Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 15
Lycium barbarum Polysaccharide Inhibited Hypoxia-Inducible Factor 1 in COPD Patients
Authors Chen LJ , Xu W, Li YP, Ma LT, Zhang HF, Huang XB, Yu GG, Ma XQ, Chen C, Liu YH, Wu J, Wang LJ, Xu Y
Received 16 March 2020
Accepted for publication 12 June 2020
Published 24 August 2020 Volume 2020:15 Pages 1997—2004
DOI https://doi.org/10.2147/COPD.S254172
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Li-Jun Chen,1,2 Wang Xu,1 Ya-Ping Li,3 Li-Ting Ma,1 Hui-Fang Zhang,1 Xiao-Bo Huang,1 Geng-Geng Yu,1 Xiu-Qin Ma,1 Chao Chen,1 Yan-Hong Liu,1 Jie Wu,4 Li-Jun Wang,4 Yuan Xu4
1Department of Respiratory and Critical Medicine, The First People’s Hospital of Yinchuan City, Yinchuan, Ningxia, People’s Republic of China; 2Department of Respiratory and Critical Medicine, The Second Affiliated Hospital of Ningxia Medical University, Yinchuan, Ningxia, People’s Republic of China; 3Department of Respiratory Medicine, Weihai Municipal Hospital of Shandong Province, Weihai, Shandong, People’s Republic of China; 4Department of Clinical Institute, Ningxia Medical University, Yinchuan, Ningxia, People’s Republic of China
Correspondence: Li-Jun Chen
Department of Respiratory and Critical Medicine, The Second Affiliated Hospital of Ningxia Medical University, No. 2, Liqun West Street, Xingqing District, Yinchuan, Ningxia 750001, People’s Republic of China
Tel +86-13895016600
Fax +86-951-6192235
Email [email protected]
Background: Chronic obstructive pulmonary disease (COPD) is a chronic airway inflammatory disease characterized by irreversible airflow obstruction. Pathogenic mechanisms underlying COPD remain largely unknown.
Objective: The current study was designed to explore serum concentration of hypoxia-inducible factor 1α (HIF-1α) in stable COPD patients and the potential effect of Lycium barbarum polysaccharides (LBP) on HIF-1α protein expression.
Methods: Serum HIF-1α was quantified by ELISA in 102 stable COPD patients before and after 2-week orally taken LBP (100 mL/time, twice daily, 5– 15 mg/mL). Correlation of serum LBP and lung function (FEV1%) or blood gas (PO2 and PCO2) was also analyzed. As a control, 105 healthy subjects were also enrolled into this study.
Results: Serum concentration of HIF-1α was significantly higher in the stable COPD patients (37.34 ± 7.20 pg/mL) than that in the healthy subjects (29.55 ± 9.66 pg/mL, P< 0.001). Oral administration of LBP (5 mg/mL, 100 mL, twice daily for 2 weeks) not only relieved COPD symptoms but also significantly reduced serum HIF-1α concentration (36.94 ± 9.23 vs 30.49 ± 6.42 pg/mL, P< 0.05). In addition, level of serum HIF-1α concentration was significantly correlated with PCO2 (r = 0.283, P< 0.001), but negatively and significantly correlated with PO2 (r = − 0.490, P=0.005) or FEV1%(r = − 0.420, P=0.018).
Conclusion: These findings suggested that activation of HIF-1 signaling pathway may be involved in the pathophysiology of COPD and that stabilization of serum HIF-1α concentration by LBP might benefit the stable COPD patients.
Keywords: chronic obstructive pulmonary disease, COPD, hypoxia-induced factor 1, HIF-1, Lycium barbarum polysaccharides, LBP
Background
Chronic obstructive pulmonary disease (COPD) is a chronic inflammatory disease characterized by progressive and irreversible obstruction of airflow.1 Cigarette smoking is the most common risk factor for COPD.2 However, only 25% of smokers suffer from COPD, which indicates that other risk factors or molecular factors may be involved in the pathogenesis and progression of COPD.3
Hypoxia-inducible factor 1 (HIF-1), a heterodimeric transcription factor composed of HIF-1α and HIF-1ß subunits, is induced by hypoxia under physiological as well as pathological conditions such as COPD. HIF-1 modulates oxygen homeostasis and physiological responses through its effects on vascular remodeling and oxygen utilization through involvement in redox homeostasis and glucose metabolism.4–6 HIF-1 also regulates genes related to angiogenesis, energy metabolism, cell proliferation, and apoptosis.7 Recently, studies indicated that the HIF-1 signaling pathway may be involved in the pathogenesis of COPD.8,9
Lycium barbarum polysaccharide (LBP) is isolated from the Chinese herbal Lycium barbarum. LBP consists of six monosaccharides, namely, glucose, arabinose, galactose, mannose, rhamnose, and xylose.10 They are popular and taken as health supplements in China owing to a number of therapeutic effects, including anti-aging,11 anti-oxidizing properties and metabolic effects,12 and even improving male fertility.13 LBP has also been used in the treatment and/or prevention of various diseases14,15 in that LBP has multiple biological effects including antitumor activity,16,17 immune-regulation,18,19 neuro-protective effect,20 and cardio-protective activity.21
The current study was, therefore, designed to explore serum concentrations of HIF-1 signaling pathway-related protein (HIF-1α) in stable COPD patients in comparison to healthy subjects, and their association with the clinic-pathological characteristics of COPD patients including lung function and blood gas analysis. In addition, the effect of LBP on the alteration of serum HIF-1α was explored.
Methods
Participants
A total of 102 stable COPD patients, who visited The Second Affiliated Hospital of Ningxia Medical University from March 2016 through January 2018, were enrolled into this study. For the control, 105 healthy volunteers were also enrolled.
Patient Inclusion Criteria
Patients who met the following criteria were enrolled: 1) Met the diagnostic criteria of “Diagnostic and Therapeutic Guidelines of Chronic Obstructive Pulmonary Disease (2018) ”defined by The Respiratory Branch, Chinese Thoracic Society.22 2) Stable COPD patients with mild symptoms including cough, expectoration, shortness of breath, and wheezing. 3) FEV1/FVC < 70%; FEV1 reversibility within 15 minute of inhaling ß2-agonist was < 15%; and PO2 < 80%. 4) In order to stabilize COPD symptoms during this study, patients were allowed to use their daily medicines including inhaled corticosteroid (ICS), long acting beta-agonist (LABA), and long acting muscarinic antagonist (LAMA).
Patient Exclusion Criteria
1) Patients complicated with other respiratory system diseases. 2) Patients complicated with malignancy, metabolic disease, autoimmunity disease, thyroid disease, tuberculosis, severe heart failure, or cerebrovascular disease. 3) Patients had used antibiotics within 1 month before the enrollment. 4). Patients who had an acute exacerbation of COPD within 1 month before enrollment.
Healthy control subjects were enrolled from the volunteers who visited the hospital for a preventive physical check. All patients and control subjects were informed about the study plan and a signed consent form was obtained from each participant. The study protocol was approved by the Ethics Committee of The Second Affiliated Hospital, Ningxia Medical University, Ningxia Hui Autonomous Region, People's Republic of China (#: 2016–231).
LBP Treatment
Oral LBP was provided by the Ningxia Kaiyuan Biotechnology Inc. Patients and normal subjects were randomly assigned to the following three groups: low dose group: 5 mg/mL, 100 mL/time, twice daily; medium dose group: 10 mg/mL, 100 mL/time, twice daily; high dose group: 15 mg/mL, 100 mL/time, twice daily. Before and after 2 weeks of LBP administration, blood samples (5 mL) were collected from each participant and serum was stored at −20°C until HIF-1α quantification by ELISA as described below.
HIF-1α Quantification by ELISA
HIF-1α was quantified using an ELISA kit following the manufacturer’s instruction (Shanghai ELISA Biotech, Shanghai, People's Republic of China).
Artery Blood Gas Analysis
Artery blood sample was collected from each participant before and after 2 weeks of treatment with LBP. Blood gas analyses including PO2 and PCO2 were performed using Blood Gas Analysis equipment (RAPIDPiont500, Siemens Healthcare Diagnostics, Germany).
Pulmonary Function Test
Pulmonary function tests including FEV1%, FEV1/FVC% were performed using a spirometer (CHEST HI-101, Japan).
Statistical Analysis
Data were presented as mean ± standard derivation from three independent replications. Statistical differences between the two groups were analyzed using the Student's t=test, and between three or more groups were analyzed with the one-way analysis of variance (ANOVA). Correlation was analyzed by Spearman correlation analysis method. The SPSS version 22.0 software (SPSS Inc., IBM Corporation, Armonk, NY, USA) was used to perform all the statistical analysis. A P-value of < 0.05 was considered to indicate a statistically significant result.
Results
As shown in Table 1, a total of 105 healthy control subjects and 102 stable COPD patients were enrolled into the current study. There were no significant differences in age, height, weight, and gender ratio between the control and COPD groups. However, baseline FEV1, FVC and CAT score were significantly different between the two groups (Table 1). In addition, blood HIF-1α and PCO2 were significantly higher in the COPD patients (HIF-1α: 37.34 ± 7.20 pg/mL; PCO2: 43.06 ±10.44 mmHg) than that in the healthy control subjects (29.55 ± 9.66 pg/mL and 35.70 ± 5.36 mmHg, respectively, P<0.001, Table 1). In contrast, PO2 was significantly lower in the COPD patients (66.05 ± 10.82 mmHg) compared to that in control group (85.34 ± 4.64 mmHg, P<0.001, Table 1).
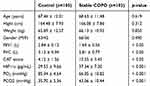 |
Table 1 Comparison of Basic and Clinical Parameters in the Two Groups |
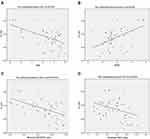
Correlation analyses between HIF-1α and blood gas parameters or lung function tests in stable COPD patients were performed. As shown in Table 2 and Figure 1, HIF-1α was significantly and negatively correlated with PO2 (r = −0.490, P=0.005, Figure 1A), but significantly correlated with PCO2 (r = 0.283, P<0.001, Figure 1B). HIF-1α was significantly and negatively correlated with FEV1% (r = −0.420, P=0.018, Figure 1C) and with FEV1/FVC% (r = −0.540, P=0.002, Figure 1D).
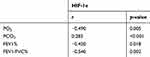 |
Table 2 Correlation Between HIF-1α and Blood Gas Analysis or Lung Function Test |
Stable COPD patients were randomly assigned into the following three groups: a low dose LBP group (34 patients), a medium dose group (34 patients), and a high dose group (34 patients). As shown in Table 3, HIF-1α concentrations before LBP treatment were 36.94 ± 9.23 pg/mL (low), 39.07 ± 7.20 pg/mL (medium), 36.00 ± 4.44 pg/mL (high), respectively. There was no significant difference in the HIF-1α between the three dose groups before LBP treatment. After 2 weeks of treatment with 5 mg/mL (low), 10 mg/mL (medium), and 15 mg/mL (high) LBP, HIF-1α concentration was significantly reduced (low dose: 30.49 ± 6.42; medium dose: 36.62 ± 6.37; high dose: 32.21 ± 6.67, Table 3), which were significantly different between the groups of LBP doses as analyzed by variance analysis (Fdose = 5.358, P<0.01, Table 3), as well as at different time points (Ftime = 7.438, P<0.01, Table 3). However, there was no interaction between different doses of LBP and examination time (F = 0.571, P>0.05).
 |
Table 3 Effect of Various Doses of LBP on HIF-1α |
After 2 weeks of treatment with LBP, the CAT score was evaluated in the COPD patients. As shown in Table 4, after LBP treatment, 13 out of 43 patients (30.23%) had significant relief in chest tightness and shortness of breath; 7 out of 27 patients (25.92%) had significant improvement in sputum expectoration; 7 out of 39 patients (17.95%) had significant improvement in immunity and reduction in suffering from common cold; and 2 out of 11 patients (18.18%) had significant improvement in vitality. However, as shown in Table 5, after LBP treatment, 4 out of 51 patients (7.84%) had constipation and dry mouth; 1 out of 51 patients (1.96%) had gingival swelling; and 1 out of 51 patients (1.96%) had stomach ache. All of the aforementioned adverse effects disappeared after stopping LBP treatment (100% recovery).
 |
Table 4 Effect of LBP on COPD Patients’ Symptom Improvement |
 |
Table 5 Adverse Effect of LBP in the Stable COPD Patients |
Discussion
COPD is a progressive and chronic lung disease associated with inflammation. Hypoxia is one of the pathologic outcomes of chronic airway obstruction. Hypoxia-inducible factor is known to be involved in the pathogenesis of various diseases including COPD.9,23,24 Here, we reported the effect of LBP administration on the level of serum HIF-1α in the stable COPD patients and normal healthy subjects. It was found that serum HIF-1α was significantly higher in the stable COPD patients compared to that of healthy control subjects; that HIF-1α was significantly and negatively correlated with PO2 or FEV1%, but significantly correlated with PCO2; and that serum HIF-1α was significantly reduced after 2 weeks administration of LBP in the stable COPD patients.
COPD is a progressive obstructive lung disease with wheezing and productive cough in clinic. Emphysema and airflow limitation caused by the remodeling of lung structure in COPD result in ventilation/perfusion mismatch, leading to hypoxic conditions, which activates the hypoxia signaling pathway through hypoxia-inducible factors. Hypoxia-inducible factor-1α (HIF-1α) is a vital transcription factor that regulates hypoxic responses.25 HIF-1 is widely expressed in many mammalian and human tissue cells, which are composed of α and β subunits. The independent transactivation domain and an oxygen-dependent degradation domain in carboxyl-terminal determine the HIF-1 activity.25 Typically, oxygen-independent pathways regulate HIF-1 protein expression, while oxygen-dependent pathways regulate HIF-1 degradation.26 Li et al27 reported that HIF-1α regulates the oxygen balance, hypoxia adaptation, inflammatory response, and tumor development. In addition, the role of HIF-1α in allergic inflammation has also been reported.28–30 Here, we have reported that serum HIF-1α was significantly increased in the stable COPD patients even if average PO2 was 66% in these patients, suggesting HIF-1α protein may be up-regulated through oxygen-independent pathway in the stable COPD patients. Furthermore, level of HIF-1α was negatively correlated with PO2 and FEV1%, suggesting HIF-1α might be involved in the pathogenesis of COPD.
Following hypoxia activation of the hypoxia signaling pathway, HIF stabilization plays a key role in the tissue oxygen balance and tissue repair. Numerous studies have demonstrated that stabilization of HIF can reduce tissue inflammation and promote its repair.31–34 In this regard, HIF-1α can render the tissue to metabolically adapt to oxygen deprivation and anaerobic ATP synthesis through up-regulation of glycolytic genes such as phosphoglycerate kinase (PGK) and lactate dehydrogenase A (LDHA).35 Stabilization of HIF by pharmacologic intervention displays a universally protective phenotype across all organs. Accordingly, HIF and its downstream targets are emerging as novel therapeutic options to treat various organ injuries, including the heart, lung, liver, and kidney.15 In the current study, therefore, the effect of LBP intervention on HIF-1α has been investigated. We found that oral administration of LBP could significantly reduce serum HIF-1α in the stable COPD patients. In addition, we found that serum level of HIF-1α was negatively associated with blood PO2 and FEV1%, while HIF-1α was significantly associated with PCO2. Consistently, Sheng and Fan36 reported that LBP increased mice tolerance ability to hypoxia and fatigue, and Li et al37 reported that LBP improved tissue oxygen availability in mice and thus prolonged mice life spans. In addition, it has also reported that LBP significantly suppressed hypoxia-induced up-regulation of HIF-1α mRNA and protein.38 These findings suggested that targeting the HIF signaling pathway in chronic lung disease might be a promising intervention in delaying the progression of disease.
LBP, scopoletin, and 2-O-β-D- glucopyranosyl-L-ascorbic acid (AA-2βG) are the major constituents of the Chinese herbal Lycium barbarum or wolfberry.39 Of them, LBP is the key bioactive ingredient in wolfberry.40 LBP is a popular health supplement due to its wide range of health benefits. LBP has multiple biological activities and functions including anti-aging associated with their anti-oxidizing properties, metabolic effects,11,12 neuro-protective effects in neuro-degeneration and neurotoxicity,41–43 improving male fertility,13 antitumor activity,16,17,44 immune-regulation,18,19,45 and cardio-protective activity.21 Furthermore, LBP could enhance immunity by improving lymphocyte proliferation, and by increasing macrophage phagocytosis and cytotoxic T lymphocyte (CTL) activity.16,44 However, the effect of LBP in chronic lung disease has not been extensively investigated. In this regard, it has been reported that, after orally taking LBP for 4–8 weeks, 85% of the aged population had improvement in sleep and appetite, and 29–85% of the aged population had enhanced immunity and reduced frequency of suffering from the common cold.46 Consistently, here, we have reported that oral administration of LBP could relieve COPD symptoms such as chest tightness and shortness of breath, and reduced frequency of suffering from the common cold in the COPD patients. These findings suggested that LBP might benefit the COPD by enhancing immunity and relieving respiratory symptoms. Interestingly, however, lower dose of LBP had the most significant effect on suppression of HIF-1α. While the mechanism remains to be defined, the lower dose (5 mg/mL) is sufficient and can be used in future studies.
While no documented adverse reactions related to LBP usage have been reported in clinic, there is a lack of awareness amongst the medical and scientific community regarding the safety profile on the use of LBP as a therapeutic agent. In this regard, animal studies found that LBP had no toxicity or sperm deformity effect.47,48 However, the current study demonstrated that oral administration of LBP could result in mild adverse effects including constipation or dry mouth, gingival swelling, and gastric reaction. Nevertheless, the aforementioned adverse effects in response to LBP intake disappeared when the patients stopped taking LBP, suggesting LBP-associated side effects are transient and reversible.
There were limitations in the current study. First, COPD patients enrolled into this study were at a stable stage and allowed to continue using their daily medicines including ICS, LABA, and LAMA, which might interact with LBP. Second, clinical symptoms and CAT scores were compared before and after LBP treatment, but not between the three-dose treatment groups due to the limited number of cases. Third, HIF-1α is a transcription factor that may be involved in mediating COPD pathogenesis. While the primary finding of the current study was that LBP significantly suppressed HIF-1α protein, the biological impact of LBP suppression on HIF-1α in COPD remains to be further investigated.
Taken together, the current study demonstrated that serum HIF-1α was significantly higher in the stable COPD patients compared to that in the normal subject. The level of HIF-1α was significantly correlated with the PCO2 level, but negatively correlated with PO2 or FEV1% in COPD patients. Oral administration of LBP could significantly reduce serum HIF-1α concentration in the stable COPD patients. These findings suggest that HIF-1α may be involved in the pathophysiology of COPD and LBP may benefit stable COPD patients through reducing serum HIF-1α.
Abbreviations
COPD, chronic obstructive pulmonary disease; HIF-1, hypoxia-inducible factor 1; LBP, Lycium barbarum polysaccharides.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the Declaration of Helsinki. The study protocol was approved by the Ethics Committee of The Second Affiliated Hospital of Ningxia Medical University. Written informed consent was obtained from all study subjects before enrollment.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Vestbo J, Hurd SS, Rodriguez-Roisin R. The 2011 revision of the global strategy for the diagnosis, management and prevention of COPD (GOLD)–why and what? Clin Respir J. 2012;6(4):208–214. doi:10.1111/crj.12002
2. Fullerton DG, Gordon SB, Calverley PM. Chronic obstructive pulmonary disease in non-smokers. Lancet. 2009;374(9706):
3. Barnes PJ. Cellular and molecular mechanisms of chronic obstructive pulmonary disease. Clin Chest Med. 2014;35(1):71–86. doi:10.1016/j.ccm.2013.10.004
4. Semenza GL. Hypoxia-inducible factor 1 and cardiovascular disease. Annu Rev Physiol. 2014;76:39–56. doi:10.1146/annurev-physiol-021113-170322
5. Zhao X, Gao S, Ren H, et al. Hypoxia-inducible factor-1 promotes pancreatic ductal adenocarcinoma invasion and metastasis by activating transcription of the actin-bundling protein fascin. Cancer Res. 2014;74(9):2455–2464. doi:10.1158/0008-5472.CAN-13-3009
6. Gui D, Li Y, Chen X, Gao D, Yang Y, Li X. HIF1 signaling pathway involving iNOS, COX2 and caspase9 mediates the neuroprotection provided by erythropoietin in the retina of chronic ocular hypertension rats. Mol Med Rep. 2015;11(2):1490–1496. doi:10.3892/mmr.2014.2859
7. Szkandera J, Knechtel G, Stotz M, et al. Association of hypoxia-inducible factor 1-alpha gene polymorphisms and colorectal cancer prognosis. Anticancer Res. 2010;30(6):2393–2397.
8. Yu ZG, Wang BZ, Cheng ZZ. The association of genetic polymorphisms of hypoxia inducible factor-1 alpha and vascular endothelial growth factor with increased risk of chronic obstructive pulmonary disease: a case-control study. Kaohsiung J Med Sci. 2017;33(9):433–441. doi:10.1016/j.kjms.2017.05.014
9. Fu X, Zhang F. Role of the HIF-1 signaling pathway in chronic obstructive pulmonary disease. Exp Ther Med. 2018;16(6):4553–4561. doi:10.3892/etm.2018.6785
10. Cheng J, Zhou ZW, Sheng HP, et al. An evidence-based update on the pharmacological activities and possible molecular targets of Lycium barbarum polysaccharides. Drug Des Devel Ther. 2015;9:33–78. doi:10.2147/DDDT.S72892
11. Deng HB, Cui DP, Jiang JM, Feng YC, Cai NS, Li DD. Inhibiting effects of Achyranthes bidentata polysaccharide and Lycium barbarum polysaccharide on nonenzyme glycation in D-galactose induced mouse aging model. Biomed Environ Sci. 2003;16(3):267–275.
12. Luo Q, Cai Y, Yan J, Sun M, Corke H. Hypoglycemic and hypolipidemic effects and antioxidant activity of fruit extracts from Lycium barbarum. Life Sci. 2004;76(2):137–149. doi:10.1016/j.lfs.2004.04.056
13. Shi GJ, Zheng J, Wu J, et al. Protective effects of Lycium barbarum polysaccharide on male sexual dysfunction and fertility impairments by activating hypothalamic pituitary gonadal axis in streptozotocin-induced type-1 diabetic male mice. Endocr J. 2017;64(9):907–922. doi:10.1507/endocrj.EJ16-0430
14. Kwok SS, Bu Y, Lo AC, et al. A systematic review of potential therapeutic use of Lycium barbarum polysaccharides in disease. Biomed Res Int. 2019;2019:4615745. doi:10.1155/2019/4615745
15. Lee JW, Ko J, Ju C, Eltzschig HK. Hypoxia signaling in human diseases and therapeutic targets. Exp Mol Med. 2019;51(6):68. doi:10.1038/s12276-019-0235-1
16. Gan L, Hua Zhang S, Liang Yang X, Bi Xu H. Immunomodulation and antitumor activity by a polysaccharide-protein complex from Lycium barbarum. Int Immunopharmacol. 2004;4(4):563–569. doi:10.1016/j.intimp.2004.01.023
17. Zhang M, Tang X, Wang F, Zhang Q, Zhang Z. Characterization of Lycium barbarum polysaccharide and its effect on human hepatoma cells. Int J Biol Macromol. 2013;61:270–275. doi:10.1016/j.ijbiomac.2013.06.031
18. Bo R, Sun Y, Zhou S, et al. Simple nanoliposomes encapsulating Lycium barbarum polysaccharides as adjuvants improve humoral and cellular immunity in mice. Int J Nanomedicine. 2017;12:6289–6301. doi:10.2147/IJN.S136820
19. Zhang XR, Qi CH, Cheng JP, et al. Lycium barbarum polysaccharide LBPF4-OL may be a new Toll-like receptor 4/MD2-MAPK signaling pathway activator and inducer. Int Immunopharmacol. 2014;19(1):132–141. doi:10.1016/j.intimp.2014.01.010
20. Teng P, Li Y, Cheng W, Zhou L, Shen Y, Wang Y. Neuroprotective effects of Lycium barbarum polysaccharides in lipopolysaccharide-induced BV2 microglial cells. Mol Med Rep. 2013;7(6):1977–1981. doi:10.3892/mmr.2013.1442
21. Xin YF, Wan LL, Peng JL, Guo C. Alleviation of the acute doxorubicin-induced cardiotoxicity by Lycium barbarum polysaccharides through the suppression of oxidative stress. Food Chem Toxicol. 2011;49(1):259–264. doi:10.1016/j.fct.2010.10.028
22. CTS. Guidelines of COPD for primary doctors. Chin J Gen Pract. 2018;11(17):856–870.
23. Yasuo M, Mizuno S, Kraskauskas D, et al. Hypoxia inducible factor-1alpha in human emphysema lung tissue. Eur Respir J. 2011;37(4):775–783. doi:10.1183/09031936.00022910
24. Zhang HX, Yang JJ, Zhang SA, et al. HIF-1alpha promotes inflammatory response of chronic obstructive pulmonary disease by activating EGFR/PI3K/AKT pathway. Eur Rev Med Pharmacol Sci. 2018;22(18):6077–6084. doi:10.26355/eurrev_201809_15946
25. Mo JH, Kim JH, Lim DJ, Kim EH. The role of hypoxia-inducible factor 1alpha in allergic rhinitis. Am J Rhinol Allergy. 2014;28(2):e100–e106. doi:10.2500/ajra.2014.28.4025
26. Semenza GL. Targeting HIF-1 for cancer therapy. Nat Rev Cancer. 2003;3(10):721–732. doi:10.1038/nrc1187
27. Li J, Xu Y, Jiao H, Wang W, Mei Z, Chen G. Sumoylation of hypoxia inducible factor-1alpha and its significance in cancer. Sci China Life Sci. 2014;57(7):657–664. doi:10.1007/s11427-014-4685-3
28. Karpel-Massler G, Westhoff MA, Kast RE, et al. Simultaneous Interference with HER1/EGFR and RAC1 signaling drives cytostasis and suppression of survivin in human glioma cells in vitro. Neurochem Res. 2017;42(5):1543–1554. doi:10.1007/s11064-017-2213-0
29. York ER, Varella-Garcia M, Bang TJ, Aisner DL, Camidge DR. Tolerable and effective combination of full-dose crizotinib and osimertinib targeting MET amplification sequentially emerging after T790M positivity in EGFR-mutant non-small cell lung cancer. J Thorac Oncol. 2017;12(7):e85–e88. doi:10.1016/j.jtho.2017.02.020
30. Tosuner Z, Bozkurt SU, Kilic T, Yilmaz B. The role of EGFR, hepatocyte growth factor receptor (c-Met), c-ErbB2 (HER2-neu) and clinicopathological parameters in the pathogenesis and prognosis of chordoma. Turk Patoloji Derg. 2017;33(2):112–120. doi:10.5146/tjpath.2016.01378
31. Kiers D, Wielockx B, Peters E, et al. Short-term hypoxia dampens inflammation in vivo via enhanced adenosine release and adenosine 2B receptor stimulation. EBioMedicine. 2018;33:144–156. doi:10.1016/j.ebiom.2018.06.021
32. Bowser JL, Lee JW, Yuan X, Eltzschig HK. The hypoxia-adenosine link during inflammation. J Appl Physiol. 2017;123(5):1303–1320. doi:10.1152/japplphysiol.00101.2017
33. Riegel AK, Faigle M, Zug S, et al. Selective induction of endothelial P2Y6 nucleotide receptor promotes vascular inflammation. Blood. 2011;117(8):2548–2555. doi:10.1182/blood-2010-10-313957
34. Yuan X, Lee JW, Bowser JL, Neudecker V, Sridhar S, Eltzschig HK. Targeting hypoxia signaling for perioperative organ injury. Anesth Analg. 2018;126(1):308–321. doi:10.1213/ANE.0000000000002288
35. Hu CJ, Wang LY, Chodosh LA, Keith B, Simon MC. Differential roles of hypoxia-inducible factor 1alpha (HIF-1alpha) and HIF-2alpha in hypoxic gene regulation. Mol Cell Biol. 2003;23(24):9361–9374. doi:10.1128/MCB.23.24.9361-9374.2003
36. Sheng W, Fan W. Effect of Lycium barbarum polysaccharide on ability of hypoxia and anti-fatigue in mice. J Xinxiang Med Coll. 2011;28(3):298–300.
37. Li X, Wang B, Liu J, Zhang S. Study of effect of LBP on antihypoxia in mice. J Huazhong Agricl Univ. 1999;18(3):283–285.
38. Zhu Y, Sun Y, Guan W, et al. Lycium barbarum polysaccharides enhances SIRT1 expression and decreases MMP-9 and HIF-1a expression in hypoxic pulmonary vascular smooth muscle cells. Chin J Cell Mol Immunol. 2016;7(7):906–940.
39. Chen W, Cheng X, Chen J, et al. Lycium barbarum polysaccharides prevent memory and neurogenesis impairments in scopolamine-treated rats. PLoS One. 2014;9(2):e88076. doi:10.1371/journal.pone.0088076
40. Kou L, Du M, Zhang C, et al. Polysaccharide purified from Lycium barbarum protects differentiated PC12 cells against LGlu-induced toxicity via the mitochondria-associated pathway. Mol Med Rep. 2017;16(4):5533–5540. doi:10.3892/mmr.2017.7289
41. Ho YS, Yu MS, Lai CS, So KF, Yuen WH, Chang RC. Characterizing the neuroprotective effects of alkaline extract of Lycium barbarum on beta-amyloid peptide neurotoxicity. Brain Res. 2007;1158:123–134. doi:10.1016/j.brainres.2007.04.075
42. Ho YS, Yu MS, Yik SY, So KF, Yuen WH, Chang RC. Polysaccharides from wolfberry antagonizes glutamate excitotoxicity in rat cortical neurons. Cell Mol Neurobiol. 2009;29(8):1233–1244. doi:10.1007/s10571-009-9419-x
43. Chiu K, Chan HC, Yeung SC, et al. Modulation of microglia by wolfberry on the survival of retinal ganglion cells in a rat ocular hypertension model. J Ocul Biol Dis Infor. 2009;2(2):47–56. doi:10.1007/s12177-009-9023-9
44. Zhu C, Zhang S. The antitumor and immunoenhancement activity of Lycium barbarum polysaccharides in hepatoma H-22-bearing mice. Acta Nutr Sin. 2006;28:182–183.
45. Zhu J, Zhao LH, Zhao XP, Chen Z. Lycium barbarum polysaccharides regulate phenotypic and functional maturation of murine dendritic cells. Cell Biol Int. 2007;31(6):615–619. doi:10.1016/j.cellbi.2006.12.002
46. Sheng B, Zhao X, Liang K. Regulatory effect of Lycium barbarum on immunity in over 60 seniors. Pharmacol Clin Chin Mater Med. 1988;4(2):43–44.
47. Mu B, Liu X, Xiong J, Gou A. Acute toxicity and mutagenicity of Lycium barbarum polysaccharides. J Environ Occup Med. 2002;19(2):201–202.
48. Li W, Dai S, Shao W. Effect of oral administration of Lycium barbarum on superoxide dismutase, Hb, and LPD in seniors. Chin Traditional Herbal Drugs. 1991;22(6):25–26.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.