Back to Journals » Journal of Blood Medicine » Volume 11
Magnitude of Anemia and Its Associated Factors Among Pregnant Women Attending Antenatal Care in Southern Ethiopia: A Cross-Sectional Study
Authors Argaw D, Hussen Kabthymer R , Birhane M
Received 25 May 2020
Accepted for publication 11 September 2020
Published 9 October 2020 Volume 2020:11 Pages 335—344
DOI https://doi.org/10.2147/JBM.S264369
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Dirshaye Argaw, Robel Hussen Kabthymer, Mahlet Birhane
Human Nutrition Unit, School of Public Health, Dilla University, Dilla, Ethiopia
Correspondence: Robel Hussen Kabthymer Human Nutrition Unit
School of Public Health, Dilla University, Dilla 419, Ethiopia
Tel +251913575702
Email [email protected]
Purpose: The aim of this study was to assess the magnitude of anemia and its associated factors among pregnant women attending antenatal care (ANC) at Dilla University referral Hospital, South Ethiopia.
Patients and Methods: An institution-based cross-sectional study was conducted from January to February 2019, among 373 pregnant women who attended antenatal care at Dilla University referral hospital. Socio-demographic factors, nutritional, medical and obstetric information of the study participants were collected using a structured questionnaire. Hemoglobin was measured using a hemacue machine, and fecal specimens were examined to detect intestinal parasites. Bivariate and multiple variable binary logistic regressions were used to identify predictors of anemia. A p-value less than 0.05 was used to declare statistical significance.
Results: Overall prevalence of anemia was 28.7%, of which 19.6% had mild anemia. Decreased odds of anemia were found in women with good nutritional status (MUAC ≥ 24 cm) (AOR= 0.07 95% CI: 0.03– 0.1), iron supplementation (AOR=0.06 95% CI: 0.02– 0.15) and birth spacing ≥ 2 yrs (AOR=0.03 95% CI: 0.009– 0.45). However, increased odds of anemia were seen in pregnant women with intestinal parasites (AOR=6.11 95% CI 7.70– 37.0).
Conclusion: The magnitude of anemia among pregnant women was found to be a moderate public health problem. Iron supplementation, good nutritional status (MUAC> 24 cm), and birth spacing reduce the odds of anemia. But having intestinal parasites was found to increase the likelihood of anemia during pregnancy. Counseling on birth spacing, strengthening iron supplementation, and intestinal parasite management during pregnancy should be given due emphasis.
Keywords: pregnancy, anemia, Dilla, Ethiopia, prevalence
Introduction
Anemia is a condition which exists when there is less than the normal hemoglobin (Hb) level in the body, which decreases oxygen-carrying capacity of red blood cells to tissues. The Hb levels for each class of anemia during pregnancy are 10.0–10.9 g/dl (mild), 7–9.9 g/dl (moderate) and <7 g/dl (severe).1
Anemia affects more than 2 billion people globally, accounting for nearly 30% of the world’s population. Anemia is the most common public health problem particularly in developing countries, occurring at all stages of the life cycle. The prevalence of anemia in developing and developed countries is estimated to be 43% and 9%, respectively.2 Magnitude of anemia exceeds 50% in most sub-Saharan African countries.3,4 As reported in 2005 Ethiopian demographic health survey (EDHS), anemia has severe public health significance in Ethiopia. In 2016, the national prevalence among pregnant women was 29% and the figure did not decline over the previous decade.5,6
Anemia during pregnancy remains one of the top public health concerns in developing countries due to various socio cultural problems like illiteracy, poverty, lack of awareness, cultural and religious taboos, poor dietary habits, and high prevalence of parasitic infestation. Current estimates from the World Health Organization reports indicate that 41.8% of pregnant women are anemic, with the highest burden of share found in Africa (61.3%) and South East Asia (52.5%).2,7
Pregnancy makes women more vulnerable to anemia. According to Ethiopian demographic health survey (EDHS 2016), 22% of Ethiopian women aged 15–49 years are anemic, of which 17% have mild anemia, 5% have moderate anemia, and 1% have severe anemia. Proportions of anemia during pregnancy are higher (22%) than in women who are breastfeeding (19%) and women who are neither pregnant nor breastfeeding (15%).5
The main risk factors of anemia include a low dietary intake of iron, poor absorption of iron from diets, and period of life where iron requirements become high (ie, growth and pregnancy).4 Among other causes of anemia, heavy blood loss, acute and chronic infections, cancer, tuberculosis, and HIV can also lower blood Hb concentrations. The presence of other micronutrient deficiencies like vitamin A, vitamin B12, folic acid, riboflavin and copper increases the risk of anemia.4,7,8
There have been different measures to control anemia like iron/folic acid supplementation, food fortification, dietary diversification, deworming and, malaria treatment and control.2 Despite these efforts, the burden of anemia remains alarmingly high. Current strategies to prevent and control anemia have to be re-evaluated to ensure that the various factors contributing to anemia have been identified and addressed properly in an integrated manner.
The availability of local information on the magnitude and related risk factors has a major role in the management and control of anemia, especially during pregnancy. Since there is inadequate scientific in the study area, the aim of this study was to assess the magnitude and its associated factors of anemia among pregnant women attending antenatal clinic in DURH, Southern Ethiopia.
Methods
Study Area
The study was conducted in Dilla University referral hospital (DURH), which is located in Dilla city of southern Ethiopia. The hospital provides medical service for 49,849 and 3,226 clients in outpatient and inpatient settings respectively. Dilla is 365 KM away from the capital Addis Ababa. At the time of the study the total population of Dilla city was 102,624, among this 50,286 were males and 52,338 were females. In the city there is one referral and teaching hospital, and three public health centers. DURH is a referral hospital for the catchment population of more than 2,119,100. It is located in the southern part of the country along the main Addis Ababa – Nairobi international road. The ANC is run by the maternity department of the hospital. About 30 women attend the ANC clinic daily. In Ethiopia, “package of services” provided within the ANC include iron folic acid supplementation, deworming, HIV testing, nutrition counseling and intermittent preventive treatment for malaria.
Study Design and Period
Institutional-based cross-sectional study was conducted from November 2017 to January 2018.
Source Population
Source population for this study was all pregnant women attending antenatal care (ANC) in Dilla University referral hospital.
Study Population
All selected pregnant women who were attending antenatal care (ANC) in Dilla University referral hospital at the time of data collection.
Eligibility Criteria
Pregnant women who attended ANC in DURH were included in the study, whilepregnant women with recent blood loss, severe dehydration were excluded.
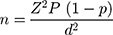
Sample Size Determination
The sample size required for this study was determined using a single population proportion formula with the assumption of confidence level 95%, power of 80%, margin of error 5% and prevalence of anemia 32.8% from previous institution-based cross-sectional study conducted in Arbaminch health care settings.9 In addition a 10% non-response rate was added.
n=sample size
Z= 95% confidence interval (1.96)
P= prevalence = 32.8%
n = 339+10% non-response=373
The sample size was also calculated considering the significant associated factors using epi info software but 373 was found to be the largest sample size.
Sampling Procedure
First we reviewed the records of monthly flow of pregnant women for ANC utilization in DURH ANC clinic and the previous 3 months total pregnant women who visited DURH ANC were 1113. Using this data we calculated a sampling interval of 3 (K=1113/373). Hence, 373 pregnant women visiting ANC during November 2018 to January 2019 were selected by using systematic random sampling.
Operational Definition of Variables
- Anemia: defined as a condition of pregnant women in which the hemoglobin concentration measured is less than 11 g/dl. And anemia was classified as:
mild = hemoglobin concentration of 10–10.9 g/dl
moderate= 7–9.9 g/dl
- Dietary diversity score: the total score calculated for each individual from the selected 9 food groups consumed in the last 24 hours without place and time restriction. From those nine food groups, those who consumed ≥6 food groups were labeled as “highly diversified food”, 4 and 5 food groups as “medium dietary diversity” and ≤3 food groups as ”undiversified”.10
- Intestinal parasite: parasites that cause blood loss in the body were assessed by stool examination. Some of these parasites are hook worms, schistosomiasis, Trichuris trichiura, Giardia lamblia, Entamoeba histolytica and Ascaris lumbricoides.11
- Nutritional status: mid upper arm circumference (MUAC) was measured to the nearest 0.1 cm using flexible and non-stretchable measuring tapes following the standard procedures. Mothers were considered under-nourished when their MUAC value was less than 24.0 cm and those with MUAC ≥ 24 were considered well nourished.12
Data Collection Tools and Procedures
A structured and pretested interviewer administered questionnaire was used to obtain socio-demographic information, dietary habits, and obstetric history. To obtain dietary habits, a multiple pass 24 hour recall method was used to assess the intake of various food items for the past 24 hours. The questionnaire was developed in English and then translated into Amharic language for simplicity then back-translated to English language to check its consistency by two different language experts who speak both English and Amharic fluently. The nutritional status of the women was measured by using mid-upper arm circumference (MUAC) measuring tape.
Household Food Insecurity Level
The household food insecurity access scale was adapted from food and nutrition technical assistance (FANTA) Version 3. Each of the questions was asked with a recall period in the last four weeks (30 days). Responses were counted for occurrence, and frequency of occurrence which produced a score for each household. This score is finally classified into four categories: as “food secure”, “mildly food insecure”, “moderately food insecure”, and “severely food insecure”.13
Hemoglobin Measurement
Hemoglobin measurement was done from capillary blood by collecting one drop of blood carefully from the middle finger. The finger of the pregnant woman was pricked after cleaning the fingertip with sterile cotton (immersing in 70% alcohol) with a sterile disposable lancet. Calibrated HEMOCUE Hb 301, HEMOCUE AB, ANGELHOLM SWEDEN machines were used to assess the hemoglobin concentration, which was recommended for use in resource-limited settings and the results were expressed in g/dl, then categorized based on criteria of WHO cut off point.14
Stool Specimen Collection and Examination for Intestinal Parasites
Stool samples were collected for the study after explanation about the procedure and its importance. Stool samples were collected from the women using clean containers and within an hour of collection stool microscopy was done at the laboratory by Bachelor degree holder laboratory technician. Direct microscopy with Formalin-ether concentration technique was employed to identify the parasites.15
Data Quality
Two day intensive training was given to data collectors regarding study objectives, interviewing techniques, and ethical issues during data collection. A pretest was done among 5% of the total sample size at nearby Yirgachefe district hospital. Functionality and performance of instruments were cross-checked by using quality control samples, for Hemocue it was checked against CBC machine.
Data Analysis
The collected data were checked for completeness and consistency. Data were entered into EpiData version 3.2, and then exported to SPSS version 20 for cleaning and analysis. Tables and graphs were used to summarize descriptive results of the data. Bivariate and multiple variable binary logistic regression models were used. Those variables with p-value < 0.25 at the bivariate level were included in a multivariate logistic regression model to control potential confounding factors. After adjusting, those variables with a p value < 0.05 were considered as statistically significant factors associated independently with anemia. Crude and adjusted odds ratios with 95% confidence intervals were reported.
Results
Socio-Demographic Characteristics
A total of 373 pregnant women were included in this study making a response rate of 99.9%. Majority, (324 [76.5%]) of study participants resided in urban areas and regarding marital status, 307 (82.3%) were married (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Pregnant Women Attending Antenatal Care in DURH, Southern Ethiopia, 2019 |
Socio Economic Characteristics
(Table 2).
 |
Table 2 Socio-Economic Characteristics of Pregnant Women Attending Antenatal Care in DURH, Southern Ethiopia, 2019 |
Dietary-Related Characteristics
Nearly three fourths (82.8%) of the respondents consumed meat once per week or less. From the total study participants, 142 (38.1%) respondents drank more than 3 cups of coffee per day. More than half, (229 [61.4%]), of the respondents had a medium dietary diversity score (4–5), and the rest, 100 (26.8%), and 44 (11.8%), had a low and high dietary diversity score respectively (Table 3).
 |
Table 3 Dietary-Related Characteristics of Pregnant Women Attending Antenatal Care in DURH, Southern Ethiopia, 2019 |
Nutrition-Related Characteristics
Majority, 277 (74.3%), of the participants had MUAC ≥24 cm and 271 (72.7%) were currently taking iron with folic acid supplement (Table 4).
 |
Table 4 Nutrition-Related Characteristics of Pregnant Women Attending Antenatal Care in DURH, Southern Ethiopia, 2019 |
Chronic and Acute Illness
From the total study participants almost all (341 [91.4%]) of the respondents had no known chronic illness and only 91 (24.4%) respondents had a recent history of malarial infection.
Reproductive Health Characteristics
Only one third, (117 [31.4%]), of the respondents were nulliparious. From the total study participants, 160 (42.9%) were in 3rd trimester and 179 (48.0%) were in their 2nd trimester. Majority (196 [52.5%]) of study participants spaced their latest inter pregnancy interval by greater than 2 years (Table 5).
 |
Table 5 Reproductive Health History of Pregnant Women Attending Antenatal Care in DURH, South Ethiopia, 2019 |
Parasitic Infection
From the total study participants, 238 (63.8%) had no parasitic infection. More than a third of pregnant women were infected with different intestinal parasites. Of this, Entamoeba histolytica and Giardialamblia were predominant (Figure 1).
 |
Figure 1 Types of intestinal parasites identified from the pregnant women, DURH, South Ethiopia, 2019. |
Prevalence of Anemia
The overall prevalence of anemia in this study was 28.7%, (95% CI: 24.1–33.5). Of this 68.2%, 29.9% and 1.9% were mild, moderate, and severe anemia respectively (Figure 2).
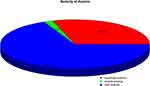 |
Figure 2 Severity of anemia among pregnant women attending antenatal care in DURH, Southern Ethiopia, 2019 (n=373). |
Factors Associated with Anemia Among Pregnant Women
On bivariate analysis, age, educational status, occupational status, residence, family size, household income, frequency of meat consumption, drinking coffee, presence of intestinal parasitic infection, iron supplementation, nutrition education, 24-hour dietary diversity score, latest inter pregnancy interval, and MUAC were associated with anemia with p-value > 0.25. After multivariate analysis, iron folate supplementation, presence of intestinal infection, inter pregnancy interval, and MUAC were significantly associated with anemia in pregnant women (Table 6).
 |
Table 6 Factors Associated with Anemia Among Pregnant Women Attending Antenatal Care in DURH, South Ethiopia, 2019 |
Pregnant women who had good nutritional status (MUAC ≥24 cm) were 93% less likely to develop anemia as compared to women with MUAC < 24 cm [AOR= 0.07 (0.03, 0.18)]. In addition, pregnant women who had iron/folate supplementation were less likely to develop anemia by 94% [AOR=0.06 (0.02, 0.15)]. Pregnant women whom spaced the previous birth and their latest pregnancy by ≥2 yrs were 97% less likely to develop anemia as compared to their counterparts [AOR=0.03 (95% CI 0.009, 0.45)]. The odds of being anemic among pregnant women who had intestinal parasites were 6 times [AOR=6.11 (7.70, 37.0)] more likely as compared to those who had no intestinal parasites.
Discussion
In this study, the overall prevalence of anemia among pregnant women attending antenatal care was found to be 28.7% (95% CI: 24.1–33.5). Out of which 19.57% had mild anemia, 8.58% had moderate anemia, and 0.55% had severe anemia.
The magnitude of anemia among pregnant women in this study is a moderate public health problem.4 The prevalence found in this study is comparable with studies done in Southeast Ethiopia (27.9%), Western Ethiopia (29%), and Arbaminch town (33%).7,9,16 These similarities might be due to similar socio economic characteristics and settings of the studies. But, the prevalence in this study was higher than in studies done in Tigray region (19.3%),7 and in Gondar town Amhara region (16.6%).17 These variations might be due to differences in cutoffs used to define anemia, geographic location, as well as the time differences (when the studies were undertaken).
In the present study, the odds of having anemia were significantly higher among pregnant who did not take iron supplementation during pregnancy as compared to those pregnant women who took iron supplementation. This finding was similar to a study done in North Western Tigray18 and Southern Ethiopia.19 The possible explanation for this association might be that pregnant women who take their iron tablets can meet their pregnancy-increased iron need, which in turn prevents the occurrence of anemia. Hence, focusing on strengthening the adherence of iron/folate supplementation will prevent anemia and its negative impacts on birth outcome.
Pregnant women who had a good nutritional status (MUAC ≥24 cm) were 93% less likely to develop anemia during pregnancy as compared to their counterparts. This result was supported by studies done in urban area of Eastern Ethiopia20 and Oromia region.21 The possible explanation for the observed association could be increased overall nutritional demand during pregnancy, which results in both macro and micro nutrient deficiency, if intake is not sufficient.22 Those malnourished pregnant women might also be affected by micronutrient deficiency, hence leading to depletion of stored iron in the body and bone marrow, which results in anemia.
Birth spacing by ≥2 yrs reduces the likelihood of developing anemia during pregnancy by 97%. Similar finding was reported from studies done in Mekelle town7 and Arbaminch.9 The relationship between anemia and birth spacing can be explained by the fact that birth spacing will give mothers enough time to restore, replenish, and prepare their bodies for the next pregnancy. This implies family planning has a huge role in the health of mothers, children, and the family as a whole.
Having intestinal parasites increases the risk of anemia 6 times as compared to those who had no intestinal parasites. Our finding was in agreement with different studies conducted in different parts of Ethiopia and other countries that reported higher odds of anemia among pregnant women with intestinal parasites.16,19,23 Intestinal parasites, particularly hookworm infection has long been recognized among the major causes of anemia in poor communities. Evidence has shown that increased hookworm infection intensity is associated with lower hemoglobin levels in pregnant women.19 Intestinal parasites reduce iron status via sucking blood from intestinal wall or by facilitating chronic blood loss, reducing appetite and nutrient intake.24,25
This result implies that, other than routine prenatal iron supplementation, preventive or therapeutic deworming integrated with ANC help to reduce the burden of maternal anemia. According to the national guidelines of Ethiopia, pregnant women should be routinely dewormed in the second or third trimester of pregnancy. Different measures should be designed to increase ANC coverage to reach those who do not come to ANC clinics.
Strength and Limitation
A strength could be the high response rate. The limitation could be the fact that it was an institution-based study, with a cross-sectional design which was unadjusted for altitude as the participants come from different areas.
Conclusion
The overall prevalence of anemia among pregnant women attending antenatal care in the study area was found to be a moderate public health problem. Iron supplementation, good nutritional status (MUAC> 24 cm), and birth spacing reduce the odds of anemia. But having intestinal parasites was found to increase the likelihood of anemia during pregnancy.
Abbreviations
ANC, antenatal care; AOR, adjusted odds ratio; COR, crude odd ratio; DDS, dietary diversity score; EDHS, Ethiopian Demographic and Health Survey; Hgb, hemoglobin; HIV, human immunodeficiency virus; MUAC, mid upper arm circumference; SNNPR, Southern Nations, Nationalities, and Peoples Region; SPSS, Statistical Package for Social Sciences; WFP, World Food Program; WHO, World Health Organization.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon request.
Ethics Approval and Consent to Participate
Ethical clearance was obtained from institutional review board of Dilla University, College of health sciences and medicine. Participants were informed about the purpose of the study, and written informed consent was obtained. Confidentiality was maintained by omitting their names on the questionnaire. We confirm this study was conducted in accordance with Declaration of Helsinki. While collecting the data, the pregnant women with Hgb <11 g/dl and women with IPIs were immediately advised to see health professionals at the ANC clinic for treatment and follow up.
Acknowledgments
We would like to thank Dilla University College of Medicine and Health Sciences for giving us permission to conduct this study. We also acknowledge our data collectors and study participants.
Author Contributions
All authors made a significant contribution to the work reported, that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Dilla University funded the expenses for data collection.
Disclosure
The authors report no conflicts of interest in this work.
References
1. WHO. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and mineral nutrition information system. Geneva: World Health Organization; 2011. Available from: http://www.who.int/vmnis/indicators/haemoglobin. pdf.
2. WHO. The global prevalence of anaemia in 2011. Geneva: World Health Organization; 2015. Available from: https://apps.who.int › iris › bitstream › 9789241564960_eng.
3. Kassebaum NJ, Jasrasaria R, Naghavi M, et al. A systematic analysis of global anemia burden from 1990 to 2010. Blood. 2014;123(5):615–624. doi:10.1182/blood-2013-06-508325
4. De Benoist B, McLean E, Egli I, Cogswell M editors. Worldwide Prevalence of Anaemia. Vol. 1993–2005. Geneva: WHO Global Database on Anaemia. World Health Organization; 2008.
5. Central Statistical Agency [Ethiopia], the DHS Program. Ethiopia: demographic and health survey 2016. Addis Ababa and Maryland: CSA and ICF; 2017.
6. Central Statistical Agency [Ethiopia], the DHS Program. Ethiopia: demographic and health survey 2005. Addis Ababa and Maryland: CSA and ICF; 2006.
7. Abriha A, Yesuf ME, Wassie MM. Prevalence and associated factors of anemia among pregnant women of Mekelle town: a cross sectional study. BMC Res Notes. 2014;7:888. doi:10.1186/1756-0500-7-888
8. Ejeta E, Alemnew B, Fikadu A, Fikadu M, Tesfaye L, Birhanu T. Prevalence of anemia in pregnant women’s and associated risk factors in Western Ethiopia. Food Sci Qual Manag. 2014;31:82–91.
9. Bekele A, Tilahun M, Mekuria A. Prevalence of anemia and its associated factors among pregnant women attending antenatal care in health institutions of Arba Minch Town, Southern Ethiopia. Anemia. 2016;2016:1–9. doi:10.1155/2016/1073192
10. FAO and FHI 360. Minimum Dietary Diversity for Women: A Guide for Measurement. Rome: FAO; 2016.
11. World Health Organization. Soil-transmitted helminth infections: key facts. 2018. Available from: http://www.who.int/news-room/fact-sheets/detail/soil-transmitted-helminth-infections.
12. Tang AM, Chung M, Dong K, et al. Determining a global mid-upper arm circumference cutoff to assess malnutrition in pregnant women. Food Nutr Tech Assist. 2016.
13. Coates J, Swindale A, Bilinsky P. Household food insecurity access scale (HFIAS) for measurement of household food access: indicator guide (v. 3). Washington, D.C: Food and Nutrition Technical Assistance Project, Academy for Educational Development; August, 2007.
14. Nkrumah B, Nguah SB, Sarpong N, et al. Hemoglobin estimation by the HemoCue® portable hemoglobin photometer in a resource poor setting. BMC Clin Phatol. 2011;11:5. doi:10.1186/1472-6890-11-5
15. Cheesbrough M. District Laboratory Practice in Tropical Countries. Cambridge: Cambridge University Press; 2006.
16. Kefiyalew F, Zemene E, Asres Y, Gedefaw L. Anemia among pregnant women in Southeast Ethiopia: prevalence, severity and associated risk Factors. BMC Res Notes. 2014;7:771. doi:10.1186/1756-0500-7-771
17. Melku M, Addis Z, Alem M, Enawgaw B. Prevalence and predictors of maternal anemia during pregnancy in Gondar, Northwest Ethiopia: an institutional based cross-sectional study. Anemia. 2014. doi:10.1155/2014/108593
18. Gebre A, Mulugeta A. Prevalence of anemia and associated factors among pregnant women in North Western Zone of Tigray, Northern Ethiopia: a cross-sectional study. J Nutr Metab. 2015;2(4).
19. Lebso M, Anato A, Loha E. Prevalence of anemia and associated factors among pregnant women in Southern Ethiopia: a community based cross-sectional study. PLoS One. 2017;12(12):e0188783. doi:10.1371/journal.pone.0188783
20. Kedir H, Berhane Y, Worku A. Khat chewing and restrictive dietary behaviors are associated with anemia among pregnant women in high prevalence rural communities in eastern Ethiopia. PLoS One. 2013;8(11):e78601. doi:10.1371/journal.pone.0078601
21. Unicef. Prevention and control of nutritional anaemia: a South Asia priority. UNICEF Regional Office for South Asia; 2002. Available from: https://hetv.org/pdf/anaemia-pc.pdf.
22. Conde‐Agudelo A, Rosas‐Bermudez A, Castaño F, Norton MH. Effects of birth spacing on maternal, perinatal, infant, and child health: a systematic review of causal mechanisms. Stud Fam Plann. 2012;43(2):93–114. doi:10.1111/j.1728-4465.2012.00308.x
23. Tefera G. Determinants of anemia among pregnant women with emphasis on intestinal helminthic infection at Sher- Ethiopia Hospital, Ziway, Southern Ethiopia. J Microbiol Immunol Infect Dis. 2014;2(4):33–39.
24. Pullan R, Brooker S. The health impact of polyparasitism in humans: are we under-estimating the burden of parasitic diseases? Parasitology. 2008;135(7):783–794. doi:10.1017/S0031182008000346
25. Stephenson LS, Latham MC, Ottesen EA. Malnutrition and parasitic helminth infections. Parasitology. 2000;121:S23–38. doi:10.1017/S0031182000006491
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.