Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 15
Madelung’s Disease: Analysis of Clinical Characteristics, Fatty Mass Distribution, Comorbidities and Treatment of 54 Patients in China
Authors Li R, Wang C, Bu Q, Pu W, Zhou B, Che L, Zhang H, Xu Y, Luan H
Received 3 March 2022
Accepted for publication 26 July 2022
Published 6 August 2022 Volume 2022:15 Pages 2365—2375
DOI https://doi.org/10.2147/DMSO.S363836
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Runze Li,1,2,* Chuanxiao Wang,3,* Quandong Bu,4 Wenshen Pu,5 Bin Zhou,4 Lin Che,4 Hui Zhang,4 Yan Xu,4 Hong Luan4
1Department of Medicine, Qingdao University, Qingdao, People’s Republic of China; 2Department of Endocrine, Affiliated Hospital of Qingdao University, Qingdao, People’s Republic of China; 3Department of Thoracic Surgery, Qingdao Municipal Hospital, Qingdao, People’s Republic of China; 4Department of Nephrology, Affiliated Hospital of Qingdao University, Qingdao, People’s Republic of China; 5Department of Nephrology, Baoshan People’s Hospital, Baoshan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Hong Luan, Department of Nephrology, Affiliated Hospital of Qingdao University, 16 Jiangsu Road, Qingdao, 266003, People’s Republic of China, Tel +86 18661803208, Fax +86 532-82911601, Email [email protected]
Purpose: Madelung’s disease (MD) is a rare disease characterized by the deposition of unencapsulated fat masses on the face, neck, chest, back and other areas of patients. The aim of the study was to analyze the clinical characteristics, comorbidities and treatment of MD in Chinese populations.
Patients and Methods: We retrospectively reviewed the medical records of 54 patients who were diagnosed with MD at the Affiliated Hospital of Qingdao University and Qingdao Municipal Hospital from January 2005 to February 2021 and collected the subjects’ demographic information, clinical indicators, location of fat deposits, treatment, complications and prognostic data.
Results: Among 54 MD patients in the study, only 1 (1.85%) was female, and the subjects had an average age of 56.65 ± 7.93 years. More than 70% of patients had a history of long-term smoking or/and alcohol abuse. In our study, type I accounted for approximately 61.11% of cases according to Donhauser’s classification, and almost all patients had neck fat deposition. MD patients often have multiple comorbidities across several systems, such as the endocrine, digestive, circulatory, urinary, and neurological systems. Among these, endocrine system diseases were the most common comorbidities in our study, accounting for 81.48%. Notably, up to 20.37% of cases were complicated with cancer, especially digestive system tumors. More than 70% of the patients received surgical treatment, and nearly 40% experienced postoperative recurrence.
Conclusion: Considering that MD patients often have comorbidities of multiple systems and that a small number of cases are even complicated by cancer, we recommend that clinicians comprehensively assess a patient’s condition and complications, advocate that patients quit consuming alcohol and smoking as soon as possible, establish healthy dietary and living habits, and formulate individualized and comprehensive diagnosis and treatment plans.
Keywords: Madelung’s disease, multiple symmetric lipomatosis, Launois-Bensaude syndrome, benign symmetric lipomatosis, alcohol abuse
Introduction
Madelung’s disease (MD), also known as Launois-Bensaude syndrome, benign symmetric lipomatosis (BSL), and multiple symmetric lipomatosis, was first mentioned by Brodie in 1846 and systematically described by Madelung in 1888.1–3 It is characterized by the presence of multiple symmetrical, nonencapsulated fat masses on the neck, chest, back and other areas and is more common in alcoholic men between the ages of 30 and 60 years. The pathophysiology of the disease is currently not fully understood. Alcohol is often thought to be a facilitator of MD, but the exact mechanism has not been elucidated.4–7
MD usually progresses slowly and generally does not undergo malignant transformation, so it is considered a benign disease. As an uncommon illness of unknown etiology, MD is mostly sporadic. The reported incidence of MD is 1:25,000, with a male-to-female ratio of approximately 15:1 to 30:1.8,9 A recent review systematically reviewed previously published reports on MD, with the majority of patients located in Europe (79.7%), especially Portugal (37%) and Italy (21.3%). However, in Asian populations, only sporadic cases and few systematic retrospective analyses have been reported in recent years.3,10–12 The exact incidence of MD in Asia or China has not yet been reported. In addition, the diagnosis and treatment of MD has not yet been standardized, which has caused uncertainty and increased the difficulty of clinical prevention, diagnosis and treatment of MD to a certain extent. Systematic analysis of the characteristics of MD patients in the Asian population may promote a comprehensive understanding of MD to facilitate favorable resolution of MD. Therefore, we collected detailed clinical data from 54 MD patients at two medical centers in Qingdao and conducted a systematic retrospective analysis to improve the understanding of disease characteristics and provide new ideas for the scientific management and comprehensive treatment of MD patients.
Methods
Patients
We retrospectively reviewed the medical records of 54 patients who were diagnosed with MD at the Affiliated Hospital of Qingdao University and Qingdao Municipal Hospital from January 2005 to February 2021. All MD patients were interviewed by telephone and advised to return to our hospital for review. The staff presented our study to the patients at the outpatient clinic and obtained their informed consent. Every participant voluntarily provided written informed consent. The study was performed in accordance with the tenets of the Declaration of Helsinki and approved by the research ethics committee of the Affiliated Hospital of Qingdao University (QYFY WZLL 27027). The diagnosis of MD depended on physical examination, clinical history, and imaging findings of symmetrical fat deposition sites, and some patients who underwent surgery were further confirmed by histopathology. We collected and sorted the demographic information, clinical indicators, location of fat deposits, treatment complications and prognosis data of 54 patients with MD.
Study Variables
We retrospectively analyzed the electronic medical records of all participants and recorded their sex, age, body mass index (BMI), systolic blood pressure (SBP), diastolic blood pressure (DBP), albumin (Alb), direct bilirubin, indirect bilirubin, serum alanine aminotransferase (ALT), serum aspartate aminotransferase (AST), glutamyl transpeptidase, serum triglyceride (TG), serum cholesterol (TC), high-density lipoprotein (HDL), low-density lipoprotein (LDL), fasting blood glucose (Glu), blood urea nitrogen (BUN), serum creatinine (Scr), serum uric acid (UA), estimated glomerular filtration rate (eGFR), history of alcohol and smoking, and surgical results. The eGFR was calculated from the following CKD-EPI equation: eGFR = 141 × min(Scr/κ, 1)α × max(Scr/κ, 1)−1.209 × 0.993Age × 1.018 [if female]_1.159 [if black], where Scr is serum creatinine, κ is 0.7 for females and 0.9 for males, α is −0.329 for females and −0.411 for males, min indicates the minimum of Scr/κ or 1, and max indicates the maximum of Scr/κ or 1.
The definitions of the research variables are shown below. Alcohol drinking was defined as the regular intake of any alcoholic beverage in the past personal life. Data on alcohol history included frequency of drinking (times/week), alcohol consumption (g/week), duration of drinking (years), and type of drinking (beer/liquor/wine). Most of our patients were accustomed to drinking high-grade liquor with an alcohol content above 50%. According to the ratio recommended in the “Dietary Guidelines for Chinese Residents” (2021),13 25 g alcohol (ethanol) is equivalent to 750 mL beer, 250 mL wine, and 50 g liquor. The average weekly alcohol consumption was obtained by multiplying the consumption of each alcoholic beverage by its ethanol content and then multiplying this value by the drinking frequency (times/week). The type of drinking was recorded as the most frequently consumed alcoholic beverage. Smoking history was defined as having smoked at least one cigarette per day for at least six months.
According to the “Chinese Guidelines for the Prevention and Treatment of Dyslipidemia in Adults” (2016),14,15 participants who meet one of the following criteria are defined as having hyperlipidemia: (1) TC ≥ 5.2 mmol/l or TG ≥ 1.70 mmol/L; (2) previously diagnosed with hyperlipidemia by an experienced physician or currently undergoing specific treatment for previously diagnosed hyperlipidemia.
CKD was defined as an abnormality in kidney structure or function that persisted for more than 3 months. This included 1 or more of the following: (1) an eGFR less than 60 mL/min/1.73 m2; (2) albuminuria (ie, a urine albumin level ≥ 30 mg per 24 hours or a urine albumin-to-creatinine ratio ≥ 30 mg/g); (3) abnormalities in urinary sediment, histology, or imaging suggestive of kidney damage; (4) renal tubular disorders; or (5) a history of kidney transplantation.16 Obesity was defined as BMI ≥ 28 kg/m2.17 Other comorbidities, such as type 2 diabetes, impaired fasting glucose, hypothyroidism, hypertension and liver disease, were all defined according to the specified clinical diagnostic criteria.18–21 All participants received standard clinical and laboratory examinations and assessments.
Enzi et al first proposed two types of MD based on the anatomical distribution of fat masses in 1984.22 Donhauser et al further improved the classification method and proposed three types of MD in 1991:23 type 1 (horse collar lipomata), type 2 (pseudoathletic appearance), and type 3 (gynecoid distribution). Type 1 mainly manifests as symmetrical fat deposition in the neck, upper back, shoulders, and upper arms. Type 2 has an exaggerated fat distribution in the shoulder girdle, deltoid region, upper arms, and thorax. Type 3 shows an excess of lipomatous tissue in the lower body, especially the thighs and medial side of the knees.23,24 Compared with traditional classification, Donhauser’s classification is clearer and more intuitive in anatomical relationships, so we used Donhauser’s classification to classify our patients with MD.
Statistical Analysis
Continuous variables are expressed as medians or means ± standard deviations (SDs), and categorical variables are expressed as numbers and percentages in the present study. All statistical analyses were conducted with the software package SPSS version 25.0 for Windows, and P < 0.05 was considered significant.
Results
Epidemiological and Clinical Characteristics of the Participants
Among 54 patients with MD in the study, 53 (98.15%) were male, only 1 (1.85%) was female, and the subjects ranged in age from 31 to 78 years (mean age: 56.65 ± 7.93 years). The average BMI of the participants was 24.02 ± 4.05 kg/m2, and their mean SBP was higher than the normal range, that is, 141.58 ± 17.58 mmHg. The glutamyl transpeptidase (γ-GT) level of most patients was significantly increased, and the mean level was 124.82 ± 212.03 U/L. Other clinical indicators are shown in Table 1.
 |
Table 1 Demographic and General Clinical Characteristics of Participants with Multiple Symmetric Lipomatosis |
History of Drinking and Smoking
We collected the past smoking and drinking history of patients in detail, and the results are shown in Table 2. A history of alcohol abuse at the time of diagnosis or earlier was admitted by 87.04% (n = 47) of the patients, of whom 46 (85.19%) were accustomed to hard liquor consumption, and only 1 (1.85%) was accustomed to beer intake. Their mean time of alcohol intake was 24.13 ± 13.15 years, and the mean alcohol amount was 180.00 ± 118.82 g/d. Among them, 11 patients had abstained from alcohol before coming to the hospital, and 5 patients (9.26%) declared complete abstinence for more than 1 year. Additionally, 42 patients (77.78%) claimed to have a history of smoking. The average time of smoking was 21.24 ± 14.69 years, and the amount was 16.24 ± 13.13 cigarettes/day.
 |
Table 2 History of Alcohol and Smoking in Participants with Multiple Symmetric Lipomatosis |
Distribution of Fat Mass Deposits and Type Situation
The distribution of fat mass in patients with MD is shown in Table 3. All patients had fat accumulation in the neck. In addition, the probability of fat deposition in the back, shoulders, pectoral and upper arms was 18.52%, 12.93%, 11.11% and 11.11%, respectively. A small percentage of patients had deposition of lipomatous tissue in the supraclavicular fossa, abdomen, face, thighs, and perineum.
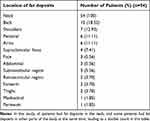 |
Table 3 The Location of Fat Deposits in Patients with Multiple Symmetric Lipomatosis |
The distribution of lipomatous tissue according to Donhauser’s classification is presented in Figure 1. Type 1 was the most common type, accounting for 61.11%. Some patients had more than one type of distribution. Sixteen patients (29.63%) had type 1 combined with other types, of whom 1 patient (1.85%) had the combination of three types at the same time.
 |
Figure 1 Donhauser’s classification in patients with multiple symmetric lipomatosis. |
Comorbidities
In our study, we found that patients with MD often had multiple comorbidities of several systems, such as endocrine, digestive, circulatory, urinary, and neurological systems (Table 4). The vast majority of participants (81.48%) had endocrine diseases, including hyperlipidemia (33.33%), hyperuricemia (29.63%), diabetes (25.93%), and obesity (16.67%). A total of 77.78% of patients with MD had digestive system diseases. Remarkably, more than three-quarters of patients had some form of liver disease, including liver dysfunction (74.07%), alcoholic cirrhosis (20.37%), and hepatic steatosis (7.41%). A minority of participants had gallstones (9.26%) or cholecystitis (5.56%).
 |
Table 4 Comorbidities in Patients with Multiple Symmetric Lipomatosis |
Regarding the comorbidities of the nervous system, a small number of patients had cerebral infarction (7.41%), hematencephalon (3.70%) and diabetes/alcoholic peripheral neuropathy (3.70%/3.70%). Moreover, obstructive sleep apnea hypopnea syndrome (OSAS) was triggered due to the large cellulite in the neck compressing the trachea in 2 patients (3.70%). Twenty-four patient cases (44.44%) were complicated with urinary system diseases, of which 17 patients (31.48%) had an eGFR < 90 mL/min/1.73 m2, and one patient underwent dialysis for uremia. In addition, there were 3 patients (5.56%) with hematuria and 4 patients (7.40%) with proteinuria.
Remarkably, the proportion of MD patients with coexisting cancer was as high as 20.37%, which included 3 cases of stomach cancer (5.56%), 2 cases of lung cancer (3.70%), 2 cases of thyroid cancer (3.70%), 1 case of liver cancer, 1 case of esophageal cancer, 1 case of laryngeal cancer, and 1 case of kidney cancer.
Treatment and Prognosis
In our study, 16 patients (29.63%) did not receive surgery and drug treatment, and 38 (70.37%) patients underwent one or more local liposuctions due to neck tracheal compression or fat mass deposition that affected their appearance. Among them, 15 (39.47%) patients had postoperative cellulite recurrence after surgery, and one patient underwent neck lipectomy three times repeatedly (Table 5). No participants used any medications to interfere with fatty tissue deposition. In addition, no spontaneous regression of the disease was found in the patients in our study. To date, 5 (9.26%) of our included participants have died of malignant tumors, 1 (1.85%) of liver disease, and 1 (1.85%) of myocardial infarction.
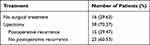 |
Table 5 The Operation Type and Postoperative Recurrence in Patients with Multiple Symmetric Lipomatosis |
Discussion
In the study, 54 patients with MD were recruited from two medical centers in Qingdao, China, and their clinical characteristics and treatment were assessed in detail, aiming to provide new evidence for understanding the disease characteristics of MD in Asia. It was found that MD patients often had multiple comorbidities of several systems, and endocrine system diseases were the most common comorbidities, accounting for 81.48%. It was noteworthy that up to 20.37% of cases were complicated with cancer, especially digestive system tumors. Multiple comorbidities may account for the poor prognosis of MD. Among all patients, more than 70% received surgical treatment, and nearly 40% experienced postoperative recurrence.
There are various hypotheses about the pathophysiological mechanism of MD, including catecholamine-stimulated lipolysis disorder and mitochondrial regulation defects in brown fat.4,25–27 Long-term alcohol abuse has been considered the cause of MD in previous studies, but the specific mechanism has not been fully elucidated.4–7 As a cofactor, alcohol has a direct impact on the metabolic process of mitochondria. Long-term alcohol abuse may lead to premature oxidation or mutations of mitochondrial DNAs in brown fat.28,29 In addition, alcoholism seems to reduce the amount and activity of β-adrenergic receptors required for fat breakdown, which hinders the lipolysis process and increases lipogenesis.4,29 In a longitudinal follow-up study of 31 patients with MD, patients who reduced ethanol intake or abstained from alcohol at the time of follow-up had a reduction in fat mass volume, while four patients who increased alcohol consumption had a progressive increase in subcutaneous lipomatous deposits.11 In a retrospective study of MD in the Chinese population, 11 MD patients were all alcoholics, with an average daily alcohol intake of more than 450 g.9 Similarly, Wan et al reported that 13 (81.25%) MD patients had drinking habits, including 8 (50%) heavy drinkers in their study.30 However, some women and children, as well as men without a history of alcohol abuse, have also been reported to be diagnosed with MD.26,31–34 In this study, up to 87% of the patients had a long history of drinking a large amount of spirits, of whom 5 patients had abstained from alcohol for more than 1 year before treatment; however, there was no spontaneous disappearance or significant reduction in adipose tissue after abstinence. Therefore, it is speculated that long-term alcoholism may be a risk factor for the occurrence and development of MD, but alcoholism is not a necessary condition. Alcohol cessation may be associated with a slight regression of the lipoma depot but cannot completely reverse the disease. This is consistent with the conclusions of previous studies.3,35 Therefore, it is advocated that healthy people should not abuse alcohol and should avoid alcohol dependence to prevent the occurrence of MD and that MD patients should abstain from alcohol in a timely manner at the early stage of the disease to avoid further enlargement of cellulite. Although these measures may not significantly reverse or improve the disease, they may help to control further deterioration.
In our study, we systematically evaluated the comorbidities of MD patients, whose cases were often complicated with endocrine, digestive, cardiovascular, nervous, respiratory and other system diseases, as well as cancer. More than 80% of the patients had endocrine system diseases, including hyperlipidemia, hyperuricemia, diabetes, and obesity, which may have been associated with the unhealthy lifestyles of the MD patients, such as long-term alcohol abuse, smoking, and an unreasonable dietary structure. In addition, patients with MD may have decreased insulin bioactivity, insulin resistance, and impaired lipid and protein metabolic pathways, which lead to the development of metabolic syndrome.35–37 Approximately 75% of patients exhibit liver diseases, including elevated liver enzymes, fatty liver, alcoholic cirrhosis, and alcoholic hepatitis. The liver is the main organ of alcohol metabolism. Long-term alcoholism may lead to activation of the oxidative stress response, mitochondrial damage, cytokine release and hepatocyte death in the liver, which further interferes with fat metabolism and results in abnormal fat deposition.38,39
Notably, 24 patients (44.44%) had cases that were complicated with urinary system diseases, including 7 patients with proteinuria or/and hematuria and 17 patients with eGFR < 90 mL/min/1.73 m2, of whom 1 was undergoing regular hemodialysis. Pan et al40 and Joo et al41 reported that alcohol abuse or dependence was associated with a nearly twofold increase in the mortality of CKD, especially in populations younger than 65 years and with an eGFR less than 60 mL/min/1.73 m2.40,41 Additionally, metabolic disorders such as obesity, glucose intolerance, hyperlipidemia and hyperuricemia, which are common in the majority of MD patients, are associated with a significantly increased risk of CKD progression.42–45 Therefore, we speculated that alcoholism and metabolic disorders may be risk factors for the increased susceptibility of patients with MD to renal impairment.
MD is recognized as a benign lesion, and abnormal fat deposition generally does not lead to further malignancy. However, in our study, it was found that more than 20% (11 patients) of MD cases were complicated with and up to now, a total of 9.26% died of malignant tumors, of which digestive tract cancer, lung cancer and thyroid cancer were more common. Previous epidemiological data have demonstrated that long-term alcohol consumption is an important risk factor for gastrointestinal cancer.46 Acetaldehyde, a metabolite of ethanol in alcoholic beverages, has been classified as a group 1 carcinogen in humans by the World Health Organization and the International Agency for Research on Cancer.47 A study of large sample data showed that smoking, overweight, consumption of red meat and processed meat, and lack of regular exercise have all been reported as common risk factors for cancer. A total of 19.0% of cancer patients were exposed to risk factors for smoking, followed by alcohol abuse (5.6%).48 Hence, we speculated that long-term heavy smoking and alcohol abuse, as well as unhealthy eating habits, are common risk factors for MD and malignancy, and their synergistic effect may be the mechanism for the increased incidence of malignant tumors in MD patients.49 Therefore, we recommend that when treating MD patients, doctors should conduct a comprehensive assessment of their comorbidities to develop individualized and integrated treatment plans.
As a rare disease, there are no widely accepted systematic diagnostic criteria yet, which causes difficulties for the clinical diagnosis of MD and increases the rate of misdiagnosis and missed diagnosis to a certain extent. The diagnosis of MD is mostly based on physical examination and clinical features, supplemented by imaging examinations, and matched with the pathological diagnosis.3,10,50 The majority of MD patients have a history of alcoholism, and the appearance is characterized by a symmetrical distribution of adipose tissue. The presence of typical “hamster cheeks”, “horse collars”, and “buffalo humps” aids in the diagnosis. Ultrasound, computed tomography, and magnetic resonance imaging show symmetrically distributed unencapsulated fat deposits within the subcutaneous tissue or in the spaces between muscles. Postoperative pathology revealed no encapsulated lipoma. It is necessary to exclude other disorders with excess adipose tissue in the differential diagnosis, such as morbid obesity, encapsulated lipoma, liposarcoma, Cushing’s syndrome, salivary gland disease, goiter, thyroid carcinoma, and cysts of the neck.9,10,50
Patients often come to the hospital for an evaluation of painless masses in areas such as the neck, chest or back. Most MD patients have no obvious symptoms, and a few patients have larger masses that compress the upper mediastinum, leading to severe symptoms such as asthma, snoring, obstructive sleep apnea symptoms and even dyspnea.35,51 At present, there is no specific drug to treat MD. Oral β2-agonists (such as salbutamol) and fibrate treatment have been reported to prevent fat deposition and promote lipolysis, but their efficacy has not been confirmed.3,52 Surgery is still the most valid treatment for MD. Common surgical procedures include lipotomy and liposuction. The selection of the surgical method should be based on the volume and location of fat deposits, the tolerance of patients to surgery and the psychological expectations of patients.10 Open surgery can completely remove fat deposition and reduce the recurrence rate due to good exposure, but the trauma is extensive.3,12 In contrast, liposuction has a smaller wound area and fewer postoperative complications, but its clearance rate is lower, and the postoperative recurrence rate is much higher than that of lipotomy. Therefore, new treatment techniques are needed to integrate the advantages of the two methods to achieve better therapeutic effects. In recent years, with the development of equipment and technology, new liposuction technologies, such as power-assisted liposuction and ultrasound-assisted liposuction, have provided new ideas for the treatment of MD.10,53 For fat deposits in the neck and small areas of cellulite, these techniques can improve the body contour and tighten the skin to achieve satisfactory local shaping and cosmetic results.54,55 In our study, more than 70% of the patients underwent one or more local lipotomies. The rate of postoperative recurrence was nearly 40%. Prominently, one patient underwent neck fat resection 3 times repeatedly due to different degrees of postoperative recurrence. In view of the high recurrence rate of MD, regular postoperative follow-up is essential.
There are some limitations to our study. First, the sample size was small, and data from larger populations are lacking, which limited our statistical power. Second, this retrospective study has the inherent weakness of retrospective analysis, with recall biases and differential follow-up among patients. Third, the monotonicity of the study population limits the universality of our results.
Conclusion
In general, MD is more likely to occur in middle-aged men with alcohol abuse, who often come to the hospital for an evaluation of painless masses in the neck or other body parts. The diagnosis of MD is primarily based on physical examination, clinical history, and imaging examinations, matched with pathological findings. Patients with MD often exhibit multiple systemic diseases, and a small number of patients may have malignant tumors. Surgery is still an effective treatment, but postoperative recurrence is relatively common. In view of the above characteristics, we recommend that doctors comprehensively assess the patient’s condition and complications when receiving MD patients, advocate that patients quit alcohol and smoking as soon as possible, establish healthy dietary and living habits, and formulate individualized and comprehensive diagnosis and treatment plans in the hope of achieving satisfactory results.
Ethical Approval
This study was performed in accordance with the tenets of the Declaration of Helsinki and approved by the Ethics Committee of the Affiliated Hospital of Qingdao University and Qingdao Municipal Hospital. Every participant voluntarily signed an informed consent form.
Funding
This work was supported by grants from the National Natural Science Foundation of Shandong Province (ZR2020QH060), the National Natural Science Foundation of China (81770679, 81470973, and 81970582), and the Qingdao Key Health Discipline Development Fund. No funding bodies had any role in the study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Brodie BC. Clinical lectures on surgery delivered at St. George’s Hospital. Philadelphia: Lea & Blanchard; 1846: 201–10.
2. Madelung OW. Ueber den Fetthals. Arch Klin Chir. 1888;37:106–130.
3. Brea-García B, Cameselle-Teijeiro J, Couto-González I, Taboada-Suárez A, González-álvarez E. Madelung’s disease: comorbidities, fatty mass distribution, and response to treatment of 22 patients. Aesthetic Plast Surg. 2013;37(2):409–416. doi:10.1007/s00266-012-9874-5
4. Pollock M, Nicholson G, Nukada H, Cameron S, Frankish P. Neuropathy in multiple symmetric lipomatosis. Madelung’s disease. Brain. 1988;111(5):1157–1171. doi:10.1093/brain/111.5.1157
5. Chen C, Fang Q, Wang X, et al. Madelung’s disease: lipectomy or liposuction? Biomed Res Int. 2018;2018:3975974. doi:10.1155/2018/3975974
6. Vassallo G, Mirijello A, Tarli C, et al. Madelung’s disease and acute alcoholic hepatitis: case report and review of literature. Eur Rev Med Pharmacol Sci. 2019;23(14):6272–6276. doi:10.26355/eurrev_201907_18448
7. Hirose A, Okada Y, Morita E, Tanaka Y. Benign symmetric lipomatosis associated with alcoholism. Intern Med. 2006;45(17):1001–1005. doi:10.2169/internalmedicine.45.1791
8. Jang JH, Lee A, Han SA, Ryu JK, Song JY. Multiple Symmetric lipomatosis (Madelung’s Disease) presenting as bilateral huge gynecomastia. J Breast Cancer. 2014;17(4):397–400. doi:10.4048/jbc.2014.17.4.397
9. Gao Y, Hu JL, Zhang XX, Zhang MS, Lu Y. Madelung’s disease: is insobriety the chief cause? Aesthetic Plast Surg. 2017;41(5):1208–1216. doi:10.1007/s00266-017-0920-1
10. Liu Q, Lyu H, Xu B, Lee J. Madelung disease epidemiology and clinical characteristics: a systemic review. Aesthetic Plast Surg. 2021;45(3):977–986. doi:10.1007/s00266-020-02083-5
11. Enzi G, Busetto L, Ceschin E, Coin A, Digito M, Pigozzo S. Multiple symmetric lipomatosis: clinical aspects and outcome in a long-term longitudinal study. Int J Obes Relat Metab Disord. 2002;26(2):253–261. doi:10.1038/sj.ijo.0801867
12. Pinto C, Carvalho P, Correia M. Madelung’s disease: revision of 59 surgical cases. Aesthetic Plast Surg. 2017;41(2):359–368. doi:10.1007/s00266-016-0759-x
13. Chinese nutrition society, dietary guidelines for Chinese residents; 2016. Available from: http://dg.cnsoc.org/article/2007b.html.
14. Wang D, Chen J, Zhou Y, et al. Association between sleep duration, sleep quality and hyperlipidemia in middle-aged and older Chinese: the Dongfeng-Tongji cohort study. Eur J Prev Cardiol. 2019;26(12):1288–1297. doi:10.1177/2047487319843068
15. Joint committee issued Chinese guideline for the management of dyslipidemia in adults. 2016年中国成人血脂异常防治指南. [2016 Chinese guideline for the management of dyslipidemia in adults]. Zhonghua Xin Xue Guan Bing Za Zhi. 2016;44(10):833–853. Chinese. doi:10.3760/cma.j.issn.0253-3758.2016.10.005
16. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39(2 Suppl 1):S1–266.
17. Gao M, Lv J, Yu C, et al. Metabolically healthy obesity, transition to unhealthy metabolic status, and vascular disease in Chinese adults: a cohort study. PLoS Med. 2020;17(10):e1003351. doi:10.1371/journal.pmed.1003351
18. American Diabetes Association. 2. classification and diagnosis of diabetes: standards of medical care in diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S14–S31. doi:10.2337/dc20-S002.
19. Chaker L, Bianco A, Jonklaas J, Peeters R. Hypothyroidism. Lancet. 2017;390(10101):1550–1562. doi:10.1016/s0140-6736(17)30703-1
20. Lu J, Lu Y, Wang X, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1·7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet. 2017;390(10112):2549–2558. doi:10.1016/s0140-6736(17)32478-9
21. Singal A, Bataller R, Ahn J, Kamath P, Shah V. ACG clinical guideline: alcoholic liver disease. Am J Gastroenterol. 2018;113(2):175–194. doi:10.1038/ajg.2017.469
22. Enzi G. Multiple symmetric lipomatosis: an updated clinical report. Medicine. 1984;63(1):56–64. doi:10.1097/00005792-198401000-00004
23. Donhauser G, Vieluf D, Ruzicka T, Braun-Falco O. Benigne symmetrische lipomatose launois-bensaude Typ III und Bureau-Barrière-Syndrom [Benign symmetric Launois-Bensaude type III lipomatosis and Bureau-Barrière syndrome]. Hautarzt. 1991;42(5):311–314.
24. Prantl L, Schreml J, Gehmert S, et al. Transcription profile in sporadic multiple symmetric lipomatosis reveals differential expression at the level of adipose tissue-derived stem cells. Plast Reconstr Surg. 2016;137(4):1181–1190. doi:10.1097/prs.0000000000002013
25. Musumeci O, Barca E, Lamperti C, et al. Lipomatosis incidence and characteristics in an Italian cohort of mitochondrial patients. Front Neurol. 2019;10:160. doi:10.3389/fneur.2019.00160
26. Plummer C, Spring PJ, Marotta R, et al. Multiple symmetrical lipomatosis–a mitochondrial disorder of brown fat. Mitochondrion. 2013;13(4):269–276. doi:10.1016/j.mito.2013.03.003
27. Caponnetto F, Manini I, Bulfoni M, et al. Human adipose-derived stem cells in Madelung’s disease: morphological and functional characterization. Cells. 2020;10(1):44. doi:10.3390/cells10010044
28. Vilà M, Gámez J, Solano A, et al. Uncoupling protein-1 mRNA expression in lipomas from patients bearing pathogenic mitochondrial DNA mutations. Biochem Biophys Res Commun. 2000;278(3):800–802. doi:10.1006/bbrc.2000.3828
29. Iglesias L, Pérez-Llantada E, Saro G, Pino M, Hernández J. Benign symmetric lipomatosis (Madelung’s disease). Eur J Intern Med. 2000;11(3):171–173. doi:10.1016/s0953-6205(00)00086-8
30. Wan SC, Huang MH, Perng CK, Liao WC. Madelung disease: analysis of clinicopathological experience in Taipei veterans general hospital. Ann Plast Surg. 2019;82(1S Suppl 1):S66–S71. doi:10.1097/SAP.0000000000001719
31. Enzi G, Busetto L, Sergi G, et al. Multiple symmetric lipomatosis: a rare disease and its possible links to brown adipose tissue. Nutr Metab Cardiovasc Dis. 2015;25(4):347–353. doi:10.1016/j.numecd.2015.01.010
32. Busetto L, Sträter D, Enzi G, et al. Differential clinical expression of multiple symmetric lipomatosis in men and women. Int J Obes Relat Metab Disord. 2003;27(11):1419–1422. doi:10.1038/sj.ijo.0802427
33. El Hasbani G, Assaker R, Nithisoontorn S, et al. Madelung’s disease leading to presenile dementia in a non-alcoholic patient. Med Arch. 2019;73(4):285–287. doi:10.5455/medarh.2019.73.285-287
34. Jung K, Lee S. A case report of Multiple Symmetric Lipomatosis (MSL) in an East Asian Female. BMC Women's Health. 2020;20(1):200. doi:10.1186/s12905-020-01055-w
35. González-García R, Rodríguez-Campo F, Sastre-Pérez J, Muñoz-Guerra M. Benign symmetric lipomatosis (Madelung’s disease): case reports and current management. Aesthetic Plast Surg. 2004;28(2):108–112. doi:10.1007/s00266-004-3123-5.
36. Kratz C, Lenard H, Ruzicka T, Gärtner J. Multiple symmetric lipomatosis: an unusual cause of childhood obesity and mental retardation. Eur J Paediatr Neurol. 2000;4(2):63–67. doi:10.1053/ejpn.2000.0264
37. Lemaitre M, Chevalier B, Jannin A, Bourry J, Espiard S, Vantyghem M. Multiple symmetric and multiple familial lipomatosis. Presse Med. 2021;50(3):104077. doi:10.1016/j.lpm.2021.104077
38. Ceni E, Mello T, Galli A. Pathogenesis of alcoholic liver disease: role of oxidative metabolism. World J Gastroenterol. 2014;20(47):17756–17772. doi:10.3748/wjg.v20.i47.17756
39. Louvet A, Mathurin P. Alcoholic liver disease: mechanisms of injury and targeted treatment. Nat Rev Gastroenterol Hepatol. 2015;12(4):231–242. doi:10.1038/nrgastro.2015.35
40. Pan C, Ju T, Lee C, et al. Alcohol use disorder tied to development of chronic kidney disease: a nationwide database analysis. PLoS One. 2018;13(9):e0203410. doi:10.1371/journal.pone.0203410
41. Joo Y, Koh H, Nam K, et al. Alcohol consumption and progression of chronic kidney disease: results from the Korean cohort study for outcome in patients with chronic kidney disease. Mayo Clin Proc. 2020;95(2):293–305. doi:10.1016/j.mayocp.2019.06.014
42. Yun H, Kim H, Park J, et al. Obesity, metabolic abnormality, and progression of CKD. Am J Kidney Dis. 2018;72(3):400–410. doi:10.1053/j.ajkd.2018.02.362
43. Nehus E. Obesity and chronic kidney disease. Curr Opin Pediatr. 2018;30(2):241–246. doi:10.1097/mop.0000000000000586
44. Mallat S, Al Kattar S, Tanios B, Jurjus A. Hyperuricemia, hypertension, and chronic kidney disease: an emerging association. Curr Hypertens Rep. 2016;18(10):74. doi:10.1007/s11906-016-0684-z
45. Snyder S, Turner G, Turner A. Obesity-related kidney disease. Prim Care. 2014;41(4):875–893. doi:10.1016/j.pop.2014.08.008
46. Pöschl G, Seitz H. Alcohol and cancer. Alcohol Alcohol. 2004;39(3):155–165. doi:10.1093/alcalc/agh057
47. Salaspuro M, Mikko S. Interactions of alcohol and tobacco in gastrointestinal cancer. J Gastroenterol Hepatol. 2012;Suppl 2:135–139. doi:10.1111/j.1440-1746.2012.07017.x
48. Islami F, Goding Sauer A, Miller K, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin. 2018;68(1):31–54. doi:10.3322/caac.21440
49. Whiteman D, Wilson L. The fractions of cancer attributable to modifiable factors: a global review. Cancer Epidemiol. 2016;44:203–221. doi:10.1016/j.canep.2016.06.013
50. Jaźwiec P, Pawłowska M, Czerwińska K, Poręba M, Gać P, Poręba R. Madelung’s disease as an example of a metabolic disease associated with alcohol abuse-diagnostic importance of computed tomography. Int J Environ Res Public Health. 2022;19(9):5168. doi:10.3390/ijerph19095168
51. Katou F, Shirai N, Motegi K, Satoh R, Satoh S. Symmetrical lipomatosis of the tongue presenting as macroglossia. Report of two cases. J Craniomaxillofac Surg. 1993;21(7):298–301. doi:10.1016/s1010-5182(05)80351-8
52. Heike Z, Gudrun U, Frank R, Vetter H, Walger P. Multiple benign symmetric lipomatosis–a differential diagnosis of obesity: is there a rationale for fibrate treatment? Obes Surg. 2008;18(2):240–242. doi:10.1007/s11695-007-9247-3
53. Tremp M, Wettstein R, Tchang L, Schaefer D, Rieger U, Kalbermatten D. Power-assisted liposuction (PAL) of multiple symmetric lipomatosis (MSL)–a longitudinal study. Surg Obes Relat Dis. 2015;11(1):155–160. doi:10.1016/j.soard.2014.05.004
54. Faga A, Valdatta L, Thione A, Buoro M. Ultrasound assisted liposuction for the palliative treatment of Madelung’s disease: a case report. Aesthetic Plast Surg. 2001;25(3):181–183. doi:10.1007/s002660010118
55. DiBernardo B. Randomized, blinded split abdomen study evaluating skin shrinkage and skin tightening in laser-assisted liposuction versus liposuction control. Aesthet Surg J. 2010;30(4):593–602. doi:10.1177/1090820x10380707
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
