Back to Journals » Clinical Ophthalmology » Volume 9
Lowered intraocular pressure in a glaucoma patient after intravitreal injection of ocriplasmin
Authors McClintock M, MacCumber M, Sun C
Received 26 March 2015
Accepted for publication 11 June 2015
Published 23 October 2015 Volume 2015:9 Pages 1995—1998
DOI https://doi.org/10.2147/OPTH.S85509
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Michael McClintock,1 Mathew W MacCumber1,2
1Department of Ophthalmology, Rush University Medical Center, 2Illinois Retina Associates, S.C., Chicago, IL, USA
Abstract: We report the case of a glaucoma patient who received a single intravitreal injection of 125 µg ocriplasmin for vitreomacular traction in the right eye. The patient had bilateral advanced glaucoma and had previously undergone an implantation of an Ahmed glaucoma valve in the right eye and trabeculectomy in both eyes. The patient was using three topical ophthalmic intraocular pressure (IOP)-lowering medications on the day of injection. Baseline uncorrected Snellen visual acuity was 20/80-1 and IOP was 19 mmHg. Resolution of vitreomacular traction was achieved 1 week after injection. IOP was transiently decreased, reaching a maximum reduction of 12 mmHg below baseline at 1 month after injection, when serous choroidal effusion was also present. IOP returned to baseline levels and choroidal effusion resolved at 2 months after injection of IOP-lowering medication. Vitrectomy with epiretinal membrane and internal limiting membrane peeling, endolaser photocoagulation, and fluid–gas exchange were performed in the right eye ~3.5 months after injection to treat persistent epiretinal membrane, and presumed tractional retinal detachment. Final visual acuity was 20/50+ and IOP was 18 mmHg at 16 weeks after surgery. To our knowledge, this is the first report of IOP reduction and serous choroidal effusion after ocriplasmin injection.
Keywords: ocriplasmin, intraocular pressure, vitrectomy, choroidal effusion
Introduction
Vitreomacular traction (VMT) is a sight-threatening condition that can lead to reduced visual acuity (VA) and metamorphopsia.1,2 Intraocular pressure (IOP) deviations are not known to be associated with VMT. Current VMT management strategies include observation, vitrectomy, and pharmacologic vitreolysis with ocriplasmin (recombinant truncated human plasmin).1,3 The safety and efficacy of a single intravitreal injection of 125 μg ocriplasmin for the resolution of symptomatic vitreomacular adhesion (including VMT) has been demonstrated.1,2 A significantly greater proportion of patients receiving ocriplasmin versus (vs) vehicle achieved resolution of vitreomacular adhesion (26.5% vs 10.1%, P<0.001).2 No substantially reduced IOP was reported, and the proportions of patients with increased IOP were similar between groups.2 We report the case of a glaucoma patient with VMT who experienced transiently lowered IOP and choroidal effusion after ocriplasmin injection.
Case description
Approval was received from the patient and Illinois Retina Associates to access the patient’s medical records. Rush University Medical Center reviewed and considered the study Institutional Review Board exempt. Dr McClintock presented this study at Rush University Medical Center.
A 77-year-old Caucasian male with bilateral advanced glaucoma previously underwent cataract extraction with posterior chamber intraocular lens implantation in both eyes. An neodymium-doped yttrium aluminum garnet capsulotomy was subsequently performed in the right eye, and an Ahmed glaucoma valve was implanted to manage high IOP (average 28 mmHg). The patient had been initially referred to us at this time for VMT with concomitant epiretinal membrane (ERM) in the right eye. With uncorrected VA 20/40 in the right eye, the patient opted for observation. Initially there was a reduction in IOP, but by 4 weeks after glaucoma surgery the IOP returned to preoperative levels. During the observation period, a bleb needling over the plate was attempted, without significant success. A month following, both eyes underwent trabeculectomy with mitomycin C. After the trabeculectomy, the IOP ranged from 18 to 22 mmHg while on three topical glaucoma (IOP-lowering) medications: dorzolamide, brimonidine, and bimatoprost. Progressive VA decline in the right eye attributable to worsening VMT prompted the patient to request ocriplasmin.
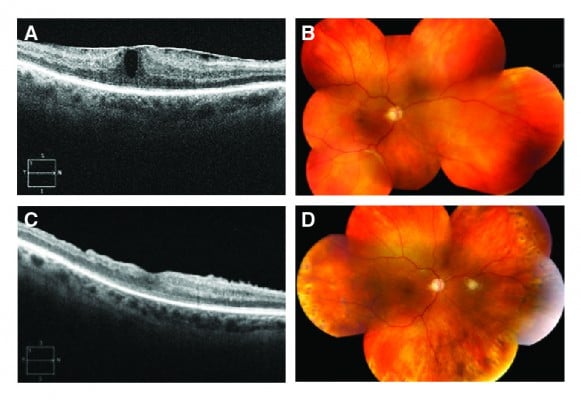
On the day of injection, VA was 20/80-1 in the right eye (Figure 1A) and 20/20-1 in the left eye. IOP was 19 mmHg in the right eye and 10 mmHg in the left eye. A preinjection exam showed a deep anterior chamber in the right eye, a superotemporal tube without visible obstruction, patent peripheral iridotomy superonasally, and posterior chamber intraocular lens with open posterior capsule. The posterior segment had trace vitreous hemorrhage inferiorly (1 week before injection); no retinal breaks were visible before or after the injection with careful scleral depression. The patient experienced photopsias in the right eye post injection.
At 1 week post injection, VMT was resolved and VA was 20/70-1 (Figure 1B). IOP decreased 8 mmHg to a final reading of 11 mmHg. At 1 month post injection, flashing lights were reported in the temporal periphery. VA was 20/70-2 and IOP decreased to 7 mmHg (Figure 1C). All glaucoma medications were discontinued in the right eye, and atropine and prednisolone were initiated. The anterior chamber was stable and deep, with Seidel-negative bleb. There was no obvious change in the trabeculectomy bleb morphology after the injection. There did appear to be elevation of the bleb over the plate following the injection; however, the conjunctiva appeared thickened. There was serous choroidal effusion and inferior retinal detachment (Figure 1D), with no visible retinal break.
At 2 months post injection, VA was 20/60-1 and IOP increased to 17 mmHg (Figure 2A). Choroidal effusion resolved. Retinal detachment persisted inferiorly (Figure 2B), with peripheral vitreous attachment noted outside of the inferotemporal arcade. The patient requested vitrectomy in the right eye to treat persistent ERM and retinal detachment, presumed tractional (ie, significant vitreous traction was seen both preoperatively and at time of vitrectomy, in addition to no visible retinal breaks).
A vitrectomy was performed approximately 3.5 months post injection. During surgery, vitreoretinal adhesion was noted for 360 degrees in the near periphery. The retinal detachment extended only to the equator and no retinal break was found in the detached retina. A small retinal hole was identified along the superotemporal arcade in attached retina. The ERM and internal limiting membrane were peeled, and retina reattached with 360-degree endolaser photocoagulation and fluid–gas exchange. At 16 weeks post surgery (Figure 2C, D), VA was 20/50+, and IOP was 18 mmHg with the patient on no glaucoma medications.
Discussion
To our knowledge, this is the first case report of IOP decrease and choroidal effusion after ocriplasmin injection. IOP was higher in the right eye vs the left eye before injection, despite treatment with IOP-lowering medications and a glaucoma drainage device in the right eye. Occluded devices can lead to IOP increases. Ocriplasmin is a recombinant truncated form of the human enzyme plasmin that has proteolytic effects on fibrin, fibrinogen, fibronectin, collagen, and laminin,2,3 and may have lowered IOP by degrading vitreous or connective tissue, in a hypothetically occluded device or the surrounding fibrous capsular bleb, resulting in serous choroidal effusion and retinal detachment. For instance, there may have been lysis of a small non-visible fibrin clot from hemorrhage, or vitreous or other proteinaceous material occluding the glaucoma drainage tube. There is also a possibility that the enzymatic activity may have increased the permeability of the pseudocapsule around the drainage implant, leading to decreased IOP. Previous reports support a role for plasmin-mediated proteolysis in clearing occluded glaucoma drainage devices.4,5 In addition, persistent peripheral vitreoretinal traction likely contributed to the persistent retinal detachment. It is unlikely that the tractional retinal detachment caused the low IOP, which is usually caused by rhegmatogenous retinal detachments. Given that there were no identifiable retinal breaks in the detached retina, aqueous humor would likely not have had access to the subretinal space. If the decrease in IOP was due to the detachment, one would expect the IOP to have increased following the repair of the detachment, which did not occur. In summary, advanced glaucoma patients with VMT should be carefully monitored for IOP changes after intravitreal injection of ocriplasmin.
Acknowledgments
Writing support provided by ThromboGenics and executed by Meridius Health Communications.
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
Dr MacCumber reported receiving consultant fees from Allergan, Genentech, Optos, Regeneron, ThromboGenics and receiving grant support from Allergan, ArcticDx, Regeneron, Sequenom, and ThromboGenics. Dr McClintock reported no conflicts of interest.
References
Jackson TL, Nicod E, Simpson A, Angelis A, Grimaccia F, Kanavos P. Symptomatic vitreomacular adhesion. Retina. 2013;33(8):1503–1511. | ||
Stalmans P, Benz MS, Gandorfer A, et al. Enzymatic vitreolysis with ocriplasmin for vitreomacular traction and macular holes. N Engl J Med. 2012;367(7):606–615. | ||
JETREA [package insert]. Iselin, NJ: ThromboGenics, Inc.; 2014. | ||
Tsui I, Airiani S, Wen A, El-Sawy T, Fine HF, Maris PJ Jr. Intravitreal injection of tissue plasminogen activator as treatment for an occluded pars plana glaucoma tube. Clin Ophthalmol. 2009;3:91–93. | ||
Zalta AH, Sweeney CP, Zalta AK, Kaufman AH. Intracameral tissue plasminogen activator use in a large series of eyes with valved glaucoma drainage implants. Arch Ophthalmol. 2002;120(11):1487–1493. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



