144.
15. WHO. HIV/AIDS Facts Sheet. Geneva: WHO; 2015.
16. Kindie E, Alamrew Anteneh Z, Worku E, Maga G. Time to development of adverse drug reactions and associated factors among adult HIV positive patients on antiretroviral treatment in Bahir Dar City, Northwest Ethiopia. PLoS One. 2017;12(12):e0189322. doi:10.1371/journal.pone.0189322
17. Moges NA, Kassa GM. Prevalence of opportunistic infections and associated factors among HIV positive patients taking antiretroviral therapy in Debre Markos referral hospital, Northwest Ethiopia. J AIDS Clin Res. 2014;5:301. doi:10.4172/2155-6113.1000301
18. World Health Organization. Chronic Diseases and Health Promotion. STEP Wise Approach to Chronic Disease Risk Factor Surveillance (STEPS). Geneva: World Health Organization; 2010.
19. Iroezindu M, Ofondu E, Hausler H, Van Wyk B. Prevalence and risk factors for opportunistic infections in HIV patients receiving antiretroviral therapy in a resource-limited setting in Nigeria. J AIDS Clin Res. 2013;3:002.
20. Damtie D, Yismaw G, Woldeyohannes D, Anagaw B. Common opportunistic infections and their CD4 cell correlates among HIV-infected patients attending at antiretroviral therapy clinic of Gondar University Hospital, Northwest Ethiopia. BMC Res Notes. 2013;6:534. doi:10.1186/1756-0500-6-534
21. Sun HY, Chen MY, Hsieh SM. Changes in the clinical spectrum of opportunistic illnesses in persons with HIV infection in Taiwan in the era of highly active antiretroviral therapy. Jpn J Infect Dis. 2006;59:311–316.
22. MacKellar DA, Valleroy LA, Secura GM, et al. Unrecognized HIV infection, risk behaviors, and perceptions of risk among young men who have sex with men: opportunities for advancing HIV prevention in the third decade of HIV/AIDS. JAIDS. 2005;38(5):603–614. doi:10.1097/01.qai.0000141481.48348.7e
23. Moges N, Kassa G. Prevalence of opportunistic infections and associated factors among HIV positive patients taking anti-retroviral therapy in Debre Markos referral hospital, Northwest Ethiopia. J AIDS Clin Res. 2014;05.
24. Missaye A, Dagnew M, Alemu A, Alemu A. Prevalence of intestinal parasites and associated risk factors among HIV/AIDS patients with pre-ART and on-ART attending Dessie hospital ART clinic, Northeast Ethiopia. AIDS Res Ther. 2013;10:7. doi:10.1186/1742-6405-10-7
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.