Back to Journals » Research and Reports in Neonatology » Volume 11
Magnitude and Determinants of Immediate Adverse Neonatal Outcomes Among Babies Born by Cesarean Section in Public Hospitals in Harari Region, Eastern Ethiopia
Authors Abdullahi YY , Assefa N , Roba HS
Received 9 December 2020
Accepted for publication 27 January 2021
Published 12 February 2021 Volume 2021:11 Pages 1—12
DOI https://doi.org/10.2147/RRN.S296534
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Robert Schelonka
Yasir Younis Abdullahi,1 Nega Assefa,2 Hirbo Shore Roba3
1Department of Obstetrics and Gynecology, Jegula Hospital, Harar, Ethiopia; 2College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia; 3Department of Public Health, Haramaya University, Harar, Ethiopia
Correspondence: Yasir Younis Abdullahi
Jegula Hospital, Harar, Ethiopia
Tel +251930340123
Email [email protected]
Purpose: To determine the magnitude and determinants of immediate adverse neonatal outcomes among babies born by cesarean section in public hospitals in the Harari region, Eastern Ethiopia.
Patients and Methods: A prospective follow-up study among 715 eligible babies born by cesarean section in Jegula and Hiwot Fana public hospitals in Harar. Neonate is said to have immediate adverse outcomes if one of the following were detected: (1) baby died, or (2) admitted to NICU, or (3) its primitive reflexes were absent within 24 hours after delivery Adjusted risk ratios (ARRs) and 95% confidence intervals (CIs) were computed using modified Poisson regression.
Results: During the follow-up period, a total of 44 babies died, 139 admitted to NICU, and 133 had absent neonatal reflexes. In general, 157 had an adverse neonatal outcome after CS. The following conditions were postively and statistically related with the outcome: estimated household income (ARR 2.19 CI 1.57– 3.07), having no Antenatal care (ARR 1.46 1.08– 1.97), history of medical or obstetric condition (ARR 1.78 CI 1.38– 2.31, having an absolute indication for delivery (ARR 1.71 CI 1.28– 2.29), presence of meconium (ARR 1.61 CI 1.22– 2.12), low birth weight (ARR 1.96 CI 1.42– 2.70), and respiratory depression at birth (ARR 2.50 CI 1.80– 3.48).
Conclusion: A fifth of babies developed immediate adverse outcomes after a cesarean section. Several maternal clinical factors were predictors for immediate adverse neonatal outcomes. Assessing previous clinical and obstetric conditions of the women during ANC would help properly plan in averting the occurrence of immediate adverse neonatal outcomes after birth.
Keywords: a follow-up study, neonatal mortality, NICU admission rate, absent neonatal reflexes, adverse neonatal outcomes
Introduction
Cesarean section (CS) is the most familiar, life-saving procedure, necessitated, or the only available delivery option.1, CS is the fetus’s birth, placenta, and membranes through an incision on the abdominal and uterine wall afterward, 28 weeks of gestation.3,4 The World Health Organization (WHO) and other organizations suggest that low or higher CS rates may reflect a pregnant women’s lack of access to care.5 Even though there is an argument the procedure over-utilized globally,6 many kinds of literature,7,8 suggest the CS rate in low-income countries, where over 60% of the world’s birth occur, is still low, indicating poor availability of comprehensive essential obstetric care services (EOC) and monitoring the service provision.9
Although CS is a safe operation, it puts mothers and their babies at risk of short- and long-term health problems when performed without medical need.10 However, most CS problems come from the cause, primarily leading to the operation and not the procedure itself.11 According to some studies, the public’s perception that CS delivery is now an almost risk-free procedure might well be contributing to the rise of CS delivery, neonatal morbidity, and mortality.12,13
In Ethiopia, neonatal mortality has contributed significantly to the under-five mortality rate. Simultaneously, discrepancies existed among regions with an estimated 29 neonatal deaths per 1000 live births in 2016.14 Several health programs targeted the optimal reduction of neonatal mortality rates improving newborn and child health quality. Providing integrated maternal, newborn, and child health and clean and safe delivery services in health facilities prevents most of this neonatal death.15
In a CS, some maternal clinical factors could lead to a higher risk of post-delivery complications. These factors are age, income, maternal obesity and morbidity, large infant size, prolonged labor, multiple pregnancies, and baby prematurity. Maternal demand for CS and fear of medical lawsuits have also influenced a significant proportion of cesarean delivery in a facility, which has increased the likelihood of neonatal admission and complications. In the absence of an indication for the procedure, the excess risk to the neonate associated with the operation itself has to be considered other than maternal clinical factors alone.11,16,17
Several studies on CS outcomes in Ethiopia reported that the magnitude of fetal complications ranges from 6.8% to 37.1% using chart review.18–21 However, there is insufficient information about immediate adverse neonatal outcomes following CS and its predictors in Ethiopia. Generating this information will provide insight for health executives, hospital managers, service providers, and clients to make an appropriate plan towards service and to take necessary precautions. Furthermore, it will provide valuable data and literature by further incorporating factors that were not studied previously like absolute indication and introduce recommendations in the performance of neonatal health services. Hence, this paper aims to determine the magnitude and determinants of the immediate adverse neonatal outcomes after CS in Harar Public Hospitals, Eastern Ethiopia.
Patients and Methods
Study Settings
This study has been done in two public hospitals (Jugal Regional Hospital and Hiwot Fana Specialized University Hospital) in Ethiopia’s Harari Region from May 1 to August 1, 2020. Both facilities provide comprehensive delivery services, including CS; the Quarterly average CS delivery and rate in both hospitals is 343 and 757, 22% and 35%, respectively. When delivering in the hospitals, it is a standard practice to triage for the stage of labor and fetomaternal condition. Either a midwife or an attending doctor follow the women using Partograph. The decision for indicating CS is the attending consultant obstetrician, resident, and integrated emergency surgical officer’s sole responsibility.
Study Design
This is a facility-based prospective follow-up study designed to assess CS’s immediate adverse neonatal outcomes and determinants. The study used a structured data-collecting checklist adopted from previous studies.21 The survey starts before 30 minutes of surgery and lasts 24 hours after the cesarean delivery. Mothers with a ruptured uterus were not eligible for the study.
Population and Sampling
The study includes 715 women who had a CS in the respective hospitals. The sample size was determined using Epi- info version 7-sample size and power calculation for unmatched cohort and cross-sectional studies. Assuming the proportion of immediate neonatal outcomes who had not had ANC and had ANC was 12.3% and 4.6%, respectively.22 Further, the assumptions taken are a two-side confidence interval of 95%, the study (1-β) of 80%, and a 10% non-response rate. After using the reported average quarter CS delivery of the respective hospital for calculating allocation, the calculated required sample size was 223 for Jugal and 492 for Hiwot Fana Specialized University Hospital. The sampling technique implemented was systematic simple random sampling techniques with a sampling interval, which was the division of quarter CS attendance and sample size, which was two. Babies of the first eligible mother who went for CS on the first day and every other baby picked on the study period. For mothers who were not eligible or unwilling to participate, the next mother operated on were taken randomly.
Data Management
The information was kept confidential using computer-generated randomized identification numbers not matched with names or other identifying information. Thus, there is no way researchers can link the study data to individual participants. Training on the study procedures and data collection steps was given to research staff.
Data Collection
Institutional Health Research Ethical Review Committee of College of Health and Medical Sciences at Haramaya University approved the study (IRERC/123/2020). Permissions on the conduct of the study were secured from hospital administrators. A pretest was conducted on 10% of the sample size to check the appropriateness of the data collection tool, consistency, and participant selection. All participants provided informed consent, and the study was conducted in accordance with the Declaration of Helsinki. The information sheet details the study title, objective, procedure, risk, and advantage of enrolling in the study. Respondents had the right not to participate or withdraw from the study at any time.
The following social and clinical characteristics were collected: maternal age, weight, height, estimated household income, gravidity, parity, gestational age, gestation, indication for CS, and presence of meconium. Gestational age was estimated using the last menstrual period or measured by ultrasound on admission. The following neonatal characteristics were also collected: sex, weight, and respiratory effort at the first minute of birth. All data collection procedures followed the national infection prevention guideline and social distancing.
Operational Definition
Emergency CS is a CS procedure performed for the unforeseen obstetric complication that needs immediate attention.23
Elective CS or Planned CS is a CS procedure performed at a prearranged time to ensure the best outcome of pregnancy.23
Fetal distress: is a term interchangeably used with non-reassuring fetal heart rate to express intrauterine fetal jeopardy due to hypoxia. In our settings, it is detected using a fetoscope and defined when the fetal heartbeat is below 110 beats or 180 beats per minute despite intrauterine resuscitation.3,24
Gestational age is the duration of pregnancy calculated from the first day of the last menstrual period measured in weeks or from Ultrasound measurement taken previously or during admission.25
Gravidity or gravida specifies the number of times someone is pregnant regardless of the outcome. A current pregnancy, if any, is included in this count. A pregnancy with multiple babies counted as one.26
Indication: clinical judgment for performing a cesarean section. It can be a maternal or fetal indication. It is classified based on low resource settings as relative and absolute.27 Absolute indication: when vaginal delivery is impossible like contracted pelvis, obstructed labor, major Antepartum hemorrhage, failed trial of labor after CS, Transverse lie, two more CS scars. Relative indication: vaginal delivery is possible but the danger to the mother or baby is high like fetal distress, minor APH, one previous CS scar, and other indications.23
Neonatal birth weight: stratified as very low birth weight (1000–1499gm), low birth weight (1500–2499gm), average birth weight (2500–3999gm), and macrosomia (>4000gm).28–30
Absent Primitive Neonatal reflex: when three or more neonatal primitive reflexes are absent after CS delivery. These include Sucking, Babinski, Moro, and Grasp reflex.31
Neonatal Death is the death of a baby within 24 hours of delivery.14,32
Immediate adverse neonatal outcome of CS: when one of the neonatal parameters occurs: neonatal death from the hospital, birth trauma, severe neonatal morbidity, admission to intensive care unit within 24 hours of the procedure.29,30
Respiratory Depression at Birth is the presence of fast breathing (> 60 breath/second) or low breathing (<30 breath/second) or difficulty breathing in the first minute of life.33–35
Data Processing and Analysis
Data were coded, entered, cleaned on Epidata version 4.6, and exported and analyzed using Stata version 16. The outcome variables were neonatal NICU admission, absent neonatal reflexes, and neonatal death. They were also recorded and categorized as immediate adverse neonatal outcomes after CS delivery or not when 1) neonate died, or 2) admitted to NICU, or 3) has depressed reflexes within 24 hours after birth. The NICU admission in 24 hours after birth and neonatal reflexes was checked by evaluating and observing the neonate’s necessary laboratory and treatment findings of the physician and the charts. To check for an association between predictors and the outcome, modified Poisson regression is used, taking the immediate neonatal outcomes following CS as a dependent variable.36,37 Variables with more than 50% missing values were removed from the data. Factors found to have p-values < 0.25 in bivariate analysis were retained for the final model. Crude risk ratios (CRRs) and adjusted risk ratios (ARRs) were calculated with 95% confidence intervals (CIs). For the final model, statistical significance is considered at a p-value < 0.05. Before running the final model, the Multicollinearity was tested using the coefficients’ covariance matrix, was checked, and only covariates with covariance < 0.5 are included. Sensitivity analysis was computed for the composite outcome to determine the effect of unmeasured confounding factors.
Results
From May-August 2020, there were 1214 and 2145 deliveries at Jugual and Hiwot-Fana specialized University hospitals, respectively. Of these, 361 and 807 were cesarean deliveries, respectively. Seven hundred fifteen (715) women who were willing to be enrolled in the study were enrolled in the follow-up.
Maternal Characteristics
The mean age (±SD) of the women was 26 0.7 (±5.5) years. Most delivering women, 648 (90.6%) had a singleton pregnancy. The majority, 553 (77.34%), had ANC during their pregnancy at least once. The mean estimated gestational age is statistically different across booked mothers and un-booked as well as a singleton and multiple pregnancies (p= 0.0001) (Table 1 below).
 |
Table 1 Sociodemographic and Clinical Characteristics of Mothers Attending Cesarean Section in Harari Public Hospitals Harar, Ethiopia 2020 |
Delivery and Cesarean-Related Characteristics
Sixty-seven percent of study participants had labor before CS. Even though partograph was not used to follow, the majority of emergency CS, more than half (311/569 or 54.68%) of them had either early or no labor. Out of planned CS (146 or 20.42% of all births performed in the study period), nearly half 78 (53.42%) of them requested CS. Most CS deliveries, 703 (98.32%) ended with live births. Nearly half of the newborns 329, (46.80%) had respiratory depression in the first minute of life. Many of the newborns (73.49%) had average birth weight. Of low-birth-weight newborns, many of them were premature (70/99) and had respiratory depression (64/99) (Table 2 below).
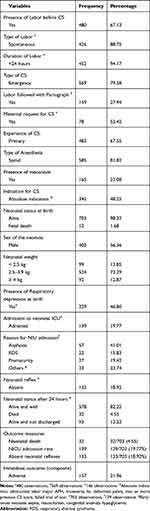 |
Table 2 Delivery and Newborn Characteristics of Mothers Who Gave Birth by Cesarean Section in Harari Public Hospitals Harar, Ethiopia 2020 |
Immediate Neonatal Outcome and Related Characteristics
Of live births, the neonatal admission rate was.19.44% and 18.92% had absent primitive neonatal reflexes within 24 hours of birth. Of those who were admitted to the NICU, most of them (91.37%) had absent primitive neonatal reflex, the majority 105, (75.54%) had respiratory depression in the operation theater, and 32 (23.02%) of them died within 24 hours. The top three causes for NICU admission were asphyxia (57/139), prematurity (27/139), and respiratory distress syndrome (22/139), respectively. Early neonatal death and perinatal mortality rates were 45.52/1000 live births and 61.54/1000 total birth, respectively. Overall, the frequency of immediate adverse neonatal outcomes was 157 (22% 95% CI: 19.1, 25.2). Birth trauma was not observed in the study period. (Tables 2 and 3 below).
 |
Table 3 Immediate Adverse Outcomes of Neonates Born by Cesarean Section in Harar Public Hospitals Harar, Ethiopia 2020 |
The Factors Associated with the Immediate Neonatal Outcomes After CS
After adjusting for maternal age and possible confounders in the final analysis, household income, history of medical/obstetric illness, ANC follow-up, the presence of meconium, having absolute CS indication, low birth weight, and respiratory depression was positively and statistically associated with adverse outcome measure. Neonates born to mothers whose age was greater than or equal to 35 years were 43% more likely (ARR 1.43; CI 1.03, 1.99) to develop absent neonatal reflexes immediately after CS compared to women whose age is 20 to 34 years. Maternal age lost its statistical association in the final model for NICU admission and adverse outcomes. For mothers whose estimated monthly household income less than 5200 Ethiopian Birr, their newborns had twice the risk (ARR 2.32; CI 1.63, 3.30) of admission to NICU and (ARR 2.14; CI 1.50, 3.05) had absent reflexes immediately after CS in comparision their counterparts.
After CS, the risk of neonatal mortality is 4.37 times (ARR 4.37; CI 2.25, 8.52) the risk among babies from grand multi-para women compared to their counterparts. For babies from women with no ANC, the risk of absent primitive reflexes, NICU admission, and the overall adverse outcome has increased by 57% (ARR 1.57; CI 1.13, 2.17), 45% (ARR 1.45; CI 1.06, 1.98), and 46% (ARR 1.46; CI 1.08, 1.97) immediately after CS delivery compared to their respective counterparts. For babies with meconium-stained amniotic fluid, the risk of NICU admission and absence of neonatal reflexes after CS increased by 56% (ARR 1.56; CI 1.17, 2.08) and 66% (ARR 1.66; CI 1.23, 2.24), respectively. Babies born with an absolute indication of CS had an increased risk of 73% (ARR 1.73; CI 1.26–2.36), and 58% (ARR 1.58; CI 1.17–2.13), for loss of their primitive reflex, and NICU admittance than those with relative indications. Underweight babies were two times (ARR 2.01; CI 1.44, 2.81) and 2.28 times (ARR 2.28; CI 1.65, 3.17) as likely to have the risk of NICU admission and loss of neonatal reflexes than those with average weight. Newborns that had respiratory depression at birth in the first minute were 2.5 times (ARR 2.50; CI 1.80, 3.48) as likely to have an immediate adverse outcome. The absolute risk of NICU admission and absence of neonatal reflexes was 15.62 and 15.13% for babies with respiratory depression (Tables 4 and 5).
 |
Table 5 Determining Factors of Adverse Neonatal Outcome After Cesarean Section in Harari Public Hospitals Harar, Ethiopia 2020 |
Discussion
In this study, the magnitude of immediate adverse neonatal outcomes for babies born with CS in Harar public hospitals is 22%. The neonatal mortality rate is 45.52 per 1000 live births, NICU admission rate, and absence of neonatal reflexes were 19.77% and 18.92%, respectively. Babies born from women with an estimated household monthly income of less than 5200 Ethiopian Birr (144 USD) had a statistically significant increase in the likelihood of immediate adverse neonatal outcomes. Women with a history of medical or obstetrical problems, those who had no ANC follow-up, and meconium staining of the amniotic fluid were associated with adverse neonatal outcomes. Neonatal factors such as low birth weight and respiratory depression at the first minute of birth were also associated with adverse neonatal outcomes following CS.
The magnitude of immediate adverse neonatal outcomes of CS in this study is 22%, statistically high (p<0.05) compared to facilities in southwest Ethiopia,38 which was 6.5%, but low in the eastern part and the northern part of Ethiopia.20,21 In terms of neonatal mortality, other studies in the eastern part of Ethiopia also reported a facility neonatal mortality of 20% (95 CI 16.7–23.8), statistically lower than our findings. This is likely related to the nature of the hospital where this study is conducted. Some seventy percent of the study participants were enrolled from the university hospital that received complicated cases.39
Babies born from women who have aged 35 and above had an excess risk of six-percentage points for adverse outcomes after cesarean delivery compared to the other age groups. Even though less than one-eighth of the observation was in that age group, it was statistically insignificant in the final analysis. It could be due to a smaller proportion of the study sample observed were in advanced maternal age than other age groups. With increased maternal age, other studies reported that the risk of fetal intra-uterine insults, pregnancy or delivery complications, cesarean sections, and chromosomal abnormalities are increased significantly.40–42 But the finding is in line with a cohort study conducted in Saudi Arabia, where maternal age alone is not a strong predictor for a poor neonatal outcome, although it has a snowball effect with grand multiparity.43 The relationship is hypothetically and clinically meaningful, but we could not establish strong statistical evidence for it.
This study showed that the excess risk of babies born from women whose estimated household income is less than 5200 Ethiopian Birr (144 USD) * were fourteen percentage points for having immediate adverse neonatal outcomes after CS than those with higher incomes. This could be explained by a higher restrain on financial freedom in the household that would hinder health priorities to pregnant women. This may include expenditure for nutrition and difficulty accessing health care in emergencies.44,45 Thus, the expectation is that low-income women are more prone to have delays in seeking medical care.3 Many studies had outlined and linked that poorer and less educated women would have babies with immediate adverse outcomes in Sub-Saharan Africa.41
The risk of an immediate adverse outcome nearly doubled among women who had previous medical or obstetric problems than those who had not. The finding is in line with other studies in Ethiopia.21,22 Because medical or obstetrical conditions may persist during pregnancy affecting fetal development and maturity, many women with obstetric and medical conditions undergo cesarean delivery, jeopardizing the neonate’s survival.46
Consistent with other studies, babies would have an excess risk of immediate adverse outcomes one-twelfth as their mothers have no ANC follow-up at least one follow-up but not for neonatal death.47 Preterm neonates had one-sixth and one-ninth excess risk than afull- term neonate for adverse outcomes and neonatal death after CS. This result was statistically and clinically significant that prematurity predisposes the newborn for breathing difficulty, hypoxia, and hypothermia, all implicated in neonatal morbidity and mortality.48 Moreover, our finding was not in agreement with a prospective study in Addis Ababa, which reported ANC booking not being a predictor but not for average newborn weight, which was protective for neonatal mortality.49 It is important to note ANC has been established to detect early pregnancy-related problems, promote maternal health, facilitate identification of abnormalities, and plan appropriate kinds of delivery in preparation for birth preparedness and complication readiness.3 This difference could result from different methodologies implemented, as others investigated both cesarean and vaginal birth.
Similarly, many preterm newborns in our sample had low birth weight and respiratory depression as well. The finding is also in line with other studies that found prematurity was significantly associated with an increased risk of NICU admission and neonatal mortality.32,50 Neonates with respiratory depression at birth had seventeen percent excess risk to develop immediate adverse outcomes than those without respiratory depression. Since neonates with respiratory depression may have impeding meconium aspiration, Respiratory Acidosis, prematurity, Encephalopathy, and Hypoxia requiring resuscitation and admission to the NICU.51,52 Our finding points out strengthening the quality and equity of NICU services would be essential in decreasing neonatal complication and death.46
The presence of meconium was statistically associated with the immediate adverse neonatal outcomes, with meconium the excess risk was one-tenth higher relative to neonates with clear amniotic fluid. This result could be related to the fact that meconium is an indicator of fetal Hypoxia and placental insufficiency and predisposes the fetus to aspiration.25
For neonates, whose mother had a CS for absolute indication, the excess risk of immediate adverse neonatal outcomes was eleven percent higher than women with relative indication. The relationship had strong statistical evidence, and was clinically essential and expected that the absolute indication makes vaginal delivery impossible.53 To the best knowledge of the authors, this paper is the first to report an association between an absolute indication with adverse outcome measures of CS in developing countries. A higher proportion of absolute indication of CS could also indicate a disparity on basic essential obstetric care,27 although this paper does not address this question and further community-level studies are recommended in differentiating the gap.
Limitation
It is imperative to note that the study has limitations. As a hospital-based follow-up study, it cannot show a causal relationship and did not control for vaginal delivery, which could limit the study’s statistical power. Gestational age estimation with late ultrasound measurement also introduces potential measurement error in the study. The long-term outcomes of the CS were not studied in this paper. Other potential risk factors that could interact and predict adverse neonatal outcomes of CS such as maternal infection and hemorrhage, were not documented in the study. Because of a large quantity of missing or uncollected data for key predictors such as total pregnancy weight gain data and neonatal parameters like small or large for gestational age were not used in this study. This may affect the interaction and association between the factors and the outcomes. The reader should take into consideration BMI at delivery does not show a nutritional problem in pregnancy, rather BMI before pregnancy and gestational weight gain are needed as a proxy to measure the condition.
Conclusion
We showed that immediate adverse neonatal outcomes of cesarean section are high in public hospitals in the study setting. We have identified estimated household monthly income of less than 5200 Ethiopian Birr, history of medical and obstetric conditions, absence of antenatal care during the index pregnancy, low birth weight, presence of meconium and respiratory depression, and absolute indication are statistically and positively related with immediate adverse neonatal outcome. Pre-pregnancy maternal health, early detection, and management of abnormalities in pregnancy and labor may decrease immediate adverse neonatal outcomes following CS.
Abbreviations
ANC, antenatal care; ARR, adjusted risk ratio; APH, antepartum hemorrhage; BMI, body mass index; CRR, crude risk ratio; CS, cesarean section; NRFHRP, non-reassuring fetal heart rate pattern; RDS, respiratory distress syndrome, USD, United States Dollar.
Data Sharing Statement
The datasets used and analyzed during this study are available from the corresponding author on reasonable request.
Acknowledgments
The authors wish to thank Professor Darren Hudson and kelsey Carthew for editing this paper. The authors would also like to thank Haramaya University and the administrative bodies at Jugal and Hiwot-Fana Specialized University Hospital for facilitating the study. Finally, our gratitude goes to Dr. Refiq Remadan, Dr. Ibsa, and Dr. Tadesse for their help and cooperation during data collection.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Gibbons L, Belizan JM, Lauer JA, Betran AP, Merialdi M, Althabe F. Inequities in the use of cesarean section deliveries in the world. Am J Obstet Gynecol. 2012;206(4):331e331–319. doi:10.1016/j.ajog.2012.02.026
2. World Health Organization. WHO Statement on caesarean section rates. Reprod Health Matters. 2015;23(45):149–150. doi:10.1016/j.rhm.2015.07.007
3. Federal Ministry of Health. Management Protocol on Selected Obstetrics Topics. Federal Democratic Republic of Ethiopia; 2010.
4. Adelaiye SM, Olusanya A, Onwuhafua PI. Cesarean section in Ahmadu Bello University Teaching Hospital Zaria, Nigeria: a five-year appraisal. Trop J Obstet Gynaecol. 2017;34(1):34. doi:10.4103/TJOG.TJOG_58_16
5. World Health Organization, UNICEF. Indicators to Monitor Maternal Health Goals: Report of a Technical Working Group, Geneva, 8–12 November 1993. Geneva: World Health Organization; 1994.
6. Boerma T, Ronsmans C, Melesse DY, et al. Global epidemiology of use of and disparities in caesarean sections. Lancet. 2018;392(10155):1341–1348. doi:10.1016/S0140-6736(18)31928-7
7. Yaya S, Uthman OA, Amouzou A, Bishwajit G. Disparities in caesarean section prevalence and determinants across sub-Saharan Africa countries. Glob Health Res Policy. 2018;3:19. doi:10.1186/s41256-018-0074-y
8. Adewuyi EO, Auta A, Khanal V, Tapshak SJ, Zhao Y. Cesarean delivery in Nigeria: prevalence and associated factors-a population-based cross-sectional study. BMJ Open. 2019;9(6):e027273–e027273. doi:10.1136/bmjopen-2018-027273
9. Reddy KM, Kodimala SC, Pathakamudi P, Betha K. Prevalence and determinants of caesarean section in a rural tertiary teaching hospital: a 6-year retrospective study. Int J Reproduction, Contraception, Obstet Gynecol. 2019;8(2):560. doi:10.18203/2320-1770.ijrcog20190284
10. Sandall J, Tribe RM, Avery L, et al. Short-term and long-term effects of caesarean section on the health of women and children. Lancet. 2018;392(10155):1349–1357. doi:10.1016/S0140-6736(18)31930-5
11. Am B, Sa AD, Ys K, et al. Cesarean section: incidence, causes, associated factors and outcomes: a national prospective study from Jordan. Gynecol Obstet Case Report. 2017;03:03. doi:10.21767/2471-8165.1000055
12. Chigbu CO, Ezeome IV, Iloabachie GC. Cesarean section on request in a developing country. Int J Gynaecol Obstet. 2007;96(1):54–56. doi:10.1016/j.ijgo.2006.09.032
13. Long Q, Kingdon C, Yang F, et al. Prevalence of and reasons for women’s, family members’, and health professionals’ preferences for cesarean section in China: a mixed-methods systematic review. PLoS Med. 2018;15(10):e1002672. doi:10.1371/journal.pmed.1002672
14. Central Statistical Agency (CSA), ICF. Ethiopia Demographic and Health Survey. Addis Ababa, Ethiopia and Rockville, Maryland, USA: CSA and ICF; 2016.
15. Federal Ministry of Health. National Newborn and Child Survival Strategy Document Brief Summary 2015/16-2019/20. Addis Ababa: FMOH; 2015.
16. Polkowski M, Kuehnle E, Schippert C, Kundu S, Hillemanns P, Staboulidou I. Neonatal and maternal short-term outcome parameters in instrument-assisted vaginal delivery compared to second stage cesarean section in labour: a retrospective 11-year analysis. Gynecol Obstet Invest. 2018;83(1):90–98. doi:10.1159/000458524
17. Sharma P, Gurung T, Shrestha R, Gurung G, Gurung RT. Prevalence and outcome of cesarean section at Gandaki Medical College Teaching Hospital and Research Centre, Pokhara, Nepal. J Gandaki Med College-Nepal. 2017;9(2):1–6. doi:10.3126/jgmcn.v9i2.17858
18. Ayano M, Beyene W, Geremew M. Prevalence and Outcome of Caesarean Section in Attat Hospital. Gurage Zone, SNNPR, Ethiopia: Arch Med, Jimma University; 2015.
19. Mengistie B, Tsega F, Dessie Y, Merid. M. Prevalence of cesarean section in urban health facilities and associated factors in Eastern Ethiopia: hospital based cross sectional study. J Pregnancy Child Health. 2015;02:03.
20. Chernet L, Nega A. Neonatal Outcomes of Operative Deliveries at Gelemso General Hospital, Oromia Regional State, Eastern Ethiopia. Harar: School of Medicine, Harmaya University; 2016.
21. Mengesha MB, Adhanu HH, Weldegeorges DA, et al. Maternal and fetal outcomes of cesarean delivery and factors associated with its unfavorable management outcomes; in Ayder Specialized Comprehensive Hospital, Mekelle, Tigray, Ethiopia, 2017. BMC Res Notes. 2019;12(1):650. doi:10.1186/s13104-019-4690-5
22. Akki JS, Gemeda DH, Akessa GM. A review of caesarean delivery in Southwest Ethiopia: incidence, indications and outcomes. African J Midwifery Women’s Health. 2015;9(3):106–111. doi:10.12968/ajmw.2015.9.3.106
23. Konar H, Dutta DC. Operative Obstetrics. DC Dutta’s Textbook of Obstetrics. Jaypee Brothers Medical Publishers (P) Ltd; 2015:642.
24. Maaløe N, Bygbjerg IC, Onesmo R, Secher NJ, Sorensen BL. Disclosing doubtful indications for emergency cesarean sections in rural hospitals in Tanzania: a retrospective criterion-based audit. Acta Obstet Gynecol Scand. 2012;91(9):1069–1076. doi:10.1111/j.1600-0412.2012.01474.x
25. Cunningham FG, Gant NF, Leveno KJ, Larry C. Williams Obstetrics. J Midwifery Women’s Health. 2003;48(5):369. doi:10.1016/S1526-9523(03)00291-5
26. Anesthesia and Analgesia for Assisted Reproduction Techniques and other Procedures during the First Trimester. Anesthesia and the Fetus. 2013:147–155
27. Stanton C, Ronsmans C. Baltimore Group on C. Recommendations for routine reporting on indications for cesarean delivery in developing countries. Birth. 2008;35(3):204–211. doi:10.1111/j.1523-536X.2008.00241.x
28. World Health Organization, UNICEF., UNFPA. Pregnancy, Childbirth, Postpartum, and Newborn Care: A Guide for Essential Practice. WHO; 2003.
29. Knight HE, Oddie SJ, Harron KL, et al. Establishing a composite neonatal adverse outcome indicator using English hospital administrative data. Arch Dis Child Fetal Neonatal Ed. 2019;104(5):F502–F509. doi:10.1136/archdischild-2018-315147
30. Lain SJ, Algert CS, Nassar N, Bowen JR, Roberts CL. Incidence of severe adverse neonatal outcomes: use of a composite indicator in a population cohort. Matern Child Health J. 2012;16(3):600–608. doi:10.1007/s10995-011-0797-6
31. Sohn M, Ahn Y, Lee S. Assessment of primitive reflexes in high-risk newborns. J Clin Med Res. 2011;3(6):285–290. doi:10.4021/jocmr706w
32. Getiye Y, Fantahun M. Factors associated with perinatal mortality among public health deliveries in Addis Ababa, Ethiopia, an unmatched case control study. BMC Pregnancy Childbirth. 2017;17(1):245. doi:10.1186/s12884-017-1420-7
33. Sweet LR, Keech C, Klein NP, et al. Respiratory distress in the neonate: case definition & guidelines for data collection, analysis, and presentation of maternal immunization safety data. Vaccine. 2017;35(48Pt A):6506–6517. doi:10.1016/j.vaccine.2017.01.046
34. Reuter S, Moser C, Baack M. Respiratory distress in the newborn. Pediatr Rev. 2014;35(10):
35. Terada S, Irikoma S, Yamashita A, Murakoshi T. Incidence of respiratory depression after epidural administration of morphine for cesarean delivery: findings using a continuous respiratory rate monitoring system. Int J Obstet Anesth. 2019;38:32–36. doi:10.1016/j.ijoa.2018.10.009
36. Chen W, Qian L, Shi J, Franklin M. Comparing performance between log-binomial and robust Poisson regression models for estimating risk ratios under model misspecification. BMC Med Res Methodol. 2018;18(1):63. doi:10.1186/s12874-018-0519-5
37. Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi:10.1093/aje/kwh090
38. Ayano B, Guto A. Indications and outcomes of emergency caesarean section at St Paul’s HospitalMedical College, Addis Ababa, Ethiopia 2017: (Afoul Month Retrospective Cohort Study). Investigations Gynecol Res Womens Health. 2018;2:2. doi:10.31031/IGRWH.2018.02.000535
39. Melesse MB, Geremew AB, Abebe SM. High prevalence of caesarean birth among mothers delivered at health facilities in Bahir Dar city, Amhara region, Ethiopia. A comparative study. PLoS One. 2020;15(4):e0231631. doi:10.1371/journal.pone.0231631
40. Kim SY, Park JY, Bak SE. et al. Effect of maternal age on emergency cesarean section. J Matern Fetal Neonatal Med;2019. 1–8. doi: 10.1080/14767058.2019.1593958
41. Nyirahabimana N, Ufashingabire CM, Lin Y, et al. Maternal predictors of neonatal outcomes after emergency cesarean section: a retrospective study in three rural district hospitals in Rwanda. Matern Health Neonatol Perinatol. 2017;3:11. doi:10.1186/s40748-017-0050-4
42. Cunningham FG. Williams Obstetrics.
43. Al-Shaikh GK, Ibrahim GH, Fayed AA, Al-Mandeel H. Grand multiparity and the possible risk of adverse maternal and neonatal outcomes: a dilemma to be deciphered. BMC Pregnancy Childbirth. 2017;17(1):310. doi:10.1186/s12884-017-1508-0
44. Shah A, Fawole B, M’Imunya JM, et al. Cesarean delivery outcomes from the WHO global survey on maternal and perinatal health in Africa. Int J Gynaecol Obstet. 2009;107(3):191–197. doi:10.1016/j.ijgo.2009.08.013
45. World Health Organization. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience. WHO; 2016.
46. Kolola T, Ekubay M, Tesfa E, Morka W. Determinants of neonatal mortality in North Shoa Zone, Amhara Regional State, Ethiopia. PLoS One. 2016;11(10):e0164472. doi:10.1371/journal.pone.0164472
47. Tognon F, Borghero A, Putoto G, et al. Analysis of caesarean section and neonatal outcome using the Robson classification in a rural district hospital in Tanzania: an observational retrospective study. BMJ Open. 2019;9(12):e033348. doi:10.1136/bmjopen-2019-033348
48. Gabbe SG, Niebyl JR, Simpson JL, et al. Obstetrics: Normal and Problem Pregnancies E-Book. Elsevier Health Sciences; 2016.
49. Tekleab AM, Amaru GM, Tefera YA. Reasons for admission and neonatal outcome in the neonatal care unit of a tertiary care hospital in Addis Ababa: a prospective study. Res Rep Neonatol. 2016;17. doi:10.2147/RRN.S95455
50. Khasawneh W, Obeidat N, Yusef D, Alsulaiman JW. The impact of cesarean section on neonatal outcomes at a university-based tertiary hospital in Jordan. BMC Pregnancy Childbirth. 2020;20(1):335. doi:10.1186/s12884-020-03027-2
51. Razaz N, Cnattingius S, Joseph KS. Association between Apgar scores of 7 to 9 and neonatal mortality and morbidity: population based cohort study of term infants in Sweden. BMJ. 2019;365:l1656. doi:10.1136/bmj.l1656
52. American Academy Of Pediatrics. The Apgar Score. Pediatrics. 2015;136(4):819–822. doi:10.1542/peds.2015-2651
53. Konar H. DC Dutta’s Textbook of Obstetrics. JP Medical Ltd; 2018.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

