Back to Journals » Patient Preference and Adherence » Volume 10
Magnetic resonance enterography or video capsule endoscopy – what do Crohn’s disease patients prefer?
Authors Lahat A , Kopylov U , Amitai M, Neuman S, Levhar N, Yablecovitch D, Avidan B, Yanai H, Dotan I, Chowers Y, Weiss B, Ben-Horin S, Eliakim R
Received 2 November 2015
Accepted for publication 2 February 2016
Published 8 June 2016 Volume 2016:10 Pages 1043—1050
DOI https://doi.org/10.2147/PPA.S99690
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Adi Lahat,1,2 Uri Kopylov,1,2 Marianne M Amitai,3 Sandra Neuman,1,2 Nina Levhar,1,2 Doron Yablecovitch,1,2 Benjamin Avidan,1,2 Henit Yanai,2,4 Iris Dotan,2,4 Yehuda Chowers,5,6 Batya Weiss,7 Shomron Ben-Horin,1,2,* Rami Eliakim1,2,*
On behalf of the Israeli IBD Research Network (IIRN)
1Department of Gastroenterology, Chaim Sheba Medical Center, Tel Hashomer, Israel; 2Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel; 3Department of Diagnostic Imaging, Chaim Sheba Medical Center, Tel Hashomer, Israel; 4IBD Center, Department of Gastroenterology and Liver Diseases, Tel Aviv Medical Center, Tel Aviv, Isarel; 5Rambam Health Care Campus, Haifa, Israel; 6Bruce Rappaport School of Medicine, Technion Israel Institute of Technology, Haifa, Israel; 7Edmond and Lily Safra Children’s Hospital, Tel Hashomer, Israel
*These authors contributed equally to this work
Background: Despite differences in the information obtained by capsule endoscopy (CE) and magnetic resonance enterography (MRE), one of these modalities is usually needed when evaluating disease activity. There are no data on patients’ preference that would help guide the choice between these two modalities in these instances.
Aim: To compare patients’ tolerance and preference to MRE versus CE.
Patients and methods: Patients with known small bowel Crohn’s disease (CD) in clinical remission (Crohn’s disease activity index [CDAI] <150) or with mild symptoms (CDAI <220) were prospectively recruited. All patients underwent MRE followed by CE. Patients were asked to fill out a questionnaire addressing specific points regarding inconvenience during the preparation for the procedures, the procedures, and postprocedures. Side effects and procedure preference were addressed. Questionnaires were included for analysis only when more than 95% of the items were addressed.
Results: Fifty-six patients fulfilled inclusion criteria. Pre-exam discomfort, during-exam discomfort, nausea, vomiting, bloating, and abdominal pain were all significantly more prominent in MRE as compared to CE (P<0.0001, P<0.0001, P<0.0001, P=0.009, P=0.0002, P<0.0001, respectively). MRE was perceived as a more difficult procedure (P<0.0001). Furthermore, MRE was associated with a specific adverse event – claustrophobia. Seventy-eight percent of patients (44 patients) preferred to repeat CE as compared to 22% (P<0.0001) who preferred MRE.
Conclusion: CE was better tolerated by CD patients compared to MRE and was preferred by 78% of patients. The superior tolerability of CE should be considered along with the diagnostic features, and more data sought when choosing between these two modalities for CD patients for long-term follow-up.
Keywords: inflammatory bowel disease, Crohn’s imaging, MRE, capsule endoscopy, patients’ preference
Background
Crohn’s disease (CD) is a chronic inflammatory disorder that may affect the gastrointestinal tract from the mouth to the anus. Inflammation is transmural and therefore may be complicated by fistula, abscess formation, perforations, and fibrotic strictures. The disease may cause significant morbidity and diminished quality of life.1–5 Disease behavior is characterized by periods of flare-ups with active symptomatic disease and periods of remission.6
Imaging studies are essential in the diagnosis, treatment, and follow-up of inflammatory bowel disease (IBD) patients. The use of bowel imaging serves to confirm the diagnosis, assess disease extent and characteristics (inflammatory versus fibrostenotic), and complications.
Bowel imaging is essential during follow-up of patients with chronic disease and affects treatment strategy, medications choices and dosages, and recommendations for surgical or endoscopic interventions. Increasingly, bowel imaging is becoming a routine monitoring tool of treatment outcomes and guides further management even in patients with clinical response or mild symptoms. Overall, patients are required to undergo increasing numbers of repeated bowel imaging studies throughout their disease course.
Two of the most sensitive small bowel imaging modalities are – magnetic resonance enterography (MRE) and small bowel capsule endoscopy (SBCE). Both modalities are radiation free. When performing MRE, examination sequences can be repeated in different techniques and different planes in order to achieve maximum information regarding small bowel wall and lumen, and high-quality imaging of extraintestinal complications as abscesses and fistulas may be obtained. Performing double bowel estimation with positive, followed by negative, contrast material during the same examination is possible, and there is also an option for imaging of small bowel peristalsis (functional examination).7–11
Alternatively, SBCE is the most sensitive method for assessing small bowel mucosa,12 and preliminary data suggest it has higher sensitivity and specificity for subtle small bowel lesions than MRE.13 However, it can only provide information concerning intraluminal disease.
Patient acceptability of a diagnostic procedure is a further important point to bear in mind when choosing between imaging modalities. This is especially true for patients with chronic disease who are increasingly required to undergo repeated and multiple examinations throughout their disease course. However, to the best of our knowledge, there is no data regarding the acceptability of MRE compared to CE. Better understanding of patients’ preferences may improve compliance and lead to better disease management.
We therefore aimed to assess MRE and CE tolerability in CD patients.
Patients and methods
This was an observational cohort study. The study population included adult (>18 years) CD patients with known small bowel disease in remission or experiencing mild disease symptoms, as determined by the validated Crohn’s disease activity index (CDAI) of <150 or 150–220, respectively. In order to be included, patients had to be in corticosteroid-free remission for 3–24 months and were treated with a stable medication dose (60 days of thiopurines and methotrexate, 60 days of infliximab, and 30 days of adalimumab and aminosalicylate [5-ASA] agents).
Patients were excluded if they were unable to understand or provide informed consent; had severe comorbidities such as liver, kidney neurologic, metabolic, or cardiorespiratory disorders not controlled at the time of enrollment; had difficulty in swallowing, history of aspirations, or dysphagia; claustrophobia or implanted metal objects or cardiac pacemaker precluding performance of magnetic resonance imaging (MRI); or known or suspected intestinal obstruction or severe stricture.
All patients provided written informed consent, and the study was approved by the ethics committee of Chaim Sheba Medical Center, Tel HaShomer.
Patients were recruited between July 2013 and February 2015. MRE and video CE (VCE) were performed as part of the study protocol for meticulous disease follow-up. All patients included in the study underwent both procedures (MRE then VCE), with time difference between MRE to VCE of no more than 30 days. All patients underwent an MRE upon enrollment. All MRE examinations were performed using a 1.5T GE Optima MR450w scanner with GEM Suite (GE Healthcare, Little Chalfont, UK) with oral and intravenous contrast. Patients were asked to drink 1,000 mL of mannitol (5%) 60 minutes prior to the examination, followed by intravenous injection of glucagon (1 mg; GlucaGen® HypoKit/Novo Nordisk A/S, Bagsværd, Denmark) and gadolinium (0.1 mmol/kg; gadoterate dimeglumine, Dotarem®, Guerbet, Villepinte, France). The MRE protocol included axial, coronal, and sagittal FIESTA (TR/TE 4.3/1.9 milliseconds); axial and coronal 2D SSFSE T2W (TR/TE 1,680–3,200/92.7 milliseconds); axial and coronal FSPGR FS BH (TR/TE 150/1.3 milliseconds); and coronal LAVA (TR/TE 4.2/2.1 milliseconds) pre- and postgadolinium injection. Field of view was 32–40 cm, with slice width 3.6–6 mm (previously described protocol).14
A patency capsule (PC) test was performed in all patients with active small bowel disease detected on MRE. If no active small bowel disease was detected by MRE, a PC study was not performed. If a PC was not eliminated from the small bowel within 30 hours, the patients were withdrawn from the study. In patients with L1 disease by the Montreal classification, SB-III capsule (Given Imaging, Yokneam Illit, Israel) was used. In patients with established ileocolonic disease (L3 disease), a colonic capsule (PillCam colon2 capsule, Given Imaging) was administered.
The preparation for VCE included ingestion of only clear fluids for 24 hours prior to the procedure and a 12-hour overnight fast. For a colonic capsule study, a 4 L split-dose polyethylene glycol (PEG) preparation was used. An additional bolus with picosulfate (Pico-Salax®, Ferring, Germany) was given after the capsule reached the small bowel to facilitate small bowel transit, and another bolus was given 2 hours thereafter.
After completing each procedure, patients were asked to fill a questionnaire assessing their tolerance of MRE versus CE (Figure S1). Specific assessment points included: inconvenience during preparation; inconvenience during the procedure; different side effects such as nausea, vomiting, bloating, abdominal pain, tenesmus, and claustrophobia during the examination; time needed to complete the examination; grade of exam’s difficulty; and patients’ consent to repeat the exam. Degree of severity was graded from 1 (not at all) to 5 (severe). Questionnaires were included for analysis only when more than 95% of the items were addressed.
Because different preparations were prescribed for colon capsule and for small bowel capsule, a separate subanalysis was also performed, whereby results were analyzed separately for each capsule category.
Statistical analysis
Descriptive statistics were presented as mean ± standard deviation for continuous variables and percentages for categorical variables. Categorical variables were analyzed by chi-square/Fisher’s exact test and continuous variables by Student’s t-test/Mann–Whitney U test, as appropriate. P<0.05 was considered significant. All computations were performed with the MedCalc Software (version 15.8; MedCalc, Mariakerke, Ostend, Belgium).
Results
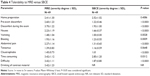
Of the 62 patients who were approached, 58 agreed to answer the questionnaire and 56 fulfilled inclusion criteria. Two patients were excluded because of incomplete data. Of these patients, 49 underwent SBCE and seven underwent colon CE. Patients’ characteristics are shown in Table 1.
  | Table 1 Demographic data and disease characteristics |
Patient-reported scores for the main aspects of procedure tolerability are depicted in Figure 1A–C. For most parameters addressed, patients graded CE as significantly easier and more convenient than MRE. The average score for each modality and corresponding P-values are shown in Table 2. CE was graded as significantly causing less discomfort before and during the exam, as well as causing less nausea, bloating, tinnitus, and abdominal pain. In addition, MRE was distinctive for causing claustrophobia in 16 patients (28.6%), which was naturally not observed in any of the CE procedures. Claustrophobia was never experienced by these patients before. Seventy-eight percent of patients (44 patients) preferred to repeat CE as compared to 22% (P<0.0001) of patients who preferred MRE.
Overall, seven patients included in the study underwent colonic CE. Because precolonic capsule preparation is considered as relatively inconvenient, separate analysis was performed for colon capsule versus MRE (Table 3) and for SBCE versus MRE (Table 4).
Differing from patients who underwent SBCE, patients who underwent colonic CE tended to grade the discomfort during home preparation and before the exam as more severe than MRE (not statistically significant). Other factors such as nausea, vomiting, time consuming, and difficulty were graded as severe, as in MRE. Comparison between colonic CE and SBCE is shown in Table 5. As shown in the table, pre-exam discomfort, nausea, and vomiting were significantly more severe in patients undergoing colonic CE. The examination was also considered as more time consuming and difficult than SBCE.
Nevertheless, five patients still preferred to repeat colonic CE, and three patients preferred MRE.
Discussion
SBCE and MRE are both highly sensitive imaging modalities for the assessment of the small bowel of patients with CD. Although SBCE is the most sensitive modality for fine intraluminal lesion detection, MRE has the advantage of detecting extraluminal disease and complications.
In recent years, assessing disease’s response to therapy and/or disease progression with consecutive bowel imaging has become the standard of care in many medical centers.15 Because patients are required to undergo repeated and frequent examinations, their acceptance and preference becomes an important issue to bear in mind. However, data in the literature are scarce.
In the present prospective study, patients who underwent both procedures significantly preferred CE to MRE. CE caused significantly less preprocedural and intraprocedural discomfort, less nausea and abdominal pain, and was considered as an easier procedure. Seventy-eight percent of patients preferred to repeat CE.
Unlike SBCE, colonic CE necessitates strict and prolonged preparation. Bowel preparation before colonic CE is highly intensive, as it requires ingestion of a 4 L split dose PEG as well as two boosters with Pico-Salax®. Many patients find this preparation difficult and inconvenient.
Thus, colonic CE showed no superiority over MRE when assessing patients’ discomfort. SBCE showed significantly less pre-exam discomfort, and less nausea and vomiting than colonic CE. Furthermore, SBCE was graded as less time consuming and less difficult.
Interestingly, of the seven patients who underwent colonic CE, five still preferred to repeat the capsule, and two preferred MRE.
MRE is considered as an uncomfortable procedure.16–18 Nausea and abdominal pain are the symptoms that were reported as contributing mostly to patients’ inconvenience.19 A previous study addressed the issue of patients’ acceptance of MRE,19 although comparison with CE was not performed. In this study, Negaard et al19 compared the acceptance of small bowel MRI with oral contrast material compared to magnetic resonance (MR) enteroclysis with nasogastric catheter. Not surprisingly, most patients preferred the oral ingestion of contrast material to the instillation through a nasogastric catheter. Both methods caused symptoms of nausea, vomiting, and abdominal pain. These side effects were reported by our patients as well. Other causes of patients’ discomfort, such as claustrophobia or the prolonged duration of the procedure, which were reported by our patients, were not addressed in the prior study. Another study compared MR enteroclysis to SBCE and to double-balloon enteroscopy.20 In this study, the patient population included both patients with occult gastrointestinal bleeding and patients with suspected or known Crohn’s disease. Similar to our results, CE was significantly preferred to MR enteroclysis and balloon-assisted enteroscopy with regard to bowel preparation, swallowing of the capsule (compared to insertion of the tube/scope), burden of the entire examination, duration, and accordance with the prestudy information. Other specific adverse effects of the procedures were not addressed.
Our study has a few limitations. First, only a small number of patients underwent colonic CE, and results of colon capsule subanalysis may be underpowered to detect differences. Nonetheless, it is noteworthy that the better overall tolerability of CE was demonstrated in the main analysis even when incorporating the results of colon CE patients. Moreover, 70% of colon CE patients still preferred to repeat colon CE to MRE. Another limitation is possible selection bias – only patients who were willing to participate in a long-term follow-up study compelling repeated and frequent imaging, and blood and stool examinations were included. These patients may not be fully representative of the entire IBD population and may be more tolerant to medical procedures compared with patients who did not agree to participate in this CE/MRE prospective study. However, we speculate that patients who are less tolerant to medical procedures will have at least the same severity of side effects, if not worse.
Conclusion
In our study, CE was significantly better tolerated than MRE in most parameters and preferred by 78% of patients. These observations should be borne in mind and integrated with the diagnostic yield and specific data being sought, when choosing the imaging modality for CD patients, in particular when repeated follow-up procedures are required.
Acknowledgments
The authors would like to thank Along Lang, MD; Dan Carter, MD; Amir Weizbard, MD; and Eayl Shachar, MD for their contribution to the study. The study was sponsored by the Helmsley Charitable Trust, New York, NY, USA.
Disclosure
The authors report no conflicts of interest in this work.
References
Love JR, Irvine EJ, Fedorak RN. Quality of life in IBD. J Clin Gastroenterol. 1992;14:15–19. | ||
Casellas F, Arenas JI, Baudet JS, et al. Impairment of health-related quality of life in patients with inflammatory bowel disease: a Spanish multicenter study. Inflamm Bowel Dis. 2005;11:488–496. | ||
Rubin GP, Hungin AP, Chinn DJ, Dwarakanath D. Quality of life in patients with established inflammatory bowel disease: a UK general practice survey. Aliment Pharmacol Ther. 2004;19:529–535. | ||
Casellas F, López-Vivancos J, Badia X, Vilaseca J, Malagelada JR. Influence of inflammatory bowel disease on different dimensions of quality of life. Eur J Gastroenterol Hepatol. 2001;13:567–572. | ||
Canavan C, Abrams KR, Hawthorne B, Drossman D, Mayberry JF. Long-term prognosis in Crohn’s disease: factors that affect quality of life. Aliment Pharmacol Ther. 2006;23:377–385. | ||
Latella G, Papi C. Crucial steps in the natural history of inflammatory bowel disease. World J Gastroenterol. 2012;18:3790–3799. | ||
Gourtsoyiannis N, Papanikolaou N, Grammatikakis J, Maris T, Prassopoulos P. Enteroclysis protocol optimization: comparison between 3D FLASH with fat saturation after intravenous gadolinium injection and true FISP sequences. Eur Radiol. 2001;11:908–913. | ||
Maccioni F, Viscido A, Broglia L, et al. Evaluation of Crohn’s disease activity with magnetic resonance imaging. Abdom Imaging. 2000;25:219–228. | ||
Low RN, Sebrechts CP, Politoske DA, et al. Crohn’s disease with endoscopic correlation: single-shot fast spin-echo and gadolinium-enhanced fast-suppressed spoiled gradientecho MR imaging. Radiology. 2002;222:652–660. | ||
Wiarda BM, Kuipers EJ, Heitbrink MA, van Oijen A, Stoker J. MR enteroclysis of inflammatory small-bowel diseases. AJR Am J Roentgenol. 2006;187:522–531. | ||
Leyendecker JR, Bloomfeld RS, DiSantis DJ, Waters GS, Mott R, Bechtold RE. MR enterography in the management of patients with Crohn’s disease. Radiographics. 2009;29:1827–1846. | ||
Bourreille A, Ignjatovic A, Aabakken L, et al. Role of small-bowel endoscopy in the management of patients with inflammatory bowel disease: an international OMED-ECCO consensus. Endoscopy. 2009;41:618–637. | ||
Greener T, Klang E, Yablecovitch D, et al. The impact of magnetic resonance enterography and capsule endoscopy on the re-classification of disease in patients with known Crohn’s disease: a prospective Israeli IBD research nucleus (IIRN) study. J Crohns Colitis. Epub Jan 2016. | ||
Shrot S, Konen E, Hertz M, Amitai MM. Magnetic resonance enterography: 4 years experience in a tertiary medical center. Isr Med Assoc J. 2011;13:172–177. | ||
Eliakim R, Magro F. Imaging techniques in IBD and their role in follow-up and surveillance. Nat Rev Gastroenterol Hepatol. 2014;11:722–736. | ||
Lauenstein TC, Schneemann H, Vogt FM, Herborn CU, Ruhm SG, Debatin JF. Optimization of oral contrast agents for MR imaging of the small bowel. Radiology. 2003;228:279–283. | ||
Schreyer AG, Geissler A, Albrich H, et al. Abdominal MRI after enteroclysis or with oral contrast in patients with suspected or proven Crohn’s disease. Clin Gastroenterol Hepatol. 2004;2:491–497. | ||
Ajaj W, Goyen M, Schneemann H, et al. Oral contrast agents for small bowel distension in MRI: influence of the osmolarity for small bowel distention. Eur Radiol. 2005;15:1400–1406. | ||
Negaard A, Sandvik L, Berstad AE, et al. MRI of the small bowel with oral contrast or nasojejunal intubation in Crohn’s disease: randomized comparison of patient acceptance. Scand J Gastroenterol. 2008;43:44–51. | ||
Wiarda BM, Stolk M, Heine DG, et al. Patient burden and patient preference: comparing magnetic resonance enteroclysis, capsule endoscopy and balloon-assisted enteroscopy. J Gastroenterol Hepatol. 2013;28:464–467. |
Supplementary material
  | Figure S1 Questionnaire – post CE. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.